Introduction
Thyroglossal duct cysts (TGDCs) are unusual remnants
of the thyroid gland that can arise anywhere along the thyroid
migration pathway (1). This
phenomenon is the most prevalent type of congenital neck mass in
children, with a frequency of ~7% in the general population
(1). During embryonic development,
in the first six weeks of pregnancy, the thyroid gland begins to
descend toward its definitive anatomical position, and afterward,
the thyroglossal duct normally undergoes complete atrophy by the
tenth week (1). However, failure to
undergo atrophy can lead to the formation of TGDC, which can be in
the form of a cyst, fistula, duct, tract or ectopic thyroid tissue
(2). The cyst manifests as a solid,
clearly delineated, painless mass that ascends with the protrusion
of the tongue and during swallowing, connecting to the foramen
caecum through the embryonic duct (3). In the pediatric population, TGDCs have
been reported to primarily affect male individuals, while in
adults, the prevalence is notably higher among females. The area
beneath the hyoid bone emerges as the predominant site of origin
for the anomaly. Complications associated with this congenital
anomaly may include severe infection, localized inflammation, pain,
swelling, malignancy and the development of fistulas (1). According to the literature, cancer
rarely develops from TGDCs. The incidence of primary carcinoma
within TGDCs among all cases subjected to TGDC removal was
documented to vary between 0.7 and 6%. (1,4-7).
This rare but significant occurrence presents a diagnostic and
management challenge due to its rarity and our limited
understanding, as the majority of the available data are from case
reports, with some small case series (1,2,4,5,7).
The present study aims to showcase the clinical characteristics,
diagnosis and management of patients with TGDC carcinoma.
Materials and methods
Study design
This was a retrospective single-center study
conducted at the thyroid clinic of the Smart Health Tower
(Sulaimani, Iraq) from February 2016 to February 2020. It involved
the retrospective analysis of a series of cases who had undergone a
Sistrunk operation or thyroid operation (partial or total
thyroidectomy) for the removal of TGDC.
Participants
Patients with a proven histopathological examination
of thyroglossal carcinoma (TGC) were included in this study.
Patients under 18 years of age, those who presented with neck
swelling due to other causes than thyroglossal abnormalities and
those with incomplete data were excluded.
Data collection
All the required data were collected from the
center's electronic health records, including demographic data,
presentations, physical examination, pre-operative thyroid state,
neck US finding, radiation history, fine needle aspiration cytology
(FNAC) results, histopathological examination report, surgery
indication, type of operations, postoperative need for receiving
radioactive iodine, complications, size of the cyst, a
postoperative suppressive dose of thyroxine and recurrence.
Intervention
All cases underwent the Sistrunk procedure, which is
a standard surgical operation for TGDC. In addition, all cases that
had both TGDC with carcinoma and carcinoma in the thyroid gland
underwent a thyroidectomy or thyroid lobectomy for managing thyroid
cancers. All operations were conducted under general anesthesia in
a supine position with the neck extended, after skin preparation
and disinfection. A transverse incision was made in the neck over
the mass of suspected TGC or along the incision for a thyroid
operation. After opening the skin and platysma, dissection was
done, including strap muscles as much as needed to avoid rupture of
the cyst to avoid recurrence. The cyst was removed, including the
anterior horn of the hyoid bone. If there was an extra-cystic
extension of papillary carcinoma, careful dissection was undertaken
to ensure complete removal of the tumor extension. In cases of
proven thyroid cancer with positive cervical lymph nodes, total
thyroidectomy with cervical lymph node dissection was performed
after ligating the upper pole of the thyroid artery and then
exploring and preserving the recurrent laryngeal nerve. All lymph
nodes from levels II, III, IV and VI were removed. The close-vacuum
drain was inserted, and then, the strap muscle and skin were
sutured.
Histopathological procedure
After labeling, the surgical specimens were stored
in neutral buffered formalin (10%) for a duration of 10 h at 25˚C.
Subsequently, Histo-Tek® VP1-(Sakura Finetek Europe) was
used for fixation and dehydration of the tissue samples for 18-22
h. By using Histo Core Arcadia H (Leica Microsystems GmbH), the
samples were embedded in paraffin wax to form blocks. The staining
was performed using hematoxylin and eosin (H&E) for 1-3 min,
according to the manufacturer protocol (Leica Microsystems).
Results
Patient demographics and clinical
findings
A total of 10 patients were included in this study.
The clinicopathological characteristics of the cohort are presented
in Table I and individual
information of each patient is in Table II. The mean and median age of the
patients was 39.1 and 40 years, ranging from 25 to 48 years. The
majority of the cases were female (n=8, 80%). Only one (10%) case
had a family history of thyroid cancer. The subjects had no past
exposure to radiation. A total of eight cases (80%) had normal
thyroid function, one (10%) had hypothyroidism and one (10%) had
hyperthyroidism. Anterior neck swelling was the only clinical
manifestation in all cases (100%).
 | Table ISummary of demographic data and
clinical characteristics of included patients. |
Table I
Summary of demographic data and
clinical characteristics of included patients.
| Variable | Value |
|---|
| Mean and median age
(range), years | 39.1, 40 (25-48) |
| Gender | |
|
Male | 2(20) |
|
Female | 8(80) |
| Family history of
thyroid cancer | 1(10) |
| History of
radiation | 0 (0) |
| Thyroid state | |
|
Euthyroid | 8(80) |
|
Hypothyroid | 1(10) |
|
Hyperthyroid | 1(10) |
| Drug history | 2(20) |
| Presence of anterior
neck swelling | 10(100) |
| Mean, median duration
(range), months | 4.2, 2 (1-12) |
| Ultrasound
findings | |
|
Cystic
lesion | 4(40) |
|
Complex
lesion | 3(30) |
|
Cystic
lesion with microcalcification and mural nodule | 3(30) |
| FNA of suspected
cyst | |
|
Negative for
malignancy | 1(10) |
|
Suspicious
for malignancy | 6(60) |
|
N/A | 3(30) |
| Surgery indication
for cancer | 10(100) |
| Operation type | |
|
Sistrunk
operation | 5(50) |
|
Sistrunk
operation and total thyroidectomy | 4(40) |
|
Sistrunk
operation and lobectomy | 1(10) |
| Histopathological
examination | |
|
PTC in
TGDC | 5(50) |
|
PTC with PTC
in TGDC | 2(20) |
|
PTMC with
PTC in TGDC | 3(30) |
| Cyst size, cm | |
|
<1.5 | 4(40) |
|
≥1.5 | 6(60) |
| Lymphovascular
invasion | 10(100) |
| Suppressive dose of
thyroxine | 4(40) |
| Postoperative
radiation | 2(20) |
| Need for receiving
radioactive iodine | 1(10) |
| Postoperative
ultrasound follow-up | |
|
No
suspicious lesion | 10(100) |
|
Suspicious
lesion | 0 (0) |
 | Table IIDemographic data and clinical
characteristics of each patient. |
Table II
Demographic data and clinical
characteristics of each patient.
| Case no. | Age, years | Gender | Symptoms/ PEF | Radiation
history | POTS | U/S findings | Cyst size, cm | FNAC findings | Surgery
indication | Type of
operation | HPE findings | NRRI | Complications | PSDT | Recurrence |
|---|
| 1 | 35 | Female | Anterior neck
swelling | None | Hypothyroid | Infected
thyroglossal cyst | 1 | FNAC was not
conducted for TGDC FNA for thyroid and cervical LNS was positive
for PTC | Cancer | Sistrunk's
operation and total thyroidect omy + Lt lateral group II, III, IV
dissection | PTC with PTC of
TGDC | No | No | Yes | No |
| 2 | 48 | Female | Anterior neck
swelling | None | Euthyroid | Complex cyst | 1.3 | Content of
cyst | Cancer | Sistrunk's
operation + Lt lobectomy | PTC of TGDC +
hyperplastic nodule | No | No | No | No |
| 3 | 36 | Female | Anterior neck
swelling | None | Euthyroid | Cystic lesion with
microcalcification with a mural nodule | 1.7 | Not conducted | Cancer | Sistrunk's
operation | PTC of TGDC | No | No | No | No |
| 4 | 38 | Female | Anterior neck
swelling | None | Hyperthyroid | Cystic lesion with
microcalcification with a mural nodule | 1.5 | Suspicion of PTC +
PTC for bilateral thyroid nodules | Cancer | Total thyroidect
omy with Lt central and lateral neck dissection + Sistrunk's
operation | PTMC with PTC of
TGDC | Yes | No | Yes | No |
| 5 | 43 | Female | Anterior neck
swelling | None | Euthyroid | Cystic lesion with
solid mural nodule containing calcification | 1.3 | Suspicion of
PTC | Cancer | Sistrunk's
operation | PTC of TGDC | No | No | No | No |
| 6 | 48 | Female | Anterior neck
swelling | None | Euthyroid | Cystic lesion | 1.3 | Suspicion of
PTC | Cancer | Sistrunk's
operation | PTMC with PTC of
TGDC | No | No | No | No |
| 7 | 25 | Female | Anterior neck
swelling | None | Euthyroid | Complex cyst | 2 | Suspicion of
PTC | Cancer | Sistrunk's
operation | PTC of TGDC | No | No | No | No |
| 8 | 42 | Female | Anterior neck
swelling | None | Euthyroid | Cystic lesion | 1.5 | Suspicion of
PTC | Cancer | Sistrunk's
operation | PTC of TGDC | No | No | No | No |
| 9 | 43 | Male | Anterior neck
swelling | None | Euthyroid | Complex nodule | 1.5 | Right thyroid
nodule was suspicious for PTC FNAC was not conducted for TGDC | Cancer | Total thyroidect
omy and Sistrunk's operation | PTC with PTC of
TGDC | No | No | Yes | No |
| 10 | 33 | Male | Anterior neck
swelling | None | Euthyroid | Cystic lesion | 1.9 | Suspicion of
PTC | Cancer | Total thyroidect
omy and Sistrunk's operation | PTMC with PTC of
TGDC | No | No | Yes | No |
Diagnostic findings and
management
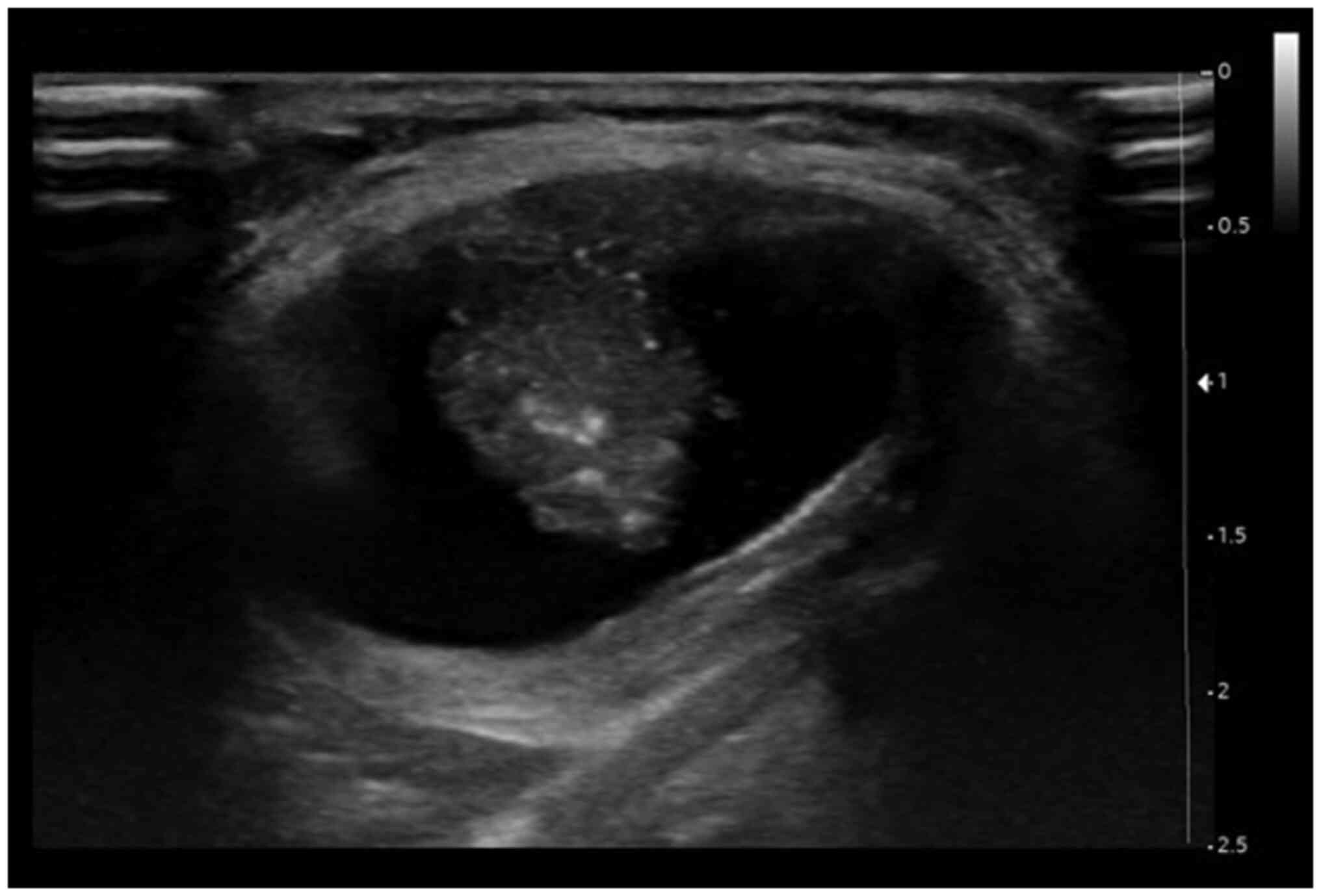
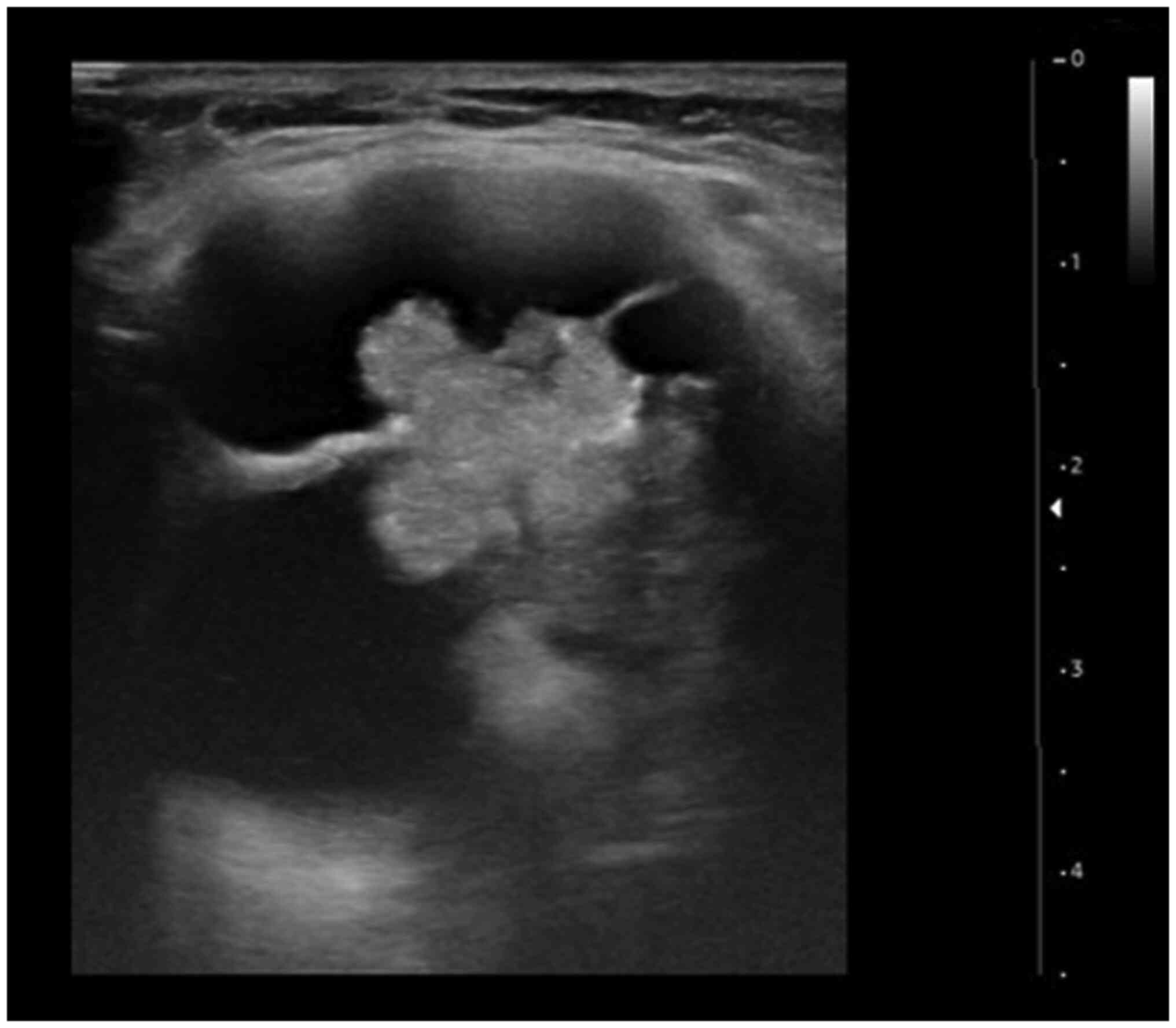
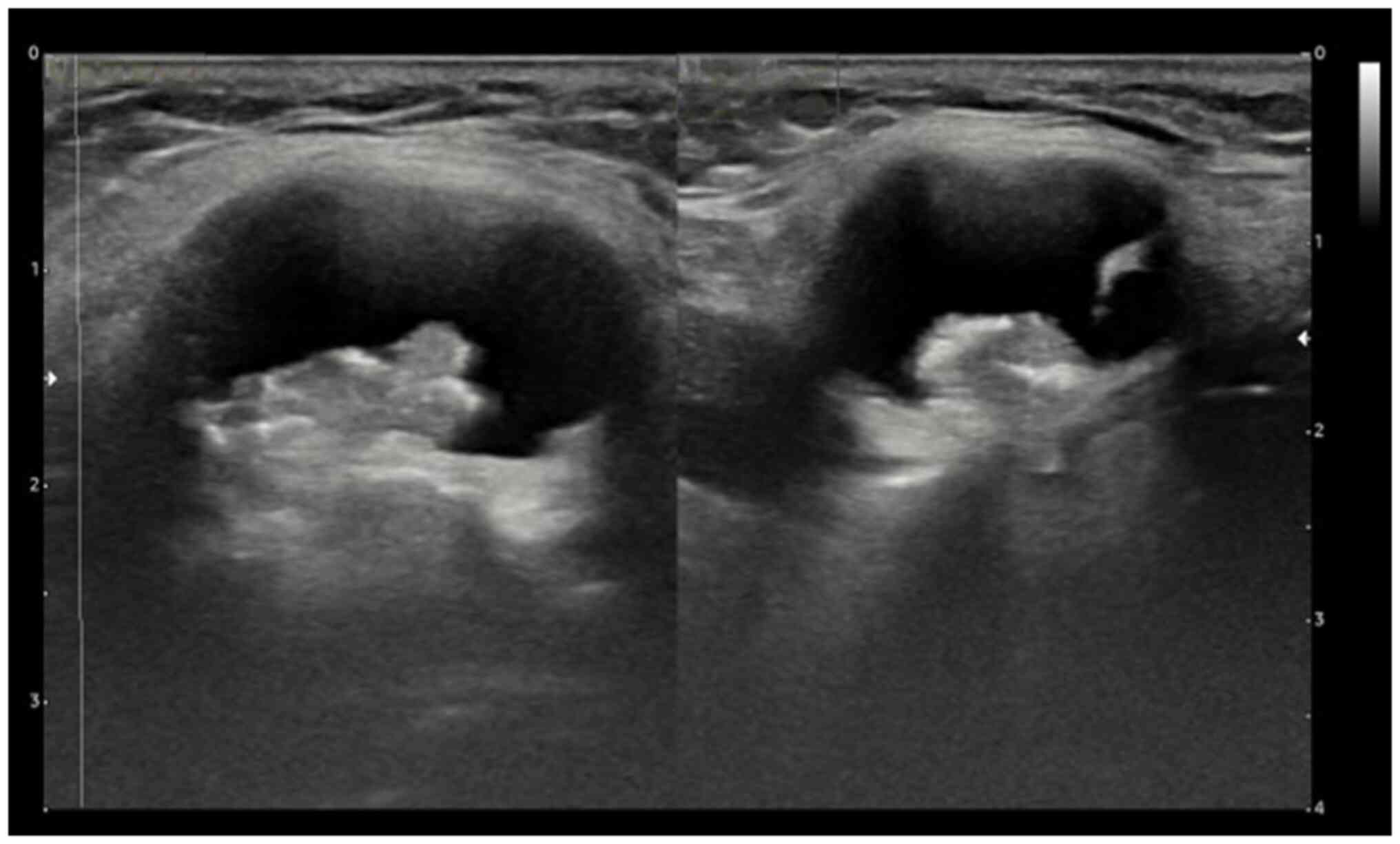
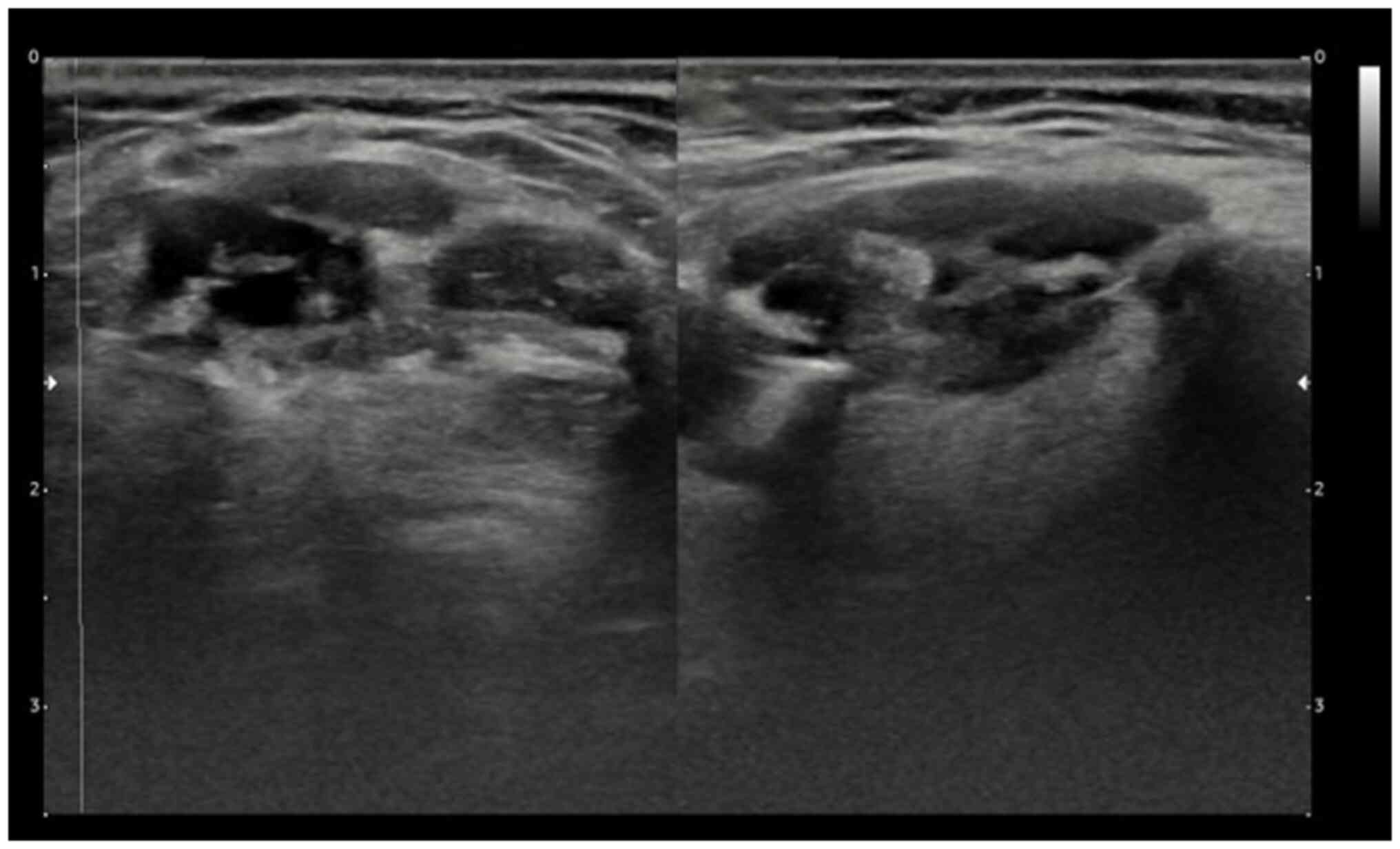
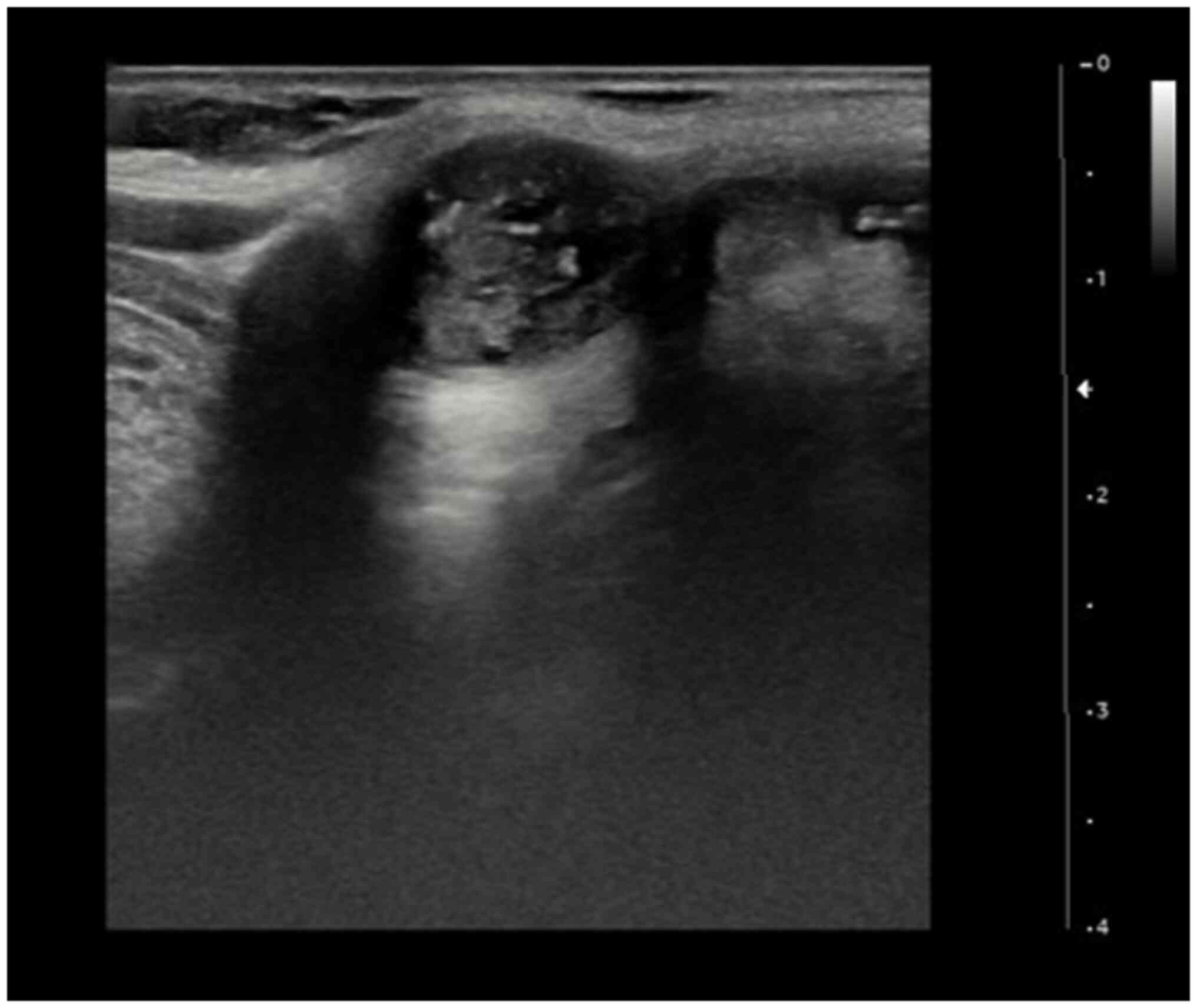
US studies revealed cystic lesions in four (40%)
cases, complex nodules in three cases (30%) and mural nodules with
cystic lesions in three cases (30%) (Fig. 1, Fig.
2, Fig. 3, Fig. 4 and Fig.
5). FNAC of suspected nodules was positive for malignancy in
six (60%) cases and negative in one (10%). Half (50%) of the cases
underwent the Sistrunk operation alone; four (40%) cases underwent
the Sistrunk operation plus total thyroidectomy; and one (10%) case
underwent the Sistrunk operation plus lobectomy. Lymph node
metastasis was only found in 2 (20%) cases. Nodes were positive
only in the lateral neck compartments in one (10%) of the cases
without central region metastasis. However, nodes were positive in
the lateral and central neck compartments in one (10%) patient.
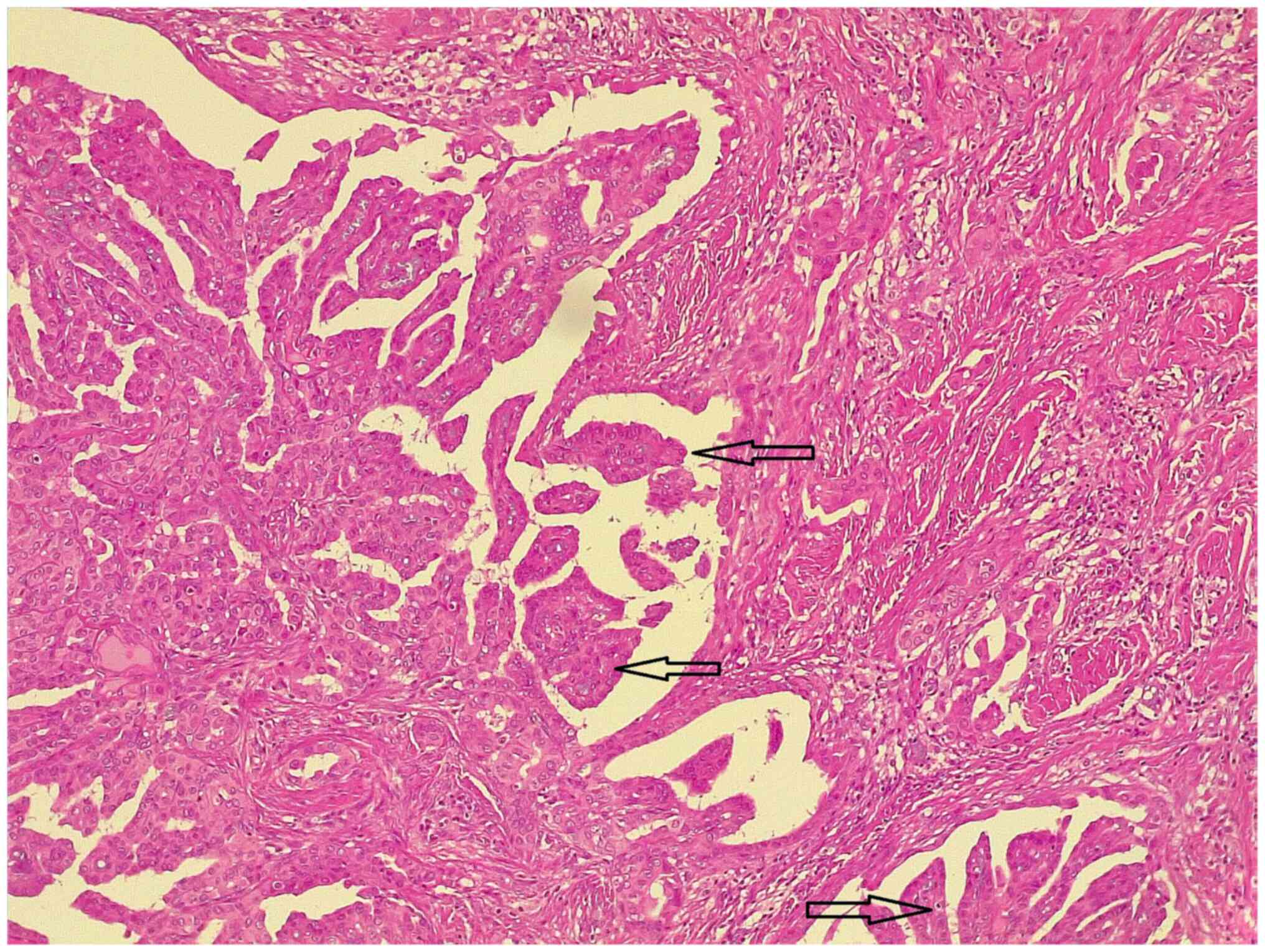
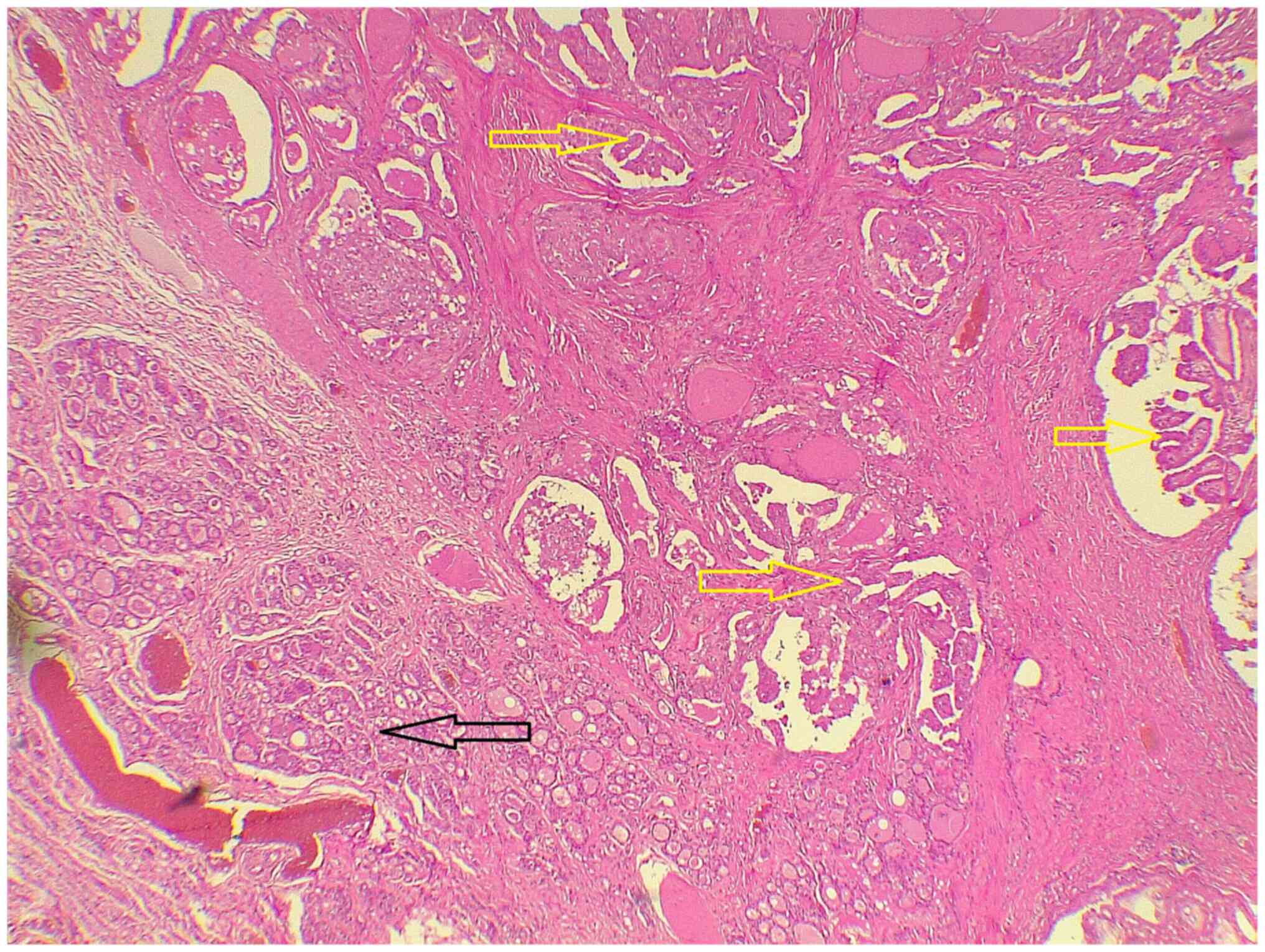
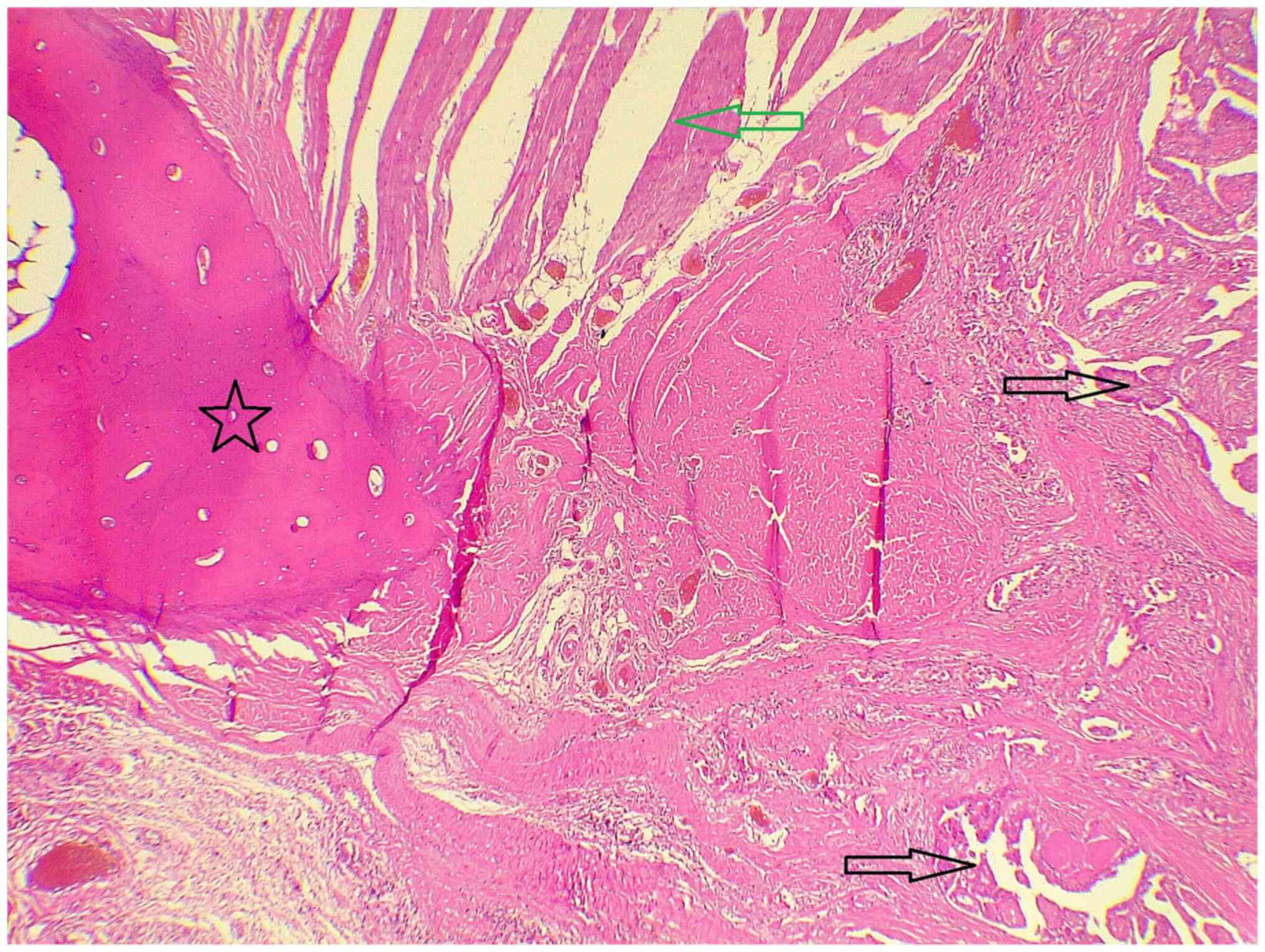
Histopathological examination confirmed papillary thyroid carcinoma
(PTC) in TGDC in all the cases (100%) (Fig. 6). In addition, in the thyroid
tissue, 2 cases (20%) also had PTC and 3 cases (30%) had papillary
thyroid microcarcinoma (Figs. 7 and
8).
Postoperative treatment and follow
up
Overall, one patient (10%) was given radioactive
iodine as well as a suppressive dosage of thyroxine and three (30%)
were only given suppressive thyroxine. The patients were followed
up every three months and a three-year follow-up with US revealed
no suspicious lesions in any of the cases. Patients with total
thyroidectomy still receive treatment (thyroxine).
Discussion
TGDC is one of the most common congenital anomalies,
with a wide range of differential diagnoses, that is rarely
associated with carcinoma (1,8,9).
Although it is uncertain how cancer arises at this location, it is
thought to be the result of the neoplastic transformation of normal
residual thyroid tissue throughout the thyroglossal cystic tube.
The papillary histotype of the condition has two possible origins:
Ectopic thyroid tissue formation or metastases from a primary
thyroid malignancy, with the latter receiving less attention
(4).
TGDC is typically seen in children, yet adults can
also be affected. However, it is challenging to pinpoint an exact
age distribution for TGDC due to the varied reporting time frames,
which may be reported as the age at which the condition was first
diagnosed when symptoms began, or some authors may reference the
patient's life decade rather than their precise age. Consequently,
there is no agreement in the literature concerning the age
demographics of patients with TGDC. In previous studies, the age
distribution of malignant TGDCs has been reported to be 41-47 years
(4,10). In the current study, the mean and
median age of the patients were 39.1 and 40 years,
respectively.
The usual presentation of TGDC is a moveable,
painless midline or, less commonly, a lateral neck mass (11), while malignant TGDC should be
suspected in any cysts that are irregular, hard, rapidly increasing
in size, fixed to surrounding tissues or present in cervical lymph
nodes (12,13). Most of the time, it is impossible to
clinically differentiate between a TGC and a benign TGDC. Usually,
the diagnosis is made by histopathological examination after
excision of the resected tissue (14,15). A
study by Kennedy et al (16)
showed only three cases of PTC and a single case of squamous cell
carcinoma (SCC) in a large review of 115 cases of TGDC, whose
presentations were the same as that of benign TGDC. Khalaf et
al (17) reported a case of a
44-year-old female with coexisting hyperthyroidism and TGDC. In the
current study, all of the cases had anterior neck swelling for a
mean and median of 4.2 and 2 months, respectively. Only one case
had hypothyroidism, one had hyperthyroidism and the others were
euthyroid.
Imaging diagnostic tools for neck masses include US,
scintigraphy and computerized tomography (CT), which are less
likely to diagnose malignant diseases preoperatively (18,19).
The US of TGDC frequently shows a well-defined cystic area with
anechoic fluid. Their walls are thin without internal vascularity.
On the other hand, the presence of microcalcification and a solid
component within the cyst can predict malignancy (7). Branstetter et al (20) reported that carcinoma should be
suspected in TGDC when a mural nodule or calcification is seen on
CT. Acultae et al (7)
reported a case of a 21-year-old female diagnosed with TGC in whom
the neck US revealed a predominantly cystic lesion with a central
solid component lying between the hyoid bone and thyroid cartilage.
In this study, the US revealed a cystic lesion in four cases (50%),
a complex nodule in three cases (30%), a cystic lesion with
microcalcification and a mural nodule in three cases (30%) (cases
3, 4 and 5).
The role of FNAC in detecting TGC has been well
investigated (21). In particular,
US-guided FNAC is the main diagnostic investigation of TGC, with a
positive accuracy rate of 53% and a false negative rate of 47%.
Peripheral locations of swelling in some of the patients, low
cellularity of aspirated cytology due to dilution of the cystic
region after aspiration and small tumor size make TGC diagnosis by
FNAC challenging (6,21). Repeating the FNAC under US guidance
and taking a sample from the solid part of the cystic area or soft
tissue mass may improve diagnostic accuracy (13). In the current study, only seven of
the cases had a preoperative FNAC of TGDC. Of the cases, six were
suspected to have PTC and there was just cystic content in the
sample of one of the cases.
The first case of PTC in a TGDC was reported by Owen
and coworkers in 1927(5). The
majority of these malignancies come from the thyroid gland, with
75-85% being PTC, 7% being mixed papillary and follicular carcinoma
and ~5% being SCC, which has the poorest prognosis (7). In a previous study, 4% of TGDC cases
were found to be carcinomas and all of these were PTC (1). This aligns with prior research that
also identified PTC as the most common type of carcinoma associated
with TGDC (22). All of the TGCs in
this study were PTC.
A common treatment for TGDC is Sistrunk's operation,
which consists of the surgical removal of the TGDC and the hyoid
bone central segment, along with a portion of tissue surrounding
the thyroglossal tract extending towards the oral cavity at the
foramen cecum (12). More
aggressive management, such as the Sistrunk operation combined with
a complete thyroidectomy and neck dissection, followed by treatment
with radioactive iodine and thyroxine suppressive dose is
beneficial for high-risk patients (older than 45 years, presence of
invasion or metastatic lymph nodes in the neck, history of head and
neck radiation and patients who present with a malignant thyroid
nodule) (13). On the other hand,
some authors recommend having a total thyroidectomy when the size
of the carcinoma is >10 mm. When the size is <10 mm, a total
thyroidectomy should be considered when there is a presence of cyst
wall invasion, enlarged cervical lymph nodes clinically or
radiologically, or a prior history of radiation (7). Furthermore, total thyroidectomy
combined with Sistrunk's procedure for TGC allows for more accurate
staging and therapy, as well as long-term follow-up with
thyroglobulin level monitoring and a whole-body scan (13). Sistrunk surgery was performed on
five patients in this study alone. A total of four of the
individuals had malignant thyroid nodules, necessitating both a
Sistrunk surgery and a total thyroidectomy. Due to abnormal lymph
nodes in the neck, two of them underwent lateral neck dissection.
Furthermore, one patient was given radioactive iodine as well as a
suppressive dosage of thyroxine. The cited resources in this study
have been checked for eligibility (23). The limitations of this study include
the availability of only a small number of histopathological
images. As some examinations were conducted in external
histopathology centers, not all images could be retrieved and the
mutation profiles of the patients could not be obtained due to the
high cost of the examinations.
In conclusion, carcinomas arising from TGDC remnants
are uncommon and may solely present as anterior neck swelling. The
use of FNAC in the preoperative assessment of cystic lesions in the
neck can be beneficial. If TGC is suspected, both the thyroid gland
and different lymph node compartments should be evaluated for
malignancy. The Sistrunk operation serves as the gold treatment
approach with good outcomes. However, additional management for
high-risk TGCs should be considered, such as total or partial
thyroidectomy, ablation using radioactive iodine, lateral neck
dissection and suppressive therapy with thyroid hormones.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YAS, ASM and HMD: Data collection, follow-up of the
patients and final approval of the manuscript. AMS: Supervision of
the manuscript, major contribution to the conception of the study,
as well as in the literature search for related studies. AJQ:
Radiologist who assessed the subjects' thyroid. AMA: Pathologist
who examined the specimens. SHH and FHK: Confirmation of the
authenticity of all the raw data, critical revision of the
manuscript and contribution to the conception of the study. BOH,
BAA and MBAA: Literature review, final approval of the manuscript
and processing of the tables. SFA and HMR: Involved in the
literature review, the writing of the manuscript and data analysis
and interpretation. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Ethical approval for the study was granted by the
Ethics Committee of Sulaimani University (Sulaimani, Iraq; approval
no. 090). Written informed consent was obtained from all individual
participants included in the study.
Patient consent for publication
The patients provided written informed consent for
the publication of any data and/or accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Muhialdeen AS, Salih AM, Ahmed MM, Saeed
YA, Qaradakhy AJ, Baba HO, Abdullah AM, Kakamad FH, Mohammed SH,
Hiwa DS, et al: Thyroglossal duct diseases: Presentation and
outcomes. J Int Med Res. 51(3000605231154392)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Balalaa N, Megahed M, Al Ashari MA and
Branicki F: Thyroglossal duct cyst papillary carcinoma. Case Rep
Oncol. 4:39–43. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zaman SU, Ikram M, Awan MS and Hassan NH:
A decade of experience of management of thyroglossal duct cyst in a
tertiary care hospital: Differentiation between children and
adults. Indian J Otolaryngol Head Neck Surg. 69:97–101.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rossi ED, Martini M, Straccia P, Cocomazzi
A, Pennacchia I, Revelli L, Rossi A, Lombardi CP, Larocca LM and
Fadda G: Thyroglossal duct cyst cancer most likely arises from a
thyroid gland remnant. Virchows Archiv. 465:67–72. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pribitkin EA and Friedman O: Papillary
carcinoma in a thyroglossal duct remnant. Arch Otolaryngol Head
Neck Surg. 128:461–462; discussion 463-4. 2002.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mahmood ZH, Mohemed FM, Fatih BN, Qadir AA
and Abdalla SH: Cancer publications in one year; a cross-sectional
study. Barw Med J. 1:2023.
|
|
7
|
Aculate NR, Jones HB, Bansal A and Ho MW:
Papillary carcinoma within a thyroglossal duct cyst: Significance
of a central solid component on ultrasound imaging. Br J Oral
Maxillofac Surg. 52:277–278. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mondin V, Ferlito A, Muzzi E, Silver CE,
Fagan JJ, Devaney KO and Rinaldo A: Thyroglossal duct cyst:
Personal experience and literature review. Auris Nasus Larynx.
35:11–25. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Agarwal K, Puri V and Singh S: Critical
appraisal of FNAC in the diagnosis of primary papillary carcinoma
arising in thyroglossal cyst: A case report with review of the
literature on FNAC and its diagnostic pitfalls. J Cytol. 27:22–25.
2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pellegriti G, Lumera G, Malandrino P,
Latina A, Masucci R, Scollo C, Spadaro A, Sapuppo G, Regalbuto C,
Pezzino V and Vigneri R: Thyroid cancer in thyroglossal duct cysts
requires a specific approach due to its unpredictable extension. J
Clin Endocrinol Metab. 98:458–465. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chen KT: Cytology of thyroglossal cyst
papillary carcinoma. Diagn Cytopathol. 9:318–321. 1993.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Albayrak Y, Albayrak F, Kaya Z, Kabalar E
and Aylu B: A case of papillary carcinoma in a thyroglossal cyst
without a carcinoma in the thyroid gland. Diagn Cytopathol.
39:38–41. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Cherian MP, Nair B, Thomas S, Somanathan T
and Sebastian P: Synchronous papillary carcinoma in thyroglossal
duct cyst and thyroid gland: Case report and review of literature.
Head Neck. 31:1387–1391. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Heshmati HM, Fatourechi V, Van Heerden JA,
Hay ID and Goellner JR: Thyroglossal duct carcinoma: Report of 12
cases. Mayo Clin Proc. 72:315–319. 1997.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Motamed M and McGlashan JA: Thyroglossal
duct carcinoma. Curr Opin Otolaryngol Head Neck Surg. 12:106–109.
2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kennedy TL, Whitaker M and Wadih G:
Thyroglossal duct carcinoma: A rational approach to management.
Laryngoscope. 108 (8 Pt 1):1154–1158. 1998.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Khalaf S, Sarwani A, Al Fardan R, Maki M
and Al Saeed M: A uniquely challenging case of poorly controlled
hyperthyroidism with a coexisting thyroglossal cyst. Cureus.
13(e14271)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Martin-Perez E, Larranaga E, Marrón C and
Monje F: Primary papillary carcinoma arising in a thyroglossal duct
cyst. Eur J Surg. 163:143–145. 1997.PubMed/NCBI
|
|
19
|
Muhialdeen AS, Baba HO, Salih AM, Saeed
YA, Abdullah IY, Qaradakhy AJ, Salih KM, Tahir SH, Kakamad FH,
Abdullah HO, et al: Redo thyroidectomy: A modified technique to
eliminate complications. Barw Med J. 1:2023.
|
|
20
|
Branstetter BF, Weissman JL, Kennedy TL
and Whitaker M: The CT appearance of thyroglossal duct carcinoma.
AJNR Am J Neuroradiol. 21:1547–1550. 2000.PubMed/NCBI
|
|
21
|
Bardales RH, Suhrland MJ, Korourian S,
Schaefer RF, Hanna EY and Stanley MW: Cytologic findings in
thyroglossal duct carcinoma. Am J Clin Pathol. 106:615–619.
1996.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chrisoulidou A, Iliadou P, Doumala E,
Mathiopoulou L, Boudina M, Alevizaki M, Patakiouta F, Xinou E and
Pazaitou-Panayiotou K: Thyroglossal duct cyst carcinomas: Is there
a need for thyroidectomy? Hormones (Athens). 12:522–528.
2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Muhialdeen AS, Ahmed JO, Baba HO, Abdullah
IY, Hassan HA, Najar KA, Mikael TM, Mustafa MQ, Mohammed DA, Omer
DA, et al: Kscien's List; A New Strategy to Discourage Predatory
Journals and Publishers (Second Version). Barw Med J. 1:1–3.
2023.
|