Introduction
The treatment of patients with refractory or
relapsed aggressive non-Hodgkin lymphoma (NHL) represents a
challenge. In addition to polychemotherapy with regimens such as
R-DHAP (rituximab, dexamethasone, high-dose cytarabine and
cisplatin), R-ICE (rituximab, ifosfamide, carboplatin and
etoposide) or Dexa-BEAM (dexamethasone, carmustine, etoposide,
cytarabine and melphalan), hematopoietic stem cell transplantation
(HSCT) constitutes a therapeutic option. Autologous and allogeneic
HSCT (allo-HSCT) have been employed in this setting. The most
satisfactory results for autologous HSCT have been obtained in
patients with relapsed but chemosensitive diffuse large B-cell
lymphoma (1). However, the patient
characteristics have changed over the years, as the majority of the
patients received antibody-based immunochemotherapies. Moreover,
other aggressive histological types, such as peripheral T-cell
lymphoma, mantle cell lymphoma and Burkitt lymphoma, generally do
not achieve sustained remissions following autologous HSCT
(2,3). Under these conditions, the patients
may benefit from the graft-versus-lymphoma (GvL) effect following
allo-HSCT, despite target structures still requiring proper
definition in NHL. By contrast, autologous transplantation lacking
this allo-recognition may not be sufficient, particularly for
patients with early relapse (ER) or refractory disease (4). As regards allo-HSCT,
reduced-intensity conditioning (RIC) has been used for patients
with relapsed or refractory NHL, due to the fact that these
patients are extensively pretreated and may be older than 60 years
(5,6).
The combination of treosulfan and fludarabine as a
conditioning regimen has been proven to be feasible and efficient
in several types of malignancies, including acute myeloid leukemia,
myelodysplastic syndrome and multiple myeloma (7–10).
However, despite encouraging data, treosulfan/fludarabine
conditioning preceding allo-HSCT has not been systemically
investigated in patients with relapsed or refractory NHL.
To the best of our knowledge, this study is the
first to present an analysis of 88 patients with refractory or
relapsed aggressive NHL who received this conditioning regimen and
an allo-HSCT at the transplantation units of the University of
Essen, the University of Jena and the University of Rostock. The
efficacy of the treosulfan/fludarabine regimen was assessed, as was
the time to engraftment, acute and chronic graft-versus-host
disease (cGvHD), graft failure, overall survival (OS) and
disease-free survival (DFS).
Patients and methods
Patient characteristics
A total of 88 patients with relapsed or refractory
NHL were treated at the Stem Cell Transplant Units of the
University of Essen (n=45), the University of Jena (n=10) and the
University of Rostock (n=33), between 2001 and 2010. The patient
characteristics are summarized in Table I.
 | Table IPatient characteristics (n=88). |
Table I
Patient characteristics (n=88).
| Variables | Values |
|---|
| Median age at HSCT,
years (range) | 50 (21–71) |
| Male/female, n
(%) | 52/36 (59/41) |
| Earlier
therapies |
| Prior therapy
regimens, n (range) | 2.5 (1–7) |
| Prior auto-HSCT,
n | 47 |
| Histology, n (%) |
| Chronic lymphocytic
leukemia | 23 (26.1) |
| Diffuse large B-cell
lymphoma | 22 (25.0) |
| Transformed
aggressive NHL | 11 (12.5) |
| Mantle cell
lymphoma | 8 (9.1) |
| Follicular
lymphoma | 7 (8.0) |
| High-grade
T-NHL | 4 (4.5) |
| Peripheral T-cell
lymphoma-NOS | 4 (4.5) |
| Immunocytoma | 2 (2.3) |
| Primary mediastinal
large B-cell lymphoma | 2 (2.3) |
| Anaplastic
large-cell lymphoma | 2 (2.3) |
| T-cell
prolymphocytic leukemia | 2 (2.3) |
| Burkitt
lymphoma | 1 (1.1) |
| Relapsed patients, n
(%) |
| Total relapses | 73 (83.0) |
| Early relapses
(<6 months) | 18 (20.5) |
| Remission status
directly prior to HSCT, n (%) | 88 |
| CR | 26 (29.5) |
| PR | 43 (48.9) |
| SD | 7 (8.0) |
| PD | 12 (13.6) |
Notably, the treatment of NHL prior to the
transplantation included a mean of 2.5 therapy regimens, with a
range of 1–7 pre-therapies. These therapies included R-CHOP
(rituximab, cyclophosphamide, daunorubicin, vincristin,
prednisolone), R-DHAP, Dexa-BEAM, as well as prior autologous HSCT
in 47 of the 88 patients (53.4%). Of the 88 patients, 73 (83.0%)
relapsed, with 18 patients (20.5%) relapsing within 6 months after
the initial treatment. The remission status was assessed according
to the guidelines of the National Cancer Institute-sponsored
International Working Group (11).
This study was performed in accordance with the
Declaration of Helsinki and was approved by the Institutional
Review Board (University of Rostock, Rostock, Germany). All the
patients signed an informed consent prior to this study.
Conditioning regimen
Treosulfan (Medac GmbH, Hamburg, Germany) was
administered on 3 consecutive days (days 6-4), at a dose of 14
g/m2, or on 5 consecutive days (days 6-2), at a dose of
10 g/m2. Fludarabine (Schering AG, Berlin, Germany) was
administered intravenously at a dose of 30 mg/m2 on 5
consecutive days (days 6-2), to a total dose of 150
mg/m2.
GvHD prophylaxis and anti-infective
prophylaxis
In case of matched unrelated donors, but not in the
case of matched related donors, anti-thymocyte globulin was
administered at a dose of 10 mg/kg body weight (BW) (days 4-2). The
patients received cyclosporine A at a dosage of 1.5 mg/kg BW every
12 hours. Full dosage of cyclosporine was maintained for 3 months
and tapered thereafter. As an additional immunosuppressant, the
patients received either methotrexate or mycophenolate mofetil
(CellCept; F. Hoffmann-La Roche Ltd., Basel, Switzerland). The
patients received a standard prophylaxis for viral, bacterial and
fungal infections and for Pneumocystis jirovecii, according
to local standards.
Definition of engraftment, GvHD
Leukocyte engraftment was defined as the first of 3
consecutive days, with an absolute neutrophil count of
≥0.5×109/l neutrophils.
Acute GvHD was evaluated in patients surviving for
at least 30 days and classified according to the modified Seattle
Glucksberg criteria (12). cGvHD
was assessed in patients with a follow-up of at least 100 days
post-transplantation and scored according to the revised Seattle
criteria (13).
Statistical analysis
The disease remission status and response were
classified on an intent-to-treat basis. Patients with a survival or
follow-up of at least 60 days after the HSCT were included in the
response analysis. DFS was defined as the time from HSCT to death
or disease progression/relapse. OS was defined as the time from the
HSCT to death or the last follow-up.
The SPSS/PC software package, version 15.0 (SPSS
Inc., Chicago, IL, USA) was used for processing and statistical
analysis of all data. Descriptive statistics were computed for
continuous and categorical variables. The computed statistics
included mean or median and range of continuous variables,
frequencies and percentages of categorical factors. OS and DFS were
calculated and graphically presented using the Kaplan-Meier method.
Differences between curves were assessed by the Mantel’s log-rank
test for censored survival data.
All the P values resulted from two-sided statistical
tests and P<0.05 was considered to indicate a statistically
significant difference. The calculation of the median follow-up was
based on the time from the HSCT to the last follow-up for patients
who were alive and from the HSCT to June 1, 2010 as reference data
for patients who succumbed to the disease.
Results
Sequence of transplantation and
hematopoietic reconstitution
A total of 88 patients with different types of NHL
were included in the analysis of this retrospective study (Table I). Of these 88 patients, 39
received only an allogeneic graft and 47 received tandem
transplantation with ≥1 autologous grafts, followed by allogeneic
transplantation preceded by a conditioning regimen with
treosulfan/fludarabine. One of the patients received
treosulfan/fludarabine conditioning prior to both autologous and
allo-HSCT. Two patients received a second allograft due to graft
rejection. Of the 88 patients with allo-HSCT, 22 received a graft
from a matched related donor, 19 received a graft from a mismatched
unrelated donor and the majority (47/88) received a graft from a
matched unrelated donor. Further specification of the mode and
sequence of transplantations is provided in Table II on a patient-per-patient basis.
The mean number of transplanted CD34+ HSCs/kg BW of the
recipient was 6.08 (range, 1.15–16.86). Hematopoietic
reconstitution occurred in all but one patient, who experienced a
graft failure. The mean duration of neutropenia was 16.7 days
(range, 8–36 days).
 | Table IISynopsis of patient characteristics
and results. |
Table II
Synopsis of patient characteristics
and results.
| Patient no. | Age/gender | Donor type | Diagnosis | No. of
chemotherapies prior to auto-/allo-Tx | Remission status
prior to auto-/allo-Tx |
Chemo-sensivity | Response after
auto-/allo-HSCT |
aTreo/flud in allo-or
auto-Tx | No. of
CD34+ cells per kg BW | Duration of
neutropenia (days) | Survival (days
after HSCT) | DFS | Cause of death | aGvHD (overall
grading) | cGvHD |
|---|
| 1 | 57/M | MUD | MCL | 1 | PR, PR | Yes | CR/CR |
Auto/Alloa | 1.49 | 25 | 125 | 125 | Alive | 0 | No |
| 2 | 43/M | MRD | DLBCL | 1 | ER, SD | No | CR/CR |
Autoa/Allo | 3.02 | 10 | 147 | 138 | Relapse | 0 | No |
| 3 | 60/M | MUD | DLBCL | 1 | ER, CR | Yes | CR |
Alloa | 6.54 | 16 | 196 | 44 | Alive | 0 | No |
| 4 | 47/M | MUD | CLL | 3 | PD | No | CR |
Alloa | 5.06 | 15 | 386 | 210 | Alive | 2 | No |
| 5 | 49/M | MUD | CLL | 2 | R, PR | Yes | CR |
Alloa | 7.02 | 16 | 420 | 420 | Alive | 1 | No |
| 6 | 21/M | MUD | Hm T-NHL | 1 | ER, PR | Yes | PR/CR |
Auto/Alloa | 5.33 | 10 | 134 | 134 | PD, sepsis | 2 | No |
| 7 | 49/F | MRD | DLBCL | 1 | ER, PR | Yes | PD |
Auto/Alloa | 4.02 | 28 | 120 | 120 | PD | 0 | No |
| 8 | 57/M | MUD | CLL | 1 | PD | No | CR |
Alloa | 3.60 | 12 | 921 | 768 | Alive | 2 | Limited |
| 9 | 60/M | MUD | MCL | 1 | R, CR | Yes | CR |
Auto/Alloa | 3.38 | 16 | 301 | 101 | PD, sepsis | 0 | Limited |
| 10 | 53/M | MUD | Trans hm NHL | 1 | ER, PR | No | PR |
Autoa/Allo | 1.15 | 12 | 152 | 0 | PD | 3 | No |
| 11 | 51/M | MUD | MCL | 1 | ER, CR | Yes | CR |
Autoa/Alloa | 5.51 | 10 | 1165 | 1165 | Alive | 2 | Extensive |
| 12 | 54/M | MMUD | IC | 3 | ER, PD | Yes | CR |
Alloa | 7.06 | 15 | 305 | 305 | Pneumonia, MOF | 0 | Limited |
| 13 | 51/M | MRD | BL | 1 | ER, CR | Yes | PD |
Auto/Alloa | 4.26 | 17 | 69 | 0 | PD | 0 | No |
| 14 | 55/M | MRD | CLL | 1 | PR | Yes | CR |
Alloa | 3.20 | 16 | 2005 | 2005 | NSCLC | 1 | No |
| 15 | 44/f | MRD | DLBCL | 1 | ER, SD | No | CR |
Auto/Alloa | 5.13 | 20 | 1989 | 1989 | Alive | 0 | No |
| 16 | 53/M | MUD | FL | 2 | RD, PR | Yes | CR |
Alloa | 2.05 | 24 | 2042 | 2042 | Alive | 0 | No |
| 17 | 34/M | MRD | DLBCL | 1 | PD | No | PR |
Auto/Alloa | 2.14 | 15 | 93 | 0 | Sepsis→MOF | 3 | No |
| 18 | 38/F | MUD | DLBCL | 1 | R, PD | No | PD |
Auto/Alloa | 2.71 | 31 | 104 | 0 | PD | 0 | No |
| 19 | 59/M | MUD | DLBCL | 1 | R, CR | Yes | CR |
Auto/Alloa | 3.17 | 21 | 83 | 83 | Sepsis→MOF | 3 | No |
| 20 | 36/M | MRD | PTCL-NOS | 1 | PR | Yes | N.E. |
Auto/Alloa | 8.17 | 17 | 44 | 44 | Sepsis, ARDS | 0 | No |
| 21 | 36/M | MRD | FL | 2 | ER, SD | No | CR |
Auto/Alloa | 1.50 | 15 | 3071 | 395 | Alive | 1 | Extensive |
| 22 | 37/F | MRD | FL | 2 | R, CR | Yes | CR |
Auto/Alloa | 3.02 | 13 | 1934 | 1934 | AV III°→CPR | 2 | Limited |
| 23 | 61/M | MUD | CLL | 2 | SD | No | CR |
Alloa | 3.40 | 13 | 273 | 273 | ICH | 4 | No |
| 24 | 43/F | MRD | FL | 2 | R, PR | Yes | CR |
Alloa | 1.79 | 11 | 2940 | 2787 | Alive | 0 | Limited |
| 25 | 48/F | MUD | CLL | 1 | R, PR | Yes | PR |
Allo/Alloa | 2.56 | 13 | 3016 | 3016 | Alive | 0 | No |
| 26 | 40/M | MUD | FL | 1 | RD, SD | No | CR |
Alloa | 3.10 | 13 | 436 | 436 | cGvHD | 4 | Extensive |
| 27 | 57/M | MUD | CLL | 4 | PR | Yes | CR |
Alloa | 2.40 | 9 | 1615 | 1615 | cGvHD | 1 | Limited |
| 28 | 43/M | MRD | PTCL-NOS | 1 | ER, CR | Yes | CR |
Alloa | 3.10 | 10 | 88 | 88 | Sepsis, GvHD,
MOF | 3 | No |
| 29 | 52/F | MUD | FL | 1 | R, CR | Yes | CR |
Alloa | 1.43 | 10 | 3331 | 2082 | Alive | 3 | No |
| 30 | 50/F | MUD | FL | 1 | R, PR | Yes | CR |
Alloa | 15.90 | 8 | 3436 | 1764 | Alive | 0 | Limited |
| 31 | 52/M | MUD | DLBCL | 2 | CR | Yes | CR |
Auto/Alloa | 6.68 | 23 | 83 | 83 | Alive | 0 | No |
| 32 | 49/F | MUD | Trans hm NHL | 2 | CR | Yes | CR |
Auto/Alloa | 5.88 | 28 | 75 | 75 | Alive | 0 | No |
| 33 | 35/F | MRD | Hm T-NHL | 2 | PR | No | CR |
Alloa | 2.28 | 13 | 61 | 61 | Alive | 0 | No |
| 34 | 52/M | MRD | MCL | 1 | CR | Yes | CR |
Alloa | 7.40 | 12 | 1373 | 1373 | Alive | 3 | Limited |
| 35 | 49/F | MMUD | DLBCL | 3 | ER, RD | No | CR |
Alloa | 9.00 | 10 | 239 | 239 | Sepsis | 2 | Extensive |
| 36 | 35/F | MMUD | DLBCL | 2 | ER, PR | Yes | CR |
Alloa | 5.79 | 26 | 249 | 128 | Sepsis, PD | 0 | No |
| 37 | 63/M | MUD | MCL | 4 | ER, PR | Yes | CR |
Alloa | 5.90 | 8 | 394 | 394 | GvHD | 2 | Extensive |
| 38 | 56/F | MUD | Hm T-NHL | 2 | R, PR | Yes | N.E. |
Alloa | 5.00 | 34 | 46 | 46 | MOF | 2 | No |
| 39 | 41/F | MUD | DLBCL | 3 | R, PR | Yes | CR |
Alloa | 4.20 | 31 | 754 | 754 | Alive | 0 | No |
| 40 | 42/F | MUD | DLBCL | 3 | ER, RD | No | N.E. |
Auto/Alloa | 6.13 | NA | 26 | 26 | MOF | 0 | No |
| 41 | 27/F | MUD | BL | 5 | ER, PR | Yes | CR |
Auto/Alloa | 7.13 | 16 | 636 | 636 | Alive | 0 | Limited |
| 42 | 51/M | MRD | DLBCL | 3 | ER, RD | No | CR |
Auto/Alloa | 7.25 | 22 | 548 | 395 | Alive | 0 | Limited |
| 43 | 50/M | MRD | Trans hm NHL | 3 | R, PR | Yes | CR |
Alloa | 7.80 | 12 | 205 | 205 | Alive | 3 | No |
| 44 | 62/F | MMUD | CLL | 1 | R, CR | Yes | CR |
Allo/Alloa | 5.38 | 18 | 2161 | 2161 | Alive | 0 | Limited |
| 45 | 47/M | MMUD | CLL | 3 | R, PD | Yes | CR |
Alloa | 3.48 | 15 | 1640 | 1640 | Alive | 3 | No |
| 46 | 60/F | MMUD | CLL | 2 | PD | Yes | PR |
Auto/Alloa | 3.23 | 18 | 684 | 684 | Alive | 2 | Extensive |
| 47 | 47/M | MUD | CLL | 3 | R, PR | Yes | CR |
Auto/Allo/Alloa | 6.68 | 16 | 1387 | 333 | Alive | 1 | No |
| 48 | 58/M | MUD | CLL | 2 | R, PR | Yes | CR |
Auto/Alloa | 9.86 | 15 | 1311 | 1311 | Alive | 1 | Limited |
| 49 | 64/F | MUD | CLL | 2 | R, PD | No | CR |
Alloa | 11.50 | 19 | 1142 | 1142 | Alive | 2 | Limited |
| 50 | 45/M | MMUD | CLL | 2 | R, PR | Yes | CR |
Alloa | 4.50 | 16 | 64 | 64 | Sepsis, MOF | 4 | No |
| 51 | 46/M | MUD | CLL | 2 | R, CR | Yes | CR |
Alloa | 5.75 | 16 | 813 | 813 | Alive | 2 | Extensive |
| 52 | 64/M | MMUD | CLL | 2 | R, PR | Yes | CR (MRD+) |
Alloa | 5.33 | 18 | 567 | 567 | Alive | 3 | Extensive |
| 53 | 56/F | MUD | CLL | 2 | R, PD | No | SD |
Alloa | 7.30 | 21 | 106 | 106 | Sepsis, MOF | 4 | Extensive |
| 54 | 57/M | MUD | CLL | 2 | R, PR | Yes | CR |
Alloa | 1.99 | 15 | 512 | 512 | Alive | 0 | Limited |
| 55 | 55/M | MRD | Trans hm NHL | 4 | R, PR | Yes | CR |
Alloa | 5.90 | 17 | 312 | 312 | Sepsis | 1 | No |
| 56 | 53/F | MMUD | CLL | 2 | R, PD | No | PR |
Alloa | 9.01 | 18 | 178 | 178 | Pneumonia, MOF | 1 | Limited |
| 57 | 59/M | MUD | CLL | 3 | R, CR | Yes | CR |
Auto/Alloa | 2.90 | 18 | 73 | 73 | GvHD | 4 | No |
| 58 | 57/M | MRD | CLL | 1 | R, PR | Yes | CR |
Alloa | 6.86 | 15 | 169 | 169 | Sepsis,
pneumonia | 0 | Extensive |
| 59 | 52/M | MMUD | CLL | 1 | ER, CR | Yes | CR |
Alloa | 16.86 | 18 | 288 | 288 | Alive | 3 | No |
| 60 | 43/M | MUD | Trans hm NHL | 3 | R, CR | Yes | CR |
Auto/Alloa | 6.95 | 16 | 735 | 181 | Relapse | 0 | No |
| 61 | 26/M | MRD | DLBCL | 7 | R, PR | Yes | SD | 3×
Auto/Alloa | 5.80 | 18 | 61 | 30 | Relapse | 2 | No |
| 62 | 37/F | MMUD | Hm T-NHL | 4 | R, SD | Yes | N.E. |
Auto/Alloa | 5.86 | 17 | 48 | 48 | Sepsis | 0 | No |
| 63 | 29/F | MUD | PMLBL | 2 | R, PR | Yes | CR |
Auto/Alloa | 7.48 | 16 | 452 | 452 | GvHD, sepsis | 1 | Extensive |
| 64 | 46/M | MUD | DLBCL | 6 | R, PR | Yes | N.E. | 2×
Auto/Alloa | 10.64 | N.A. | 2 | 2 | Sepsis | 0 | No |
| 65 | 45/M | MRD | MCL | 4 | R, PR | Yes | CR |
Auto/Alloa | 2.80 | 19 | 1406 | 551 | Pneumonia | 1 | No |
| 66 | 25/F | MMUD | DLBCL | 4 | R, PR | Yes | PR |
Auto/Allo/Alloa | 7.10 | 14 | 206 | 24 | Relapse | 0 | No |
| 67 | 36/F | MMUD | ALCL,
ALK+ | 4 | R, CR | Yes | CR |
Auto/Alloa | 3.30 | 17 | 1955 | 1955 | Alive | 1 | Limited |
| 68 | 54/M | MRD | DLBCL | 2 | R, PR | Yes | CR | 4×
Auto/Alloa | 6.60 | 17 | 1899 | 1899 | Alive | 2 | Limited |
| 69 | 46/M | MMUD | PMLBL | 3 | R, PR | Yes | CR | 3×
Auto/Alloa | 7.60 | 15 | 166 | 166 | Pneumonia | 4 | No |
| 70 | 48/F | MRD | ALCL,
ALK+ | 3 | R, CR | Yes | CR |
Auto/Alloa | 11.90 | 11 | 225 | 171 | Relapse | 0 | No |
| 71 | 62/F | MMUD | DLBCL | 7 | R, PR | Yes | CR |
Auto/Alloa | 9.29 | 12 | 102 | 102 | Sepsis, MOF | 1 | No |
| 72 | 45/M | MMUD | CLL | 3 | R, PR | Yes | CR |
Auto/Allo/Alloa | 13.00 | 15 | 1366 | 1366 | Alive | 3 | Limited |
| 73 | 42/F | MUD | Trans hm NHL | 3 | R, PR | Yes | PR |
Auto/Alloa | 10.90 | 17 | 268 | 100 | Relapse | 0 | Limited |
| 74 | 53/F | MMUD | Trans hm NHL | 3 | R, PR | Yes | CR |
Alloa | 9.96 | 22 | 918 | 918 | Alive | 0 | No |
| 75 | 57/F | MUD | MCL | 4 | R, CR | Yes | CR | 2×
Auto/Alloa | 12.56 | 21 | 120 | 120 | Pneumonia | 2 | No |
| 76 | 55/F | MRD | PTCL-NOS | 3 | R, CR | Yes | CR |
Auto/Alloa | 6.30 | 22 | 877 | 877 | Alive | 1 | Limited |
| 77 | 71/M | MUD | MCL | 7 | R, PR | Yes | N.E. |
Alloa | 5.56 | 14 | 48 | 48 | Sepsis, MOF | 2 | No |
| 78 | 59/M | MUD | Trans hm NHL | 5 | R, PR | Yes | CR |
Alloa | 4.07 | 18 | 797 | 797 | Alive | 2 | Limited |
| 79 | 70/M | MUD | Trans hm NHL | 4 | R, SD | No | N.E. |
Alloa | 5.94 | 14 | 58 | 58 | Sepsis | 3 | No |
| 80 | 55/M | MMUD | DLBCL | 3 | R, CR | Yes | CR |
Auto/Alloa | 7.60 | 36 | 463 | 463 | Alive | 0 | No |
| 81 | 57/M | MUD | Trans hm NHL | 6 | R, PR | Yes | CR | 4×
Auto/Alloa | 2.60 | 15 | 365 | 365 | Alive | 3 | Extensive |
| 82 | 55/F | MUD | DLBCL | 4 | R, CR | Yes | CR |
Auto/Alloa | 16.50 | 17 | 68 | 68 | HF | 0 | No |
| 83 | 62/F | MUD | DLBCL | 3 | R, PR | Yes | CR |
Auto/Alloa | 5.00 | 16 | 317 | 317 | Alive | 1 | No |
| 84 | 42/F | MUD | DLBCL | 2 | R, CR | Yes | CR |
Auto/Alloa | 9.32 | 13 | 264 | 264 | Alive | 0 | No |
| 85 | 57/M | MMUD | Trans hm NHL | 4 | R, PR | Yes | CR |
Auto/Alloa | 7.10 | 14 | 82 | 82 | Renal failure,
sepsis | 3 | No |
| 86 | 68/M | MUD | PTCL-NOS | 3 | R, CR | Yes | CR |
Auto/Alloa | 5.98 | 15 | 245 | 245 | Alive | 1 | No |
| 87 | 58/F | MUD | T-PLL | 3 | R, CR | Yes | CR |
Alloa | 6.89 | 15 | 947 | 947 | Alive | 2 | Limited |
| 88 | 52/F | MUD | T-PLL | 2 | R, CR | Yes | CR |
Alloa | 11.05 | 14 | 185 | 136 | Relapse | 0 | Extensive |
Response to treatment and survival
The results patient-per-patient are presented in
Table II. In general, the
majority of the patients maintained or developed a complete
remission (CR). In 69 of the 88 patients, a CR was observed
post-transplantation, 7 patients achieved or maintained a partial
remission (PR) and 3 patients developed progressive disease (PD).
Prior to allo-HSCT, 69 of the 88 patients (78.4%) were in CR and
PR, but only 29 of these were in CR. Notably, 5 of the 7 patients
with stable disease (SD) prior to allo-HSCT achieved a CR after
allo-HSCT. Of the 12 patients with PD prior to allo-HSCT, 9
achieved a remission (6 CR and 3 PR). Of note, 1 patient with PD
achieved a CR following administration of a donor lymphocyte
infusion. Seven patients died within 60 days of the transplant and
were therefore not evaluable for response to treatment (Table III).
 | Table IIISummary of results after
allo-HSCT. |
Table III
Summary of results after
allo-HSCT.
| Outcome | Patient no. |
|---|
| Response to
treatment (n=88) |
| CR | 69 |
| PR | 7 |
| PDa | 3 |
| SD | 2 |
| NEb | 7 |
| Causes of death
(n=45) |
| Disease
progression | 4 |
| Disease progression
and infectious complications | 3 |
| Infection, sepsis,
MOF without progression | 22 |
| GvHD | 4 |
| Relapse | 7 |
| Other causes of
death |
| Intracranial
bleeding | 1 (d +273 in
CR) |
| NSCLC | 1 (d +2,005 in
CR) |
| AV III°, CPR | 1 (d +1,943 in
CR) |
| Heart failure | 1 (d +68 in
CR) |
| Renal failure | 1 (d +82 in
CR) |
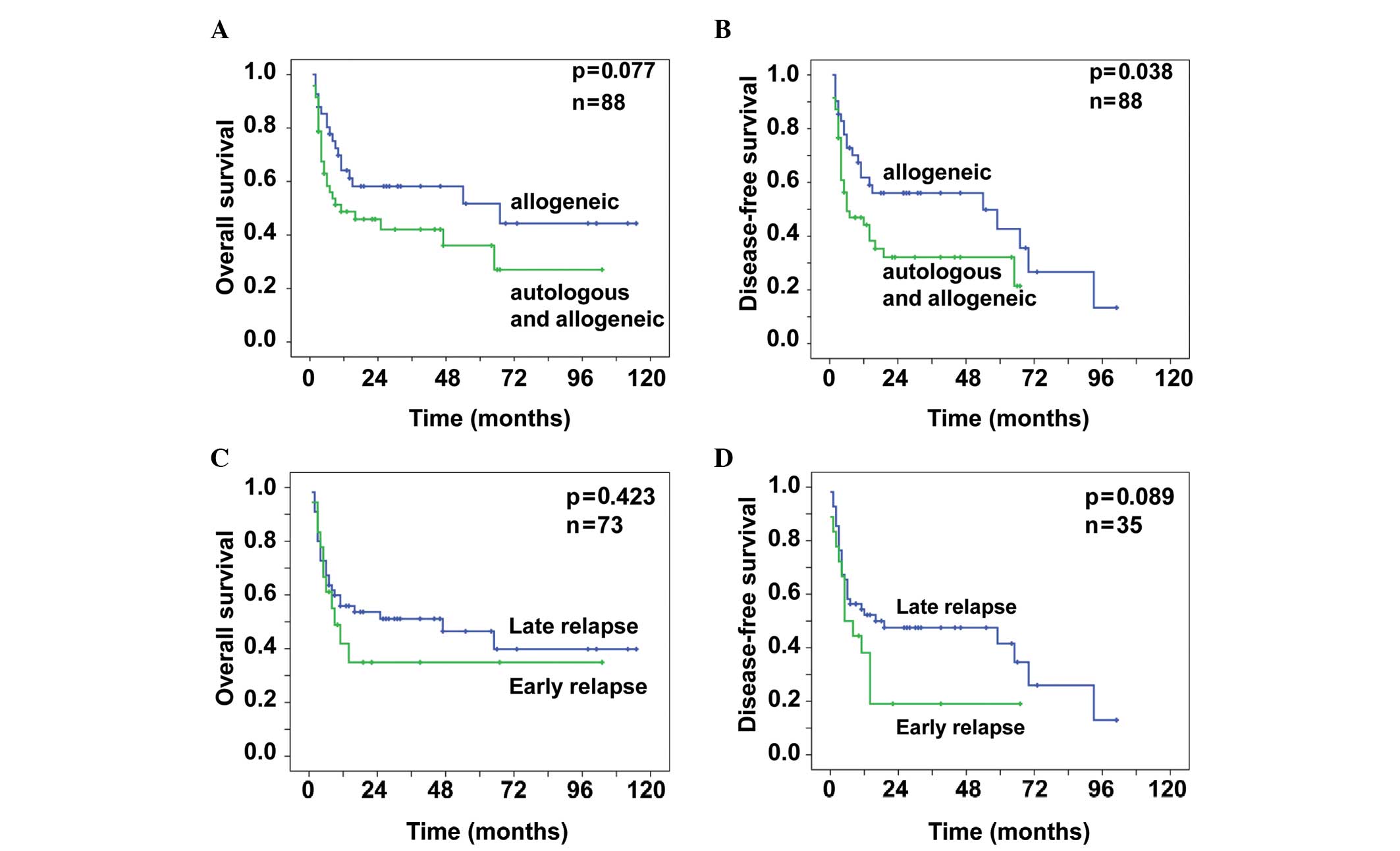
The patients who directly underwent allo-HSCT
without preceding auto-HSCT had an OS probability of 0.58±0.08
after 3 years and 0.44±0.11 after 7 years (Fig. 1A). For these patients, the
probability of DFS was 0.56±0.08 after 3 years and 0.27±0.11 after
7 years (Fig. 1B). For the
patients who received allo-HSCT following an autologous graft, the
OS probability was 0.42±0.08 after 3 years. After 7 years,
0.27±0.10 of these patients remained alive (Fig. 1A) and the probability of DFS was
0.32±0.08 after 3 years (Fig. 1B).
The difference in the DFS in favor of the patients who directly
received an allogeneic graft was significant (P=0.038), with a
similar tendency for OS (P=0.077).
Of the 88 patients, 45 succumbed to the disease. Of
these 45 patients, 14 died due to progression or relapse of the
underlying disease, 4 experienced progression following
transplantation and 3 developed infectious complications. A total
of 26 patients succumbed to transplantation-associated
complications, 22 of whom developed infectious complications,
followed by sepsis and multi-organ failure. Four patients died from
acute GvHD. Five patients died while in CR, 3 of which during
long-term follow-up, due to disease- or treatment-independent
reasons: 1 patient died from intracranial bleeding on day +273; 1
patient developed non-small-cell lung cancer and died on day +2,005
following transplantation; 1 patient died on day +1,934 due to a
cardiac arrest, despite cardiopulmonary resuscitation; 1 patient
died on day +68 due to heart failure; and 1 patient died due to
renal failure on day +82.
Relapse
Patients with ER, i.e., relapse within 6 months
following the completion of chemotherapy, had a worse outcome
compared with patients who exhibited a later relapse. Notably,
there was no significant difference in the probability of OS
(P=0.423). After 3 and 7 years, 0.51±0.07 and 0.40±0.09 of the
relapsed patients, respectively, remained alive. The probability of
OS of the patients who relapsed within the first 6 months was
0.35±0.12 after 3 and 7 years (Fig.
1C).
The difference in the DFS displayed a tendency in
favor of patients with late relapse (P=0.089). The probability of
DFS was 0.48±0.07 and 0.26±0.10 after 3 and 7 years, respectively,
for those patients. Patients with ER had a probability of DFS of
0.19±0.10 after 3 years (Fig.
1D).
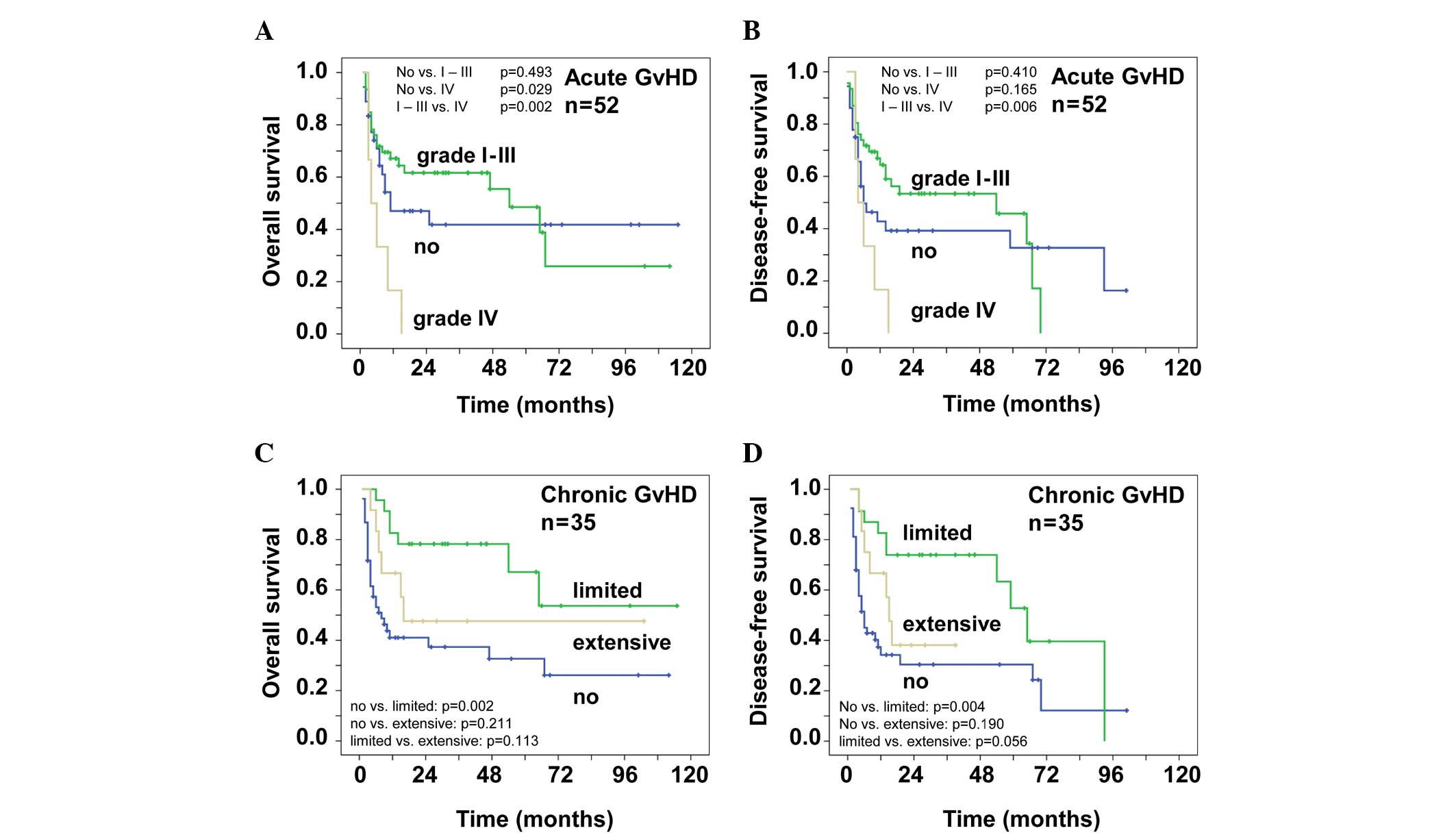
GvHD
Of the 88 patients included in this analysis, 52
patients experienced acute GvHD. Fifteen patients developed acute
GvHD grade I, 17 patients grade II, 14 patients grade III and 6
patients grade IV. Table IV
specifies the organ manifestations of acute GvHD. GvHD of the gut
was not histologically proven. Fig.
2A shows the OS of patients with acute GvHD. Patients with
grade IV acute GvHD succumbed to the disease within the first 15
months. The probability of OS for patients without acute GvHD
reached an early plateau: 0.42±0.09 after 3 and 7 years. Patients
with grade I–III acute GvHD had a probability of OS of 0.62±0.07
after 3 years and 0.26±0.13 after 7 years. The difference between
grade IV acute GvHD vs. no GvHD and grade I–III acute GvHD was
highly significant (P=0.029 and P=0.002, respectively). Similar
results were observed for the probability of DFS (Fig. 2B). After 3 years 0.53±0.08 of the
patients with grade I–III acute GvHD were disease-free. The
patients that did not develop acute GvHD had a probability of DFS
of 0.39±0.09 and 0.33±0.09 after 3 and 7 years, respectively.
 | Table IVAcute GvHD (n=52). |
Table IV
Acute GvHD (n=52).
| Grade | Skin | Gut | Liver | Overall
assessment |
|---|
| I | 9 | 12 | 4 | 15 |
| II | 20 | 6 | 4 | 17 |
| III | 14 | 6 | 2 | 14 |
| IV | 1 | 5 | 3 | 6 |
| All | 44 | 29 | 13 | 52 |
The occurrence of cGvHD correlated with the survival
of the NHL patients included in this study. A total of 35 patients
developed cGvHD, 13 of whom developed extensive and 22 patients
limited disease, mainly involving the skin and mucosae. Fig. 2C shows a better OS in patients with
cGvHD. The probability of OS of patients with limited and no cGvHD
was 0.78±0.09 and 0.37±0.08, respectively, after 3 years. After 7
years, the probability of OS was 0.54±0.16 for patients with
limited GvHD and 0.26±0.09 for patients without cGvHD. The patients
with extensive cGvHD reached a plateau early, so that the
probability of OS was 0.48±0.15 after 3 and 7 years. There was a
highly significant difference between limited and no cGvHD
(P=0.002) and a tendency for a better OS in patients with limited
or no vs. extensive GvHD (P=0.113 or 0.211, respectively). These
effects are also shown in Fig. 2D
that demonstrates the time of DFS. After 3 years, 0.74±0.09 of the
patients with limited cGvHD were disease-free. The data of patients
with limited cGvHD were highly significant when compared with those
of patients with no cGvHD (P=0.004), whereas limited vs. extensive
cGvHD showed a tendency for improved survival (P=0.056). The
probability of DFS was 0.30±0.07 after 3 years and 0.12±0.10 after
7 years for patients that did not develop cGvHD. After 3 years, the
probability of OS was 0.38±0.15 for patients with extensive chronic
CGvHD.
Discussion
The treatment of patients with refractory or
relapsed NHL remains challenging, as only few salvage chemotherapy
protocols are currently available. El Gnaoui et al (14) reported the outcome of 46 patients
treated with a salvage therapy containing rituximab, gemcitabine
and oxaliplatine. The overall response rate was 83% and the 2-year
event-free survival (EFS) and OS were 43 and 65% respectively
(14). The majority of these
patients had chemotherapy-sensitive disease and a remission of ≥1
year; however, only 57% had received rituximab prior to salvage
therapy (14). In a recently
published study, Gisselbrecht et al (4) established the International
Prognostic Index, the duration of remission (<12 vs. >12
months) and the pre-treatment with rituximab as risk factors for
the outcome following autologous HSCT. In that study, 396 patients
were randomly assigned to receive either R-ICE or R-DHAP as
induction therapy, following high-dose BEAM and autologous HSCT.
With regard to the response rate, there was no difference in the
3-year OS (49%) and the 3-year EFS (31%) between the treatment
protocols. Martin et al (15) described a significantly worse
relapse rate (RR), OS and progression-free survival (PFS) in
patients with relapsed NHL after rituximab-containing first-line
therapy. Since the majority of patients currently receive a
rituximab-based therapy, this is of particular interest, as the
group of rituximab-naïve patients experiencing a relapse of
high-grade lymphoma may constitute a minority in the future.
In contrast to autologous HSCT, allo-HSCT
constitutes the only curative therapy option for patients with
aggressive NHL (16–18), mainly due to the GvL effect. The
use of RIC extended the option of allo-HSCT to elderly patients and
patients who had previously received high-dose chemotherapy and
autologous HSCT (19–22). Several studies demonstrated a more
potent GvL effect after RIC rather than after myeloablative
condition regimens (23–26). This may be due to the lower
toxicity towards T cells, which are mainly responsible for the GvL
effect.
Treosulfan as an alkylating agent has exhibited
limited organ toxicities, even when administered at the maximum
dose of 47 g/m2 (27,28).
Compared to its prodrug, busulfan, treosulfan may be less toxic,
particularly for the skin, mucosae, liver, kidney and heart, which
are the organ systems usually targeted in
transplantation-associated mortality (TAM) following conventional
conditioning. Fludarabine, a nucleoside analogue which has already
been included in a variety of RIC regimens, is characterized by its
effectiveness against lymphoid diseases and its favorable toxicity
profile (29–31). Therefore, we employed the
reduced-intensity regimen with treosulfan and fludarabine in 88
patients with relapsed or refractory lymphoma.
In our present study, for patients who received
autologous and allo-HSCT, the OS and the DFS were inferior compared
to those in patients who only underwent allo-HSCT (Fig. 1A and B). This may be due to the
fact that patients with more agressive NHLs achieved a PR only
after salvage chemotherapy and were first subjected to autologous
HSCT for further reduction of the tumor burden. Furthermore,
autologous HSCT preceding the allograft may have caused organ
toxicities without eradicating the aggressive disease. Therefore,
provided that the patient is eligible, allo-HSCT should be
considered and performed early during the course of the disease. We
demonstrated that GvHD, in particular limited cGvHD, improved the
patient outcome (Fig. 2). However,
we did not observe a difference in the outcome of patients with
early or late disease relapse (Fig. 1C
and D). This finding may indicate that allo-HSCT should be
considered even for patients with ER, particulary if they have
responded to salvage chemotherapy. Of the 88 patients, 26 (29.5%)
succumbed to GvHD and/or infectious complications, i.e., TAM was
within the expected range.
A previous study by Hamadani et al (6) was conducted on a cohort of 46
patients with relapsed chemorefractory aggressive NHL. In contrast
to our cohort, those patients were treated with a myeloablative
regimen (84% of the patients received busulfan and
cyclophosphamide). The median follow-up was 5 years. The 5-year OS,
PFS and RR were 38, 34 and 35%, respectively. The data of our
cohort demonstrated an OS and a DFS of 43 and 37%, respectively.
The rate of acute and chronic GvHD was 43 and 75% in the study by
Hamadani et al (6) vs. 59
and 40% in our study.
The Lymphoma Working Party of the European Bone
Marrow Transplantation Association reported the outcome of 188
lymphoma patients who underwent allo-HSCT after RIC. Twenty-one of
these patients had chemotherapy-resistant disease. The sensitivity
to chemotherapy was the most important factor in PFS (32). In addition, a previous study by
Bishop et al (5)
demonstrated the correlation of pre-transplantation and early
post-transplantation response assessment with the outcome after RIC
allo-HSCT for NHL. Fig. 1C and D
demonstrates that there was no significant difference in our study
between patients who relapsed within the first 6 months and those
who relapsed at any time. This may be due to the fact that there
were fewer patients with ER (Table
I). In the present study we also observed that patients with
good sensitivity to chemotherapy (70/88) exhibited a better
survival compared to patients without response to chemotherapy
(Table II).
Our findings suggest that RIC with
treosulfan/fludarabine and allo-HSCT is feasible and effective in
NHL patients, even those with ER and at the stage of SD or PD. The
reduction of the tumor load to a minimum appears to be crucial. The
occurrence of GvHD is favourable for the outcome of the patients,
suggesting a potent GvL effect. This therapeutic option should
therefore be considered early during the course of the disease and
integrated into the long-run concept of lymphoma therapy.
Acknowledgements
Michael Schmitt, Inken Hilgendorf, Michael
Koenigsmann, Jochen Casper and Dietrich W. Beelen received travel
grants to conferences from Medac GmbH. Mathias Freund received
research funding and honoraria from Medac GmbH.
References
|
1
|
Verdonck LF, van Putten WL, Hagenbeek A,
et al: Comparison of CHOP chemotherapy with autologous bone marrow
transplantation for slowly responding patients with aggressive
non-Hodgkin’s lymphoma. N Engl J Med. 332:1045–1051.
1995.PubMed/NCBI
|
|
2
|
Chen AI, McMillan A, Negrin RS, et al:
Long-term results of autologous hematopoietic cell transplantation
for peripheral T cell lymphoma: the Stanford experience. Biol Blood
Marrow Transplant. 14:741–747. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hamadani M, Benson DM Jr, Lin TS, et al:
High-dose therapy and autologous stem cell transplantation for
follicular lymphoma undergoing transformation to diffuse large
B-cell lymphoma. Eur J Haematol. 81:425–431. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koenigsmann M, Casper J, Kahl C, et al:
Risk-adapted, treosulfan-based therapy with auto- and allo-SCT for
relapsed/refractory aggressive NHL: a prospective phase-II trial.
Bone Marrow Transplant. 49:410–415. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bishop MR, Dean RM, Steinberg SM, et al:
Correlation of pretransplant and early post-transplant response
assessment with outcomes after reduced-intensity allogeneic
hematopoietic stem cell transplantation for non-Hodgkin’s lymphoma.
Cancer. 116:852–862. 2010.PubMed/NCBI
|
|
6
|
Hamadani M, Benson DM Jr, Hofmeister CC,
et al: Allogeneic stem cell transplantation for patients with
relapsed chemorefractory aggressive non-Hodgkin lymphomas. Biol
Blood Marrow Transplant. 15:547–553. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Casper J, Knauf W, Kiefer T, et al:
Treosulfan and fludarabine: a new toxicity-reduced conditioning
regimen for allogeneic hematopoietic stem cell transplantation.
Blood. 103:725–731. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schmidt-Hieber M, Blau IW, Trenschel R, et
al: Reduced-toxicity conditioning with fludarabine and treosulfan
prior to allogeneic stem cell transplantation in multiple myeloma.
Bone Marrow Transplant. 39:389–396. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Casper J, Wolff D, Knauf W, et al:
Allogeneic hematopoietic stem-cell transplantation in patients with
hematologic malignancies after dose-escalated
treosulfan/fludarabine conditioning. J Clin Oncol. 28:3344–3351.
2010. View Article : Google Scholar
|
|
10
|
Hilgendorf I, Wolff D, Gromke T, et al:
Retrospective analysis of treosulfan-based conditioning in
comparison with standard conditioning in patients with
myelodysplastic syndrome. Bone Marrow Transplant. 46:502–509. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cheson BD, Horning SJ, Coiffier B, et al:
Report of an international workshop to standardize response
criteria for non-Hodgkin’s lymphomas. NCI Sponsored International
Working Group. J Clin Oncol. 17:12441999.PubMed/NCBI
|
|
12
|
Cutler C and Antin JH: Manifestations and
treatment of acute graft-versus-host disease. Thomas’ Hematopoetic
Cell Transplantation. Appelbaum FR, Forman SJ, Negrin RS and Blume
KG: 4th edition. Willey-Blackwell; London: pp. 1287–1303. 2009
|
|
13
|
Lee SJ, Vogelsang G and Flowers ME:
Chronic graft-versus-host disease. Biol Blood Marrow Transplant.
9:215–233. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
El Gnaoui T, Dupuis J, Belhadj K, et al:
Rituximab, gemcitabine and oxaliplatin: an effective salvage
regimen for patients with relapsed or refractory B-cell lymphoma
not candidates for high-dose therapy. Ann Oncol. 18:1363–1368.
2007.PubMed/NCBI
|
|
15
|
Martin A, Conde E, Arnan M, et al;
GEL/TAMO Cooperative Group. R-ESHAP as salvage therapy for patients
with relapsed or refractory diffuse large B-cell lymphoma: the
influence of prior exposure to rituximab on outcome. A GEL/TAMO
study. Haematologica. 93:1829–1836. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Le Gouill S, Milpied N, Buzyn A, et al:
Société Française de Greffe de Moëlle et de Thérapie Cellulaire:
Graft-versus-lymphoma effect for aggressive T-cell lymphomas in
adults: a study by the Societé Française de Greffe de Moëlle et de
Thérapie Cellulaire. J Clin Oncol. 26:2264–2271. 2008.
|
|
17
|
Khouri IF, McLaughlin P, Saliba RM, et al:
Eight-year experience with allogeneic stem cell transplantation for
relapsed follicular lymphoma after nonmyeloablative conditioning
with fludarabine, cyclophosphamide, and rituximab. Blood.
111:5530–5536. 2008.
|
|
18
|
Dietrich S, Tielesch B, Rieger M, et al:
Patterns and outcome of relapse after autologous stem cell
transplantation for mantle cell lymphoma. Cancer. 117:1901–1910.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chopra R, Goldstone AH, Pearce R, et al:
Autologous versus allogeneic bone marrow transplantation for
non-Hodgkin’s lymphoma: a case-controlled analysis of the European
Bone Marrow Transplant Group Registry data. J Clin Oncol.
10:1690–1695. 1992.
|
|
20
|
Peniket AJ, Ruiz de Elvira MC, Taghipour
G, et al: European Bone Marrow Transplantation (EBMT) Lymphoma
Registry: An EBMT registry matched study of allogeneic stem cell
transplants for lymphoma: allogeneic transplantation is associated
with a lower relapse rate but a higher procedure-related mortality
rate than autologous transplantation. Bone Marrow Transplant.
31:667–678. 2003.
|
|
21
|
Bierman PJ, Sweetenham JW, Loberiza FR, et
al: Lymphoma Working Committee of the International Bone Marrow
Transplant Registry and the European Group for Blood and Marrow
Transplantation: Syngeneic hematopoietic stem-cell transplantation
for non-Hodgkin’s lymphoma: a comparison with allogeneic and
autologous transplantation - The Lymphoma Working Committee of the
International Bone Marrow Transplant Registry and the European
Group for Blood and Marrow Transplantation. J Clin Oncol.
21:3744–3753. 2003.PubMed/NCBI
|
|
22
|
McSweeney PA, Niederweiser D, Shizuru JA,
et al: Hemapoietic cell transplantation in older patients with
hematologic malignancies: replacing high-dose cytotoxic therapy
with graft-versus-tumor effects. Blood. 97:3390–3400. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Khouri IF, Saliba RM, Giralt SA, et al:
Nonablative allogeneic hematopoietic transplantation as adoptive
immunotherapy for indolent lymphoma: low incidence of toxicity,
acute graft-versus-host disease, and treatment-related mortality.
Blood. 98:3595–3599. 2001. View Article : Google Scholar
|
|
24
|
Escalon MP, Champlin RE, Saliba RM, et al:
Nonmyeloablative allogeneic hematopoietic transplantation: a
promising salvage therapy for patients with non-Hodgkin’s lymphoma
whose disease has failed a prior autologous transplantation. J Clin
Oncol. 22:2419–2423. 2004.PubMed/NCBI
|
|
25
|
Rezvani AR, Storer B, Maris M, et al:
Nonmyeloablative allogeneic hematopoietic cell transplantation in
relapsed, refractory, and transformed indolent non-Hodgkin’s
lymphoma. J Clin Oncol. 26:211–217. 2008.PubMed/NCBI
|
|
26
|
Glass B, Nickelsen M, Dreger P, et al:
Reduced-intensity conditioning prior to allogeneic transplantation
of hematopoietic stem cells: the need for T cells early after
transplantation to induce a graft-versus-lymphoma effect. Bone
Marrow Transplant. 34:391–397. 2004. View Article : Google Scholar
|
|
27
|
Beelen DW, Trenschel R, Casper J, et al:
Dose-escalated treosulphan in combination with cyclophosphamide as
a new preparative regimen for allogeneic hematopoietic stem cell
transplantation in patients with an increased risk for
regimen-related complications. Bone Marrow Transplant. 35:233–241.
2005. View Article : Google Scholar
|
|
28
|
Scheulen ME, Hilger RA, Oberhoff C, et al:
Clinical phase I dose escalation and pharmacokinetic study of
high-dose chemotherapy with treosulfan and autologous peripheral
blood stem cell transplantation in patients with advanced
malignancies. Clin Cancer Res. 6:4209–4216. 2000.
|
|
29
|
Banna GL, Aversa S, Sileni VC, et al:
Nonmyeloablative allogeneic stem cell transplantation (NST) after
truly nonmyeloablative and reduced intensity conditioning regimens.
Crit Rev Oncol Hematol. 51:171–189. 2004. View Article : Google Scholar
|
|
30
|
Schetelig J, Bornhauser M, Kiehl M, et al:
Reduced-intensity conditioning with busulfan and fludarabine with
or without antithymocyte globulin in HLA-identical sibling
tranplantation - a retrospective analysis. Bone Marrow Transplant.
33:483–490. 2004. View Article : Google Scholar
|
|
31
|
Slavin S, Nagler A, Naparstek E, et al:
Nonmyeloablative stem cell transplantation and cell therapy as an
alternative to conventional bone marrow transplantation with lethal
cytoreduction for the treatment of malignant and nonmalignant
hematologic diseases. Blood. 91:756–763. 1998.
|
|
32
|
Robinson SP, Goldstone AH, Mackinnon S, et
al: Lymphoma Working Party of the European Group for Blood and Bone
Marrow Transplantation: Chemoresistant or aggressive lymphoma
predicts for a poor outcome following reduced-intensity allogeneic
progenitor cell transplantation: an analysis from the Lymphoma
Working Party of the European Group for Blood and Bone Marrow
Transplantation. Blood. 100:4310–4316. 2002.
|