Introduction
Breast diseases encompass a wide spectrum of
inflammatory, benign and malignant conditions. However, sometimes
malignant lesions may arise from benign ones, or these conditions
may mimic or mask one another, presenting clinicians with intricate
diagnostic and management challenges (1). Granulomatous mastitis (GM) is a rare
inflammatory condition of the breasts with an unknown etiology,
with an estimated incidence of 2.4 per 100,000 women (2). This infrequent non-malignant disease
typically impacts women during their childbearing years, with a
higher incidence in some Middle Eastern countries such as Iran and
Turkey (3). The primary feature of
the condition is non-caseous granulomatous inflammation located
near the ducts and lobules of the breast (4,5).
Ductal carcinoma in situ (DCIS) is the pre-cancerous stage
of breast cancer, and it refers to an abnormal growth of luminal
cells restricted to the ductal-lobular system of the breast
(6,7). Before the development of breast
screening, DCIS was rarely diagnosed (7); it used to account for only 1-2% of
newly diagnosed breast cancer cases, but more recently, the rate
has markedly increased to 20-30% (8-10).
Through penetration of the ductal basement membrane and invasion of
the surrounding tissues, DCIS can transform into invasive breast
cancer (7). Synchronous
presentation of carcinoma in situ with GM is an extremely
rare phenomenon, with only a few cases being reported in the
literature (11-13).
The present study reports an intriguing case of a
30-year-old lactating woman who was initially diagnosed with
recurrent GM, which eventually proved to be masking an underlying
DCIS.
Case report
Patient information
A 30-year-old woman presented to the Breast Clinic
at Smart Health Tower (Sulaymaniyah, Iraq) on December 2022 with
left breast pain that had persisted for 7 days. The patient had
three children and had experienced one miscarriage. The patient was
currently lactating due to a newborn child and had lactated from
the right breast for a total of 4 years and 3 months. A paternal
aunt had been diagnosed with breast cancer when in her forties and
was still alive. The patient stated that she had undergone an
operation for resection of a left axillary mass in 2013 and that
the histopathological examination (HPE) was benign. Other than a
history of using anti-inflammatory medication, the patient had no
other notable medical history, no oral contraceptive use and no
history of smoking.
The first presentation to the same breast clinic
mentioned with lumps and swelling at the same site dates back to
December 2020. Investigations such as breast ultrasound (US)
examination were performed. The patient had a painful lump,
swelling and axillary lymphadenopathy, and the US finding showed a
large collection of unknown fluid with surrounding inflammation,
and an inverted nipple with associated axillary nodal enlargement.
The patient was clinically diagnosed with GM and underwent
conservative management with antibiotics, steroids and methotrexate
as follows: 500 mg ciprofloxacin twice per day orally for 5 days,
20 mg prednisolone daily orally for 7 days and 2.5 mg methotrexate
twice per day orally for 7 days. On December 2020 (7 days post
presentation), the patient returned to the clinic. The antibiotic
was stopped, the methotrexate dose was tapered (2.5 mg daily for 30
days) and the prednisolone was continued at the same dose. On
January 2021, a new US examination showed multiple collections on
the skin and decrease of the inflamed tissue next to the skin
surface, showing regression of the disease; therefore, drainage was
performed for the breast collection under local anesthesia, with a
prescription of prednisolone (20 mg daily for 20 days). After ~20
days, in January 2021, the disease responded to the medications and
an almost total response was achieved. Tapering of the prednisolone
was started (10 mg daily for 1 week, 5 mg daily for 1 week and then
5 mg on alternative days for 1 week) and a 3-month follow-up was
advised. The patient returned in June 2021 and US results showed
only marks of old mastitis; therefore, a 1-year follow-up was
advised. In June 2022, when the patient came back in the first
trimester of pregnancy, a breast US examination showed the same
result as that on the last visit, hence the patient was advised to
come back after delivery, which is when presentations of the
disease were once again apparent.
Clinical findings
On clinical examination, there was a large, palpable
and painful lump in the left breast with axillary lymphadenopathy
associated with localized swelling of the lower part of the
breast.
Diagnostic assessment
Breast US showed a full-length ectatic duct from the
nipple root toward the 5-7 o'clock position, with a heterogenous
internal echo associated with mild surrounding edema and reactive
axillary lymph nodes. This was suggestive of the recurrence of
GM.
Therapeutic intervention
Surgical resection was decided upon due to the
recurrence of GM at the same site that was refractory to therapy.
Following a preoperative assessment, under general anesthesia,
excision of the left breast lump was performed using a 10-cm radial
elliptical incision, a corrugate drain was put in and the wound was
closed in layers. The surgical specimen was marked with stitches
and sent for HPE (Data S1). The
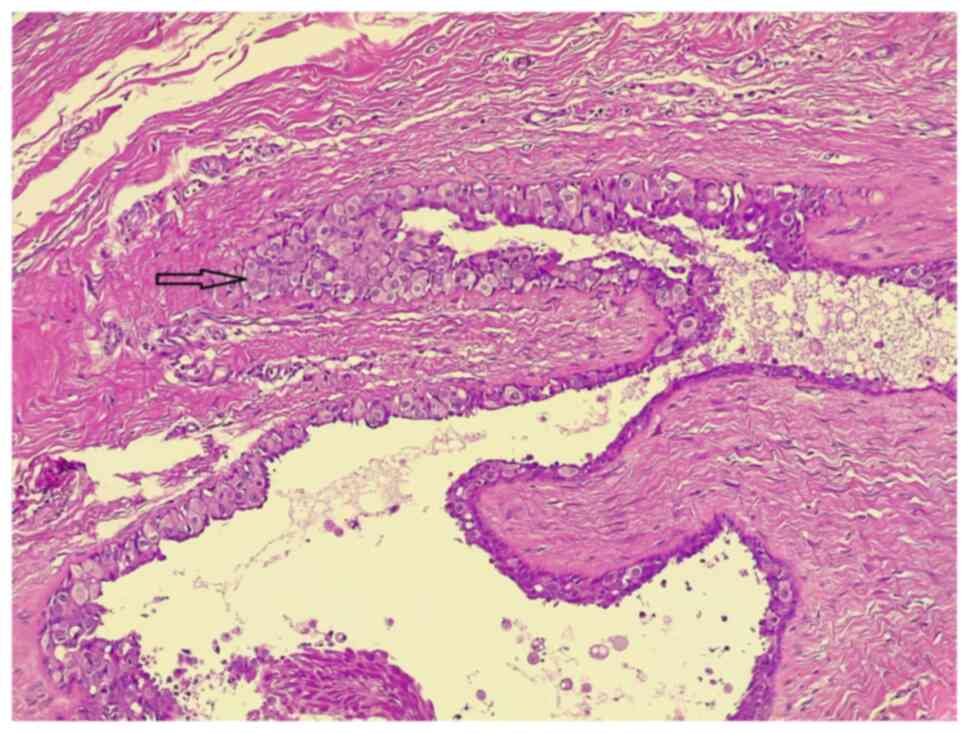
HPE revealed extensive DCIS with apocrine features without invasion
(Fig. 1), while other pathological
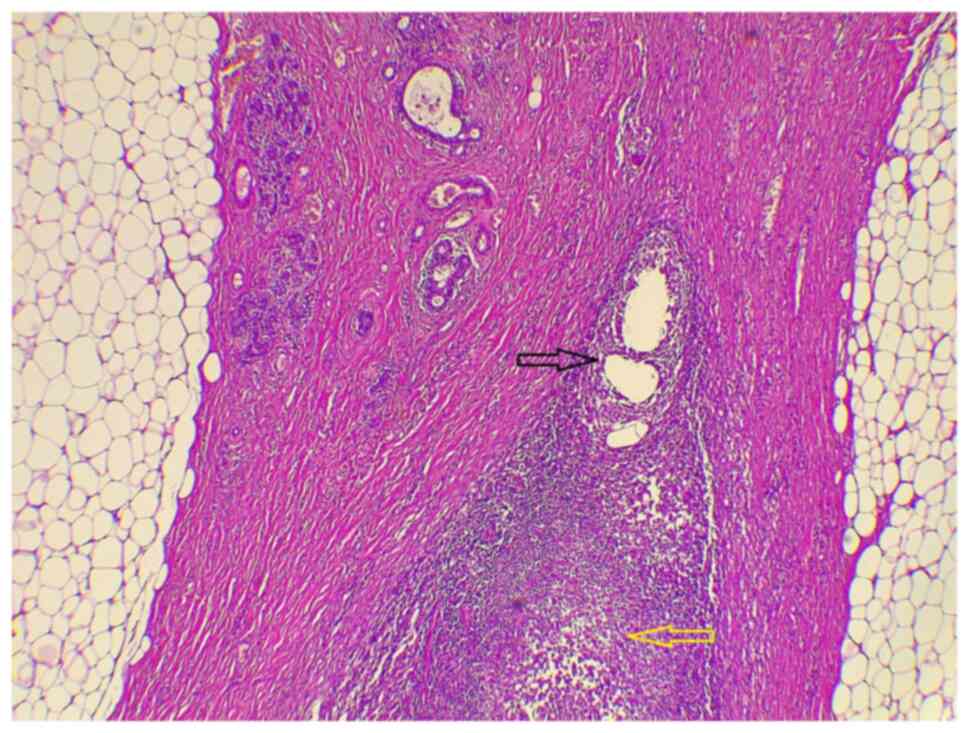
findings included lactational changes, acute suppurative GM with
abscess formation and fat necrosis (Fig. 2). The pathological staging from the
Tumor-Node-Metastasis staging system was pTisNx (14).
Following breast multidisciplinary team (MDT)
recommendations, additional investigations such as mammography
(MMG) and magnetic resonance imaging (MRI) were performed. The MMG
of the right breast showed only a solitary benign-looking
calcification, while that of the upper outer quadrant of the left
breast showed an operative bed deformity with trabecular
thickening, associated with regional skin thickening. Additionally,
in the central part of the left breast, at mid-depth, below the
scar line, there were two rounded scattered faint
micro-calcifications; the breast imaging-reporting and data system
(BI-RADS) score (15) was M2
bilaterally. Breast MRI revealed a clumped focal non-mass-like
enhancement measuring 20x6 mm within a focally ecstatic duct in the
left breast and other smaller borderline foci measuring 4-5 m. The
collective measurements were 60x50 mm, with a BI-RADS score of
MR-4. In addition, in the surgical bed, there was a focal
heterogenous non-mass-like enhancement measuring 19x13 mm and
ending 12 mm from the pectoralis major muscle. Both axillae were
clear and no suspicious lymph nodes were apparent
radiologically.
The investigation results were presented again in
another MDT session, and the decision was made to perform a
revision of the left breast surgical bed in the form of a simple
mastectomy, with axillary sentinel lymph node biopsy (SLNB) and
right breast-wide local excision (WLE) of the non-mass-like
enhancement after marking on the skin. A left-sided mastectomy was
performed by Stewart incision with axillary SLNB after methyline
blue dye injection. The right breast WLE of the marked area on the
skin was performed using a crescent incision; both wounds were
closed in layers, and the sample was again sent for HPE. For the
left breast, the HPE report showed no residual invasive tumor, no
carcinoma in situ, tumor-free excised axillary lymph nodes
and N0 pathological staging. The report of the right breast showed
only benign non-proliferative fibrocystic changes, duct ectasia
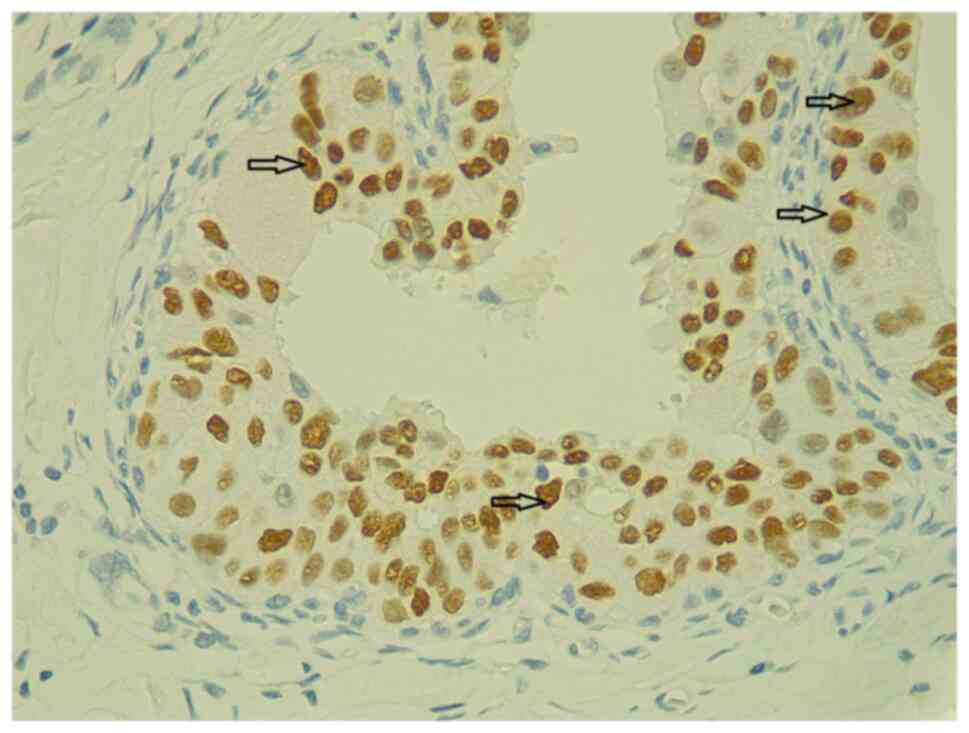
with stromal fibrosis and no malignancy. The immunohistochemical
(IHC) study of estrogen receptor expression showed positive
staining with a score of 8 in the Allred scoring system (16), supporting the DCIS component
(Fig. 3) (Data S1).
Follow-up
The postoperative period was uneventful after both
surgical sessions. The patient was referred to an oncologist for
further management. Adjuvant hormone therapy using tamoxifen (20
mg, 1*1) was initiated for 5 years, and after 6 months, follow-up
by breast US was performed, with an annual MMG and MRI recommended
if indicated. Genetic testing was offered by the oncologist but the
patient refused it due to the cost. The patient remained free of
disease for 6 months after the surgical procedure and the last
follow-up was in September 2023.
Discussion
DCIS is an unusual proliferation of the epithelial
cells of the mammary ducts without movement into other parts of the
breast parenchyma (17). DCIS is
surrounded by an intact basement membrane and bordered by a layer
of semi-continuous myoepithelial cells (18). Among the benign chronic inflammatory
breast diseases, such as periductal mastitis and lactational
mastitis (19), GM is the least
common and has an unclear etiology; it is characterized by the
formation of a non-caseating granuloma, with an abscess and the
presence of lymphocytes, multi-nucleated giant cells, plasma cells
and epithelioid histiocytes (17,20).
In 1972, Kessler and Wolloch (18) reported the first case of GM and
stated that it can be confused with breast cancer, since the
diseases share similarities in clinical signs and presentations,
such as lumps, pain, swelling, skin changes, abscesses,
ulcerations, sinus tracts and fistulas, in severe or chronic
patients, and are sometimes associated with axillary
lymphadenopathy. By contrast, DCIS is rarely symptomatic or
palpable clinically (21). In some
instances, patients have been clinically diasgnosed with breast
cancer, leading to a complete mastectomy and lymph node removal,
only to later discover through pathological analysis that they
actually had GM (18). Furthermore,
there have been uncommon cases of individuals first diagnosed with
GM and managed non-invasively, who were then discovered to have
breast cancer after surgical intervention due to no significant
improvement in their condition (22). Only in rare instances, has the
literature reported concurrent GM and carcinoma in the same breast
(11-13).
The reason behind the development of DCIS from
normal breast tissue is unknown; genetic predisposition plays a
role, not in all, but in some patients who have BRCA1 DNA repair
associated (BRCA1) and BRCA2 mutations (23). Some studies have shown that there
are other risk factors, such as being 35 years of age or older,
ethnicity, nulliparity or pregnancy at an older age, dense breasts
and a family history of breast cancer, especially in first-degree
relations. Other studies have investigated the relationship between
the incidence of DCIS and behavioral risk factors, such as the use
of nonsteroidal anti-inflammatory medications, aspirin, alcohol,
smoking, physical activity and the intake of dietary β-carotene
(24-26).
Moreover, the pathogenesis of GM has also not been determined and
scholars have different hypotheses regarding the mechanisms
involved, for instance: i) Autoimmunity, since GM has a significant
response to immunosuppressants such as steroids and methotrexate;
ii) infections, even though the exact pathogenic bacteria have not
been discovered yet; and iii) hormonal disorders, where
hyperprolactinemia seems to act as a triggering factor (23). Inflammation has been linked to
increased cancer risk and death (27,28).
In cohort studies with a large population size, Lambe et al
(29) and Chen et al
(30) reported that women with a
history of mastitis had a significantly higher risk of developing
breast cancer (P<0.001). In an analysis of genetic polymorphisms
in breast cancer and GM, gene mutations in the
methylenetetrahydrofolate reductase C677T variant, plasminogen
activator inhibitor 1 and angiotensin I converting enzyme were
discovered (31). In another study
of series of three GM cases in 2021, 12,115 mRNAs were analyzed
from GM and normal tissues, and GM was found to be enriched in
genes that were significantly highly expressed in breast cancer
tissues (32). After a review of
the literature, no association was found between BRCA1 or BRCA2
gene mutation and GM.
The current study presents the case of a patient
with a synchronous diagnosis of GM and DCIS. The patient had a
second-degree family history of breast cancer and a history of
using anti-inflammatory medication. Similar to the patients in most
of the concurrent GM and breast cancer cases, the current patient
was also of reproductive age. In a study by Özşen et al
(11), a similar 35-year-old woman
presented with swelling in the right breast. Via core needle
biopsy, the patient was initially diagnosed with GM; however, a
later excisional surgery was performed, as the patient lacked a
proper response to treatment, which resulted in a diagnosis of DCIS
after a second HPE and IHC examination. Oddó et al (12) presented the case of another
44-year-old woman with painful swelling in the left breast. The
patient was diagnosed with GM, but did not respond to any of the
provided antibiotics. A biopsy was performed, which again showed GM
with DCIS. The study by Tavakol et al (13), which is the last concurrent case
report at the time of the present study, reported the case of
a 35-year-old female presenting with pain and a lump in the right
breast. A core needle biopsy showed lobular carcinoma in
situ and GM, and the patient was treated (prednisolone,
nonsteroidal anti-inflammatory drugs and hydroxychloroquine) and
kept on follow-up (13). In the
present study, as well as the aforementioned studies, both GM and
breast carcinoma were found in the same breast. However, it is
still feasible to have GM present in one breast and carcinoma in
the other breast (33).
The only approach for a definite diagnosis of GM is
tissue diagnosis to exclude other pathologies, such as breast
carcinoma (34). DCIS can be easily
detected by MMG since ~75% of DCIS lesions contain calcifications,
but the other 25% can be underestimated by MMG, so the procedure
should be followed by a tissue biopsy for a definite diagnosis
(7). For the current case, a tissue
biopsy was obtained after the first presentation in 2020, and the
HPE result was GM. As the site was the same as the previous
pathology, a tissue biopsy was not taken again after the last
presentation, with the assumption of reccurrence.
Scientists and clinicians have always been intrigued
by the connection between inflammation and cancer. Inflammation may
be a result of infection or autoimmune diseases, but the precise
biological link between GM and malignant lesions remains unclear
due to the limited number of case studies. Long-term inflammation
causing DNA damage is one of the key causes of malignancy. Other
possible causes include DNA methylation, abnormal regulation of
microRNA, and the presence of common genes involved in both
autoimmunity and cancer development (13,35).
Treatment options for GM vary due to a vague
etiology, including surgical management (drainage, excision and
mastectomy), close observation, antibiotics, immunosuppressants and
anti-inflammatory medications (20). For patients diagnosed with DCIS, a
combination of surgery, radiation and endocrine therapy is used
accordingly (36). Multiple
treatment plans, including antibiotics, anti-inflammatory drugs,
immunosuppressants, drainage and surgical excision, were used for
the current case during chronic presentations on follow-up
examination. The final decision after full investigations and
confirmation of both diseases was to perform a mastectomy with
axillary SLNB.
In conclusion, the present case demonstrates the
challenges associated with identifying and diagnosing breast cancer
in a patient with recurrent GM or a previous history of GM, making
the presence of GM a key alert for surgeons to search for secondary
pathologies. The question of whether GM can lead to the development
of cancer remains debatable unless even more cases are encountered
and further research establishes a connection between breast cancer
and GM.
Supplementary Material
Supplementary Materials and
methods
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
SHH was responsible for the data collection, follow
up of the patient and final approval of the manuscript. AMS was a
major contributor to the conception of the study, as well as in the
literature search for related studies. LRAP was the radiologist who
performed the assessment of the GM. AMA was the pathologist who
perfomed the histopathological diagnosis. HMD and HOA were involved
in the literature review, the design of the study and the critical
revision of the manuscript. FHK, BOH and ASM were involved in the
literature review, the writing of the manuscript, and the data
analysis and interpretation. BOH and FHK confirm the authenticity
of all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Salih AM, Pshtiwan LR, Abdullah AM,
Qaradakhy AJ, Kakamad FH, Ali HO, Salih KM, Rahim HM, Abdalla BA,
Hassan MN and Mohammed SH: Carcinoma arising from fibroadenoma;
presentation and management; a case series. Barw Med J. 1:1–28.
2023.
|
|
2
|
Bacon DR, Ngeve SM and Jordan SG:
Granulomatous mastitis: An underdiagnosed inflammatory disease
afflicting minority women. Radiol Case Rep. 16:3990–3994.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Martinez-Ramos D, Simon-Monterde L,
Suelves-Piqueres C, Queralt-Martin R, Granel-Villach L,
Laguna-Sastre JM, Nicolau MJ and Escrig-Sos J: Idiopathic
granulomatous mastitis: A systematic review of 3060 patients.
Breast J. 25:1245–1250. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Esmaeil NK, Salih AM, Hammood ZD, Pshtiwan
LR, Abdullah AM, Kakamad FH, Abdullah HO, Ahmed GS, Abdalla BA and
Salih RQ: Clinical, microbiological, immunological and hormonal
profiles of patients with granulomatous mastitis. Biomed Rep.
18(41)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Esmaeil NK, Salih AM, Pshtiwan LR,
Muhialdeen AS, Abdullah AM, Hama JI, Hammood ZD, Kakamad FH, Tahir
SH, Abdalla BA, et al: Management of idiopathic granulomatous
mastitis: A single institution experience. Breast Care (Basel).
18:231–238. 2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mahmood ZH, Mohemed FM, Fatih BN, Qadir AA
and Abdalla SH: Cancer publications in one year (2022); a
cross-sectional study. Barw Med J. 1:2023.
|
|
7
|
Van Seijen M, Lips EH, Thompson AM,
Nik-Zainal S, Futreal A, Hwang ES, Verschuur E, Lane J, Jonkers J,
Rea DW, et al: Ductal carcinoma in situ: To treat or not to treat,
that is the question. Br J Cancer. 121:285–292. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Allred DC: Ductal carcinoma in situ:
Terminology, classification, and natural history. J Natl Cancer
Inst Monogr. 2010:134–138. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ward EM, DeSantis CE, Lin CC, Kramer JL,
Jemal A, Kohler B, Brawley OW and Gansler T: Cancer statistics:
Breast cancer in situ. CA Cancer J Clin. 65:481–495.
2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ryser MD, Hendrix LH, Worni M, Liu Y,
Hyslop T and Hwang ES: Incidence of ductal carcinoma in situ in the
United States, 2000-2014. Cancer Epidemiol Biomarkers Prev.
28:1316–1323. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Özşen M, Tolunay Ş and Gökgöz MŞ: Case
report: Ductal carcinoma in situ within a granulomatous mastitis.
Eur J Breast Health. 14:186–188. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Oddó D, Domínguez F, Gómez N, Méndez GP
and Navarro ME: Granulomatous lobular mastitis associated with
ductal carcinoma in situ of the breast. SAGE Open Med Case Rep.
7(2050313X19836583)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Tavakol M, Alvand S, Azmoudeh Ardalan F
and Assarian A: Idiopathic granulomatous mastitis with incidental
lobular carcinoma in situ: A case report. Arch Breast Cancer.
9:315–319. 2022.
|
|
14
|
Rami-Porta R, Bolejack V and Goldstraw P:
The new tumor, node, and metastasis staging system. Semin Respir
Crit Care Med. 32:44–51. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Balleyguier C, Ayadi S, Van Nguyen K,
Vanel D, Dromain C and Sigal R: BIRADS classification in
mammography. Eur J Radiol. 61:192–194. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hammond ME, Hayes DF, Dowsett M, Allred
DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS,
Hayes M, et al: American society of clinical oncology/college of
American pathologists guideline recommendations for
immunohistochemical testing of estrogen and progesterone receptors
in breast cancer (unabridged version). Arch Pathol Lab Med.
134:e48–e72. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Benson JR and Dumitru D: Idiopathic
granulomatous mastitis: Presentation, investigation and management.
Future Oncol. 12:1381–1394. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kessler E and Wolloch Y: Granulomatous
mastitis: A lesion clinically simulating carcinoma. Am J Clin
Pathol. 58:642–646. 1972.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Scott DM: Inflammatory diseases of the
breast. Best Pract Res Clin Obstet Gynaecol. 83:72–87.
2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wolfrum A, Kümmel S, Theuerkauf I, Pelz E
and Reinisch M: Granulomatous mastitis: A therapeutic and
diagnostic challenge. Breast Care (Basel). 13:413–418.
2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kerlikowske K: Epidemiology of ductal
carcinoma in situ. J Natl Cancer Inst Monogr. 2010:139–141.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sakurai T, Oura S, Tanino H, Yoshimasu T,
Kokawa Y, Kinoshita T and Okamura Y: A case of granulomatous
mastitis mimicking breast carcinoma. Breast Cancer. 9:265–268.
2002.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yin Y, Liu X, Meng Q, Han X, Zhang H and
Lv Y: Idiopathic granulomatous mastitis: Etiology, clinical
manifestation, diagnosis and treatment. J Invest Surg. 35:709–720.
2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Virnig BA, Wang SY, Shamilyan T, Kane RL
and Tuttle TM: Ductal carcinoma in situ: Risk factors and impact of
screening. J Natl Cancer Inst Monogr. 2010:113–116. 2010.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Trentham-Dietz A, Newcomb PA, Storer BE
and Remington PL: Risk factors for carcinoma in situ of the breast.
Cancer Epidemiol Biomarkers Prev. 9:697–703. 2000.PubMed/NCBI
|
|
26
|
Wohlfahrt J, Rank F, Kroman N and Melbye
M: A comparison of reproductive risk factors for CIS lesions and
invasive breast cancer. Int J Cancer. 108:750–753. 2004.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Moore MM, Chua W, Charles KA and Clarke
SJ: Inflammation and cancer: Causes and consequences. Clin
Pharmacol Ther. 87:504–508. 2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Morrison L, Laukkanen JA, Ronkainen K,
Kurl S, Kauhanen J and Toriola AT: Inflammatory biomarker score and
cancer: A population-based prospective cohort study. BMC Cancer.
16(80)2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lambe M, Johansson ALV, Altman D and
Eloranta S: Mastitis and the risk of breast cancer. Epidemiology.
20:747–751. 2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chen YC, Chan CH, Lim YB, Yang SF, Yeh LT,
Wang YH, Chou MC and Yeh CB: Risk of breast cancer in women with
mastitis: A retrospective population-based cohort study. Medicina
(Kaunas). 56(372)2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Destek S, Gul VO and Ahioglu S: A variety
of gene polymorphisms associated with idiopathic granulomatous
mastitis. J Surg Case Rep. 2016(rjw156)2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhu Q, Wang L and Wang P: The
identification of gene expression profiles associated with
granulomatous mastitis. Breast Care (Basel). 16:319–327.
2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kaviani A, Zand S, Karbaksh M and Ardalan
FA: Synchronous idiopathic granulomatosis mastitis and breast
cancer: A case report and review of literature. Arch Breast Cancer.
4:32–36. 2017.
|
|
34
|
Kiyak G, Dumlu EG, Kilinc I, Tokaç M,
Akbaba S, Gurer A, Ozkardes AB and Kilic M: Management of
idiopathic granulomatous mastitis: Dilemmas in diagnosis and
treatment. BMC Surg. 14(66)2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cappelli LC and Shah AA: The relationships
between cancer and autoimmune rheumatic diseases. Best Pract Res
Clin Rheumatol. 34(101472)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Mitchell KB and Kuerer H: Ductal carcinoma
in situ: Treatment update and current trends. Curr Oncol Rep.
17(48)2015.PubMed/NCBI View Article : Google Scholar
|