Introduction
Primary benign vascular lesions are more frequently
located in the skin and subcutaneous soft tissues compared with the
viscera, particularly the genitourinary system. In 2009, Montgomery
and Epstein (1) described for the
first time a novel subtype of benign vascular lesion, which was
termed an ‘anastomosing hemangioma’ (AH), of the genitourinary
tract (kidney and testis). Subsequently, several cases of AH were
reported in the adrenal gland, ovary, liver and gastrointestinal
tract (2–4). Although AH occurs relatively
infrequently, an incidence of AH in the bladder has arisen during
our medical researches. In the present case study, to the best of
our knowledge, the first case of AH in the bladder has been
reported, accompanied by a review of the literature on AH.
Case report
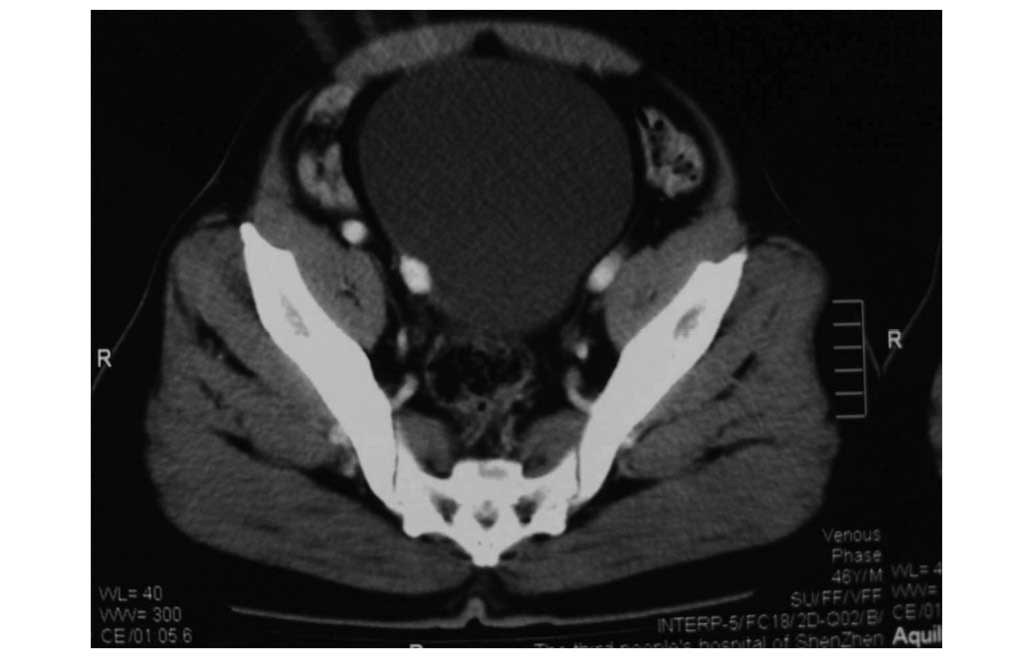
The patient was a 46-year-old Chinese man who had a
history of renal calculus and who underwent extracorporeal shock
wave lithotripsy twice (in 2009 and 2013). During a medical
examination (in March 2015), abdominal ultrasonography revealed
that, within the right wall of the bladder, there was a substantial
low echo nodule, measuring 14×11 mm, which was papillary in shape
and protruded into the bladder lumen. However, the patient remained
asymptomatic, and neither a physical examination nor a standard
laboratory examination revealed any noteworthy phenomena. The
lesion was further investigated using a contrast-enhanced
computerized tomography scan, and the results confirmed the
identification of an oval, sharply defined lesion within the right
wall of the bladder, which exhibited a marked homogeneous
enhancement (Figs. 1 and 2). This indicated the possibility that the
lesion may have been a vascular tumor. Subsequently, cystoscopy was
performed, and a sample of the lesion tissue was removed prior to
pathological examination. No characteristic tumor tissue was
identified on the mucosal surface of the bladder, although
congestive mucosa was observed on the right wall of the bladder,
and the pathological results revealed partial nuclear atypia.
On the basis of the results of the imaging and the
pathological findings, the patient finally underwent a partial
cystectomy (in April 2015). The pathological diagnosis was given as
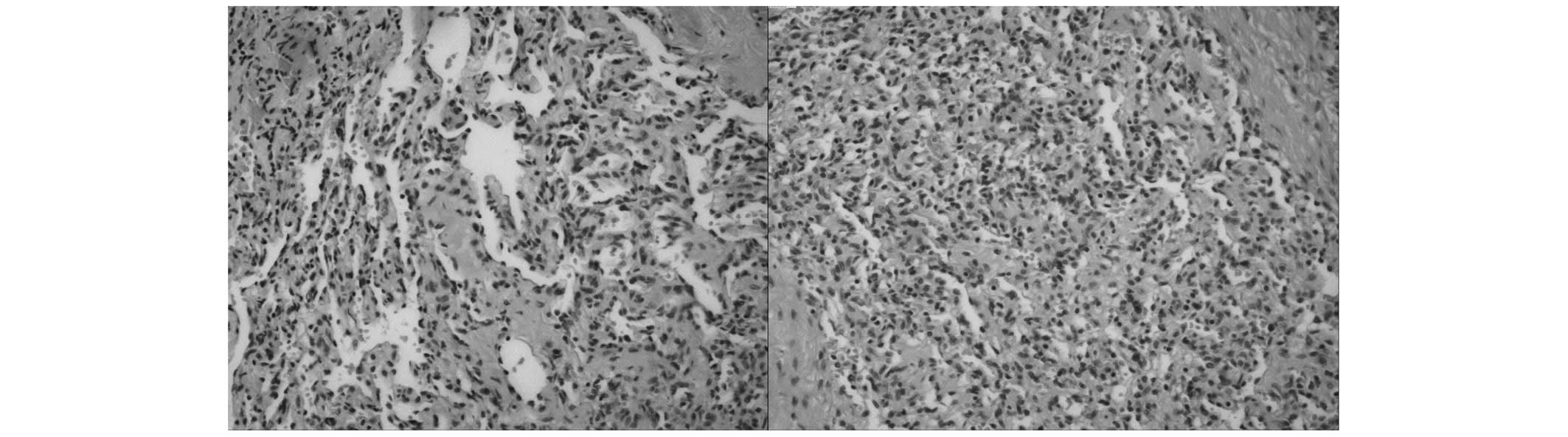
‘intramural AH of the bladder’. The gross pathological examination
revealed a well-circumscribed, russet-colored tissue, bearing a
fish/meat-like, gray-brown cut surface. The microscopic examination
revealed that the tumor tissue was lobulated, alternating with
sections of muscle. Furthermore, the structure of the lesion
predominantly comprised a small vascular cavity with irregularly
fenestrated, anastomosing vascular channels, with no obvious atypia
of the endothelial cells (Fig. 3).
These anatomical features supported the diagnosis of AH of the
bladder.
Discussion
Most bladder tumors are epithelial, and particularly
urothelial, in origin, and non-urothelial neoplasms occur very
rarely in the bladder. In addition, sarcoma accounts for the
majority of the non-urothelial neoplasms (5); hemangioma is extremely rare in the
urinary bladder. Non-urothelial bladder tumors, including squamous
cell carcinoma, adenocarcinoma and sarcoma, usually present a
diagnostic challenge. In the present study, to the best of our
knowledge, the first identified case of AH in the bladder has been
reported, which has increased the diagnostic challenge of
intramural tumors of the bladder. Hemangioma is very common in the
skin and subcutaneous soft tissue, and occasionally occurs in
viscera, and Montgomery and Epstein (1) first described AH in the kidney and
testis.
In the present case study, an AH located within the
bladder wall has been described, to the best of our knowledge for
the first time. To date, 29 cases of AH have been reported in the
English literature, a majority of them located in the kidney
(1–4,6–11). The immunohistochemical findings
indicated that CD34 was immunoreactive in all the tissues examined.
Generally, in the kidney, most identified lesions have occurred
singly, of median size 2 cm (range, 0.6–5 cm), and were associated
with end-stage renal disease (7).
Additionally, a majority of the patients were men, exhibiting no
characteristic symptoms. Imageological examinations proved
incapable of differentiating the AH from aggressive tumors, and
most of the patients with renal AH underwent a nephrectomy
(12). A number of the risk factors
remained unidentified, although, according to the cases reported,
being of the male gender is a risk factor.
Although the occurrence of AH is uncommon in the
genitourinary tract, pathologists and doctors ought to take it into
consideration in making the differential diagnosis, in order to
avoid misdiagnosis. In the present case study, it would have been
easy to have mistaken the AH as invasive, high-grade, urothelial
carcinoma. A differential diagnosis of AH is predominantly made
with malignant vascular tumors, including angiosarcoma, which is
usually an aggressive tumor characterized by infiltrative growth,
clear cytological atypia, high cellularity and poor prognosis.
Otherwise, in forming a diagnosis, it is essential to distinguish
the AH from other intramural tumors, including paragangliomas and
bladder sarcoma. The pathological finding that AH is composed of a
small vascular cavity with irregularly fenestrated, anastomosing
vascular channels allows the correct diagnosis to be made.
According to the previously reported cases, upon
microscopical examination, AH is typically characterized by
numerous thin-walled, vascular channels, which grow according to an
anastomosing pattern, and which lack distinct endothelial atypia or
multilayering (1). Certain variants
of glomus tumors should also be taken into consideration, for they
too possess an abundant vasculature network (12). The majority of the clinical follow-up
of the AH occurs in a time-frame of ~3 months to 3 years, the
longest reported case being of 13 years (12). Although AH is a type of tumor which
was considered to be benign, given that the most important
differential diagnosis of AH is aggressive angiosarcoma and that
imageological examinations are unable to differentiate the AH from
aggressive tumors, the majority of patients with renal AH have
undergone a nephrectomy, or partial nephrectomy (12). However, it must be recognized that
nephrectomy is an excessive treatment for patients with renal AH.
The case reported in the present study was the first identified
case of AH occurring in the bladder, and the patient underwent
partial cystectomy.
Clinically, abdominal B-ultrasonography has been
used for the initial examination of patients with bladder cancer,
and has been selected for the majority of bladder tumors due to its
non-invasive properties, speediness and the ease of convenience.
The bladder mass of the patient described in the present case study
was initially identified using ultrasonography, without any
discomfort for the patient, who is recovering well one month
following the surgery. This case has highlighted that the
differential diagnosis of intramural neoplasms in the bladder is
vitally important for managing the different treatment required,
and for the prognosis.
In conclusion, in the present case study, an AH
located in the wall of bladder was identified, to the best of our
knowledge for the first time. In view of the limited number of
reported cases, there is no ‘gold standard’ treatment for AH, and
men are considered to be at greater risk compared with women. It is
important to distinguish AH from malignant vascular tumors, since
the required therapeutic approach, and the prognosis between them,
may differ substantially.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (no. 81101922), Science and Technology
Development Fund Project of Shenzhen (nos. JCYJ20130402114702124
and JCYJ20150403091443329) and the fund of the Guangdong Key
medical subject.
References
|
1
|
Montgomery E and Epstein JI: Anastomosing
hemangioma of the genitourinary tract: A lesion mimicking
angiosarcoma. Am J Surg Pathol. 33:1364–1369. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ross M, Polcari A, Picken M, Sankary H and
Milner J: Anastomosing hemangioma arising from the adrenal gland.
Urology. 80:e27–e28. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kryvenko ON, Gupta NS, Meier FA, Lee MW
and Epstein JI: Anastomosing hemangioma of the genitourinary
system, Eight cases in the kidney and ovary with
immunohistochemical and ultrastructural analysis. Am J Clin Pathol.
136:450–457. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lin J, Bigge J, Ulbright TM and Montgomery
E: Anastomosing hemangioma of the liver and gastrointestinal tract,
An unusual variant histologically mimicking angiosarcoma. Am J Surg
Pathol. 37:1761–1765. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dahm P and Gschwend JE: Malignant
non-urothelial neoplasms of the urinary bladder: A review. Eur
Urol. 44:672–681. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chou S, Subramanian V, Lau HM and Achan A:
Renal anastomosing hemangiomas with a diverse morphologic spectrum,
Report of two cases and review of literature. Int J Surg Pathol.
22:369–373. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhao M, Li C, Zheng J and Sun K:
Anastomosing hemangioma of the kidney, A case report of a rare
subtype of hemangioma mimicking angiosarcoma and review of the
literature. Int J Clin Exp Pathol. 6:757–765. 2013.PubMed/NCBI
|
|
8
|
Tao LL, Dai Y, Yin W and Chen J: A case
report of a renal anastomosing hemangioma and a literature review,
An unusual variant histologically mimicking angiosarcoma. Diagn
Pathol. 9:1592014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tahir M and Folwell A: Anastomosing
haemangioma of kidney: A rare subtype of vascular tumour of the
kidney mimicking angiosarcoma. ANZ J Surg. 2014.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wetherell DR, Skene A, Manya K, Manecksha
RP, Chan Y and Bolton DM: Anastomosing haemangioma of the kidney A
rare morphological variant of haemangioma characteristic of
genitourinary tract location. Pathology. 45:193–196. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tran TA and Pernicone P: Anastomosing
hemangioma with fatty changes of the genitourinary tract: A lesion
mimicking angiomyolipoma. Cent European J Urol. 65:40–42. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Heidegger I, Pichler R, Schäfer G, Zelger
B, Zelger B, Aigner F, Bektic J and Horninger W: Long-term follow
up of renal anastomosing hemangioma mimicking renal angiosarcoma.
Int J Urol. 21:836–838. 2014. View Article : Google Scholar : PubMed/NCBI
|