Introduction
Fracture is the most common form of orthopedic
trauma and has a high global incidence. The prevention and
treatment of bacterial infection are important post-operation in
patients with fractures (1).
Antibiotics can effectively suppress infection by inhibiting
bacterial growth; however, bacteria can become resistant to
antibiotics after simultaneous multi-antibiotic therapy. Multi-drug
resistant organisms (MDROs) are characterized by resistance to at
least three antibiotics and infections with these organisms are
difficult to treat (2). The
occurrence of fracture-related infection often depends on the site
of injury, surgical incision size and open wounds. Although the
majority of studies on fracture-related infections have largely
identified reliable risk factors involved in the surgical and
recovery processes (1,3), little attention has been paid to MDROs
infection in patients with fractures. Notably, MDROs infection
often results in a worse outcome compared with infections with
non-resistant pathogens. Patients who suffer from
multidrug-resistant pathogens have been reported to exhibit a
3-fold increase in amputation (4,5).
Recent research has indicated that infections occurring in limb
fractures account for 80% of whole fracture-related infection
cases, and bones of the extremities are more likely to be infected
with common MDROs, such as methicillin-resistant Staphylococcus
aureus (MRSA) and extended-spectrum β-lactamases (ESBLs) (+)
Escherichia coli (6,7), suggesting that bones of the
extremities are more susceptible to MDROs infection. For patients
with fractures, effective empirical antibiotic treatment is vital
in the early periods. It has previously been indicated that
effective antibiotic use can greatly raise sensitivity and avoid
resistance (8). In addition,
eligible methods of pathogen prevention can inhibit nosocomial
infections (9). Nevertheless,
research on the prevalence of MDROs and the risk of MDROs infection
is still rare. To explore the epidemiology and drug resistance of
MDROs, and to discover the factors associated with MDROs infection
in patients with limb fractures, the present study collected
information on limb fracture cases, including age, sex, injury
sites, operative records, pathogens and drug resistance, and
provided evidence for clinical antibiotic treatment and pathogen
prevention.
Patients and methods
Data collection
The present study collected the medical records of
patients treated at Bayi Orthopedic Hospital (Chengdu, China)
between January 2020 and August 2022. The information was obtained
from the electronic medical record system, and included sex, age,
albumin levels, hemoglobin levels, diabetes diagnosis, length of
hospital stay, operative time, antibiotic use, open fracture,
repeated infection, whether patients were bedridden, operative
grade, fracture sites, implantation materials, injury factors,
incision type, surgical approach, body mass index (BMI) and
repetition of procedures. The inclusion criteria were as follows:
i) Patients diagnosed with a limb fracture; ii) infection occurred
after orthopedic surgery; iii) bacteria cultured from the wound
discharge (10). The exclusion
criteria were: i) Incomplete medical records; ii) fracture at other
sites; iii) preoperative infection. VITEK 2 Compact (bioMérieux)
automatic microbial analysis system and Microbiology Conventional
Panel MicroScan Negative Urine Combo 61 For MicroScan Analyzers 20
Panels (cat. no. B1017-414; Beckman Coulter, Inc.) were used for
strain identification and antimicrobial susceptibility testing. S.
aureus [American Type Culture Collection (ATCC) 25923], E.
coli (ATCC 25922) and Pseudomonas aeruginosa (ATCC
27853) (purchased from ATCC)were used for quality control.
Patients were considered bedridden if they were
unable to move or if they remained in bed for >2 weeks,
according to clinical need. Operative grade was scored as follows:
I, uncomplicated, low risk; Ⅱ, uncomplicated, medium risk; Ⅲ,
complicated, relatively high risk; IV, quite complicated, high
risk. Incision type was scored as follows: I, low infection risk;
II, medium infection risk; III, high infection risk.
Statistical analysis
SPSS 26.0 software (IBM Corp.) was used for
statistical analysis. The Kolmogorov-Smirnov test was used to
assess normality. Normally distributed data are presented as the
mean ± standard deviation and Student's t-test was performed to
compare group differences. Non-normally distributed data are
presented as median (Q1, Q3) and comparisons between groups were
made using Mann-Whitney U test. Categorical data are presented as
the number of cases and comparisons between the different groups
were made using the χ2 test. Binary logistic regression
was used to perform univariate and multivariate analyses. P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
A total of 114 patients with limb fractures who
suffered from infections were included in the present study. The
114 patients were divided into two groups: The MDRO group (47
cases, including 39 men and 8 women) and the non-MDRO group (67
cases, including 52 men and 15 women). The patients had a mean age
of 48.25±15.18 years, 91 (79.8%) were men and a subset of 13
(11.4%) presented with diabetes. Among the 114 patients, 47 (41.2%)
had upper limb fractures, 66 (57.9%) had lower limb fractures and
one (0.9%) had multiple fractures. Mechanical injury (38 cases,
33.3%) and fall (27 cases, 23.6%) were the main causes of
fractures. More details of patient characteristics are presented in
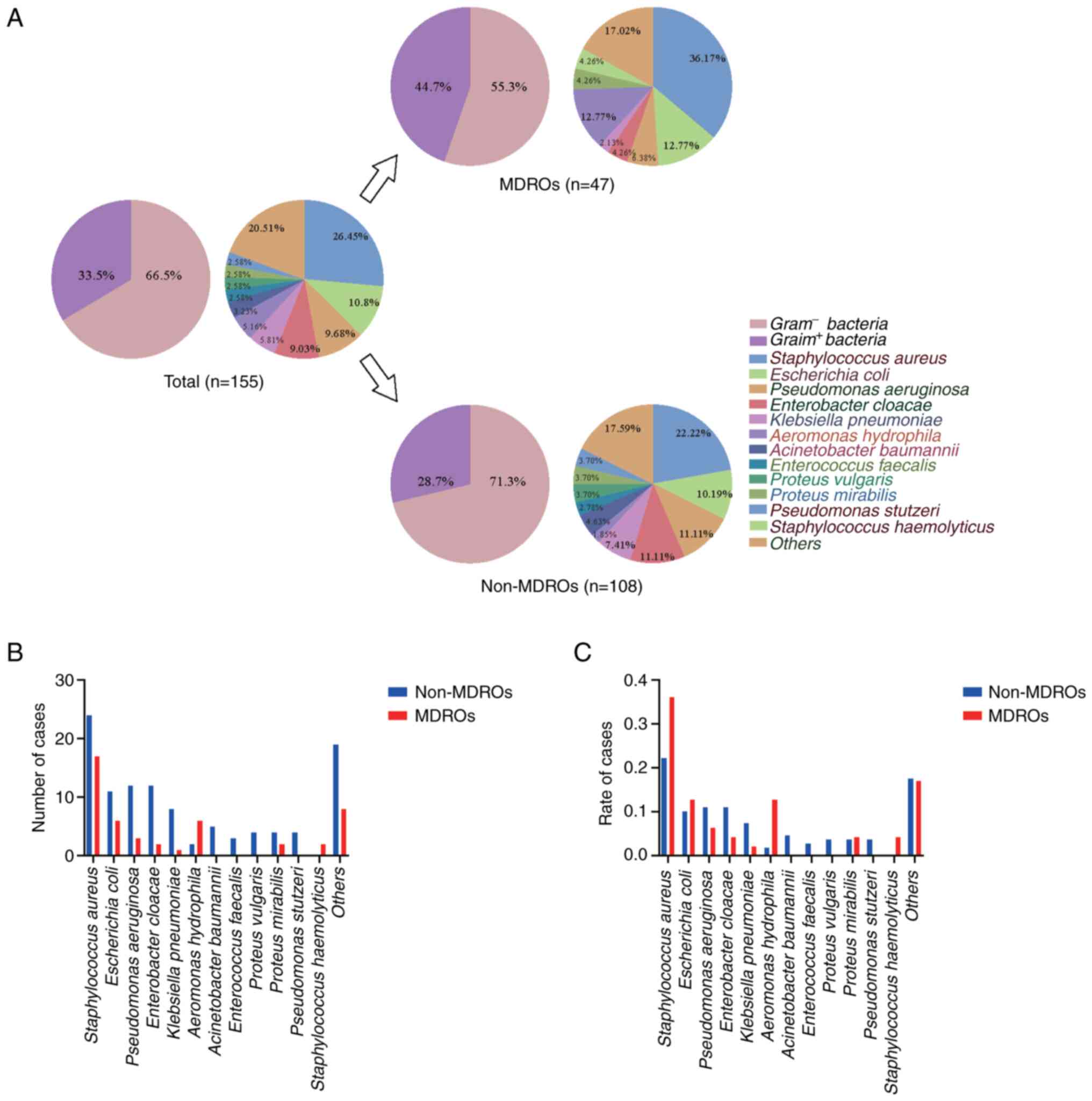
Table I. A total of 155 bacteria
were cultured from the 114 patients, of which 47 (41.2%) were
infected with MDROs. Among the 155 microorganisms, 52 (33.5%) were
gram-positive bacteria. A total of 85 (74.6%) patients were
infected with only one strain and 29 (25.4%) were infected with
multiple pathogens simultaneously. Klebsiella pneumonia,
P. aeruginosa, Enterobacter cloacae and
Proteusbacillus vulgaris infections occurred in combination
with each other in the MDROs group (Table SI). Bacteria distributions are
shown in Fig. 1A. There were
differences in the gram-positive bacteria rate between multi-drug
resistant pathogens and non-resistant pathogens. The MDROs
infection group had a higher rate of gram-positive bacterial
infections. The comparison of each bacterial strain between the
MDROs group and the non-MDROs group is shown in Fig. 1B and C. Bacteria, such as Aeromonas
hydrophila and Acinetobacter baumannii, only appeared in
the non-MDROs infection group (Fig.
1B). In addition, S. aureus was more frequently detected
in the MDROs group (Fig. 1C). In
the present study, S. aureus, a common microorganism that
usually causes nosocomial infections (3), was more likely to be resistant to
antibiotics. MRSA was the main pathogen of gram-positive MDROs
infection cases. Gram-negative pathogens, such as E. coli
and A. hydrophila also exhibited a high level of occurrence
in the MDROs group. MIC results of MDROs samples are summarized in
Tables II and III. As for gram-positive S.
aureus, resistance mainly focused on penicillins, erythromycin
and lincomycins. Gram-negative bacilli, such as E. coli and
K. pneumoniae, produce ESBLs to hydrolyze antibiotics and
thus become insensitive to cephalosporins. The clinical records of
antibiotic use were collected to analyze whether drug resistance
occurred after an antibiotic treatment. Clindamycin treatment may
induce high resistance in S. aureus. Gentamicin and
vancomycin are still effective methods to prevent those kinds of
pathogens (Table SII). Moreover,
ESBLs (+) bacteria, such as E. coli, K. pneumoniae
and P. vulgaris, accounted for almost half of the
gram-negative MDROs that exhibited resistance after prolonged
cephalosporin use (Table SII). In
summary, the results of the present study demonstrated that
bacteria varied in drug resistance during antibiotic therapy.
 | Table IDemographic and clinical
characteristics of the 114 patients with limb fractures. |
Table I
Demographic and clinical
characteristics of the 114 patients with limb fractures.
| Demographic
characteristic | Value |
|---|
| Mean ± SD age,
years | 48.25±15.18 |
| Sex, male/female
(%) | 91 (79.8)/23
(20.2) |
| Fracture sites, n
(%) | |
|
Upper
limb | |
|
Radius
and ulna | 2 (1.8) |
|
Humerus | 4 (3.5) |
|
Hand | 36 (31.5) |
|
Multiple
fracture | 5 (4.4) |
|
Lower
limb | |
|
Femur | 9 (7.9) |
|
Tibia
and fibula | 20 (17.5) |
|
Patella | 4 (3.5) |
|
Foot | 28 (24.6) |
|
Multiple
fracture | 5 (4.4) |
|
Upper and
lower | 1 (0.9) |
| Cause of injury, n
(%) | |
|
Mechanical | 38 (33.3) |
|
Fall | 27 (23.7) |
|
Traffic | 18 (15.8) |
|
Bruise | 14 (12.3) |
|
Others | 17 (14.9) |
| Clinical
characteristics | |
|
Mean ± SD
length of hospital stay, days | 19.2±11.8 |
|
Mean ± SD
hemoglobin, g/l | 130.1±19.2 |
|
Mean ± SD
albumin, g/l | 39.2±3.67 |
| Diabetes, n
(%) | 13 (11.4) |
| Infectious
pathogens, n (%) | |
|
1
strain | 85 (74.5) |
|
2
strains | 19 (16.7) |
|
>2
strains | 10 (8.8) |
| Operative grade, n
(%) | |
|
Ⅰ | 1 (0.9) |
|
Ⅱ | 10 (8.8) |
|
Ⅲ | 77 (67.5) |
|
Ⅳ | 26 (22.8) |
| Incision type, n
(%) | |
|
Ⅰ | 18 (15.8) |
|
Ⅱ | 45 (39.5) |
|
Ⅲ | 51 (44.7) |
 | Table IIResistance of multi-drug resistant
gram-positive bacteria. |
Table II
Resistance of multi-drug resistant
gram-positive bacteria.
| Antimicrobial | Staphylococcus
aureus (%) |
|---|
| Gentamicin | 5.88 |
| Ceftriaxone | 94.12 |
|
Ampicillin/Sulbactam | 94.12 |
|
Amoxicillin/Clavulanate potassium | 100.00 |
| Oxacillin | 94.12 |
| Penicillin | 94.12 |
| Vancomycin | 0.00 |
| Clindamycin | 82.35 |
| Erythromycin | 94.12 |
| Ciprofloxacin | 94.12 |
| Levofloxacin | 23.53 |
| Tetracycline | 11.76 |
| Rifampin | 29.41 |
| PCST | 35.29 |
| Cefoxitin | 5.88 |
| Moxifloxacin | 5.88 |
| Linezolid | 0.00 |
| Synercid | 5.88 |
 | Table IIIResistance of multi-drug resistant
gram-negative bacteria. |
Table III
Resistance of multi-drug resistant
gram-negative bacteria.
| Antimicrobial | Escherichia
coli (%) | Aeromonas
hydrophila (%) | Pseudomonas
aeruginosa (%) |
|---|
| Amikacin | 0.00 | 0.00 | 33.33 |
| Gentamicin | 66.67 | 0.00 | 33.33 |
| Tobramycin | 66.67 | - | 0.00 |
| Cefazolin | 100.00 | 100.00 | - |
| Cefoxitin | 16.67 | 50.00 | - |
| Cefuroxime | 100.00 | 16.67 | - |
| Ceftriaxone | 100.00 | 16.67 | - |
| Ceftazidime | 100.00 | 16.67 | 100.00 |
| Cefotaxime | 100.00 | 16.67 | - |
| Cefepime | 100.00 | 0.00 | 100.00 |
| Imipenem | 0.00 | - | 66.67 |
| Meropenem | 0.00 | 66.67 | 0.00 |
| Aztreonam | 100.00 | 0.00 | 100.00 |
|
Ampicillin/Sulbactam | 100.00 | 100.00 | - |
| Ampicillin | 100.00 | - | - |
|
Piperacillin/Tazobactam | 0.00 | 100.00 | 100.00 |
| Ciprofloxacin | 83.33 | 16.67 | 0.00 |
| Levofloxacin | 83.33 | 0.00 | 0.00 |
| PCST | 83.33 | 16.67 | - |
| Ertapenem | 0.00 | 83.33 | - |
| Tigecycline | 0.00 | 0.00 | - |
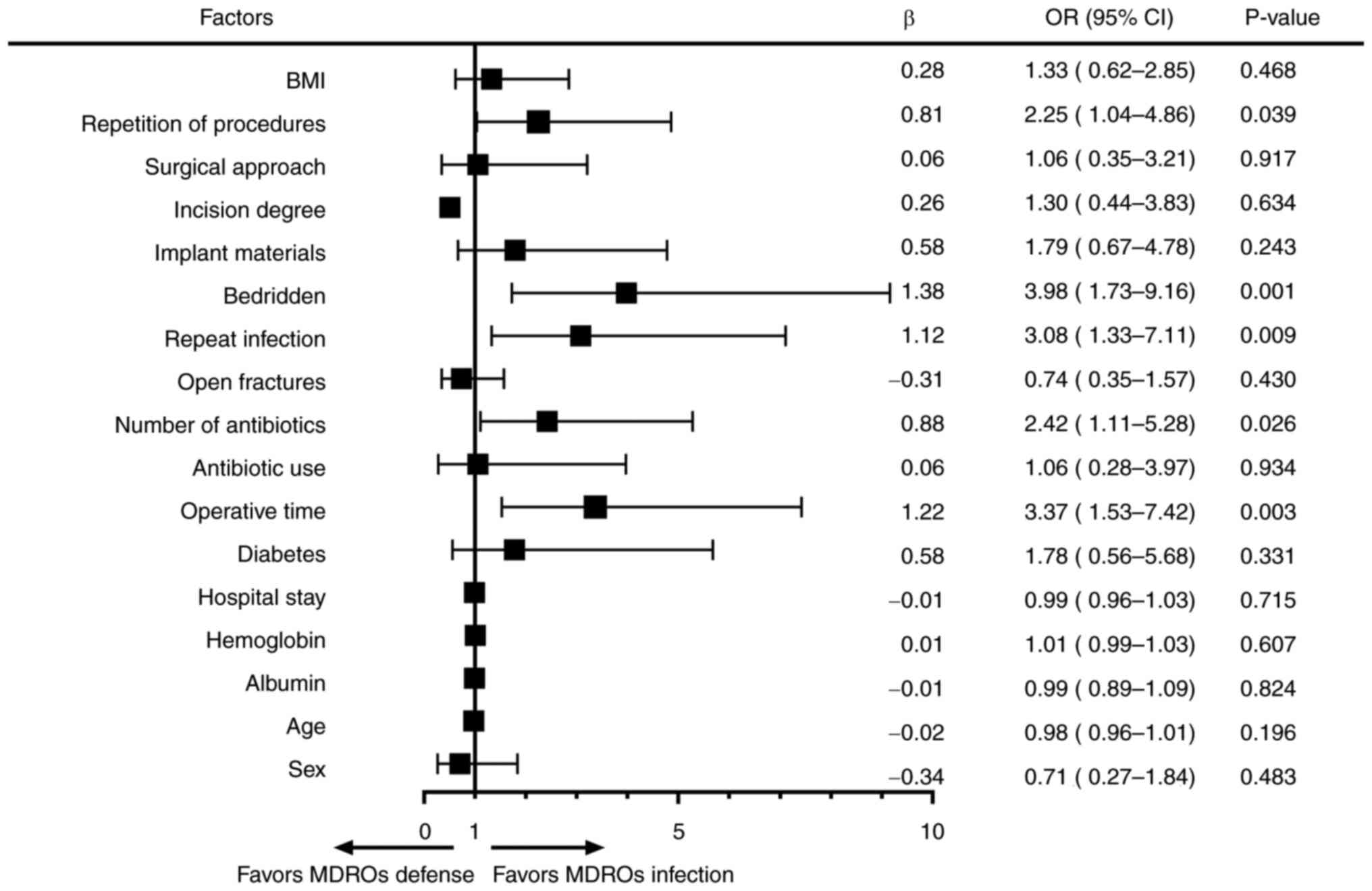
Univariate analysis of MDROs
infection
Univariate analysis was used to assess differences
between the two groups. Being bedridden, administration of >2
antibiotics, operative time >3 h, repeated infection and
repetition of procedures were closely associated with MDROs
infection (Table IV). Univariate
logistic analysis was also used to assess the hazard rate of each
factor (Fig. 2). Being bedridden
(OR, 3.98; P=0.001), administration of >2 antibiotics (OR, 2.42;
P=0.026), operative time >3 h (OR, 3.37; P=0.003), repeated
infection (OR, 3.08; P=0.009) and repetition of procedures (OR,
2.25, P=0.039) were identified as individual factors that may be
associated with MDRO infection.
 | Table IVUnivariate analysis of MDRO
infection. |
Table IV
Univariate analysis of MDRO
infection.
| Factor | Non-MDRO group | MDRO group | P-value |
|---|
| Sex | | | 0.482 |
|
Male | 52 | 39 | |
|
Female | 15 | 8 | |
| Mean ± SD age,
years | 51.3±12.0 | 46.0±14.7 | 0.196 |
| Mean ± SD albumin,
g/l | 39.2±3.5 | 39.1±4.0 | 0.826 |
| Mean ± SD
hemoglobin, g/l | 129.4±20 | 131.7±16.8 | 0.610 |
| Median hospital
stay (Q1, Q3), days | 15 (12, 24) | 13 (9, 25) | 0.327 |
| Diabetes | | | 0.326 |
|
Yes | 6 | 7 | |
|
No | 61 | 40 | |
| Operative time | | | 0.002 |
|
≥3 h | 18 | 26 | |
|
<3 h | 49 | 21 | |
| Antibiotic use | | | 0.934 |
|
Yes | 61 | 43 | |
|
No | 6 | 4 | |
| Number of
antibiotics | | | 0.025 |
|
0-2 | 48 | 24 | |
|
3+ | 19 | 23 | |
| Open fractures | | | 0.430 |
|
Yes | 42 | 26 | |
|
No | 25 | 21 | |
| Repeat
infection | | | 0.007 |
|
Yes | 13 | 20 | |
|
No | 54 | 27 | |
| Bedridden | | | 0.001 |
|
Yes | 14 | 23 | |
|
No | 53 | 24 | |
| Implant
materials | | | 0.239 |
|
Yes | 51 | 40 | |
|
No | 16 | 7 | |
| Incision
degree | | | 0.086 |
|
Ⅰ | 10 | 8 | |
|
Ⅱ | 32 | 13 | |
|
Ⅲ | 25 | 26 | |
| Surgical
approach | | | 0.917 |
|
Percutaneous | 9 | 6 | |
|
Open | 58 | 41 | |
| Repetition of
procedures | | | 0.038 |
|
Yes | 31 | 31 | |
|
No | 36 | 16 | |
| BMI | | | 0.467 |
|
≥25 | 24 | 20 | |
|
<25 | 43 | 27 | |
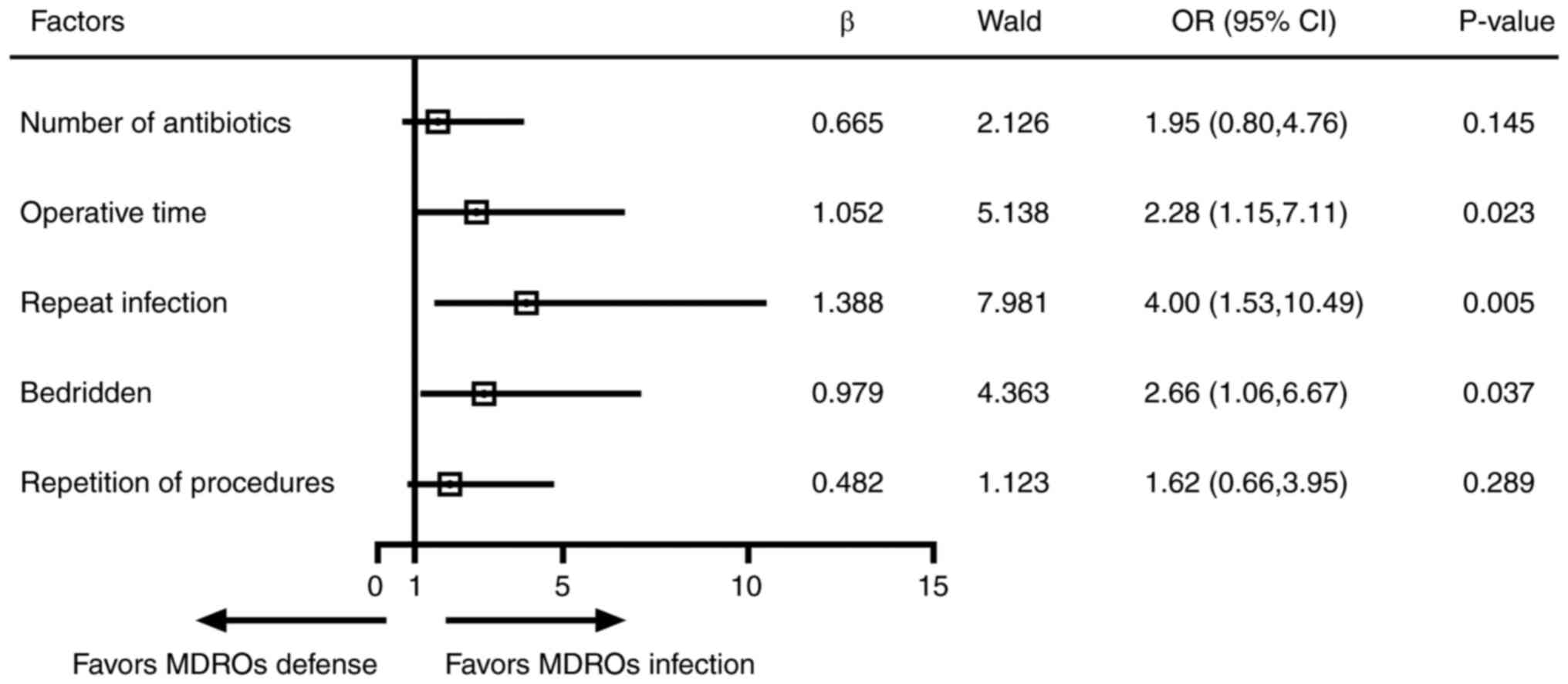
Multivariate analysis of MDROs
infection
To validate the association between the
aforementioned significant factors and MDROs infection,
multivariate binary logistic analysis was conducted. The results
showed that being bedridden (OR, 2.66; P=0.037), repeated infection
(OR, 4.00; P=0.005) and operative time >3 h (OR, 2.28; P=0.023)
were significant factors associated with MDROs infection (Fig. 3).
Discussion
Pathogens often colonize patients during orthopedic
surgery and recovery periods. Infection prevention is of great
importance to accelerate postoperative wound healing for patients
with fractures. Notably, inappropriate antimicrobial therapy can
facilitate bacterial resistance to drugs; MDROs can appear after
antibiotic use and have become a challenge to clinical treatment
and nursing (11,12). An anti-MDROs strategy is required
for pathogen defense. A study in the southwestern and northeastern
regions of China found that among all patients with fractures,
those with limb fractures have the highest likelihood of developing
infections (3). Furthermore, S.
aureus and E. coli were responsible for almost one-third
of pathogens (1,3). Similarly, the present study reported
that S. aureus and E. coli were major bacteria in
cases of limb infection. Furthermore, the majority of cases of MDRO
infection appeared to occur following corresponding antibiotic
treatment, suggesting that drug resistance mainly results from
antibiotic therapy. Perioperative use of antibacterial drugs is an
effective method of infection prevention (13). The present study found no
significant difference in antibiotic use between the two groups;
however, administration of three or more antibiotics increased the
incidence of MDROs infection. Antibiotics are the main cause of
pathogen resistance. Patients can suffer from repeated infection as
a result of failed control of pathogens in the early phase, and
supplemental and prolonged antibiotic therapy can eventually cause
bacterial resistance. It has been reported that, following lower
extremity surgery, a high proportion of patients undergo amputation
after infection with multi-drug resistant pathogens (4,5).
Multidrug-resistant pathogens colonize the wound area and can
invade the bloodstream to cause bacteremia. In addition, the
occurrence of necrosis near the unhealed wound can lead to
amputation (5).
It is well known that patients with low immunity
have an increased chance of infection with microbes, including
MDROs. Previous research has revealed that low albumin and
hemoglobin levels, often considered as evidence of low immunity,
are risk factors for clinical infection (14,15).
However, the results of the present study did not identify low
albumin and hemoglobin levels as risk factors for MDROs infection.
Diabetes, a metabolic disorder characterized by an injured immune
system, has long been reported to be associated with MDROs
infection (16,17). Previous studies have reported that
patients with a higher BMI are more likely to suffer from wound
infection (18,19). In obese patients, metabolic
disturbances can lead to chronic tissue inflammation, and impaired
adaptive and innate immunity (20).
Nevertheless, there is no evidence in the present study supporting
the relationship between diabetes or BMI and MDROs infection.
Therefore, a large cohort survey is required to verify this.
Notably, being bedridden has been shown to be associated with
pulmonary infection in elderly patients with hip fractures, and
this was also closely related with MDROs infection in the present
study (21). Being bedridden may
cause malnutrition, which decreases immune defense. In addition, a
lack of movement constrains the blood circulation to the injured
site, especially in patients with limb fracture; hypoxia in the
affected extremity can increase susceptibility to microbial
invasion (22,23).
Prolonged operative time has been reported to
increase morbidity in multiple injuries, such as in tibial plateau
fractures (24-26).
The present study demonstrated that ≥3 h of operative procedures
may increase the risk of MDROs infection. Long procedures often
result in heavy damage and incisions exposed to the air can promote
environmental bacterial colonization. A longer surgical time not
only increases the risk of infection but also inevitably increases
the possibility of MDROs infections. The subjects included in the
present study were all patients with post-operative infection.
Notably, the current study also revealed that patients that
underwent more than two operations exhibited a higher risk for
MDROs infection, suggesting that primary infection happens during a
surgical procedure. The present results are insufficient to
demonstrate the relationship between incision size and
drug-resistant bacterial infection. Further research should record
incision size in line with corresponding operative methods.
Hospital stay has long been hypothesized to affect wound healing.
Prolonged hospital stay can increase nosocomial infection risk,
especially in postoperative patients (27,28).
However, in the present study, length of hospital stay did not seem
to affect the incidence of MDROs infection. The present study also
analyzed implanted materials and surgical approaches, and it showed
that implanted materials or open surgical modes were not related to
MDROs infection, even though they were thought to have a
significant role in previous studies (29,30).
Although it has been reported that elderly patients
have a higher occurrence rate of MDROs infection (31), there was no significant difference
between the mean ages of the two groups in the present study.
Regional social structure may explain this discrepancy. Finally,
binary logistic regression analysis was performed to assess the
five factors that were revealed to be significant in MDROs
infection. Three of them were of importance in the prevention of
MDROs infection; in conclusion, shortened operative time, improved
early pathogen defense and activities in the affected limb may be
helpful to decrease MDROs invasion.
The main limitation of the present study was a
restricted sample size. In addition, the medical records are
limited to one center. A multi-center survey and additional patient
records are required in future studies. Besides, the records
included in the present study are not detailed enough. The present
study also failed to incorporate the changes in bacterial infection
before and after antibiotic usage, which is of significant
importance in developing antibiotic treatment strategies for
MDROs-infected patients. Including confounding factors, such as the
pre-admission medical conditions, in the analysis may also enhance
the reliability of the study results. The risk factors identified
in the present study should be appropriately applied in the
prevention of clinical infection. This includes the care of
long-term bedridden patients and strict measures to avoid
excessively prolonged surgical procedures. Furthermore, infections
caused by different MDROs may present variations in infection
characteristics, treatment and prognosis. A comprehensive
assessment of the impact of different MDROs on infections in
patients with limb fractures should be conducted, and tailored
intervention strategies should be developed.
Supplementary Material
Cases with co-infection.
Association between antibiotic therapy
and MDROs infection.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by Chengdu Municipal
Health Commission (grant no. 2022100).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JJ led and designed the project. HS, MZ and DD
collected data. HS performed the data analysis and statistical
analysis. HS interpreted the data and wrote the manuscript. All
authors contributed to the article, and read and approved the final
manuscript. HS and JJ confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Magiorakos AP, Srinivasan A, Carey RB,
Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter
G, Olsson-Liljequist B, et al: Multidrug-resistant, extensively
drug-resistant and pandrug-resistant bacteria: An international
expert proposal for interim standard definitions for acquired
resistance. Clin Microbiol Infect. 18:268–281. 2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lin S, Mauffrey C, Hammerberg EM, Stahel
PF and Hak DJ: Surgical site infection after open reduction and
internal fixation of tibial plateau fractures. Eur J Orthop Surg
Traumatol. 24:797–803. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Morris BJ, Unger RZ, Archer KR, Mathis SL,
Perdue AM and Obremskey WT: Risk factors of infection after ORIF of
bicondylar tibial plateau fractures. J Orthop Trauma. 27:e196–200.
2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mende K, Akers KS, Tyner SD, Bennett JW,
Simons MP, Blyth DM, Li P, Stewart L and Tribble DR:
Multidrug-Resistant and virulent organisms trauma infections:
Trauma infectious disease outcomes study initiative. Mil Med.
187(Suppl 2):S42–S51. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Campbell WR, Li P, Whitman TJ, Blyth DM,
Schnaubelt ER, Mende K and Tribble DR: Multi-Drug-Resistant
gram-negative infections in deployment-related trauma patients.
Surg Infect (Larchmt). 18:357–367. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang B, Xiao X, Zhang J, Han W, Hersi SA
and Tang X: Epidemiology and microbiology of fracture-related
infection: A multicenter study in Northeast China. J Orthop Surg
Res. 16(490)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhang Z, Liu P, Wang W, Wang S, Li B, Li
J, Yang B, Li M, Li Q, Yang H, et al: Epidemiology and drug
resistance of fracture-related infection of the long bones of the
extremities: A retrospective study at the largest Trauma Center in
Southwest China. Front Microbiol. 13(923735)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Baertl S, Walter N, Engelstaedter U,
Ehrenschwender M, Hitzenbichler F, Alt V and Rupp M: What is the
most effective empirical antibiotic treatment for early, delayed,
and late fracture-related infections? Antibiotics (Basel).
11(287)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lorenzoni VV, Rubert FDC, Rampelotto RF
and Hörner R: Increased antimicrobial resistance in Klebsiella
pneumoniae from a University Hospital in Rio Grande do Sul, Brazil.
Rev Soc Bras Med Trop. 51:676–679. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Notice on the Implementation of
Classification Management Measures for Medical Institution
Surgery-Medical Administration Office of the National Health
Commission [2022] No. 18. (http://www.nhc.gov.cn/yzygj/s7657/202212/5eb7ddbaa8004a4497c5f29d3a2a5b4d.shtml).
|
|
11
|
Lye DC, Earnest A, Ling ML, Lee TE, Yong
HC, Fisher DA, Krishnan P and Hsu LY: The impact of multidrug
resistance in healthcare-associated and nosocomial Gram-negative
bacteraemia on mortality and length of stay: Cohort study. Clin
Microbiol Infect. 18:502–508. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hung YP, Lee CC and Ko WC: Effects of
inappropriate administration of empirical antibiotics on mortality
in adults with bacteraemia: Systematic review and meta-analysis.
Front Med (Lausanne). 9(869822)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Langenhan R, Bushuven S, Reimers N and
Probst A: Peri-operative antibiotic treatment of bacteriuria
reduces early deep surgical site infections in geriatric patients
with proximal femur fracture. Int Orthop. 42:741–746.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nohl A, Hamsen U, Jensen KO, Sprengel K,
Ziegenhain F, Lefering R, Dudda M, Schildhauer TA and Wegner A:
Incidence, impact and risk factors for multidrug-resistant
organisms (MDRO) in patients with major trauma: A European
Multicenter Cohort Study. Eur J Trauma Emerg Surg. 48:659–665.
2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zhao K, Zhang J, Li J, Meng H, Wang Z, Zhu
Y, Hou Z and Zhang Y: Incidence and risk factors of surgical site
infection after intertrochanteric fracture surgery: A prospective
cohort study. Int Wound J. 17:1871–1880. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Martin ET, Kaye KS, Knott C, Nguyen H,
Santarossa M, Evans R, Bertran E and Jaber L: Diabetes and risk of
surgical site infection: A systematic review and meta-analysis.
Infect Control Hosp Epidemiol. 37:88–99. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kortram K, Bezstarosti H, Metsemakers WJ,
Raschke MJ, Van Lieshout EMM and Verhofstad MHJ: Risk factors for
infectious complications after open fractures; a systematic review
and meta-analysis. Int Orthop. 41:1965–1982. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Peel TN, Dowsey MM, Daffy JR, Stanley PA,
Choong PF and Buising KL: Risk factors for prosthetic hip and knee
infections according to arthroplasty site. J Hosp Infect.
79:129–133. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Olsen MA, Higham-Kessler J, Yokoe DS,
Butler AM, Vostok J, Stevenson KB, Khan Y and Fraser VJ: Prevention
Epicenter Program, Centers for Disease Control and Prevention.
Developing a risk stratification model for surgical site infection
after abdominal hysterectomy. Infect Control Hosp Epidemiol.
30:1077–1083. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
20
|
Andersen CJ, Murphy KE and Fernandez ML:
Impact of obesity and metabolic syndrome on immunity. Adv Nutr.
7:66–75. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yuan Y, Tian W, Deng X, Yue R, Ge X, Wu X
and Zhang P: Elderly patients with concurrent hip fracture and
lower respiratory tract infection: The pathogens and prognosis over
different bedridden periods. J Orthop Surg Res.
16(246)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Matsusaka K, Kawakami G, Kamekawa H, Momma
H, Nagatomi R, Itoh J and Yamaya M: Pneumonia risks in bedridden
patients receiving oral care and their screening tool: Malnutrition
and urinary tract infection-induced inflammation. Geriatr Gerontol
Int. 18:714–722. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Negishi K: Prevention of pressure ulcers.
Yakugaku Zasshi. 129:1483–1485. 2009.PubMed/NCBI View Article : Google Scholar : (In Japanese).
|
|
24
|
Shao J, Chang H, Zhu Y, Chen W, Zheng Z,
Zhang H and Zhang Y: Incidence and risk factors for surgical site
infection after open reduction and internal fixation of tibial
plateau fracture: A systematic review and meta-analysis. Int J
Surg. 41:176–182. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Colman M, Wright A, Gruen G, Siska P, Pape
HC and Tarkin I: Prolonged operative time increases infection rate
in tibial plateau fractures. Injury. 44:249–252. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ang H and Sun X: Risk factors for
multidrug-resistant Gram-negative bacteria infection in intensive
care units: A meta-analysis. Int J Nurs Pract.
24(e12644)2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kusachi S, Kashimura N, Konishi T, Shimizu
J, Kusunoki M, Oka M, Wakatsuki T, Kobayashi J, Sawa Y, Imoto H, et
al: Length of stay and cost for surgical site infection after
abdominal and cardiac surgery in Japanese hospitals: Multi-center
surveillance. Surg Infect (Larchmt). 13:257–265. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Mujagic E, Marti WR, Coslovsky M, Soysal
SD, Mechera R, von Strauss M, Zeindler J, Saxer F, Mueller A, Fux
CA, et al: Associations of hospital length of stay with surgical
site infections. World J Surg. 42:3888–3896. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Oliveira WF, Silva PMS, Silva RCS, Silva
GMM, Machado G, Coelho LCBB and Correia MTS: Staphylococcus aureus
and Staphylococcus epidermidis infections on implants. J Hosp
Infect. 98:111–117. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chang CC and Merritt K: Infection at the
site of implanted materials with and without preadhered bacteria. J
Orthop Res. 12:526–531. 1994.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Henig O and Kaye KS: Bacterial pneumonia
in older adults. Infect Dis Clin North Am. 31:689–713.
2017.PubMed/NCBI View Article : Google Scholar
|