Introduction
Rotator cuff injury (RCI) encompasses various
shoulder disorders affecting the rotator cuff, including tears,
tendinitis and impingement syndrome (1). Patients with RCI commonly report
shoulder pain during specific movements and experience functional
limitations (2,3), leading to sleep disturbance, stress
and disruptions to daily and professional activities (4-6).
Therefore, effective treatment is crucial to alleviate discomfort
and enhance the quality of life of patients with RCI.
Treatment options for RCI include surgery (2), exercise, manual therapy (MT),
physiotherapy, nonsteroidal anti-inflammatory drugs,
intra-articular glucocorticoid injections and therapy using
biomaterials (7-13).
Surgery can restore the anatomy of rotator cuff well, but there is
still a certain rate of retear (7).
Non-steroidal anti-inflammatory drugs and intra-articular
glucocorticoid injection can relieve pain in a short period of
time, but the improvement of function is limited (7,8).
Although biomaterials have made great progress in promoting the
repair of RCI (9-13),
they have not been widely used in clinical practice. MT is widely
used as a non-pharmacological intervention by physiotherapists,
chiropractors and osteopaths. MT involves the manipulation of
joints and surrounding tissues by healthcare professionals. In the
clinical setting, MT is administered either alone or in conjunction
with exercise therapy or multimodal physiotherapy.
While previous systematic reviews and meta-analyses
have assessed the efficacy of MT for RCI (14-16),
these analyses often conducted qualitative syntheses of outcomes
such as functional scores without pooling results into
meta-analyses. Additionally, the effectiveness of MT in isolation,
as well as its supplementary benefits when combined with exercise
or physiotherapy, remain unclarified.
Previous randomized controlled trials (RCTs) have
suggested that MT, alone or in combination with exercise or
multimodal physiotherapy, yields positive outcomes for RCI
(17-25).
To provide a comprehensive overview, an updated systematic review
and meta-analysis was conducted to evaluate the effectiveness of
MT, either alone or as part of a multimodal intervention, on pain
and function in patients with RCI.
Materials and methods
Data sources/searches
The registration number of the present systematic
review in PROSPERO database is CRD42021246202 (https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=246202).
The present study followed the guidelines of the Preferred
Reporting Items for Systematic Review and Meta-Analyses statement
(26). The following electronic
databases were searched from their date of inception to March 28,
2023: PubMed (https://pubmed.ncbi.nlm.nih.gov), Cochrane Central
Register of Controlled Trials (https://www.cochranelibrary.com), Embase (https://www.embase.com/), Web of Science (https://www.webofscience.com), Physiotherapy Evidence
Database (PEDro) (https://pedro.org.au), Chinese National Knowledge
Infrastructure (https://www.cnki.net), Wan-fang Data
(https://www.wanfangdata.com.cn/),
Chinese Scientific Journal Database (http://qikan.cqvip.com/index.html) and Chinese
Biomedical Literature database (http://www.sinomed.ac.cn/index.jsp). A combination of
MESH terms and text words was used to identify relevant articles.
These search terms were translated into Chinese for use in
searching the aforementioned Chinese databases. Additionally, the
reference lists of identified studies were screened to ensure that
no relevant studies were overlooked. The complete PubMed search
strategy is presented in Table
SI.
Study selection
Inclusion criteria. Two investigators
independently screened the studies by reading the titles, abstracts
and complete texts. The inclusion criteria were: i) participants
aged ≥18 years diagnosed with RCI, including rotator cuff
tendinopathy/tendinitis, shoulder impingement syndrome, or
subacromial bursitis, regardless of sex; ii) interventions
comparing MT vs. placebo, MT plus exercise vs. exercise alone, or
MT plus multimodal physiotherapy vs. multimodal physiotherapy
alone; iii) outcomes broadly categorized into pain and shoulder
function scores, with no restrictions; iv) RCT design and v)
publication in English or Chinese.
Exclusion criteria
The exclusion criteria were: i) inability to locate
a summary or full text; ii) studies from which data could not be
accurately extracted; and iii) inconsistent outcome indicators. For
republished studies, the most comprehensive reported data with the
longest follow-up were selected.
Data extraction
The following data were independently extracted by
two reviewers: first author, publication year, study
characteristics (sample size, age, interventions, and intervention
dosage and frequency), quality assessment details (randomization,
allocation concealment, blinding, and outcome reporting), and study
results. Data were cross-checked by two reviewers; in cases of
disagreement, a third reviewer participated in discussions until a
consensus was reached.
Outcome definitions
Outcome measures included shoulder pain and
functional scores. Pain was assessed using the visual analogue
scale, numeric pain rating scale, and pain component of composite
scales. Functional scores comprised the Disability of the Arm,
Shoulder and Hand Score, Shoulder Pain and Disability Index,
Constant-Murley Score and Pennsylvania Shoulder Score. Due to
limited long-term follow-up after the end of treatment in most
studies, only data obtained at the end of treatment were included
in the meta-analysis. A descriptive analysis was performed for
studies with long-term follow-up (the follow-up period was >1
year).
Quality assessments
The risk of bias in included trials was assessed
using items 2-11 of the PEDro scale, which gives a total score of
10(27) (Table I). The PEDro scale has favorable
reliability and validity (28-30)
and is commonly used in systematic reviews of physiotherapy
efficacy (31-33).
Trials scoring ≥6 out of 10 were considered to have a low risk of
bias (34,35). The risk of bias was independently
evaluated by two reviewers.
 | Table IPhysiotherapy evidence database
scale. |
Table I
Physiotherapy evidence database
scale.
| Item | Criteria |
|---|
| 1 | Eligibility
criteria were specified |
| 2 | Subjects were
randomly allocated to groups |
| 3 | Allocation was
concealed |
| 4 | Group were similar
at baseline for the most important prognostic indicators |
| 5 | All participants
were blinded |
| 6 | All participants
who administered therapy were blinded |
| 7 | All assessors who
measured at least one key outcome were blinded |
| 8 | Measures of at
least one key outcome measures were obtained from more than 85% of
the participants initially allocated to groups |
| 9 | All participants
for whom outcome measures were available received the treatment or
control condition as allocated, or, where this was not the case,
data for a least one key outcome was analyzed by intention to
treat |
| 10 | The results of
between group statistical analysis are reported for at least one
key outcome |
| 11 | The study provides
both point measures and measures of variability for at least one
key outcome. |
Statistical analysis
Meta-analysis was conducted by calculating effect
sizes and 95% confidence intervals in Review Manager 5.4 (Cochrane
Collaboration; https://www.cochrane.org/). Results were organized
based on outcome measures and intervention types. Numerical
variables were analyzed using the mean difference (MD) or
standardized MD (SMD). Pre- to post-treatment changes in pain and
functional scores were pooled. In studies with crossover designs,
outcome measures were analyzed at the first intervention exchange.
Subgroup analysis was performed based on intervention dosage or
frequency discrepancies.
Statistical heterogeneity was assessed using the
I2 statistic and the chi-squared test. If
I2≤50% and P≤0.05, the heterogeneity between studies was
considered acceptable (36). If
there was significant heterogeneity (I2>50% and
P<0.05) (37), the source of
heterogeneity was explored by one-by-one exclusion sensitivity
analysis. Because the included studies were from different study
populations, a random effects model was used in all meta-analyses.
P<0.05 was considered to indicate a statistically significant
difference.
Results
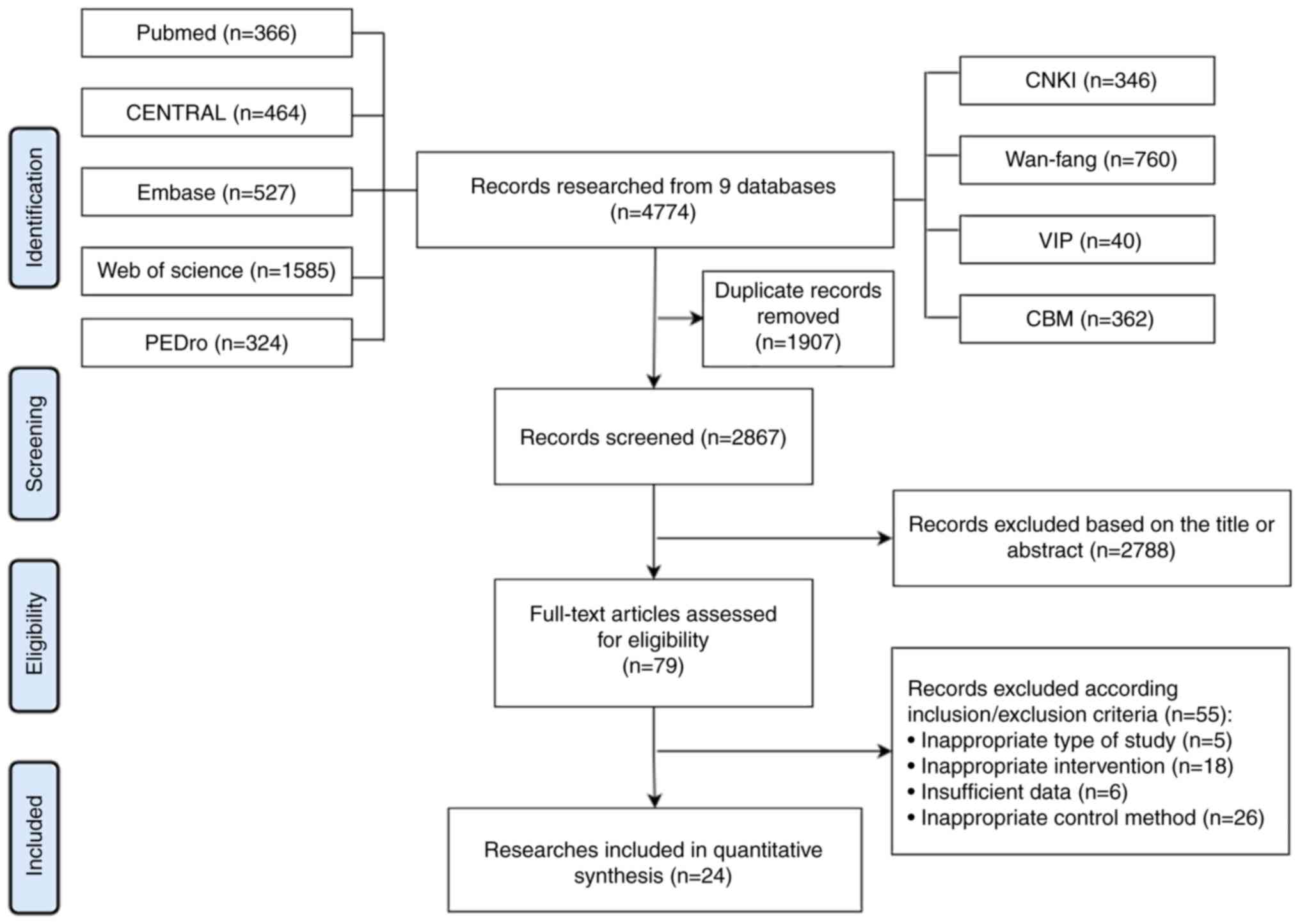
A total of 4,774 articles were retrieved from the
online databases. Among these, 1,907 articles were excluded due to
duplication, while another 2,788 articles were excluded after
independent screening of titles and abstracts by two reviewers. A
total of 24 studies (38-52)
met the inclusion criteria and were included in the quantitative
synthesis after full-text review. No republished studies were
reviewed. A detailed depiction of the literature screening process
is provided (Fig. 1).
Basic characteristics of included
studies
The characteristics of the included trials are
summarized in Table II. A total of
24 eligible RCTs evaluated the efficacy of MT for RCI, involving
1,110 participants (546 in the experimental group, 564 in the
control group). All studies included adults >18 years of age,
and only one study (24) restricted
the age range to young adults between 18-35 years of age. Among
these RCTs, 10 compared MT with placebo, 11 evaluated the
additional efficacy of MT added to exercise therapy vs. exercise
alone, and three assessed the additional benefit of MT combined
with multimodal physiotherapy vs. multimodal physiotherapy
alone.
 | Table IICharacteristics of the included
studies. |
Table II
Characteristics of the included
studies.
| Manual therapy vs.
placebo |
|---|
| Author, year | Diagnosis | Sample size
(Exp/Ctr) | Age (Exp/Ctr) | Intervention
(Exp/Ctr) | Frequency | Treatment
duration | Follow-up
period | Outcome | (Refs.) |
|---|
| Atkinson et
al, 2008 | Rotator cuff
tendinopathy | 30/30 | 41.53 (18-63)/42
(20-76) | MT/Placebo | 6 sessions in 2
weeks | 2 weeks | 2 weeks | ② | (38) |
| Aytar et al,
2015 | Subacromial
impingement syndrome | 22/22 | 52±3/52±4 | MT/Placebo | 9 sessions in 3
weeks | 3 weeks | 11 weeks | ①④ | (39) |
| Silva et al,
2019 | Rotator cuff | 30/30 |
46.06±16.11/44.46±12.14 | MT/Placebo | Only once | / | / | ① | (25) |
| Delgado-Gil et
al, 2015 | Shoulder
impingement syndrome | 21/21 |
55.4±7.8/54.3±10 | MT/Placebo | 2 sessions per
week | 2 weeks | 2 weeks | ① | (40) |
| Guimarães et
al, 2016 | Shoulder
impingement syndrome | 14/13 |
30.3±6.9/31.9±9.2 | MT/Placebo | 4 treatments (48 h
apart) | 8 days | 8 days | ②⑤ | (41) |
| Haik et al,
2017 | Shoulder
impingement syndrome | 30/31 |
32.5±12.0/31.3±11.0 | MT/Placebo | twice in a period
of 3-4 days apart | 3-4 days | 1 week | ②④ | (42) |
| Hunter et
al, 2022 | Shoulder
impingement syndrome | 25/25 |
62.0±9.6/61.4±11.3 | MT/Placebo | once a week | 4 weeks | 12 months | ①④ | (20) |
| Kardouni et
al, 2015 | Subacromial
impingement syndrome | 24/21 |
31.1±12.3/31.2±12.1 | MT/Placebo | Only once | / | / | ②⑥ | (43) |
| McClatchie et
al, 2009 | Painful arc | 7/14 | 49.8±9.8 | MT/Placebo | Only once | / | / | ① | (44) |
| Surenkok et
al, 2009 | Rotator cuff
tendinitis or tenosynovitis | 13/13 |
55.07±13.36/54.30±12.70 | MT/Placebo | Only once | / | / | ①⑦ | (45) |
| Manual therapy plus
exercise vs. exercise alone |
| Akbaba et
al, 2019 | Rotator cuff
pathology | 20/21 |
50±11.23/54.1±9.34 | MT+Ex/Ex | MT: twice a week;
Ex: twice a day | 6 weeks | 6 weeks | ①④ | (17) |
| Bang and Deyle,
2000 | Shoulder
impingement syndrome | 27/23 | 42±10.1/45±8.4 | MT+Ex/Ex | Twice a week | 3 weeks | 3 weeks | ① | (46) |
| Camargo et
al, 2015 | Shoulder
Impingement | 23/23 |
35.96±12.08/32.65±10.73 | MT+Ex/Ex | Unclear | 4 weeks | 4 weeks | ①④ | (47) |
| Eliason et
al, 2021 | Subacromial pain
syndrome | 29/52 |
43.2±9.8/45.5±8.3 | MT+Ex/Ex | MT: 1-2 times a
week; Ex: twice a week | 6 weeks | 6 months | ①⑦ | (18) |
| Haider et
al, 2018 | Subacromial
pain | 20/20 |
49.3±9.99/49.8±9.67 | MT+Ex/Ex | 3 sessions per
week | 2 weeks | 2 weeks | ②⑤ | (19) |
| Kachingwe et
al, 2008 | Shoulder
impingement | 9/8 |
48.9±13.7/47.3±20.1 | MT+Ex/Ex | MT: once per week;
Ex: once per day | 6 weeks | 6 weeks | ①⑤ | (48) |
| Kromer et
al, 2014 | Shoulder
impingement syndrome | 46/44 |
50.1±12.2/53.7±9.9 | MT+Ex/Ex | MT: 10 sessions in
5 weeks; Ex: 10 sessions in 5 weeks | 5 weeks | 12 weeks | ①⑤ | (49) |
| Park et al,
2020 | Subacromial
impingement syndrome | 10/10 |
49.2±9.48/50.9±9.1 | MT+Ex/Ex | 3 sessions per
week\ | 4 weeks | 4 weeks | ⑤ | (23) |
| Sharma et
al, 2021 | Shoulder
impingement syndrome | 40/40 |
21.3±2.1/21.8±2.8 | MT+Ex/Ex | MT:12 sessions over
8 weeks; Ex: twice per day | 8 weeks | 8 weeks | ⑤ | (24) |
| Senbursa et
al, 2007 | Shoulder
impingement syndrome | 15/15 |
48.1±7.5/49.5±7.9 | MT+Ex/Ex | MT: 3 times per
week; Ex: 7 times per week | 4 weeks | 4 weeks | ① | (50) |
| Vinuesa-Montoya
et al, 2017 | Shoulder
impingement | 21/19 |
46.85±8.02/51.21±5.29 | MT+Ex/Ex | MT: twice per week;
Ex: twice a day | 5 weeks | 5 weeks | ①④ | (51) |
| Manual therapy plus
multimodal physiotherapy vs. multimodal physiotherapy |
| Author, year | Diagnosis | Sample size
(Exp/Ctr) | Age (Exp/Ctr) | Intervention
(Exp/Ctr) | Frequency | Treatment
duration | Follow-up
period | Outcome | (Refs.) |
| Barra López et
al, 2013 | Subacromial
impingement syndrome | 40/40 |
56.2±12/59.1±11.5 | MT + MP/MP | MT: 2 sessions per
week;MP: 5 sessions per week | 3 weeks | 3 months | ①⑦ | (52) |
| İğrek and Çolak,
2021 | Subacromial
impingement syndrome | 15/14 |
44.4±11/45.9±9.7 | MT + MP/MP | 5 times per
week | 4 weeks | 16 weeks | ①④ | (21) |
| Menek et al,
2019 | Roator cuff
syndrome | 15/15 |
51.73±6.64/50.26±4.28 | MT + MP/MP | 5 times per
week | 6 weeks | 6 weeks | ①④ | (22) |
Risk of bias assessment
The average PEDro scale score across the 24 RCTs was
6.45 (Table III). A total of 19
trials scored ≥6 on the PEDro scale, indicating a low risk of bias.
Among the five studies scoring <6, the limitations primarily
involved inadequate concealment of allocation, insufficient
blinding of participants and therapists, and failure to adhere to
intention-to-treat principles.
 | Table IIIRisk of bias assessment using the
physiotherapy evidence database scale. |
Table III
Risk of bias assessment using the
physiotherapy evidence database scale.
| |
PEDro
scale |
|---|
| Trial | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|
| Atkinson et
al (38), 2008 | √ | √ | √ | √ | - | - | - | √ | - | √ | √ | 6 |
| Aytar et al
(39), 2015 | √ | √ | - | √ | √ | - | √ | √ | - | √ | √ | 7 |
| Silva et al
(25), 2019 | √ | √ | √ | √ | - | - | - | √ | √ | √ | √ | 7 |
| Delgado-Gil et
al (40), 2015 | √ | √ | √ | √ | √ | - | √ | - | √ | √ | √ | 8 |
| Guimarães et
al (41), 2016 | √ | √ | - | √ | - | - | √ | √ | √ | √ | √ | 7 |
| Haik et al
(42), 2017 | √ | √ | - | √ | √ | - | √ | √ | √ | √ | √ | 8 |
| Hunter et al
(20), 2022 | √ | √ | √ | √ | - | - | √ | - | √ | √ | √ | 7 |
| Kardouni et
al (43), 2015 | √ | √ | √ | √ | - | - | √ | √ | - | √ | √ | 7 |
| McClatchie et
al (44), 2009 | √ | √ | - | √ | - | - | √ | √ | - | √ | √ | 6 |
| Surenkok et
al (45), 2009 | √ | √ | - | - | - | - | √ | √ | - | √ | √ | 5 |
| Akbaba et al
(17), 2019 | √ | √ | √ | √ | - | - | √ | √ | √ | √ | √ | 8 |
| Bang and Deyle
(46), 2000 | √ | √ | - | √ | - | - | √ | √ | - | √ | √ | 6 |
| Camargo et
al (47), 2015 | √ | √ | √ | √ | - | - | √ | √ | √ | √ | √ | 8 |
| Eliason et
al (18), 2021 | √ | √ | √ | √ | √ | - | - | √ | √ | √ | √ | 8 |
| Haider et al
(19), 2018 | √ | √ | - | √ | - | - | - | √ | - | √ | √ | 5 |
| Kachingwe et
al (48), 2008 | √ | √ | - | - | - | - | √ | √ | - | √ | √ | 5 |
| Kromer et al
(49), 2014 | √ | √ | √ | √ | - | - | - | √ | √ | √ | √ | 7 |
| Park et al
(23), 2020 | √ | √ | √ | √ | - | - | √ | - | - | √ | √ | 6 |
| Sharma et al
(24), 2021 | √ | √ | √ | √ | √ | - | - | √ | - | √ | √ | 7 |
| Senbursa et
al (50), 2007 | √ | √ | - | √ | - | - | - | - | - | √ | √ | 4 |
| Vinuesa-Montoya
et al (51), 2017 | √ | √ | √ | √ | - | - | √ | √ | - | √ | √ | 7 |
| Barra López et
al (52), 2013 | √ | √ | - | √ | - | - | √ | - | √ | √ | √ | 6 |
| İğrek and Çolak
(21), 2021 | √ | √ | √ | √ | - | - | - | √ | √ | √ | √ | 7 |
| Menek et al
(22), 2019 | √ | √ | - | √ | - | - | - | √ | - | √ | √ | 5 |
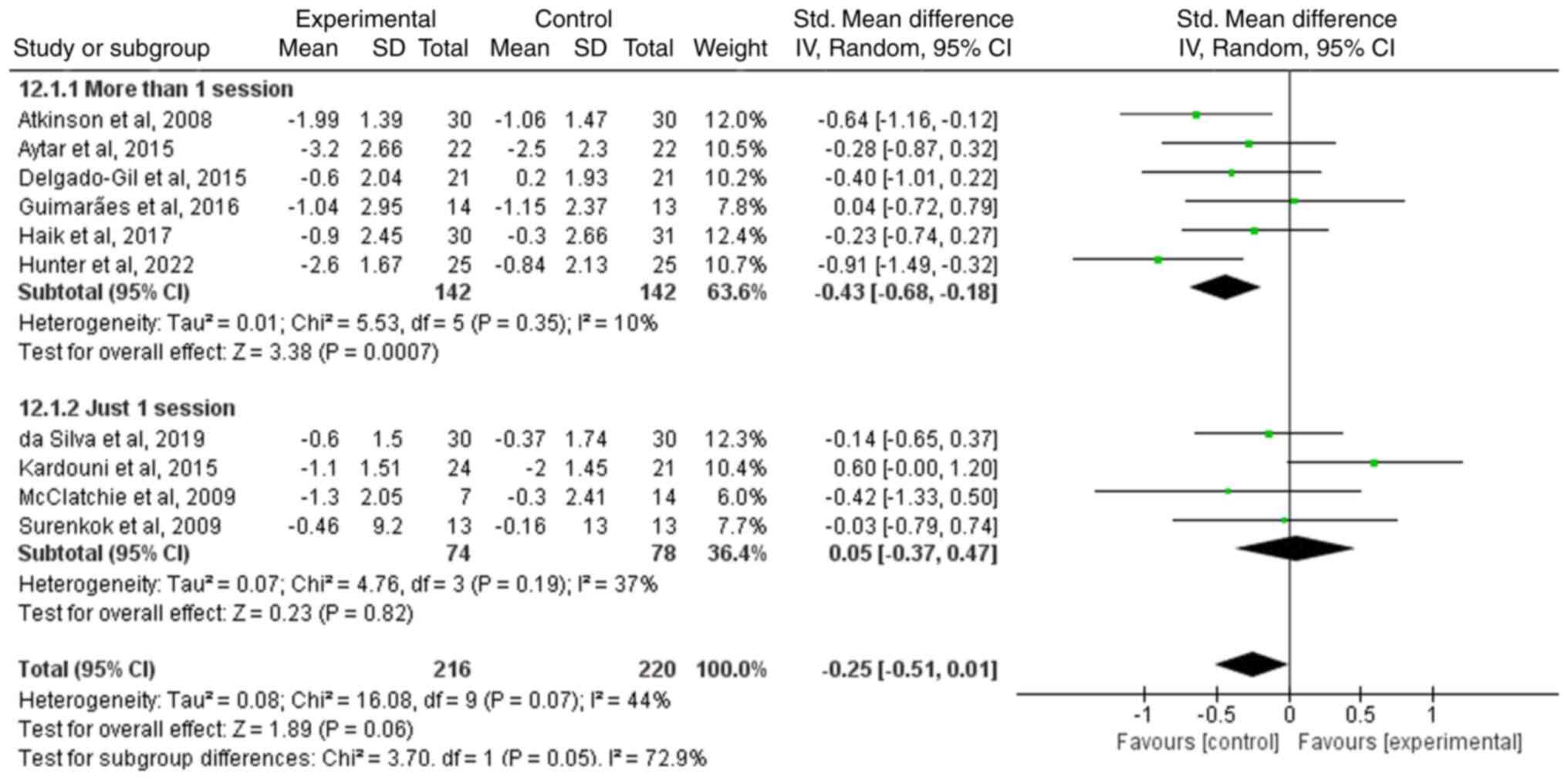
MT vs. Placebo
Pain. A total of 10 studies evaluated changes
in shoulder pain after MT compared with placebo. The heterogeneity
analysis indicated acceptable heterogeneity (I2=44% and
P=0.07). Meta-analysis demonstrated that MT could not effectively
relieve pain (SMD=-0.25; 95% CI: -0.51 to 0.01; Z=1.89; P=0.06).
Subgroup analysis revealed that while a single session of MT showed
no significant difference in pain reduction compared with placebo,
multiple MT sessions were associated with superior pain relief
(SMD=-0.43; 95% CI: -0.68 to -0.18; Z=3.38; P=0.0007) (Fig. 2). Only one study (20) conducted a 12-month long-term
follow-up, indicating sustained pain relief with MT compared with
placebo (P=0.01). In addition, subgroup analysis based on the MT
regimen were also attempted, but there was high heterogeneity in
subgroup (I2=81% and P=0.02) and no reliable conclusions
could be drawn (data not shown).
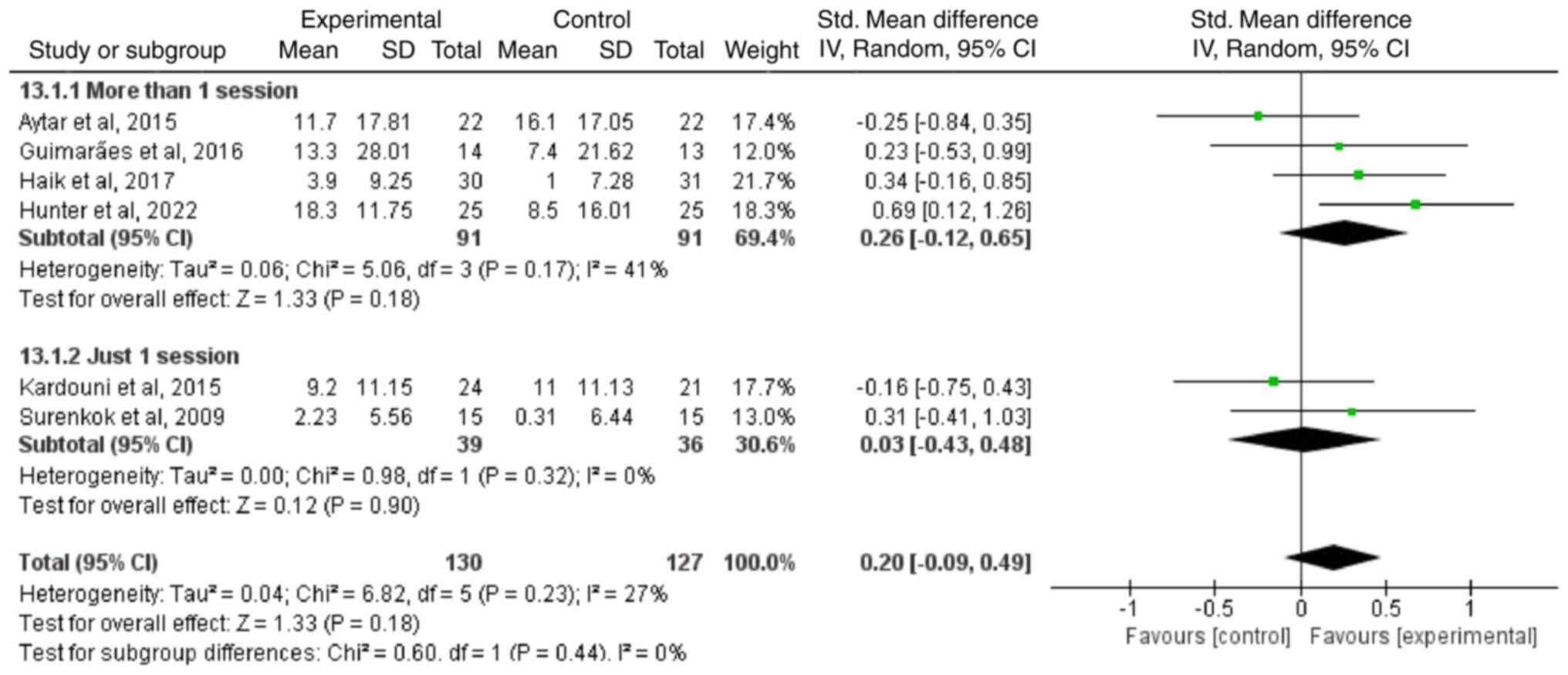
Function
A total of six studies evaluated improvements in
functional scores with MT compared with placebo. Heterogeneity
analysis revealed that I2=27% and P=0.23. Comprehensive
analysis showed no significant difference in functional improvement
between MT and placebo (SMD=0.20; 95% CI: -0.09 to 0.49; Z=1.33;
P=0.18). In subgroup analysis, there was no significant difference
in functional improvement after MT alone vs. placebo, with either a
single intervention or more than one session (Fig. 3).
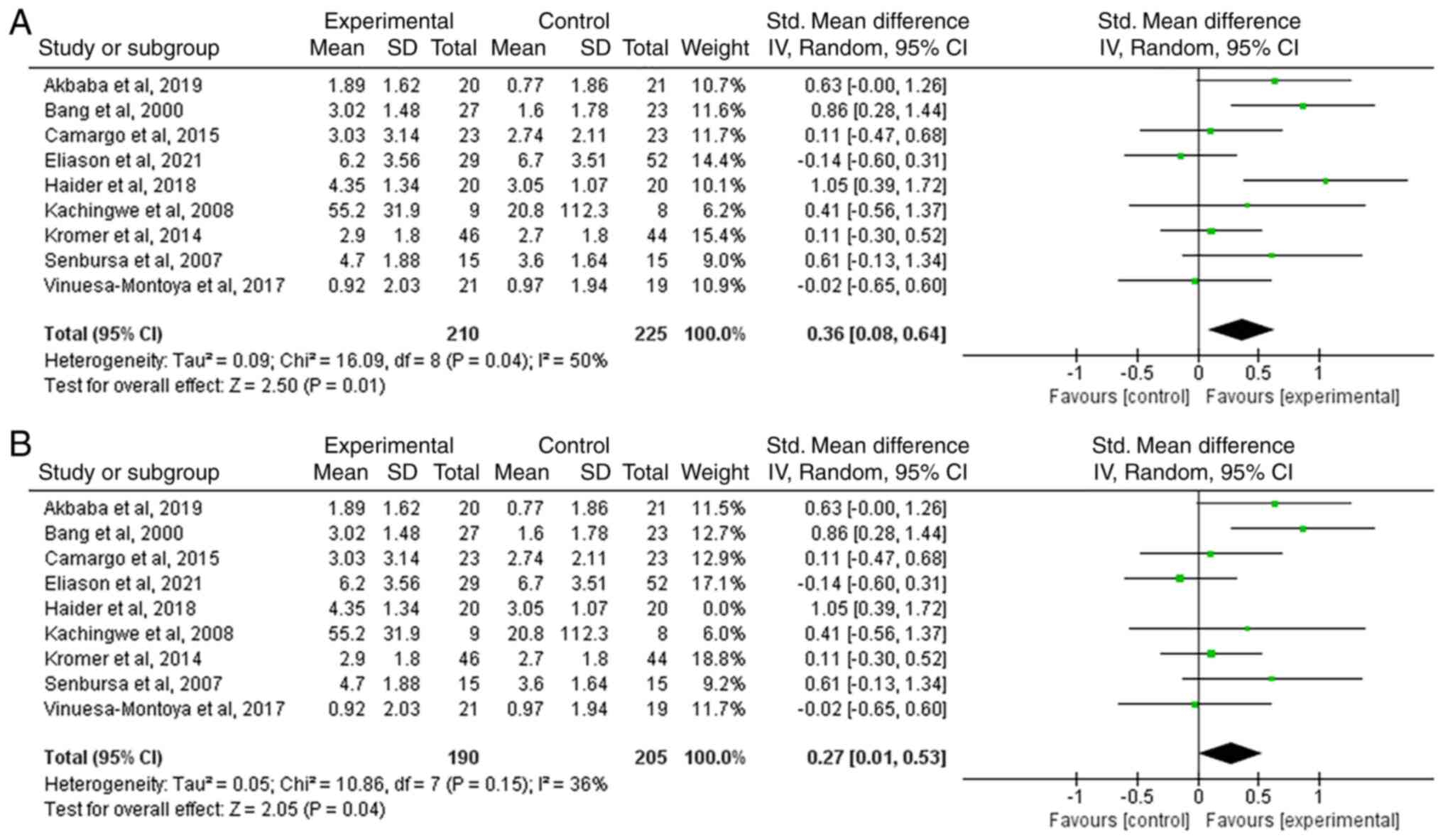
MT plus exercise vs. exercise
alone
Pain. The additional efficacy of MT in pain
reduction when added to exercise therapy was examined in nine
studies. There was high heterogeneity in the analysis
(I2=50%; P=0.04). Pooled results showed that the
addition of MT resulted in additional pain reduction compared with
exercise therapy alone (SMD=0.36; 95% CI: 0.08 to 0.64; Z=2.50;
P=0.01). A sensitivity analysis was performed because of the high
heterogeneity (I2=36%; P=0.15). Removal of the study by
Haider et al (19) provided
a significant reduction in heterogeneity but did not change the
overall findings (SMD=0.27; 95% CI: 0.01 to 0.53; Z=2.05; P=0.04)
(Fig. 4).
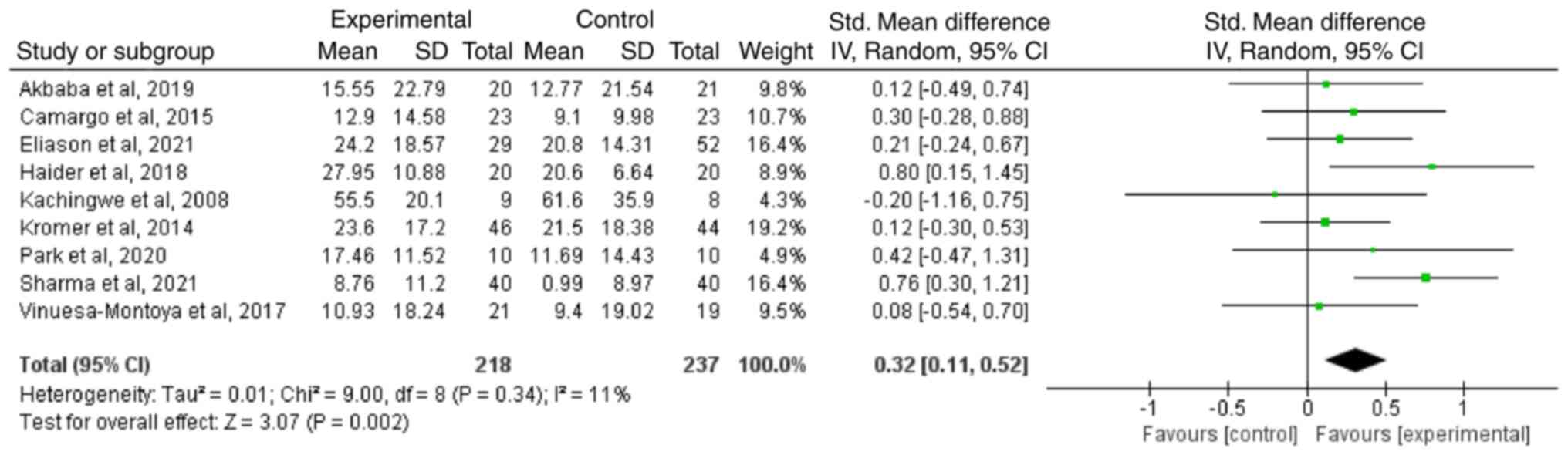
Function
A total of nine RCTs evaluated the additional
improvement in function with MT added to exercise therapy. The
heterogeneity was acceptable (I2=11%; P=0.34). Combined
results indicated that MT plus exercise therapy led to greater
functional improvement compared with exercise alone (SMD=0.32; 95%
CI: 0.11 to 0.52; Z=3.07; P=0.002) (Fig. 5).
MT plus multimodal physiotherapy vs.
multimodal physiotherapy
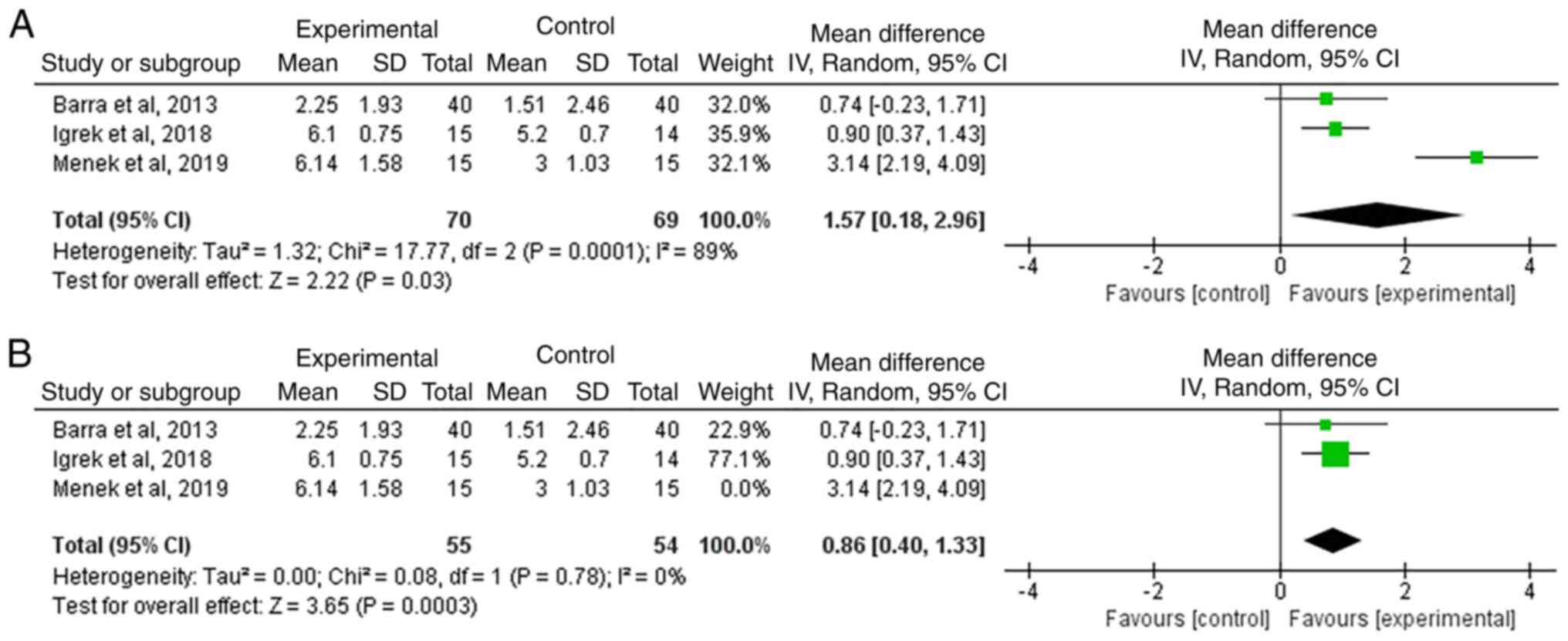
Pain. A total of three studies compared the
effect of MT plus multimodal physiotherapy vs. multimodal
physiotherapy alone on pain reduction. There was a high level of
heterogeneity (I2=89%; P=0.0001). Meta-analysis
indicated that MT combined with multimodal physiotherapy achieved
superior pain relief compared with multimodal physiotherapy alone
(MD=1.57; 95% CI: 0.18 to 2.96; Z=2.22; P=0.03). A sensitivity
analysis was performed because of the high heterogeneity. Removal
of the study by Menek et al (22) provided a significant reduction in
heterogeneity (I2=0%; P=0.78) but did not change the
overall findings (MD=0.86; 95% CI: 0.40 to 1.33; Z=3.65; P=0.0003)
(Fig. 6).
Function
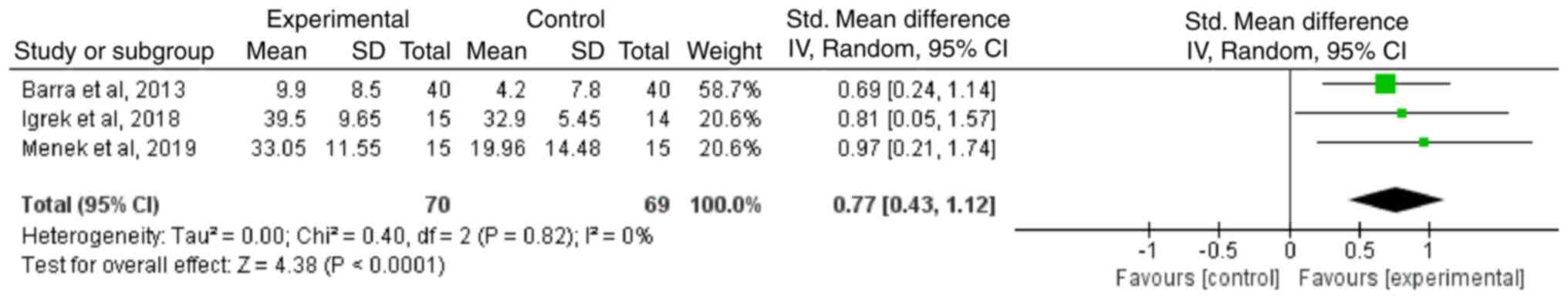
A total of three studies compared the effect of MT
plus multimodal physiotherapy with multimodal physiotherapy alone
on functional improvement. The heterogeneity was acceptable
(I2=0%; P=0.82). Meta-analysis revealed that MT combined
with multimodal physiotherapy achieved superior functional
improvement compared with multimodal physiotherapy alone (SMD=0.77;
95% CI: 0.43 to 1.12; Z=4.38; P<0.0001) (Fig. 7).
Discussion
The present systematic review and meta-analysis
assessed the efficacy of MT for RCI in terms of pain and function.
The results of the present study indicated that the improvement of
shoulder pain and function in RCI patients with MT alone is
limited. However, when combined with exercise or multimodal
physiotherapy, MT not only significantly reduced pain but also
enhanced shoulder function.
The present study revealed that MT alone is not
effective in reducing pain compared with placebo, which is
inconsistent with the findings of previous meta-analyses (14,15).
However, these previous studies had limitations in the number of
included RCTs and lacked pooled outcomes regarding functional
improvements. No significant difference in functional improvement
between MT alone and placebo were discovered. Additionally, a
variation in the number of interventions across trials was
observed, highlighting that the optimal number of MT sessions for
RCI remains unknown (53-55).
Subgroup analysis revealed that multiple intervention sessions led
to improved pain relief than single sessions, suggesting the need
to use multiple MT sessions in clinical practice.
In the clinical setting, MT and exercises are
commonly preferred as primary physiotherapy treatments for shoulder
syndromes (56). Consistent with
previous studies, the findings of the present study revealed that
combining MT with exercise yielded superior outcomes compared with
exercise alone. This may be attributed to the analgesic effect and
correction of muscle-bone imbalance by early MT, providing optimal
conditions for exercise implementation (23,24).
Exercises should be tailored to the patient's condition and
combined with appropriate restraint to regulate and repair muscle
metabolism (57).
The present study is the first systematic review to
examine the efficacy of MT added to multimodal physiotherapy for
the treatment of RCI, and it was revealed that the addition of MT
improved the effectiveness of treatment. Although multimodal
physiotherapy was not strictly defined, the included trials
commonly used exercise and electrotherapy interventions.
Electrotherapy, including infrared, therapeutic ultrasound, and
transcutaneous electrical nerve stimulation (58), is a common treatment modality for
rotator cuff disease that achieves pain relief and muscle
relaxation. The results indicated a synergistic effect of MT with
multimodal physiotherapy, especially exercise and
electrotherapy.
Several pooled results exhibited high heterogeneity
when MT was combined with exercise or multimodal physiotherapy. In
comparing the efficacy of pain reduction between the combination of
MT and exercise vs. exercise alone, a significant reduction in
heterogeneity was obtained after the study by Haider et al
(19) was excluded from the
sensitivity analysis. The study characteristics by Haider et
al were reviewed and compared with other studies and the
duration of intervention was revealed to be shorter in the present
study (2 weeks) than in other studies (at least 3 weeks). When
comparing pain improvement between MT combined with multimodal
physiotherapy and multimodal physiotherapy alone, the study by
Menek et al (22) used a
longer duration of intervention (6 weeks) than the other studies
(<4 weeks). These results suggested that duration of
intervention may be a potential source of heterogeneity.
The present study has certain limitations. Of the 24
included studies, only one (20)
had a long-term follow-up of 1 year and showed that MT improved
pain more efficiently than placebo, but the study did not report
whether there was disease progression. As a meta-analysis could not
be performed, the long-term efficacy of MT for RCI and whether it
will lead to disease progression are uncertain. Moreover,
therapeutic time window, comorbidities and degree of injury are the
confounding factors. Because of the lack of description of these
conditions in the included studies, subgroup analysis could not be
performed. Due to the limited number of studies on MT for RCI,
further network meta-analysis could not be performed.
In conclusion, the results of the present
meta-analysis demonstrated that combining MT with exercise therapy
or multimodal physiotherapy not only enhances pain relief compared
with exercise therapy or multimodal physiotherapy alone, but also
effectively improves shoulder joint function. Therefore, MT is
considered a pivotal component of conservative treatments, and its
integration with other therapeutic approaches is recommended for
optimal RCI therapy.
Supplementary Material
Search strategy of PubMed.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Medical
Innovation Project of Shanghai Science and Technology Commission
(grant nos. 21Y11921300 and 22Y11922500), the Shanghai Health and
Family Planning System Excellent Young Medical Personnel Training
Program (grant no. 2018YQ27), the Future Plan of Shanghai Municipal
Hospital of Traditional Chinese Medicine (grant nos. ZLZX001,
GZS001, MZY034 and XJRY2021003K), the Training Program for
High-caliber Talents of Clinical Research at Affiliated Hospitals
of SHUTCM (grant no. 2023LCRC18), the Shanghai University of
Traditional Chinese Medicine ‘Xinglin Hundred Talents’ Plan [grant
no. TCM (2020) 23] and the Shanghai University of Traditional
Chinese Medicine Reserve Outstanding TCM Talents [grant no.
TCM(2020) 10].
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
SL and XL conceptualized and designed the present
study. QS and XL provided administrative support. SL, LC, YF, WD
and CX carried out data collection. LS and LXF confirm the
authenticity of all the raw data. All authors participated in data
analysis and interpretation, the writing process, and read and
approved the final manuscript. All the authors confirm that the
study followed PRISMA guidelines.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lewis J, Mccreesh K, Roy JS and Ginn K:
Rotator cuff tendinopathy: Navigating the diagnosis-management
conundrum. J Orthop Sports Phys Ther. 45:923–937. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Weber S and Chahal J: Management of
rotator cuff injuries. J Am Acad Orthop Surg. 28:e193–e201.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sambandam SN, Khanna V, Gul A and
Mounasamy V: Rotator cuff tears: An evidence based approach. World
J Orthop. 6:902–918. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Godeau D, Fadel M and Descatha A: Factors
associated with limitations in daily life and at work in a
population with shoulder pain. BMC Musculoskelet Disord.
23(777)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Consigliere P, Haddo O, Levy O and Sforza
G: Subacromial impingement syndrome: management challenges. Orthop
Res Rev. 10:83–91. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ulack C, Suarez J, Brown L, Ring D,
Wallace S and Teisberg E: What are people that seek care for
rotator cuff tendinopathy experiencing in their daily life? J
Patient Exp. 9(23743735211069811)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Osborne JD, Gowda AL, Wiater B and Wiater
JM: Rotator cuff rehabilitation: Current theories and practice.
Phys Sportsmed. 44:85–92. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lewis J: Rotator cuff related shoulder
pain: Assessment, management and uncertainties. Man Ther. 23:57–68.
2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhou D, Zhou F, Sheng S, Wei Y, Chen X and
Su J: Intra-articular nanodrug delivery strategies for treating
osteoarthritis. Drug Discov Today. 28(103482)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mi CH, Qi XY, Ding YW, Zhou J, Dao JW and
Wei DX: Recent advances of medical polyhydroxyalkanoates in
musculoskeletal system. Biomater Transl. 4:234–247. 2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sun S, Liu H, Hu Y, Wang Y, Zhao M, Yuan
Y, Han Y, Jing Y, Cui J, Ren X, et al: Selection and identification
of a novel ssDNA aptamer targeting human skeletal muscle. Bioact
Mater. 20:166–178. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ying J, Yu H, Cheng L, Li J, Wu B, Song L,
Yi P, Wang H, Liu L and Zhao D: Research progress and clinical
translation of three-dimensional printed porous tantalum in
orthopaedics. Biomater Transl. 4:166–179. 2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Li J, Zhang H, Han Y, Hu Y, Geng Z and Su
J: Targeted and responsive biomaterials in osteoarthritis.
Theranostics. 13:931–954. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Desjardins-Charbonneau A, Roy JS, Dionne
CE, Frémont P, MacDermid JC and Desmeules F: The efficacy of manual
therapy for rotator cuff tendinopathy: A systematic review and
meta-analysis. J Orthop Sports Phys Ther. 45:330–350.
2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Steuri R, Sattelmayer M, Elsig S, Kolly C,
Tal A, Taeymans J and Hilfiker R: Effectiveness of conservative
interventions including exercise, manual therapy and medical
management in adults with shoulder impingement: A systematic review
and meta-analysis of RCTs. Br J Sports Med. 51:1340–1347.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Page MJ, Green S, McBain B, Surace SJ,
Deitch J, Lyttle N, Mrocki MA and Buchbinder R: Manual therapy and
exercise for rotator cuff disease. Cochrane Database Syst Rev.
2016(CD012224)2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Akbaba YA, Mutlu EK, Altun S, Turkmen E,
Birinci T and Celik D: The effectiveness of trigger point treatment
in rotator cuff pathology: A randomized controlled double-blind
study. J Back Musculoskelet Rehabil. 32:519–527. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Eliason A, Harringe M, Engström B and
Werner S: Guided exercises with or without joint mobilization or no
treatment in patients with subacromial pain syndrome: A clinical
trial. J Rehabil Med. 53(jrm00190)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Haider R, Bashir MS, Adeel M, Ijaz MJ and
Ayub A: Comparison of conservative exercise therapy with and
without maitland thoracic manipulative therapy in patients with
subacromial pain: Clinical trial. J Pak Med Assoc. 68:381–387.
2018.PubMed/NCBI
|
|
20
|
Hunter DJ, Rivett DA, Mckiernan S, Luton R
and Snodgrass SJ: Thoracic manual therapy improves pain and
disability in individuals with shoulder impingement syndrome
compared with placebo: A randomized controlled trial with 1-year
follow-up. Arch Phys Med Rehabil. 103:1533–1543. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
İğrek A and Çolak TK: Comparison of the
effectiveness of proprioceptive neuromuscular facilitation
exercises and shoulder mobilization patients with subacromial
impingement syndrome: A randomized clinical trial. J Bodyw Mov
Ther. 30:42–52. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Menek B, Tarakci D and Algun ZC: The
effect of Mulligan mobilization on pain and life quality of
patients with rotator cuff syndrome: A randomized controlled trial.
J Back Musculoskelet Rehabil. 32:171–178. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Park SJ and Kim SH and Kim SH: Effects of
thoracic mobilization and extension exercise on thoracic alignment
and shoulder function in patients with subacromial impingement
syndrome: A randomized controlled pilot study. Healthcare (Basel).
8:316–326. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sharma S, Ejaz Hussain M and Sharma S:
Effects of exercise therapy plus manual therapy on muscle activity,
latency timing and SPADI score in shoulder impingement syndrome.
Complement Ther Clin Pract. 44(101390)2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Silva ACD, Santos GM, Marques CMDG and
Marques JLB: Immediate effects of spinal manipulation on shoulder
motion range and pain in individuals with shoulder pain: A
randomized trial. J Chiropr Med. 18:19–26. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Hutton B, Salanti G, Caldwell DM, Chaimani
A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen
JP, et al: The PRISMA extension statement for reporting of
systematic reviews incorporating network meta-analyses of health
care interventions: Checklist and explanations. Ann Intern Med.
162:777–784. 2015.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Verhagen AP, De Vet HC, De Bie RA, Kessels
AG, Boers M, Bouter LM and Knipschild PG: The Delphi list: A
criteria list for quality assessment of randomized clinical trials
for conducting systematic reviews developed by Delphi consensus. J
Clin Epidemiol. 51:1235–1241. 1998.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Macedo LG, Elkins MR, Maher CG, Moseley
AM, Herbert RD and Sherrington C: There was evidence of convergent
and construct validity of physiotherapy evidence database quality
scale for physiotherapy trials. J Clin Epidemiol. 63:920–925.
2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Maher CG, Sherrington C, Herbert RD,
Moseley AM and Elkins M: Reliability of the PEDro scale for rating
quality of randomized controlled trials. Phys Ther. 83:713–721.
2003.PubMed/NCBI
|
|
30
|
Sherrington C, Herbert RD, Maher CG and
Moseley AM: PEDro. A database of randomized trials and systematic
reviews in physiotherapy. Man Ther. 5:223–226. 2000.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Karanasios S, Tsamasiotis GK, Michopoulos
K, Sakellari V and Gioftsos G: Clinical effectiveness of shockwave
therapy in lateral elbow tendinopathy: Systematic review and
meta-analysis. Clin Rehabil. 35:1383–1398. 2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Jiménez-Del-Barrio S, Cadellans-Arróniz A,
Ceballos-Laita L, Estébanez-de-Miguel E, López-de-Celis C,
Bueno-Gracia E and Pérez-Bellmunt A: The effectiveness of manual
therapy on pain, physical function, and nerve conduction studies in
carpal tunnel syndrome patients: A systematic review and
meta-analysis. Int Orthop. 46:301–312. 2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Siddall B, Ram A, Jones MD, Booth J,
Perriman D and Summers SJ: Short-term impact of combining pain
neuroscience education with exercise for chronic musculoskeletal
pain: A systematic review and meta-analysis. Pain. 163:e20–e30.
2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Hahne AJ, Ford JJ and McMeeken JM:
Conservative management of lumbar disc herniation with associated
radiculopathy: A systematic review. Spine (Phila Pa 1976).
35:E488–E504. 2010.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Slater SL, Ford JJ, Richards MC, Taylor
NF, Surkitt LD and Hahne AJ: The effectiveness of sub-group
specific manual therapy for low back pain: A systematic review. Man
Ther. 17:201–212. 2012.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Higgins JPT, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003.PubMed/NCBI View Article : Google Scholar
|
|
37
|
DerSimonian R and Laird N: Meta-analysis
in clinical trials. Control Clin Trials. 7:177–188. 1986.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Atkinson M, Matthews R, Brantingham JW,
Globe G, Cassa T, Bonnefin D and Korporaal C: A randomized
controlled trial to assess the efficacy of shoulder manipulation
versus placebo in the treatment of shoulder pain due to rotator
cuff tendinopathy. J Am Chiropr Assoc. 45:11–26. 2008.
|
|
39
|
Aytar A, Baltaci G, Uhl TL, Tuzun H, Oztop
P and Karatas M: The effects of scapular mobilization in patients
with subacromial impingement syndrome: A randomized, double-blind,
placebo-controlled clinical trial. J Sport Rehabil. 24:116–129.
2015.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Delgado-Gil JA, Prado-Robles E,
Rodrigues-de-Souza DP, Cleland JA, Fernández-de-las-Peñas C and
Alburquerque-Sendín F: Effects of mobilization with movement on
pain and range of motion in patients with unilateral shoulder
impingement syndrome: A randomized controlled trial. J Manipulative
Physiol Ther. 38:245–252. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Guimarães JF, Salvini TF, Siqueira AL Jr,
Ribeiro IL, Camargo PR and Alburquerque-Sendín F: Immediate effects
of mobilization with movement vs sham technique on range of motion,
strength, and function in patients with shoulder impingement
syndrome: Randomized clinical trial. J Manipulative Physiol Ther.
39:605–615. 2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Haik MN, Alburquerque-Sendin F and Camargo
PR: Short-term effects of thoracic spine manipulation on shoulder
impingement syndrome: A randomized controlled trial. Arch Phys Med
Rehabil. 98:1594–1605. 2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Kardouni JR, Pidcoe PE, Shaffer SW,
Finucane SD, Cheatham SA, Sousa CO and Michener LA: Thoracic spine
manipulation in individuals with subacromial impingement syndrome
does not immediately alter thoracic spine kinematics, thoracic
excursion, or scapular kinematics: A randomized controlled trial. J
Orthop Sports Phys Ther. 45:527–538. 2015.PubMed/NCBI View Article : Google Scholar
|
|
44
|
McClatchie L, Laprade J, Martin S, Jaglal
SB, Richardson D and Agur A: Mobilizations of the asymptomatic
cervical spine can reduce signs of shoulder dysfunction in adults.
Man Ther. 14:369–374. 2009.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Surenkok O, Aytar A and Baltaci G: Acute
effects of scapular mobilization in shoulder dysfunction: A
double-blind randomized placebo-controlled trial. J Sport Rehabil.
18:493–501. 2009.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Bang MD and Deyle GD: Comparison of
supervised exercise with and without manual physical therapy for
patients with shoulder impingement syndrome. J Orthop Sports Phys
Ther. 30:126–137. 2000.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Camargo PR, Alburouerque-Sendin F, Avila
MA, Haik MN, Vieira A and Salvini TF: Effects of stretching and
strengthening exercises, with and without manual therapy, on
scapular kinematics, function, and pain in individuals with
shoulder impingement: A randomized controlled trial. J Orthop
Sports Phys Ther. 45:984–997. 2015.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Kachingwe AF, Phillips B, Sletten E and
Plunkett SW: Comparison of manual therapy techniques with
therapeutic exercise in the treatment of shoulder impingement: A
randomized controlled pilot clinical trial. J Man Manip Ther.
16:238–247. 2008.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Kromer TO, de Bie RA and Bastiaenen CH:
Effectiveness of physiotherapy and costs in patients with clinical
signs of shoulder impingement syndrome: One-year follow-up of a
randomized controlled trial. J Rehabil Med. 46:1029–1036.
2014.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Senbursa G, Baltaci G and Atay A:
Comparison of conservative treatment with and without manual
physical therapy for patients with shoulder impingement syndrome: A
prospective, randomized clinical trial. Knee Surg Sports Traumatol
Arthrosc. 15:915–921. 2007.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Vinuesa-Montoya S, Aguilar-Ferrándiz ME,
Matarán-Peñarrocha GA, Fernández-Sánchez M, Fernández-Espinar EM
and Castro-Sánchez AM: A preliminary randomized clinical trial on
the effect of cervicothoracic manipulation plus supervised
exercises vs a home exercise program for the treatment of shoulder
impingement. J Chiropr Med. 16:85–93. 2017.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Barra López ME, López de Celis C,
Fernández Jentsch G, Raya de Cárdenas L, Lucha López MO and Tricás
Moreno JM: Effectiveness of diacutaneous fibrolysis for the
treatment of subacromial impingement syndrome: A randomised
controlled trial. Man Ther. 18:418–424. 2013.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Haas M, Bronfort G, Evans R, Schulz C,
Vavrek D, Takaki L, Hanson L, Leininger B and Neradilek MB:
Dose-response and efficacy of spinal manipulation for care of
cervicogenic headache: A dual-center randomized controlled trial.
Spine J. 18:1741–1754. 2018.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Sturman S and Killingback C: Is there a
dose response relationship between soft tissue manual therapy and
clinical outcomes in fibromyalgia? J Bodyw Mov Ther. 24:141–153.
2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Perlman AI, Ali A, Njike VY, Hom D, Davidi
A, Gould-Fogerite S, Milak C and Katz DL: Massage therapy for
osteoarthritis of the knee: A randomized dose-finding trial. PLoS
One. 7(e30248)2012.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Kooijman M, Swinkels I, Van Dijk C, de
Bakker D and Veenhof C: Patients with shoulder syndromes in general
and physiotherapy practice: An observational study. BMC
Musculoskelet Disord. 14(128)2013.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Eggelbusch M, Charlton BT, Bosutti A,
Ganse B, Giakoumaki I, Grootemaat AE, Hendrickse PW, Jaspers Y,
Kemp S, Kerkhoff TJ, et al: The impact of bed rest on human
skeletal muscle metabolism. Cell Rep Med. 5(101372)2024.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Page MJ, Green S, Mrocki MA, Surace SJ,
Deitch J, McBain B, Lyttle N and Buchbinder R: Electrotherapy
modalities for rotator cuff disease. Cochrane Database Syst Rev.
2016(CD012225)2016.PubMed/NCBI View Article : Google Scholar
|