Introduction
Urinary bladder cancer is the second most common
urological cancer and is responsible for 2.0% of cancer-related
mortality cases worldwide (1).
Muscle invasion is a key factor for the prognosis of patients with
bladder cancer. Non-muscle invasive bladder cancer (stages Ta, T1
and Tis) generally has a good prognosis, whereas muscle-invasive
bladder cancer (MIBC; stages T2, T3 and T4) frequently develops
metastases and has a poor prognosis, with a 5-year survival of
65–70% following radical cystectomy (2,3).
However, clinical and pathological markers for the prediction of
prognosis of patients with bladder cancer following radical
cystectomy have not yet been established.
Heat shock proteins (HSPs) are stress proteins
released in response to various stress factors, such as heat,
infection, ischemia and cancer (4). The expression of HSPs in cancer cells
has been implicated in the regulation of apoptosis (5,6).
HSPs also modulate cancer cell immunogenicity (7,8).
Heat shock protein 105 (Hsp105) is a high-molecular-weight protein
that belongs to the Hsp105/110 family. It is one of several
cancer/testis antigens that were identified by serological analysis
of antigens by recombinant expression cloning (SEREX) (9). Previous studies have suggested that
Hsp105 enhances stress-induced apoptosis in embryonal cells
(10), while suppressing
stress-induced apoptosis in neuronal (11) and cancer cells (12,13).
Hosaka et al (12) reported
that the knockdown of Hsp105 induced apoptosis in the HCT116 human
colon cancer and the KATO-3 human gastric cancer cell lines.
Furthermore, Hsp105 was shown to be overexpressed in a variety of
human cancer cells, including colorectal, pancreatic, thyroid,
esophageal, breast and bladder cancer cells (14). High expression of Hsp105 has been
associated with advanced stage of squamous cell carcinoma of the
tongue (15), in addition to
advanced stage and poor prognosis of lung adenocarcinoma (16). Recently, Hsp105 was proposed as a
target molecule for immunotherapy due to its immunogenicity
(17). However, no correlation
between the level of Hsp105 expression and the prognosis for
bladder cancer has been reported thus far.
The aim of this study was to investigate Hsp105
expression in primary bladder cancer tissues from patients treated
with radical cystectomy and its effect on cancer-specific survival
(CSS) of bladder cancer.
Materials and methods
Surgical specimens
A tissue microarray (TMA) containing 88 human
bladder specimens was used in this study. The bladder specimens
included 84 primary bladder cancer samples (81 urothelial and 3
squamous cell carcinomas) and 4 specimens of non-cancerous bladder
mucosa. The 84 primary bladder cancer samples were obtained from
patients who underwent radical cystectomy at the University of
Tokyo Hospital between 1990 and 2005. The patients comprised 70
males and 14 females, with a median age of 65 years (range, 39–81
years). The 4 non-cancerous bladder specimens were obtained from
patients who underwent cystectomy for causes other than
malignancy.
All patients provided consent for this study prior
to surgery. All analyses of human materials were performed
according to the guidelines of the Ethics Committee of the
University of Tokyo. The samples were diagnosed and classified by a
urological pathologist (T.M.) at the Department of Pathology,
University of Tokyo Hospital.
Immunohistochemical analysis
Immunohistochemical staining was performed using the
EnVision+ system HRP labelled polymer anti-rabbit kit (Dako,
Glostrup, Denmark) according to the manufacturer’s instructions.
The primary antibody used was a rabbit polyclonal anti-human Hsp105
antibody (N-187: sc-6241), purchased from Santa Cruz Biotechnology,
Inc. (Santa Cruz, CA, USA). Following the visualization of Hsp105
using Liquid DAB+ substrate chromogen system (Dako), the sections
were counterstained with hematoxylin. The immunoreactivity of
Hsp105 expression was scored by a urological pathologist (T.M.)
according to the intensity of the signal as follows: score 0, none;
score 1, mild; score 2, moderate; and score 3, intense. Hsp105
scores of 0 and 1 were defined as ‘low’, whereas scores of 2 and 3
were defined as ‘high’.
Statistical analyses
Correlation between the expression of Hsp105 and the
clinicopathological characteristics of human bladder specimens were
evaluated using the Pearson’s χ2 or the Fisher’s exact
tests. The CSS curves of patients with primary bladder cancer were
determined using the Kaplan-Meier method and statistical
significance was analyzed using the log-rank test. A multivariate
analysis of the prognostic factors was performed using the Cox
proportional hazards regression model. JMP software (SAS Institute,
Cary, NC, USA) was used for all the analyses. P<0.05 was
considered to indicate a statistically significant difference.
Results
Expression of Hsp105 in human primary
bladder cancer and correlation with clinicopathological
characteristics
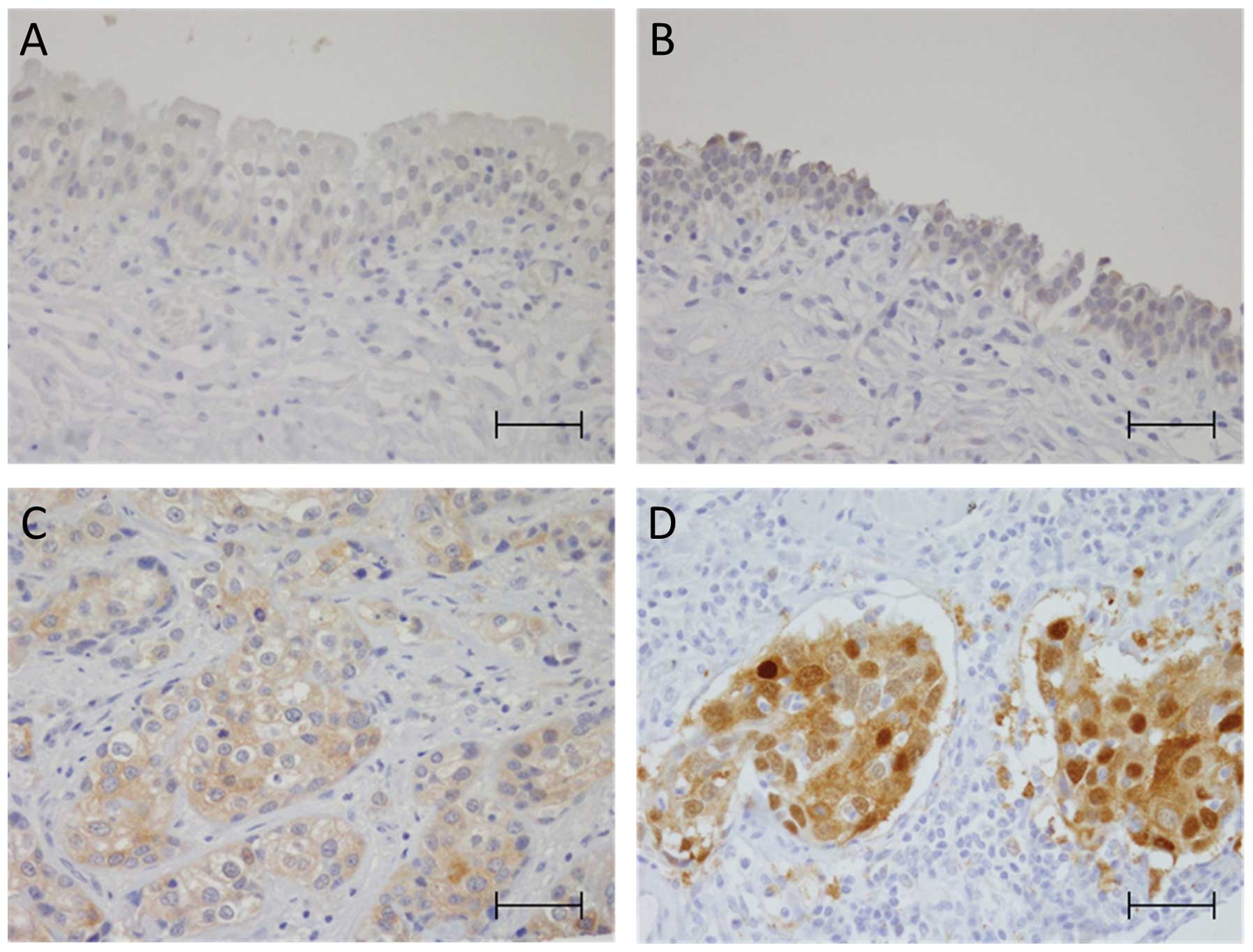
The immunoreactivity score for Hsp105 was low in all
4 non-cancerous bladder urothelium samples (score: 0 in 2 cases and
1 in 2 cases, Fig. 1A and B). In
the 84 primary bladder cancer samples, the HSP score was low in 53
cases (63%, score 0 in 23 cases and 1 in 30 cases) and high in 31
cases (37%, score 2 in 20 cases and 3 in 11 cases, Fig. 1C and D).
Subsequently the correlation between Hsp105 scores
and the clinicopathological characteristics of primary bladder
cancer was investigated. As summarized in Table I, the Hsp105 score was not
correlated with age, nuclear grade, or pathological tumor stage
(P=0.575, 0.809 and 0.995, respectively). Female gender,
lymphovascular invasion and lymph node metastasis exhibited a
tendency towards lower Hsp105 scores, although the differences were
not statistically significant (P=0.071, 0.061 and 0.175,
respectively).
 | Table I.Correlation between Hsp105 score and
clinicopathological characteristics in 84 primary bladder cancer
cases. |
Table I.
Correlation between Hsp105 score and
clinicopathological characteristics in 84 primary bladder cancer
cases.
| Clinicopathological
characteristics | n | Hsp105 score
| P-value |
|---|
| Low (0, 1) | High (2, 3) |
|---|
| All cases | 84 | 53 (63) | 31 (37) | |
| Gender | | | | |
| Male | 70 | 41 (59) | 29 (41) | 0.071 |
| Female | 14 | 12 (86) | 2 (14) | |
| Age (years) | | | | |
| <65 | 44 | 29 (66) | 15 (34) | 0.575 |
| >66 | 40 | 24 (60) | 16 (40) | |
| Nuclear gradea | | | | |
| G1/G2 | 21 | 13 (62) | 8 (38) | 0.809 |
| G3 | 60 | 37 (62) | 23 (38) | |
| Pathological tumor
stage | | | | |
| pTa/pTis/pT1 | 23 | 14 (61) | 9 (39) | 0.995 |
| pT2/pT3/pT4 | 61 | 39 (64) | 22 (36) | |
| Lymphovascular
invasion | | | | |
| Negative | 35 | 18 (51) | 17 (49) | 0.061 |
| Positive | 49 | 35 (71) | 14 (29) | |
| Lymph node
metastasis | | | | |
| pN0 | 65 | 38 (58) | 27 (42) | 0.175 |
| pN1/pN2/pN3 | 19 | 15 (79) | 4 (21) | |
| Previous BCG
therapy | | | | |
| Negative | 63 | 40 (63) | 23 (37) | 0.896 |
| Positive | 21 | 13 (62) | 8 (38) | |
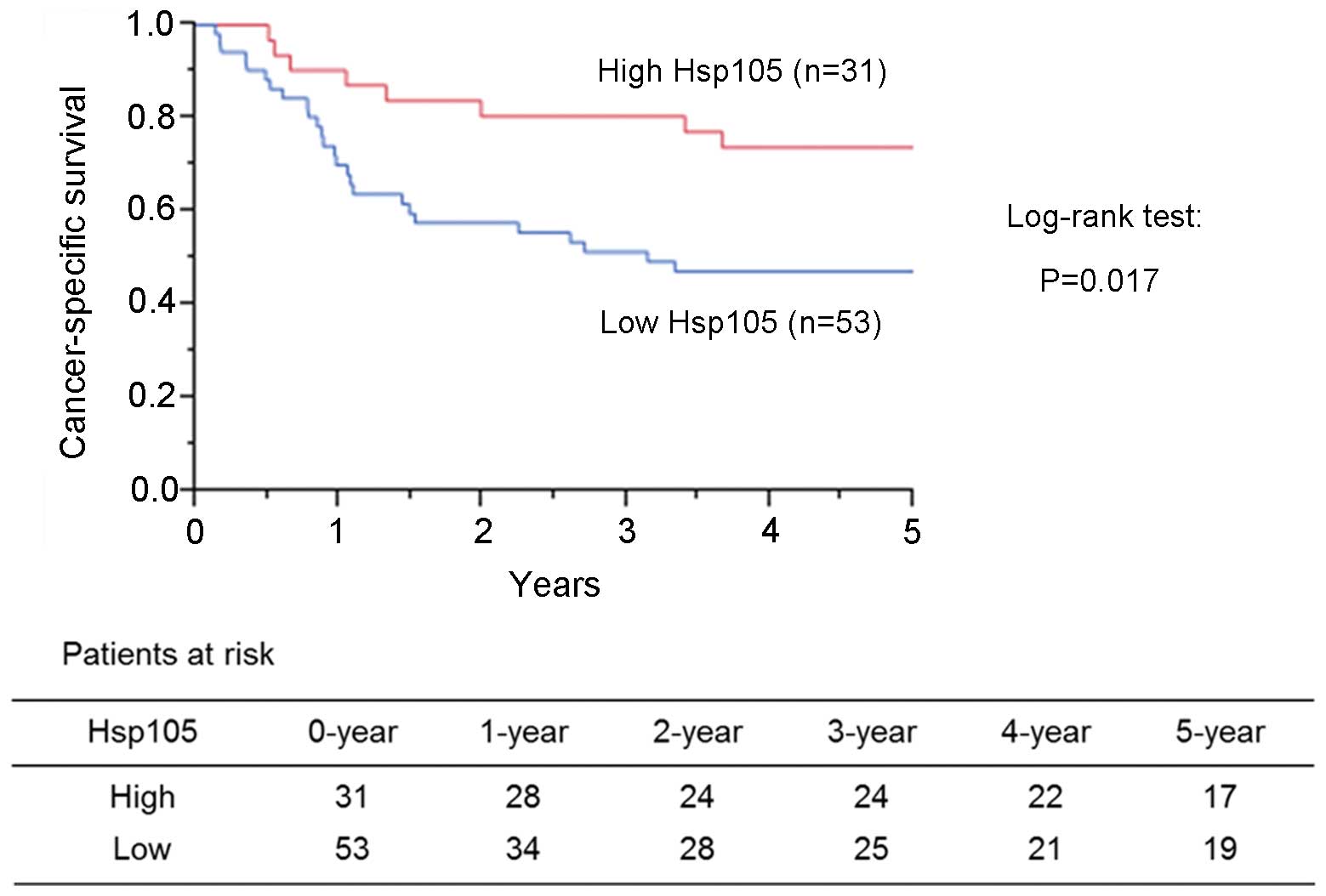
Correlation between expression of Hsp105
and the prognosis of patients with primary bladder cancer
The effect of the Hsp105 score on the CSS of
patients with primary bladder cancer was investigated. The 5-year
CSS for patients with high Hsp105 scores was 73.3% compared to
46.9% for those with low Hsp105 scores. Patients with high Hsp105
scores had a statistically better CSS compared to those with low
Hsp105 scores (P=0.017; log-rank test, Fig. 2).
The prognostic value of Hsp105 expression and the
clinicopathological characteristics for CSS was subsequently
examined (Table II). In the
univariate analysis, Hsp105 expression, pathological tumor stage,
lymphovascular invasion and lymph node metastasis were variables
significantly associated with survival. The multivariate Cox
proportional hazard analysis demonstrated that Hsp105 expression
was an independent indicator for CSS (P=0.032; hazard ratio=2.34),
along with pathological tumor stage.
 | Table II.Prognostic values of Hsp105 expression
and clinicopathological characteristics for cancer-specific
survival in 84 patients with primary bladder cancer. |
Table II.
Prognostic values of Hsp105 expression
and clinicopathological characteristics for cancer-specific
survival in 84 patients with primary bladder cancer.
| Variable | Univariate analysis
P-value | Multivariate Cox
proportional hazards regression analysis
|
|---|
| HR | 95% CI | P-value |
|---|
| Hsp105 score (high
vs. low) | 0.017a | 2.34 | 1.07–5.65 | 0.032a |
| Gender (male vs.
female) | 0.165 | - | - | - |
| Age (<65 vs.
>66 years) | 0.470 | - | - | - |
| Nuclear grade (G1/G2
vs. G3) | 0.638 | - | - | - |
| pT stage
(pTa/pTis/pT1 vs. pT2/pT3/pT4) | <0.001a | 6.69 | 1.76–44.0 | 0.003a |
| Lymph node
metastasis (negative vs. positive) | <0.001a | 1.62 | 0.746–3.55 | 0.220 |
| Lymphovascular
invasion (negative vs. positive) | <0.001a | 1.40 | 0.548–3.93 | 0.492 |
| Previous BCG
therapy (yes vs. no) | 0.099 | - | - | - |
Discussion
Previous studies have reported that a high
expression of Hsp105 in squamous cell carcinoma of the tongue
(15) and lung adenocarcinoma
(16) was associated with disease
progression and/or poor prognosis. By contrast, the present study
demonstrated that the high expression of Hsp105 was significantly
associated with a favorable prognosis in urinary bladder cancer.
These findings suggest that Hsp105 may play a different role in
bladder cancer compared to squamous cell carcinoma of the tongue
and lung adenocarcinoma. The poor prognosis observed in cases
exhibiting a low expression of Hsp105 may be attributed to their
inability to elicit an immune response.
In bladder cancer, the expression of other HSPs,
such as Hsp27, -60, -70 and -90, was previously investigated.
Lebret et al (18) reported
that low expression of Hsp27 and Hsp60 were correlated with higher
tumor stage, whereas low expression of Hsp60 and Hsp90 were
correlated with infiltrating recurrence. Kamada et al
(19) reported that Hsp27
knockdown inhibited tumor growth and enhanced sensitivity to
chemotherapy in UMUC-3 human bladder cancer cells. Urushibara et
al (20) reported that Hsp60
expression was associated with a good pathological response to
neoadjuvant chemoradiotherapy. However, Syrigos et al
(21) reported that Hsp70
expression was correlated with tumor grade, stage and overall
survival. Those reports suggested that Hsp27, -60 and -90 may be
involved in the suppression of bladder cancer, whereas Hsp70 may be
involved in the progression of bladder cancer. Our results
indicated that Hsp105 plays a protective role against bladder
cancer progression, as do Hsp27, -60 and -90.
Notably, Hsp105 expression did not correlate with
the pathological tumor stage, but correlated significantly with a
favorable prognosis of bladder cancer patients. As tumors with
lymphovascular invasion and lymph node metastasis exhibited a
tendency for low Hsp105 scores, low Hsp105 expression may be
associated with lymphovascular invasion and/or metastasis, rather
than depth of tumor invasion, leading to the poor prognosis of
patients. Furthermore, female gender was also associated with low
Hsp105 scores. Generally, the female gender was shown to be
associated with a higher recurrence rate and cancer-specific
mortality following radical cystectomy (22,23),
although the underlying causes have not been determined. A possible
explanation is that the immunogenicity of Hsp105 may be associated
with the inferior prognosis of female patients.
Zappassodi et al (17) reported that Hsp105-specific immune
responses were induced by dendritic cell-based vaccination in
relapsed B-cell non-Hodgkin lymphoma patients. The anti-lymphoma
activity of the anti-Hsp105 antibody was demonstrated in
vivo in xenotransplanted immunodeficient mice. Therefore,
anti-Hsp105-specific immune responses may contribute to the
prognosis of bladder cancer patients. However, in the present
study, plasma or serum was not available from the patients whose
specimens were used for TMA. Therefore, it remains to be elucidated
whether anti-Hsp105 immune responses are induced in bladder cancer
patients undergoing radical cystectomy. A prospective study is
currently under planning to address this issue.
The multivariate analysis revealed that the high
expression of Hsp105 was an independent factor for the prediction
of a favorable prognosis of patients treated with radical
cystectomy. Despite the advances in the methods of detection,
surgical techniques, chemotherapy and irradiation, MIBC remains
associated with a poor prognosis. The expression of Hsp105 may
provide a novel prognostic marker in bladder cancer and enable the
selection of a more appropriate treatment for patients with
MIBC.
References
|
1.
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2.
|
Hautmann RE, Gschwend JE, de Petriconi RC,
Kron M and Volkmer BG: Cystectomy for transitional cell carcinoma
of the bladder: results of a surgery only series in the neobladder
era. J Urol. 176:486–492. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Shariat SF, Karakiewicz PI, Palapattu GS,
et al: Outcomes of radical cystectomy for transitional cell
carcinoma of the bladder: a contemporary series from the Bladder
Cancer Research Consortium. J Urol. 176:2414–2422. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Lindquist S and Craig EA: The heat-shock
proteins. Annu Rev Genet. 22:631–677. 1988. View Article : Google Scholar
|
|
5.
|
Takayama S, Reed JC and Homma S:
Heat-shock proteins as regulators of apoptosis. Oncogene.
22:9041–9047. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Sreedhar AS and Csermely P: Heat shock
proteins in the regulation of apoptosis: new strategies in tumor
therapy: a comprehensive review. Pharmacol Ther. 101:227–257. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Suto R and Srivastava PK: A mechanism for
the specific immunogenicity of heat shock protein-chaperoned
peptides. Science. 269:1585–1588. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Melcher A, Todryk S, Hardwick N, Ford M,
Jacobson M and Vile RG: Tumor immunogenicity is determined by the
mechanism of cell death via induction of heat shock protein
expression. Nat Med. 4:581–587. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Nakatsura T, Senju S, Yamada K, Jotsuka T,
Ogawa M and Nishimura Y: Gene cloning of immunogenic antigens
overexpressed in pancreatic cancer. Biochem Biophys Res Commun.
281:936–944. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Yamagishi N, Saito Y, Ishihara K and
Hatayama T: Enhancement of oxidative stress-induced apoptosis by
Hsp105alpha in mouse embryonal F9 cells. Eur J Biochem.
269:4143–4151. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Hatayama T, Yamagishi N, Minobe E and
Sakai K: Role of hsp105 in protection against stress-induced
apoptosis in neuronal PC12 cells. Biochem Biophys Res Commun.
288:528–534. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Hosaka S, Nakatsura T, Tsukamoto H,
Hatayama T, Baba H and Nishimura Y: Synthetic small interfering RNA
targeting heat shock protein 105 induces apoptosis of various
cancer cells both in vitro and in vivo. Cancer Sci. 97:623–632.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Yamagishi N, Ishihara K, Saito Y and
Hatayama T: Hsp105 family proteins suppress staurosporine-induced
apoptosis by inhibiting the translocation of Bax to mitochondria in
HeLa cells. Exp Cell Res. 312:3215–3223. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Kai M, Nakatsura T, Egami H, Senju S,
Nishimura Y and Ogawa M: Heat shock protein 105 is overexpressed in
a variety of human tumors. Oncol Rep. 10:1777–1782. 2003.PubMed/NCBI
|
|
15.
|
Mohtasham N, Babakoohi S,
Montaser-Kouhsari L, et al: The expression of heat shock proteins
27 and 105 in squamous cell carcinoma of the tongue and
relationship with clinicopathological index. Med Oral Patol Oral
Cir Bucal. 16:e730–e735. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Oda T, Morii E, Inoue M, Ikeda J, Aozasa K
and Okumura M: Prognostic significance of heat shock protein 105 in
lung adenocarcinoma. Mol Med Rep. 2:603–607. 2009.PubMed/NCBI
|
|
17.
|
Zappasodi R, Bongarzone I, Ghedini GC, et
al: Serological identification of HSP105 as a novel non-Hodgkin
lymphoma therapeutic target. Blood. 118:4421–4430. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Lebret T, Watson RW, Molinie V, et al:
Heat shock proteins HSP27, HSP60, HSP70, and HSP90: expression in
bladder carcinoma. Cancer. 98:970–977. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Kamada M, So A, Muramaki M, Rocchi P,
Beraldi E and Gleave M: Hsp27 knockdown using nucleotide-based
therapies inhibit tumor growth and enhance chemotherapy in human
bladder cancer cells. Mol Cancer Ther. 6:299–308. 2007. View Article : Google Scholar
|
|
20.
|
Urushibara M, Kageyama Y, Akashi T, et al:
HSP60 may predict good pathological response to neoadjuvant
chemoradiotherapy in bladder cancer. Jpn J Clin Oncol. 37:56–61.
2007. View Article : Google Scholar
|
|
21.
|
Syrigos KN, Harrington KJ, Karayiannakis
AJ, et al: Clinical significance of heat shock protein-70
expression in bladder cancer. Urology. 61:677–680. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Fajkovic H, Halpern JA, Cha EK, et al:
Impact of gender on bladder cancer incidence, staging, and
prognosis. World J Urol. 29:457–463. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
May M, Stief C, Brookman-May S, et al:
Gender-dependent cancer-specific survival following radical
cystectomy. World J Urol. 30:707–713. 2012. View Article : Google Scholar
|