Introduction
Lymphomas constitute a group of blood cell tumors
that develop from lymphatic cells (1). There are numerous subtypes of lymphomas
(2), with the two main categories
being Hodgkin's lymphoma (HL) and non-Hodgkin lymphomas (NHLs)
(3). Approximately 90% of lymphomas
are NHLs, with diffuse large B-cell lymphoma (DLBCL) being the most
common type (3).
DLBCL occurs primarily in older individuals, with a
median age at diagnosis of ~70 years (4), although it may also occur in children
and young adults in rare cases (5).
DLBCL is an aggressive tumor, which may arise in virtually any part
of the body (6). Extranodal NHL
occurring primarily in the epiglottis is extremely rare, accounting
for merely 0.7% of all NHLs and 1% of malignant laryngeal tumors
(7). We herein present a rare case of
DLBCL involving the epiglottis.
Case report
A 55-year-old previously healthy man presented with
complaints of dysphagia and throat soreness for 2 months. The
patient did not have a history of fever, night sweats, body weight
loss or fatigue. On examination of the neck, no palpable mass was
detected and the overlying skin was not erythematous or warm to the
touch. On intraoral examination, there were no specific findings.
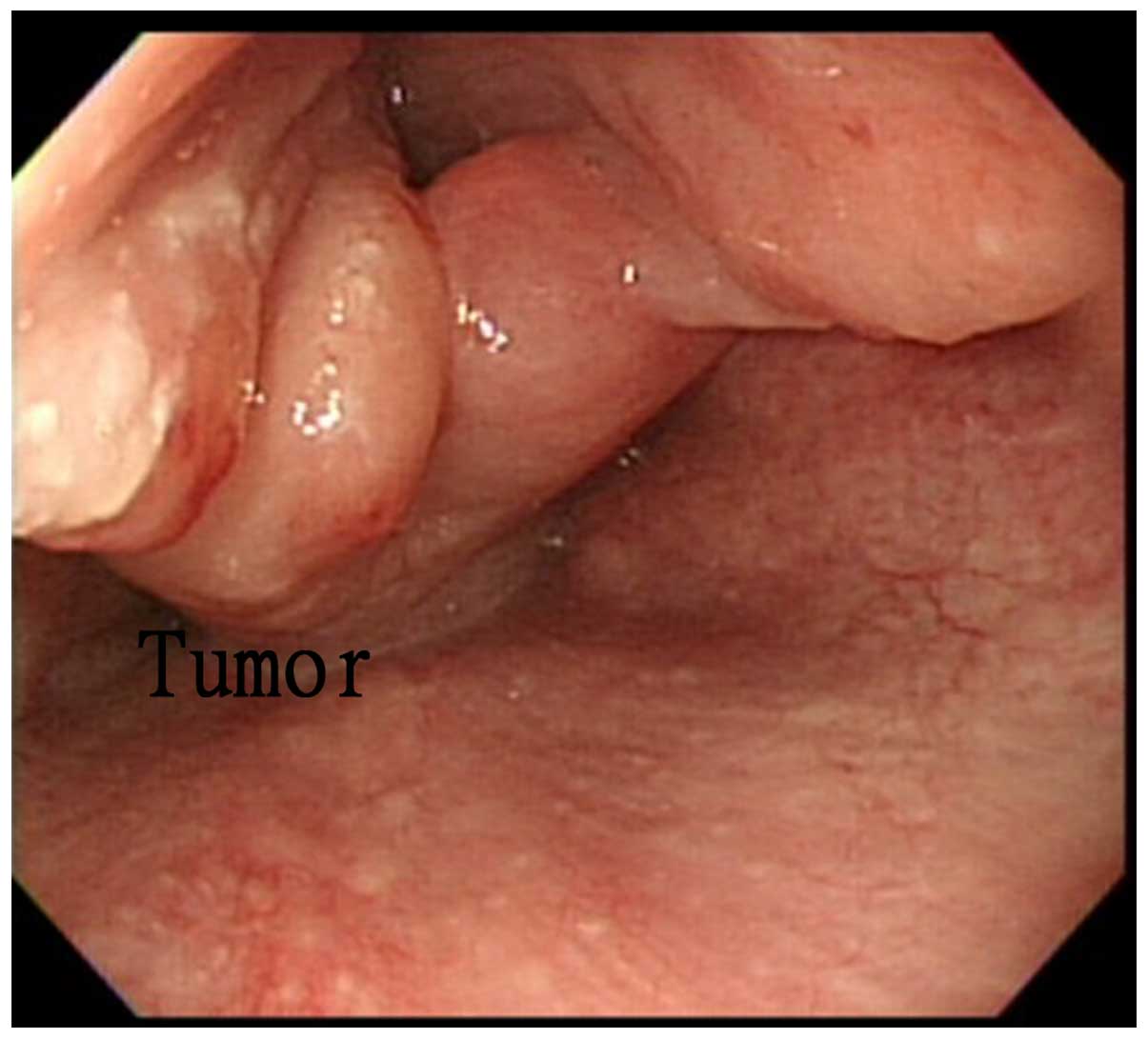
Video laryngoscopy revealed a left epiglottic tumor with an
irregular surface (Fig. 1). The
hematological tests were normal, apart from increased erythrocyte
sedimentation rate. Blood smear examination revealed no evidence of
blast cells. The renal and liver function tests were normal and the
patient was HIV-negative.
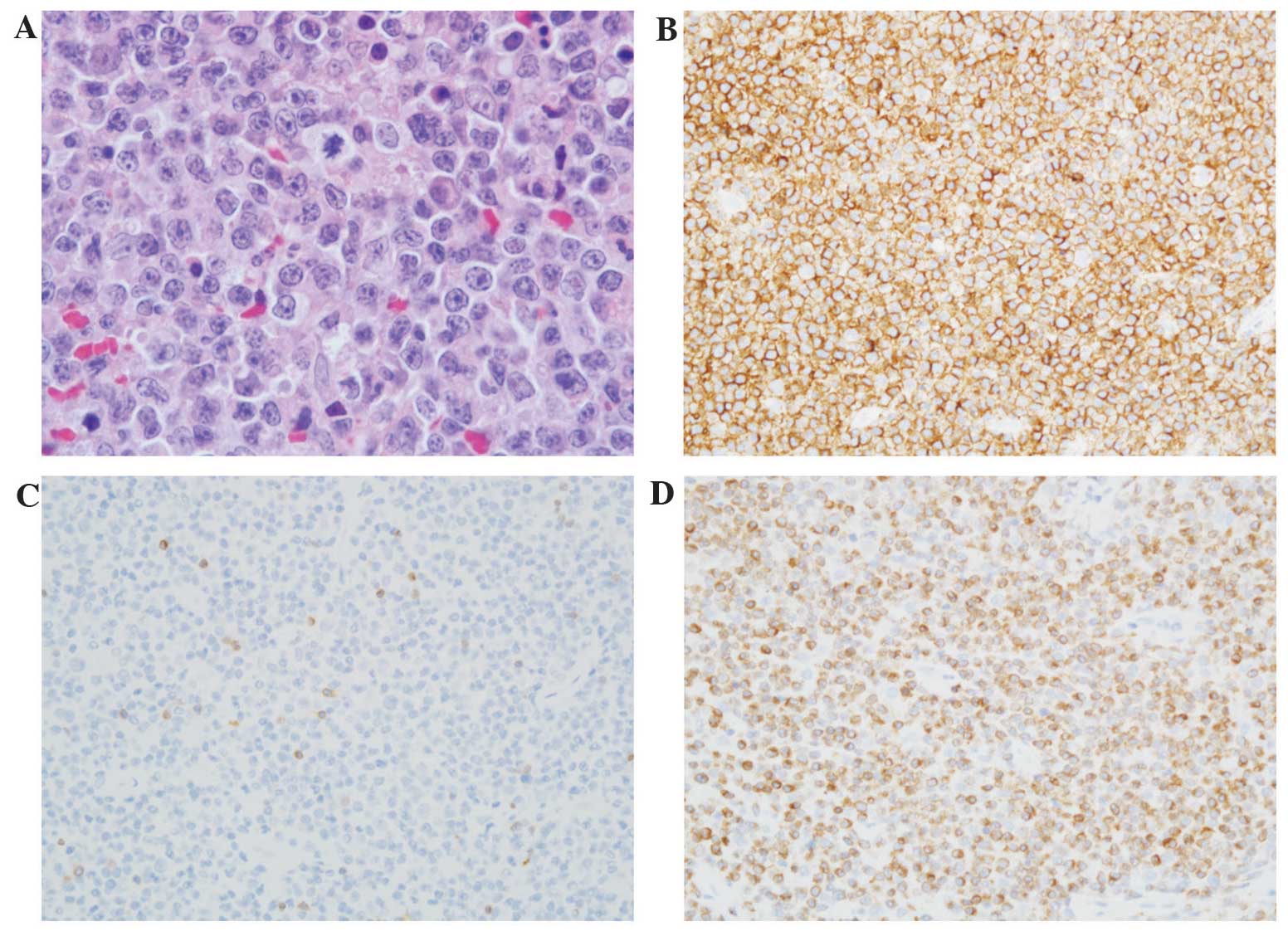
The diagnosis of malignant lymphoma was confirmed by
biopsy during laryngomicrosurgery. The specimens exhibited lymphoid
tissue with monotonous lymphoid cells, with nearly complete
destruction of lymphoid architecture and the proliferation of
medium- to large-sized atypical lymphocytes (compared with
histiocytes), characterized by moderate irregular nuclear shape,
coarse chromatin, numerous small distinct nucleoli and prominent
large nucleoli, moderate amount of light eosinophilic cytoplasm and
frequent mitoses. The atypical large lymphocytes were diffusely
positive for CD20 and Bcl-2, and negative for CD3, CD10 and Bcl-1,
indicating the diagnosis of malignant DLBCL (Fig. 2).
Tumor staging was performed. Magnetic resonance
imaging revealed an irregular infiltrative tumor sized 4×2.6×2.5 cm
in the left hypopharyngeal wall, involving the left side of the
epiglottis and the left piriform sinus. Positron emission
tomography-computed tomography revealed multiple focal areas of
increased fluorodeoxyglucose uptake involving the left hypopharynx
and bilateral neck lymph nodes, without distant metastasis. Bone
marrow biopsy was negative for tumor involvement (stage II
disease). The patient was scheduled to receive eight cycles over
4–6 weeks with rituximab 375 mg/m2 and cyclophophamide
750 mg/m2 + doxorubicin 50 mg/m2 +
vincristine 1.4 mg/m2 + prednisone 100 mg daily (R-CHOP
regimen). To date, the patient has received three cycles and is
followed up in our department.
Discussion
The symptoms of lymphoma may include enlarged lymph
nodes, fever, cold sweats, weight loss, pruritus and fatigue
(8,9).
However, our patient did not present with any of those symptoms.
There are numerous subtypes of lymphoma, the main two being HL and
NHL (2). NHLs constitute a
heterogeneous group of malignancies characterized by abnormal
clonal proliferation of T cells, B cells, or both. Approximately
90% of lymphomas are NHLs (3). The
risk factors for common types of NHL include autoimmune diseases,
HIV/AIDS, infection with human T-lymphotropic virus, consuming
large amounts of meat and fat, immunosuppressive medications and
certain pesticides (9). The diagnosis
is usually confirmed by lymph node biopsy. Blood, urine and bone
marrow tests may also be useful for diagnosis. Imaging may then be
performed to determine whether the cancer has spread and to which
location. Spread most commonly occurs to the lungs, liver and/or
brain (9). The head and neck is the
second most common region for extranodal lymphoma, the first being
the gastrointestinal tract (10).
Extranodal NHLs occurring primarily in the epiglottis are extremely
rare, accounting for merely 0.7% of all NHLs and 1% of malignant
laryngeal tumors (7). Supraglottic
cancer is almost exclusively squamous cell carcinoma. Therefore,
our case of DLBCL in the left epiglottis is very rare. The
treatment of lymphoma may combine chemotherapy, radiation therapy,
targeted therapy, surgery and other methods (8). R-CHOP is the most common
chemotherapeutic regimen for NHL and our patient was scheduled to
receive eight cycles over 4–6 weeks. In the United States, the
overall 5-year survival rate of HL is ~85% (11) and of NHL ~69% (12). According to the international
prognostic index established for patients aged <60 years, the
outcome of patients with extranodal DLBCL is similar to that of
patients with nodal DLBCL (13).
In conclusion, we presented a case of rare primary
extranodal NHL of the epiglottis. The patient is currently under
treatment with the R-CHOP regimen, and has received three cycles of
chemotherapy to date.
References
|
1
|
Taylor EJ: Dorland's Illustrated Medical
Dictionary (29th). Saunders, Philadelphia: 10382000.
|
|
2
|
Bardia A: Johns Hopkins Patients Guide to
Lymphoma. Burlington, Massachusetts: Jones and Bartlett Learning.
62010.
|
|
3
|
Leukemia and Lymphoma Society: The
Lymphoma Guide Information for Patients and Caregivers. https://www.lls.org/sites/default/files/file_assets/lymphomaguide.pdfAccessed.
June 20–2014
|
|
4
|
Smith A, Howell D, Patmore R, Jack A and
Roman E: Incidence of haematological malignancy by sub-type: A
report from the Haematological Malignancy Research Network. Br J
Cancer. 105:1684–1692. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Smith A, Roman E, Howell D, Jones R,
Patmore R and Jack A: Haematological Malignancy Research Network:
The Haematological Malignancy Research Network (HMRN): A new
information strategy for population based epidemiology and health
service research. Br J Haematol. 148:739–753. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kumar V, Abbas AK, Fausto N and Aster J:
Robbins and Cotran Pathologic Basis of Disease (8th). Philadelphia:
Elsevier Saunders. 6072010.
|
|
7
|
King AD, Yuen EH, Lei KI, Ahuja AT and Van
Hasselt A: Non-Hodgkin lymphoma of the larynx: CT and MR imaging
findings. AJNR Am J Neuroradiol. 25:12–15. 2004.PubMed/NCBI
|
|
8
|
National Cancer Institute. General
Information About Adult Hodgkin Lymphoma. http://www.cancer.gov/types/lymphoma/patient/adult-hodgkin-treatment-pdq#section/allAccessed.
June 20–2014
|
|
9
|
National Cancer Institute. General
Information About Adult Non-Hodgkin Lymphoma. http://www.cancer.gov/types/lymphoma/patient/adult-nhl-treatment-pdq#section/allAccessed.
June 20–2014
|
|
10
|
Jacobs C, Weiss L and Hoppe RT: The
management of extranodal head and neck lymphomas. Arch Otolaryngol
Head Neck Surg. 112:654–658. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
National Cancer Institute. SEER Stat Fact
Sheets-Hodgkin Lymphoma. http://seer.cancer.gov/statfacts/html/hodg.htmlAccessed.
August 26–2012
|
|
12
|
National Cancer Institute. SEER Stat Fact
Sheets: Non-Hodgkin Lymphoma. http://seer.cancer.gov/statfacts/html/nhl.htmlAccessed.
June 18–2014
|
|
13
|
Essadi I, Ismaili N, Tazi E, Elmajjaoui S,
Saidi A, Ichou M and Errihani H: Primary lymphoma of the head and
neck: Two case reports and review of the literature. Cases J.
1:4262008. View Article : Google Scholar : PubMed/NCBI
|