Introduction
The use of intensity-modulated radiation therapy
(IMRT) for postoperative cervical cancer has increased
significantly over the last few years, due to its highly conformal
dose distribution to the targets and favorable acute and chronic
toxicity profile (1–10). However, during this highly precise
radiotherapy treatment, the movement of organs at risk (OARs) and
targets may be a major issue and present the physicians with a
significant challenge.
There are several studies on radical radiotherapy
for cervical cancer, which demonstrated that significant movements
of the uterus may be observed due to the filling of the bladder and
rectum (11–15). With the different daily filling status
of OARs and the steep dose gradient, there is a potential risk of a
geographical miss; this may result in a reduction of local control
in gynecological cancer of ≤30% (16). For postoperative cervical cancer
patients, there may be similar detrimental effects; however, the
number of related studies is currently limited.
Cone-beam computed tomography (CBCT)-based
image-guided radiotherapy (IGRT) is a technology used for reducing
positional set-up errors in radiotherapy. In addition, CBCT may
achieve 3D volume imaging of organs, with sufficient soft-tissue
contrast to differentiate between these organs. Furthermore, the
daily bladder, rectum and vagina motion may be studied based on
CBCT scans.
The aim of this study was to determine the
interfractional motion and deformation of the bladder, rectum and
vagina in patients with postoperative cervical cancer treated with
IMRT.
Patients and methods
Patients
Between January, 2008 and June, 2009,
post-hysterectomy patients with cervical cancer requiring
postoperative radiotherapy or chemoradiotherapy due to positive
pelvic lymph nodes or other high-risk factors evaluated
retrospectively. Patients were considered as ineligible if they
exhibited a positive vaginal cuff, disease outside the pelvis, or
mental status alterations. A total of 8 patients receiving IMRT and
IGRT in our institution were included in the analysis. The
postoperative stages were classified as Ib-IIb and the patient age
ranged between 42 and 66 years.
Planning CT scan
The planning CT scan was performed in the supine
position. A MedTech body frame (Elekta AB, Stockholm, Sweden) and
thermoplastic body mask (Klarity Medical, Guangzhou, China) were
utilized. The slice thickness was 3 mm and the scanned volume
extended from the anus to L1. All the patients were instructed to
control the filling status of the bladder and rectum in order to
minimize organ deformation during the treatment. One hour prior to
scanning, the patients were instructed to ingest 500 ml of water
with the intention of achieving a moderately full and comfortable
bladder for contrast CT scan acquisition and during each treatment.
The patients were also instructed to encourage bowel movement so as
to have an empty rectum prior to the CT scan and each
treatment.
Treatment
Following simulation, the CT images were transferred
to the Elekta PrecisePLAN (Release 2.10) workstation to design the
external beam IMRT plan. The clinical target volume (CTV)
delineation was referred to the consensus guidelines of the
Radiation Therapy Oncology Group (11) and included the common, external,
internal iliac and presacral lymph node regions, the upper 3 cm of
the vagina and the paravaginal soft tissues. The CTV-to-planning
target volume (PTV) margin was 1 cm in all directions. The
prescribed radiation dose was 50 Gy, delivered in 25 daily
fractions of 2 Gy. All the patients were treated with 6 MV X-ray
delivered by the Elekta Synergy S system (Elekta AB).
Prior to each treatment, the patients underwent CBCT
scans to obtain daily images and set-up errors. The parameters of
CBCT imaging were 120 kV, 25 mA, with rotation starting from 182°
to end at 180° for 620 frames. Subsequently, the CBCT images were
matched to the planning CT using the bony alignment of the entire
pelvis to obtain set-up errors; if the translational error exceeded
2 mm, the patients' position was corrected by adjusting the
treatment couch. Rotation errors were not corrected due to the
limitations of the treatment couch.
Definition of the bladder, rectum and
vagina on CBCT scans
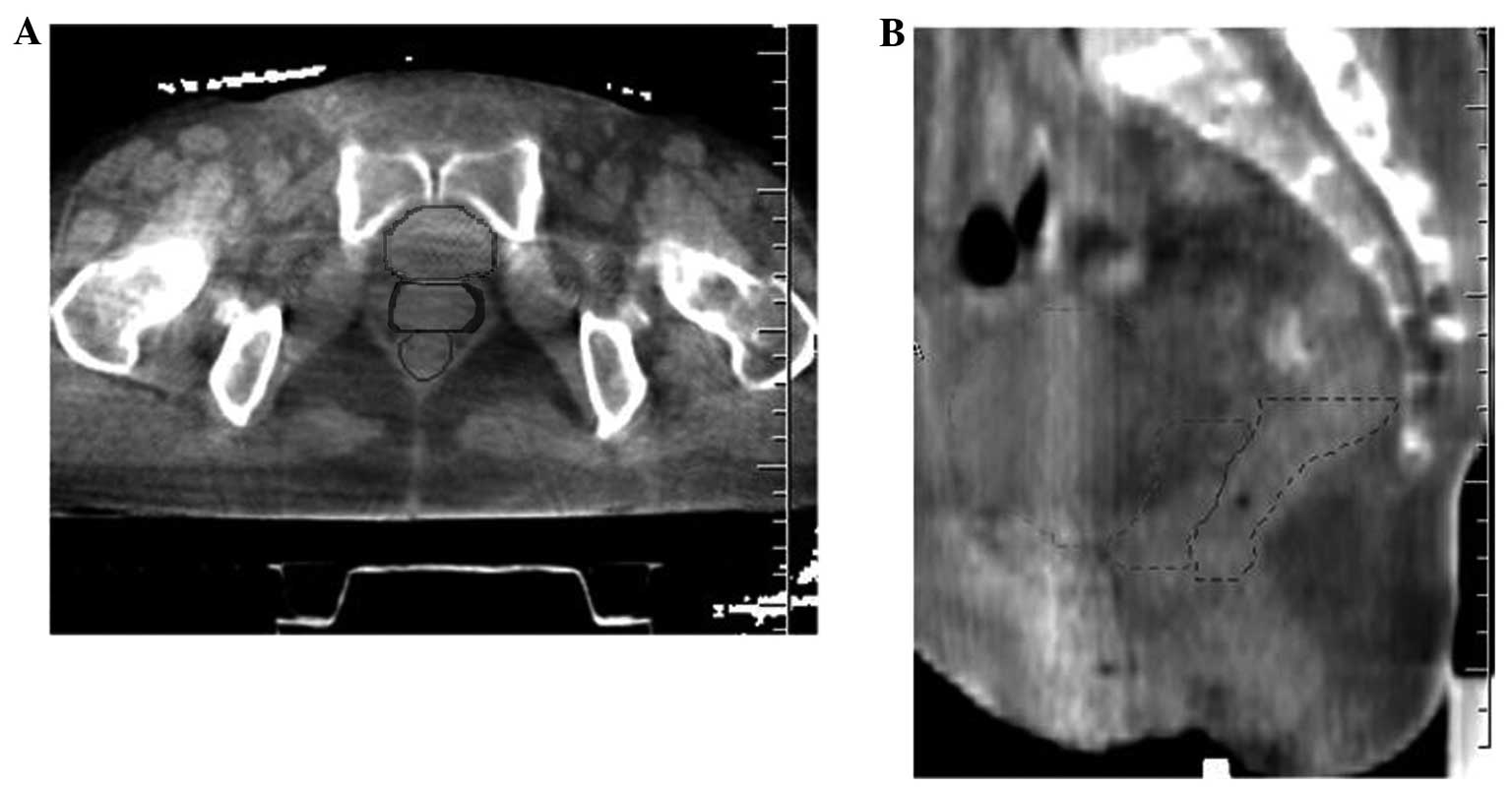
Following treatment, the CBCT scans and planning CT
images were transferred to the TomoCom 3.0 workstation (Elekta AB).
The bladder, rectum and vagina during each treatment were contoured
on these CBCT scans after the soft tissue value was adjusted to fit
for anatomical identification (Fig.
1). The part of the rectum lying between 2 cm below and 3.5 cm
above the superior border of the pubic symphysis was contoured. The
vagina was differentiated by identifying the tissue between the
posterior border of the bladder and anterior border of the rectum
on daily CBCT scans. Two physicians jointly defined the contours
when these organs were not clearly identified on CBCT scans. The
CBCT scans were then fused with the planning CT images. The quality
of the contours and each registration were reviewed and verified by
a senior physician and the structures contoured on the CBCT scans
were transferred to the planning CT images.
Analysis of organ motion
The bladder motion was first defined as the movement
of the bladder border relative to that on the planning CT. On the
midsagittal plane, the vertical distance of the anterior,
posterior, superior and inferior bladder borders between the
planning CT and each CBCT scan was measured. The bladder motion of
the left and right borders was measured on the plane vertical to
the posterior side of the pubic symphysis.
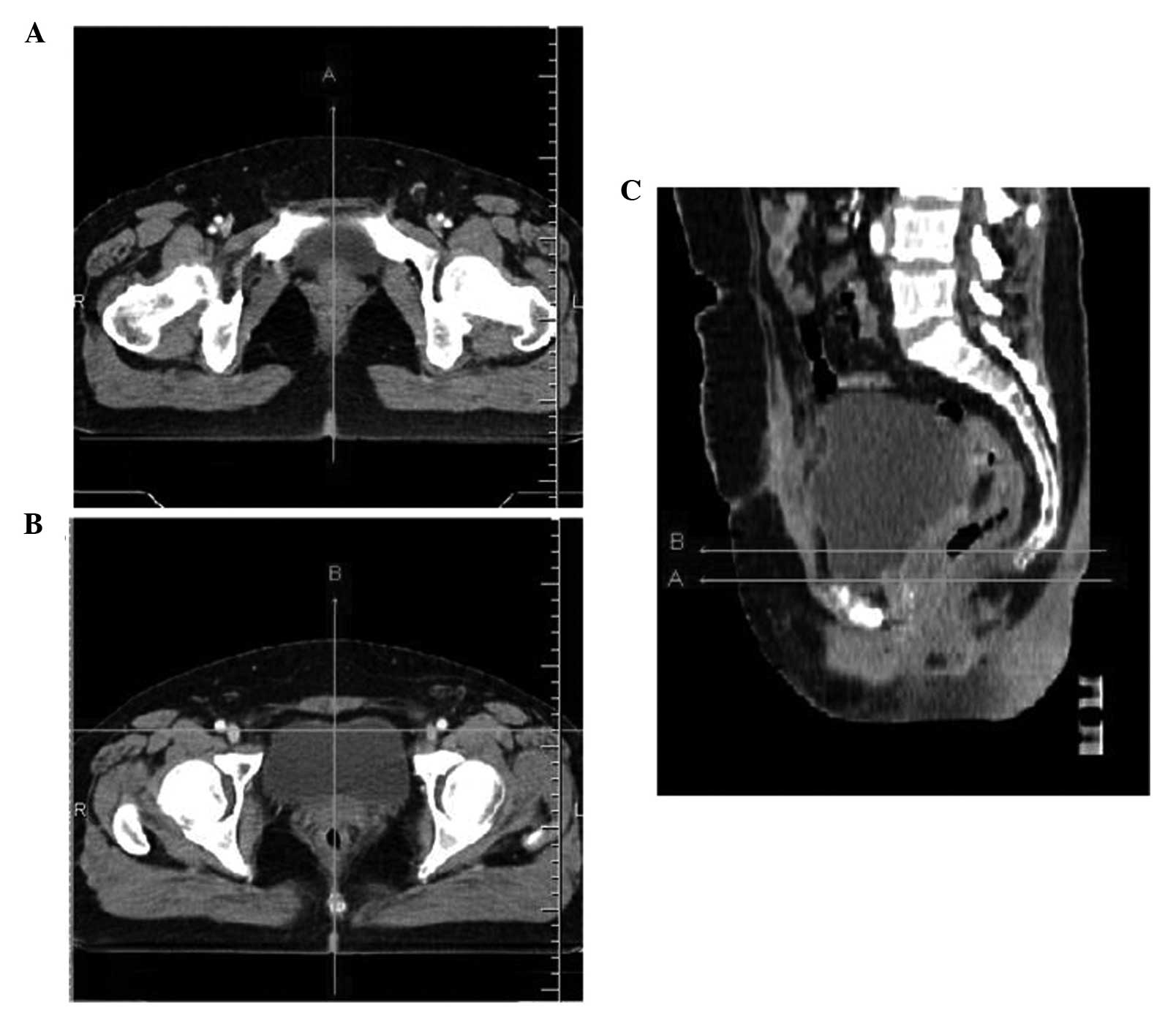
In order to assess the motion of the vagina, the
posterior bladder border and the anterior rectal border, two
reference lines were identified on the axial images using the
sagittal and coronal images on each planning CT image. Line A was
defined as the midsagital line across the superior border of the
pubic symphysis; and line B was the parallel line 1.5 cm above line
A (Fig. 2). The interfractional
motion of the posterior bladder border and anterior rectal border
were measured on lines A and B, respectively. As the apical extent
of the vagina could not be consistently identified on the CBCT scan
without implanted markers and the cephalad extent of the vagina was
variable according to the differences in the bladder filling status
(12), the motion of the vagina in
the anteroposterior (AP) direction and the AP dimension of the
vagina were measured on lines A and B, in the midline on which the
vagina was more readily identified. The bladder and rectal volumes
were also calculated and the correlation between organ motion and
changes in these volumes was analyzed.
As regards organ motion, the mean ± standard
deviation (SD) of all the data was calculated. Motion in the
posterior direction was defined as positive and in the anterior
direction as negative. Similarly, motion in the superior direction
was defined as positive and in the inferior direction as negative.
The Pearson's correlation coefficient was utilized to investigate
the correlation between the margins and the changes in the volumes
of the rectum and bladder.
Results
CBCT images
CBCT ensures adequate image quality to define the
structure and boundaries of soft tissue organs, including the
bladder, rectum and vagina in the pelvis. A total of 200 sessions
of CBCT were performed for the 8 patients, and the structures and
boundaries of the bladder, rectum and vagina were delineated on 176
CBCT images that were of good quality. On average, 22 CBCT
images/patient were usable for analysis.
Variability of bladder and rectum
volume
The repeated CBCT scans revealed extensive organ
motion and variations in the volume and shape of the bladder and
rectum. The mean volume (range) of the bladder was 158.5
(15.4–626.5) ml, with an SD of 134.3 ml. Significant differences
were observed between the planning CT scan and the following daily
CBCT scans, ranging from −471.0 to 264.4 ml. The mean volume on
weeks 1, 2, 3, 4 and 5 was 156.2, 162.5, 143.2, 138.7 and 159.2 ml,
respectively. However, there were no significant differences among
weekly scans due to the instructions (P>0.05).
The mean volume (range) of the rectum was 48.2
(11.3–139.7) ml, with an SD of 18.9 ml. Differences ranging from
−71.1 to 102.4 ml compared with the planning CT were observed. The
mean volume of the rectum on weeks 1, 2, 3, 4 and 5 was 43.5, 44.7,
50.8, 48.8 and 53.2 ml, respectively. The differences among weekly
scans were also not significant due to the instructions
(P>0.05).
Motion of the bladder and rectum
boundaries
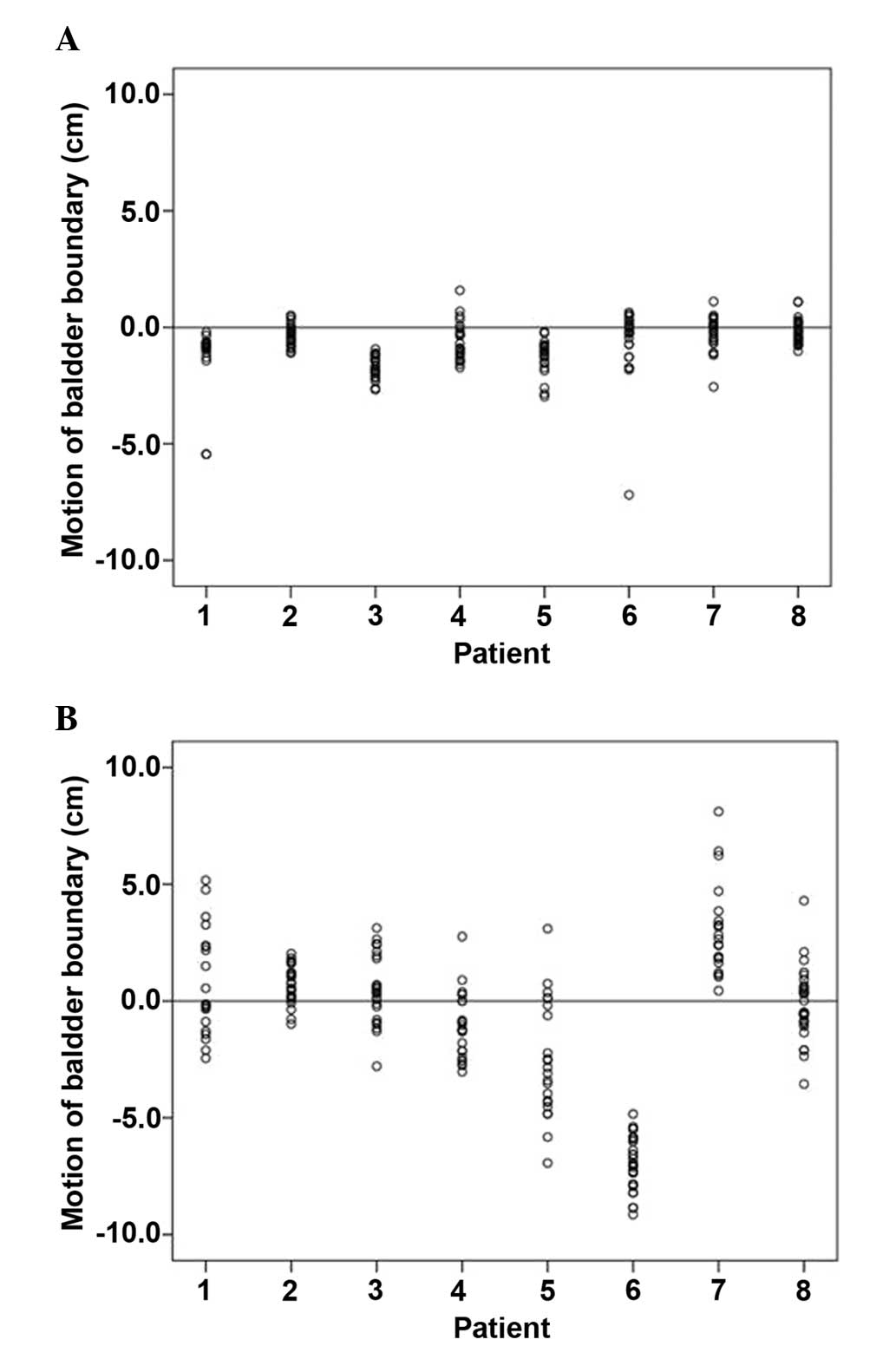
The motion and deformation of the bladder were
significant according to the daily CBCT scans. The results of
bladder motion are presented in Table
I. The motion data of the posterior and superior boundaries,
which indicated the most significant movement, are displayed in
Fig. 3. The motion of the inferior
boundary was found to be the smallest (0.1 cm; SD = 0.7 cm).
 | Table I.Bladder motion (cm). |
Table I.
Bladder motion (cm).
| Values | Anterior | Posterior | Inferior | Superior | Left | Right |
|---|
| Mean |
0.5 | −0.7 |
0.1 | −0.9 | −0.5 | −0.5 |
| SD |
0.9 |
1.0 |
0.7 |
3.3 |
0.8 |
0.7 |
| Max |
2.9 |
1.6 |
2.0 |
8.1 |
1.7 |
1.1 |
| Min | −1.6 | −7.2 | −1.1 | −9.1 | −3.6 | −3.2 |
The motion of the posterior boundary was intensively
analyzed, as it may significantly affect the delineation of CTV. In
addition, obvious motion and deformation of the rectum were also
observed based on daily CBCT scans. Similar to the posterior
boundary of the bladder, only the motion of the anterior boundary
of the rectum was intensively analyzed. These two types of motion
along lines A and B, respectively, are shown in Table II.
 | Table II.Motion of bladder and rectum
boundaries (cm). |
Table II.
Motion of bladder and rectum
boundaries (cm).
|
| Motion of posterior
boundary of bladder | Motion of anterior
boundary of rectum |
|---|
|
|
|
|
|---|
| Values | Line A | Line B | Line A | Line B |
|---|
| Mean |
0.08 | −0.4 | −0.5 | −0.7 |
| SD |
1.1 |
0.7 |
1.1 |
1.2 |
| Max |
2.9 |
1.9 |
2.1 |
1.7 |
| Min | −1.7 | −2.1 | −3.9 | −3.7 |
Position of the vagina relative to the
PTV
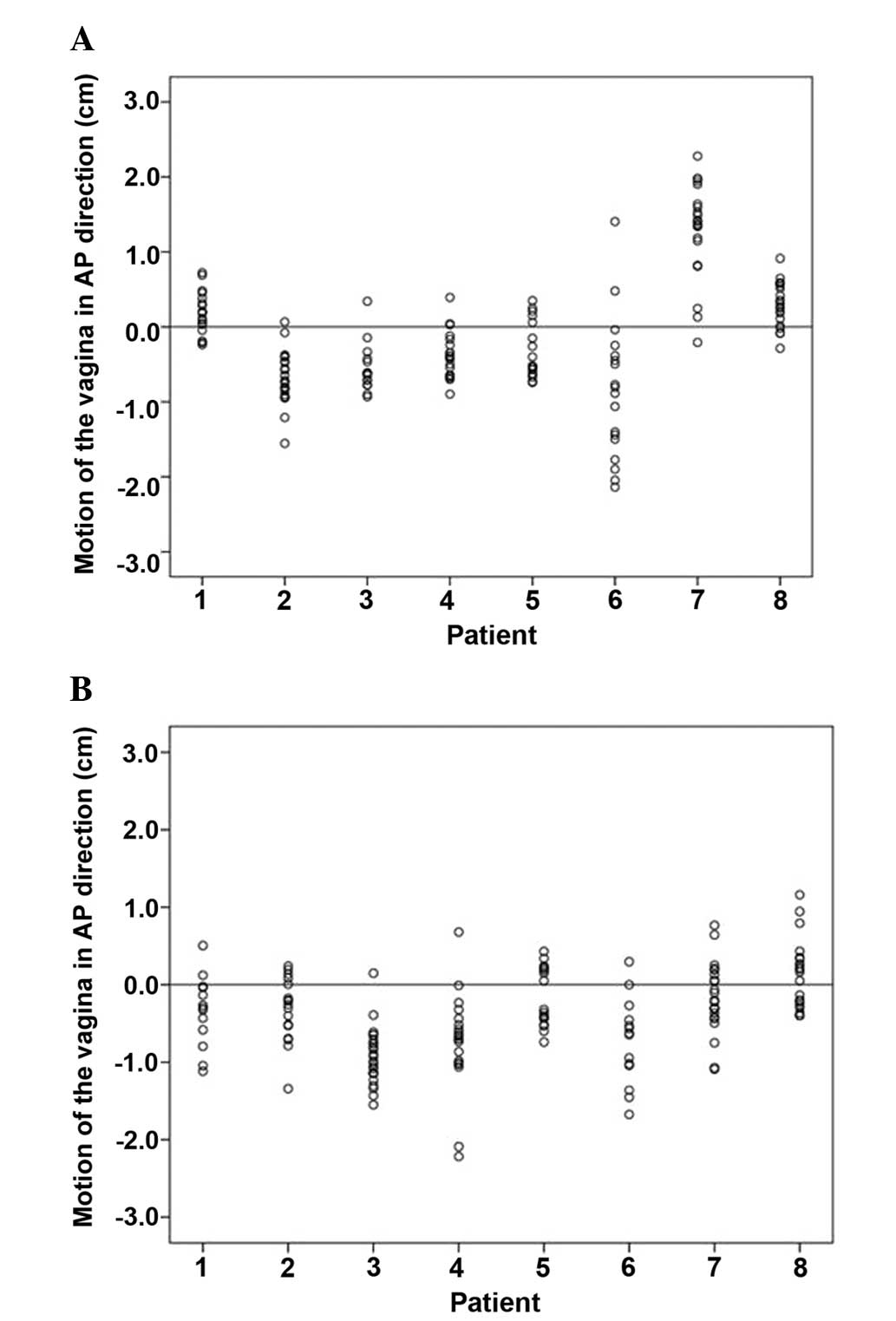
We reviewed the position of the vagina relative to
the margins of the PTV on lines A and B based on daily CBCT scans,
to assess whether the vagina was adequately covered by the
planning. For the 176 sessions of CBCT, the uniform margin of 10 mm
failed to encompass the vagina in 17.3 and 18.1% of fractions on
lines A and B, respectively. The variability of the AP dimension of
the vagina was used as a representative measure for vaginal
deformation and was also measured based on daily CBCT scans. The
mean ± SD of the AP dimension of the vagina was 1.3±0.8 cm on line
A and 1.5±0.9 cm on line B. The mean (SD) motion of the vagina was
0.3 (0.3) cm and 0.1 (0.5) cm on lines A and B, respectively; and
in the AP direction in the midline the range of motion was −2.1 to
2.3 cm and −2.2 to 2.1 cm, respectively (Fig. 4).
Correlation between organ volume and
organ motion
The change in the posterior bladder boundary
relative to the bladder volume was found to be significant on lines
A and B (P<0.05 for both; the Pearson's correlation coefficient
was 0.32 and 0.31, respectively). In addition, the change in the
anterior rectal boundary was found to be correlated with the volume
of the rectum on lines A and B (P<0.05 for both; the Pearson's
correlation coefficient was 0.29 and 0.18, respectively).
The change in the AP dimension of the vagina
relative to the bladder volume was found to be subtle but
significant on lines A and B (P<0.05 for both; the Pearson's
correlation coefficient was 0.37 and 0.30, respectively). No
correlation was found between the change in the AP dimension of the
vagina and rectum volume on lines A and B (P>0.05 for both; the
Pearson's correlation coefficient was 0.092 for both). The
correlation of the motion of the vagina in the AP direction in the
midline with bladder volume was found to be weak but significant on
lines A and B (P<0.05 for both; the Pearson's correlation
coefficient was 0.37 and 0.44, respectively). However, no
correlation was found between the motion of the vagina and rectal
volume on lines A and B (P>0.05 for both; the Pearson's
correlation coefficient was 0.026 and 0.011, respectively).
Discussion
The motion and deformation of the target and OARs
may significantly affect the accuracy of radiotherapy, particularly
IMRT. Quantification of organ motion may help define appropriate
PTV margins, optimize target volume coverage of the vagina and
spare normal tissues. Previous studies have addressed these
problems in patients with advanced cervical cancer (13–16).
However, studies on patients with cervical cancer postoperatively
are sparse. As regards the methodology for studying motion and
deformation, different modalities have been reported, including
ultrasound (17), magnetic resonance
imaging (MRI) scans (18,19), repeated CT scans and on-board imaging
(OBI) (15). CBCT is increasingly
used for online set-up correction, soft tissue targeting, safety
margin calculation (20,21) and image-guided adaptive radiotherapy
(22,23). CBCT is more convenient for daily
imaging compared with MRI and CT. Therefore, in this study, CBCT
was used daily to assess the motion and deformation of the bladder,
rectum and vagina during postoperative radiotherapy in cervical
cancer patients.
In previous studies, large variations and a time
trend of bladder filling were reported in patients undergoing
radical radiotherapy for cervical cancer when no bladder control
instructions were provided (14,24). Ahmad
et al (17) reported that the
bladder volume ranged from 30 to 770 ml. Without instructions, the
bladder volume was reported to gradually decrease weekly, and it
was usually significantly different by week 4 (14,24,25). The
bladder volume reduction was considered to be a treatment-related
side effect (17). For postoperative
radiotherapy, the variation of the bladder was also significant. It
was reported that, despite instructions regarding the significance
and method of pretreatment fluid intake, differences between the
pretreatment full bladder and each subsequent CT scan ranged from
53.2 to 698.0 cc (12). In our study,
similar results were reported and the differences ranged from
−471.0 to 264.4 ml. No obvious time trend was observed in our study
due to the specific drinking instructions. In order to achieve a
more constant bladder volume with instructions, certain researchers
suggested a personal drinking advice each treatment day based on
the biofeedback (26), or to maintain
a smaller initial bladder volume and use a patient information
sheet (27).
As regards the rectal volume, the results may be
quite different, as different regions of the rectum were delineated
in different studies. For patients receiving postoperative
radiotherapy, marked variations in rectal volume were observed
without instructions, ranging from 46 to 193 cc (12). The average rectal volume reported in
our study was smaller, which may be explained by the fact that only
part of the rectum was delineated in our study, as the upper and
lower parts of the rectum were difficult to differentiate on CBCT
scans. However, the difference in volume was similarly significant
(range, −71.1 to 102.4 ml), even with instructions. Another study
also reported variations in bowel volume, despite using laxatives
to minimize bowel content (28).
It was reported that the movements of the uterus
were found to be larger compared with those of the cervix,
particularly in the superoinferior (SI) and AP directions (29). Buchali et al (16) revealed that the uterus and cervix
moved for ≤1.5 and 0.6 cm, respectively, comparing a full bladder
with an empty bladder. Ahmad et al (17) reported that the displacement of the
uterus was 2 cm/100 ml bladder volume change. The daily cervical
movement represented by 2 seeds placed in the cervix was reported
to be 1.9, 4.1 and 4.2 mm in the right-to-left (RL), SI and AP
directions, respectively, using OBI (15). However, these results were all based
on patients not treated surgically.
To the best of our knowledge, the number of
available studies focusing on vaginal motion in postoperative
patients is limited (12,25,30,31). The
motion of the vaginal apex in postoperative patients appeared to be
more significant compared with the motion of the cervix in patients
receiving radical radiotherapy. The motion of fiducial markers
placed at the vaginal apex, which represented the motion of the
apex, was previously assessed. Harris et al (32) reported that the median motion of the
fiducials was 5.8 mm (range, 0.6–20.2 mm) and the directional
margins along the RL, SI and AP axes were 3.1, 9.5 and 12.1 mm,
respectively, using daily megavoltage CT scans. Jhingran et
al (12) reported that the median
movement of the markers was 0.59 cm (range, 0–0.9 cm), 1.46 cm
(range, 0.8–2.79 cm) and 1.2 cm (range, 0.6–2.1 cm) in the RL, AP
and SI directions, respectively, using repeat CT scans.
In addition to the motion of the vaginal apex, the
displacement of the vagina may also vary due to the differences in
the filling status of the bladder and rectum (12). However, these displacements have not
been extensively investigated. It was reported that the vaginal
CTVs change their position with a maximum displacement in the AP
direction using weekly MRI scans, with a 95% confidence level of
2.3 cm (25). In our study, we
obtained similar results on vagina motion compared with those in
the literature, by measuring the motion on two levels where the
vagina could be easily differentiated. In the majority of the
cases, the vagina could be differentiated from the bladder and
rectum on CBCT scans, with daily CBCT scans providing accurate
daily details on interfractional location and the status of the
soft tissues at the treatment time. The motion of the vaginal apex
was not assessed in our study, as the apical extent of the vagina
could not be consistently identified on the CBCT scans, and no
marker was implanted to help differentiate the vaginal apex.
To standardize the CTV delineation of the vagina, it
was suggested to maintain a 1.5-cm distance between the anterior
and posterior borders of the CTV at the midline (11). In our study, we measured the daily AP
dimensions of the vagina on two levels in the midline and our
results revealed that the mean AP distance of the vagina on lines A
and B was 1.3 and 1.5 cm, respectively, consistent with the
recommendations.
As obvious movement of the vagina, bladder and
rectum was demonstrated, the margin of the target should be
carefully considered to avoid the underdosage of the target. In
this study, we found that a uniform margin of 10 mm failed to
encompass the vagina in 17.3 and 18.1% of the fractions on lines A
and B, respectively. However, this encompassment rate appeared to
be higher compared with that of intact cervical cancer (33) and the vaginal apex postoperatively
(31). For intact cervical cancer, a
uniform margin of 10 mm reportedly failed to encompass the CTV in
59% of the fractions and failed to encompass the cervix and fundus
in 36 and 54% of the fractions, respectively (33). It was recently reported that the
probability of cuff excursion outside the CTV was reduced to 4.2%
as margin size increased to 2.0 cm in patients receiving
postoperative irradiation (31). It
was also revealed that interpatient variation was the predominant
component of high variation in margin estimates (33). Therefore, it is crucial to
individualize the internal target volume (ITV). To measure
individualized ITV, certain studies used fused planning CT scans
obtained with a full and empty bladder (11,12).
However, from our study as well as others, it is known that the
difference between the full and empty bladder would be more obvious
during the radiation treatment course compared with baseline
(12). In order to reduce the
uncertainty of target location, filling the bladder with a fixed
volume of saline was attempted; however, this may not practical for
all patients or entirely tolerable during radiotherapy (12). Apart from the bladder, the filling
status of the rectum may also affect the target location, but has
been less extensively investigated in gynecological patients. It
was reported that a Fleet enema was given to patients with prostate
cancer to decrease the uncertainty of the prostate position caused
by rectal filling; however, it was not practical for gynecological
patients due to the more severe diarrhea and hemorrhoids caused by
the larger irradiation volume. Moreover, certain researchers
suggested evaluating the rectal volume prior to simulation and
trying to limit the variations in rectal volume by advising
patients to attempt and evacuate, or by decreasing the gas in the
rectum using a rectal tube (12).
Otherwise, a 5–10-mm margin would be suggested to be added to the
posterior border of the target (12).
The association between bladder and rectal volume
and shifts in the position of uterus, cervix and vaginal apex
markers were analyzed by several studies (12,13,16,25).
The association between bladder filling and uterine movement was
controversial (13,16), while rectal filling was reported to be
correlated with the movement of the cervix and upper vagina
(13,25). Jhingran et al (12) revealed that rectal and bladder volume
were both correlated with significant displacement of the vaginal
apex. In our study, it was demonstrated that the position of the
vagina was significantly affected by the filling status of the
bladder, but not by that of the rectum.
The disadvantage of CBCT is the relatively poor soft
tissue contrast, particularly for the distal rectum and vagina.
Therefore, we only assessed the volume of the rectum that lies
between 2 cm below and 3.5 cm above the superior border of the
pubic symphysis, and assessed the motion of the vagina on line A
(the horizontal line across the superior border of the pubic
symphysis) and line B (the parallel line 1.5 cm above line A),
which could be easily identified. However, the predominant
advantage of CBCT is that it enables the acquisition of daily
images and online corrections.
In conclusion, daily kv-CBCT scanning may be used to
effectively evaluate the interfractional motion and deformation of
the OARs and the target during postoperative radiotherapy of
cervical cancer. It was demonstrated that there remain obvious
variations in target location and organ volume, even with specific
patient instructions. In addition, the variations in the filling
status of the bladder may significantly affect the position of the
vagina. During treatment, it is crucial to consider that any
uncertainty regarding the position of the OARs and the target may
affect treatment accuracy. The uniform PTV margin of 10 mm failed
to encompass the vagina in 17.3 and 18.1% of the fractions on lines
A and B, respectively. Therefore, a more effective approach to
decreasing this uncertainty is required.
Glossary
Abbreviations
Abbreviations:
|
CBCT
|
cone-beam computed tomography
|
|
IMRT
|
intensity-modulated radiotherapy
|
|
OARs
|
organs at risk
|
|
IGRT
|
image-guided radiotherapy
|
|
CTV
|
clinical target volume
|
|
PTV
|
planning target volume
|
References
|
1
|
Heron DE, Gerszten K, Selvaraj RN, et al:
Conventional 3D conformal versus intensity-modulated radiotherapy
for the adjuvant treatment of gynecologic malignancies: A
comparative dosimetric study of dose-volume histograms. Gynecol
Oncol. 91:39–45. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mundt AJ, Lujan AE, Rotmensch J, Waggoner
SE, Yamada SD, Fleming G and Roeske JC: Intensity-modulated whole
pelvic radiotherapy in women with gynecologic malignancies. Int J
Radiat Oncol Biol Phys. 52:1330–1337. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Portelance L, Chao KS, Grigsby PW, Bennet
H and Low D: Intensity-modulated radiation therapy (IMRT) reduces
small bowel, rectum and bladder doses in patients with cervical
cancer receiving pelvic and para-aortic irradiation. Int J Radiat
Oncol Biol Phys. 51:261–266. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Roeske JC, Lujan A, Rotmensch J, Waggoner
SE, Yamada D and Mundt AJ: Intensity-modulated whole pelvic
radiation therapy in patients with gynecologic malignancies. Int J
Radiat Oncol Biol Phys. 48:1613–1621. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
van de Bunt L, van der Heide UA, Ketelaars
M, de Kort GA and Jürgenliemk-Schulz IM: Conventional, conformal
and intensity-modulated radiation therapy treatment planning of
external beam radiotherapy for cervical cancer: The impact of tumor
regression. Int J Radiat Oncol Biol Phys. 64:189–196. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brixey CJ, Roeske JC, Lujan AE, Yamada SD,
Rotmensch J and Mundt AJ: Impact of intensity-modulated
radiotherapy on acute hematologic toxicity in women with
gynecologic malignancies. Int J Radiat Oncol Biol Phys.
54:1388–1396. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mundt AJ, Mell LK and Roeske JC:
Preliminary analysis of chronic gastrointestinal toxicity in
gynecology patients treated with intensity-modulated whole pelvic
radiation therapy. Int J Radiat Oncol Biol Phys. 56:1354–1360.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beriwal S, Jain SK, Heron DE, Kim H,
Gerszten K, Edwards RP and Kelley JL: Clinical outcome with
adjuvant treatment of endometrial carcinoma using
intensity-modulated radiation therapy. Gynecol Oncol. 102:195–199.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Salama JK, Mundt AJ, Roeske J and Mehta N:
Preliminary outcome and toxicity report of extended-field,
intensity-modulated radiation therapy for gynecologic malignancies.
Int J Radiat Oncol Biol Phys. 65:1170–1176. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Beriwal S, Gan GN, Heron DE, Selvaraj RN,
Kim H, Lalonde R, Kelley JL and Edwards RP: Early clinical outcome
with concurrent chemotherapy and extended-field,
intensity-modulated radiotherapy for cervical cancer. Int J Radiat
Oncol Biol Phys. 68:166–171. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Small W Jr, Mell LK, Anderson P, et al:
Consensus guidelines for delineation of clinical target volume for
intensity-modulated pelvic radiotherapy in postoperative treatment
of endometrial and cervical cancer. Int J Radiat Oncol Biol Phys.
71:428–434. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jhingran A, Salehpour M, Sam M, Levy L and
Eifel PJ: Vaginal motion and bladder and rectal volumes during
pelvic intensity-modulated radiation therapy after hysterectomy.
Int J Radiat Oncol Biol Phys. 82:256–262. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Taylor A and Powell ME: An assessment of
interfractional uterine and cervical motion: Implications for
radiotherapy target volume definition in gynaecological cancer.
Radiother Oncol. 88:250–257. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
van de Bunt L, Jürgenliemk-Schulz IM, de
Kort GA, Roesink JM, Tersteeg RJ and van der Heide UA: Motion and
deformation of the target volumes during IMRT for cervical cancer.
What margins do we need? Radiother Oncol. 88:233–240. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Haripotepornkul NH, Nath SK, Scanderbeg D,
Saenz C and Yashar CM: Evaluation of intra- and inter-fraction
movement of the cervix during intensity modulated radiation
therapy. Radiother Oncol. 98:347–351. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Buchali A, Koswig S, Dinges S, Rosenthal
P, Salk J, Lackner G, Böhmer D, Schlenger L and Budach V: Impact of
the filling status of the bladder and rectum on their integral dose
distribution and the movement of the uterus in the treatment
planning of gynaecological cancer. Radiother Oncol. 52:29–34. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ahmad R, Hoogeman MS, Quint S and Mens JW:
deP ree I and Heijmen BJ: Inter-fraction bladder filling variations
and time trends for cervical cancer patients assessed with a
portable 3-dimensional ultrasound bladder scanner. Radiother Oncol.
89:172–179. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chan P, Dinniwell R, Haider MA, Cho YB,
Jaffray D, Lockwood G, Levin W, Manchul L, Fyles A and Milosevic M:
Inter- and intrafractional tumor and organ movement in patients
with cervical cancer undergoing radiotherapy, A cinematic-MRI
point-of-interest study. Int J Radiat Oncol Biol Phys.
70:1507–1515. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kerkhof EM, van der Put RW, Raaymakers BW,
van der Heide UA, Jürgenliemk-Schulz IM and Lagendijk JJ:
Intrafraction motion in patients with cervical cancer: The benefit
of soft tissue registration using MRI. Radiother Oncol. 93:115–121.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hammoud R, Patel SH, Pradhan D, Kim J,
Guan H, Li S and Movsas B: Examining margin reduction and its
impact on dose distribution for prostate cancer patients undergoing
daily cone-beam computed tomography. Int J Radiat Oncol Biol Phys.
71:265–273. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Showalter TN, Nawaz AO, Xiao Y, Galvin JM
and Valicenti RK: A cone beam CT-based study for clinical target
definition using pelvic anatomy during postprostatectomy
radiotherapy. Int J Radiat Oncol Biol Phys. 70:431–436. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Brock KK, Hawkins M, Eccles C, Moseley JL,
Moseley DJ, Jaffray DA and Dawson LA: Improving image-guided target
localization through deformable registration. Acta Oncol.
47:1279–1285. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ding GX, Duggan DM, Coffey CW, Deeley M,
Hallahan DE, Cmelak A and Malcolm A: A study on adaptive IMRT
treatment planning using kV cone-beam CT. Radiother Oncol.
85:116–125. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kerkhof EM, Raaymakers BW, van der Heide
UA, van de Bunt L, Jürgenliemk-Schulz IM and Lagendijk JJ: Online
MRI guidance for healthy tissue sparing in patients with cervical
cancer: An IMRT planning study. Radiother Oncol. 88:241–249. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jürgenliemk-Schulz IM, Toet-Bosma MZ, de
Kort GA, Schreuder HW, Roesink JM, Tersteeg RJ and van der Heide
UA: Internal motion of the vagina after hysterectomy for
gynaecological cancer. Radiother Oncol. 98:244–248. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Stam MR, van Lin EN, van der Vight LP,
Kaanders JH and Visser AG: Bladder filling variation during
radiation treatment of prostate cancer: Can the use of a bladder
ultrasound scanner and biofeedback optimize bladder filling? Int J
Radiat Oncol Biol Phys. 65:371–377. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
O'Doherty UM, McNair HA, Norman AR, et al:
Variability of bladder filling in patients receiving radical
radiotherapy to the prostate. Radiother Oncol. 79:335–340. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lim K, Kelly V, Stewart J, et al: Pelvic
radiotherapy for cancer of the cervix: Is what you plan actually
what you deliver? Int J Radiat Oncol Biol Phys. 74:304–312. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kavanagh BD, Schefter TE, Wu Q, Tong S,
Newman F, Arnfield M, Benedict SH, McCourt S and Mohan R: Clinical
application of intensity-modulated radiotherapy for locally
advanced cervical cancer. Semin Radiat Oncol. 12:260–271. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chen MF, Tseng CJ, Tseng CC, Kuo YC, Yu CY
and Chen WC: Clinical outcome in posthysterectomy cervical cancer
patients treated with concurrent cisplatin and intensity-modulated
pelvic radiotherapy, Comparison with conventional radiotherapy. Int
J Radiat Oncol Biol Phys. 67:1438–1444. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ma DJ, Michaletz-Lorenz M, Goddu SM and
Grigsby PW: Magnitude of interfractional vaginal cuff movement,
Implications for external irradiation. Int J Radiat Oncol Biol
Phys. 82:1439–1444. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Harris EE, Latifi K, Rusthoven C, Javedan
K and Forster K: Assessment of organ motion in postoperative
endometrial and cervical cancer patients treated with
intensity-modulated radiation therapy. Int J Radiat Oncol Biol
Phys. 81:e645–e650. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tyagi N, Lewis JH, Yashar CM, Vo D, Jiang
SB, Mundt AJ and Mell LK: Daily online cone beam computed
tomography to assess interfractional motion in patients with intact
cervical cancer. Int J Radiat Oncol Biol Phys. 80:273–280. 2011.
View Article : Google Scholar : PubMed/NCBI
|