Introduction
Central bronchogenic carcinoma is usually
accompanied with cancerous invasion of the main bronchus and
pulmonary artery, and therefore the surgical operation to be
performed requires bronchial anastomosis and pulmonary angioplasty,
which are performed by traditional thoracotomy.
Video-assisted thoracoscopic surgery (VATS) is an
emerging technology in minimally invasive surgery, which provides
painless surgery with a short recovery time. Bronchial anastomosis
and pulmonary angioplasty may be completed using VATS. The
worldwide experience with VATS lobectomy is now sufficiently robust
to enable a comparison of this procedure to be made with
traditional thoracotomy. In all five lobes of the lung, the stage
of the operation that has the greatest difficulty is VATS sleeve
left upper lobectomy for the special anatomical structure. In the
present case report, and application of VATS for the treatment of
central lung cancer of the upper lobe with invasion of the main
bronchus and pulmonary artery is presented.
Case report
All procedures used in the present case study were
approved by the Clinical Medical Research Ethics Committee of the
First Affiliated Hospital of Anhui Medical University (Hefei,
China).
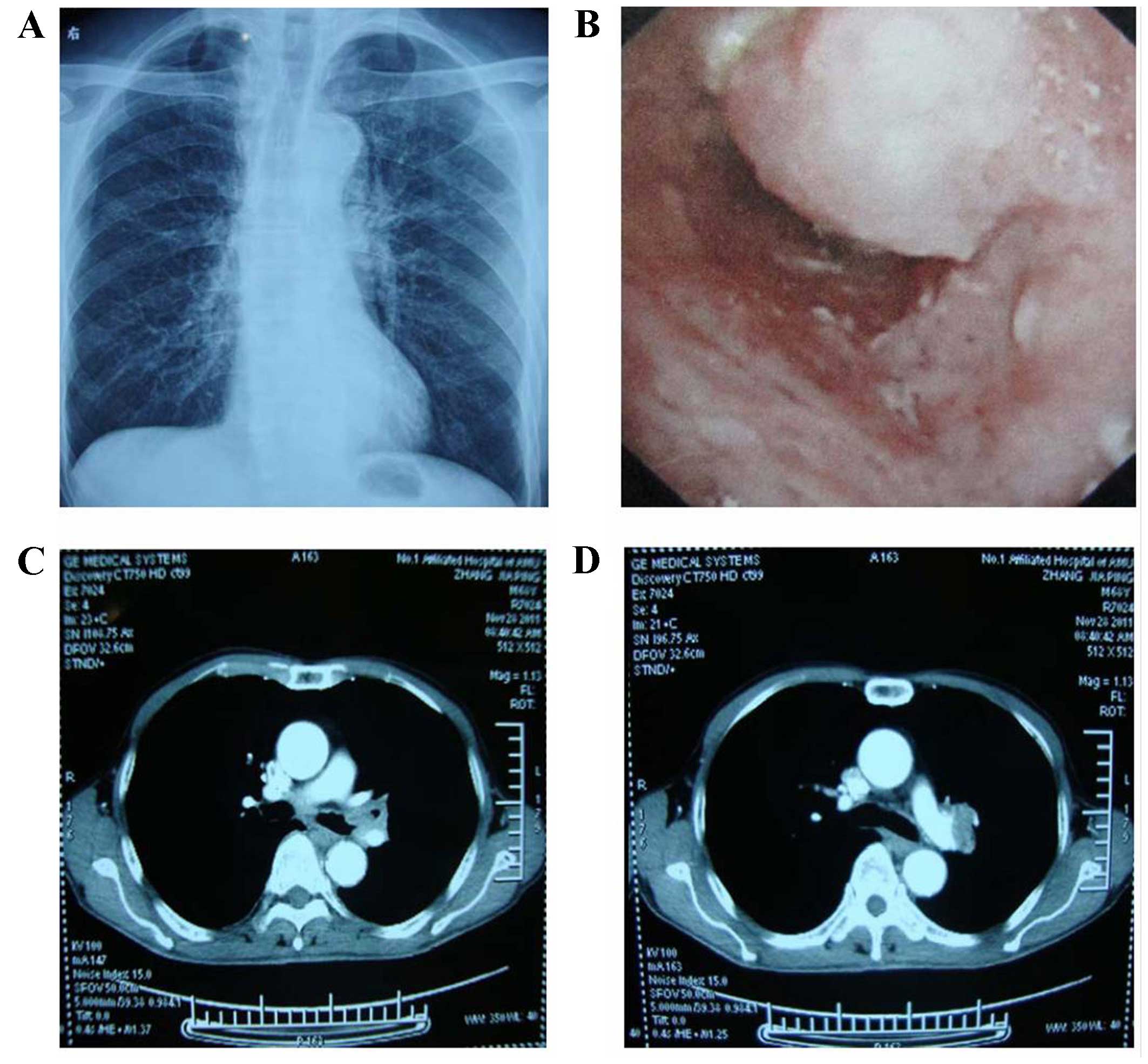
A 68-year-old man whose smoking history was 15–20
cigarettes per day for 40 years presented with a cough and
hemoptysis. In November 2011, the patient was found to have an
abnormal shadow in the left pulmonary hilum, based on a chest X-ray
(Fig. 1A), and so the patient was
referred to our hospital (The First Affiliated Hospital of Anhui
Medical University, Hefei, China) for further examination and
therapy. Physical examination revealed that there were no palpable
superficial lymph nodes. Blood chemistry data were unremarkable,
with the exception of a decreased level of total protein (TPR) of
56.1 g/l (normal range, 60.0–80.0 g/l) and a slightly increased
level of total bilirubin to 19.0 µmol/l (normal range, 5.1–19.0
µmol/l). The tumor markers for squamous cell carcinoma (SCC)
antigen (normal range, 0–2 ng/ml), sialyl SSEA-1 antigen (SLX;
normal range, 0–38 U/ml), and neuron-specific enolase (NSE; normal
range, 0–10 ng/ml) were slightly increased to 2.6 ng/ml, 44.3 U/ml
and 10.12 ng/ml, respectively. Bronchoscopy revealed an occlusion
in the distal portion of the left main bronchus by a
cauliflower-like mass (Fig. 1B). An
enhanced computed tomography (CT) scan (Siemens SOMATOM Definition
AS 64-slice computed tomography system; Siemens Healthineers,
Erlangen, Germany) revealed a well-defined mass of soft tissue,
with a coarse edge measuring 3.8×4.2×4.0 cm, in the upper lobe of
the left lung close to the hilum, and enlarged mediastinal lymph
nodes were also identified. The mass appeared to be located on the
left upper lobe bronchus, and have pulmonary artery invasion
(Fig. 1C and D). Pulmonary function
tests revealed a moderate obstructive ventilatory disorder and
severe abnormality of small airway function. Considering all the
results collectively, the preoperative stage of the tumor was
assessed to be cT2, N2, M0, IIIA, and the patient was proposed for
a VATS lobectomy.
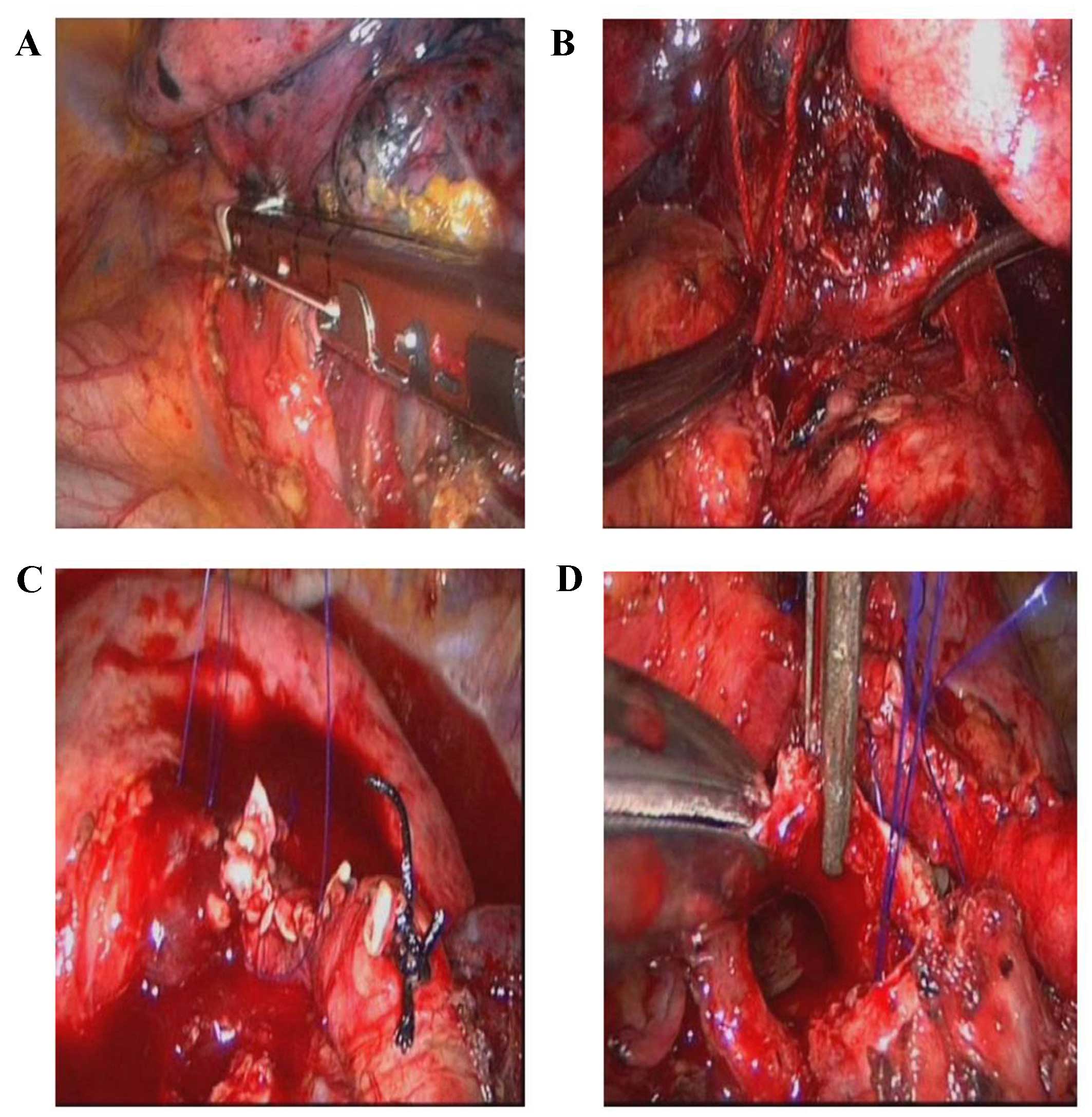
The patient was placed in the right-lateral
decubitus position. A 3.5 cm incision was made as the main
operating hole in the third intercostal space of the anterior
axillary line position. A thoracoscopic observation hole was made
using a 12 cm trocar in the eighth intercostal space of the
midaxillary line. In addition, a 3.5 cm incision was made as the
operational assist hole, and a further 12 cm trocar was placed in
the fifth intercostal space of the posterior axillary line
position. A complete fissure was identified. Digital palpation
confirmed the presence of a mass in the left upper lobe. The
instruments were inserted to start the dissection of the pulmonary
ligament and mediastinal pleura, and the superior pulmonary vein
was exposed and resected using a 45 mm white linear stapler
(Fig. 2A). Amputation of the
pulmonary fissure was performed using an endoscopic linear cutter
scalpel (Endo-GIA™; Covidien LLC, Mansfield, MA, USA), and it was
possible to observe that the carcinoma located on the left main
bronchus had partly invaded the left pulmonary artery. After having
cut and freed the left main bronchus, the left pulmonary artery was
freed and blocked (Fig. 2B). The
left upper lobe was removed in a protective bag, and a systematic
lymph node dissection was completed.
The left pulmonary artery was repaired using a
reciprocating continuous 4–0 Prolene® suture (Fig. 2C). The proximal occlusion clamp was
opened, and subsequently the telecentric end occlusion clamp was
opened to make the pulmonary perfusion. After the inferior
pulmonary ligament had been divided to release the tension of
airway anastomosis, end-to-end anastomosis was initiated. The
midpoint of the offside wall of the bronchus was chosen as the
starting point, then a 3–0 Prolene® continuous suture
was used to close the membranous and bronchial cartilage from the
posterior to the anterior end, dragging them tight simultaneously
with the help of an endoscopic knot-pusher. Following the
completion of all the procedures, the left lung was inflated, and
air leakage did not occur.
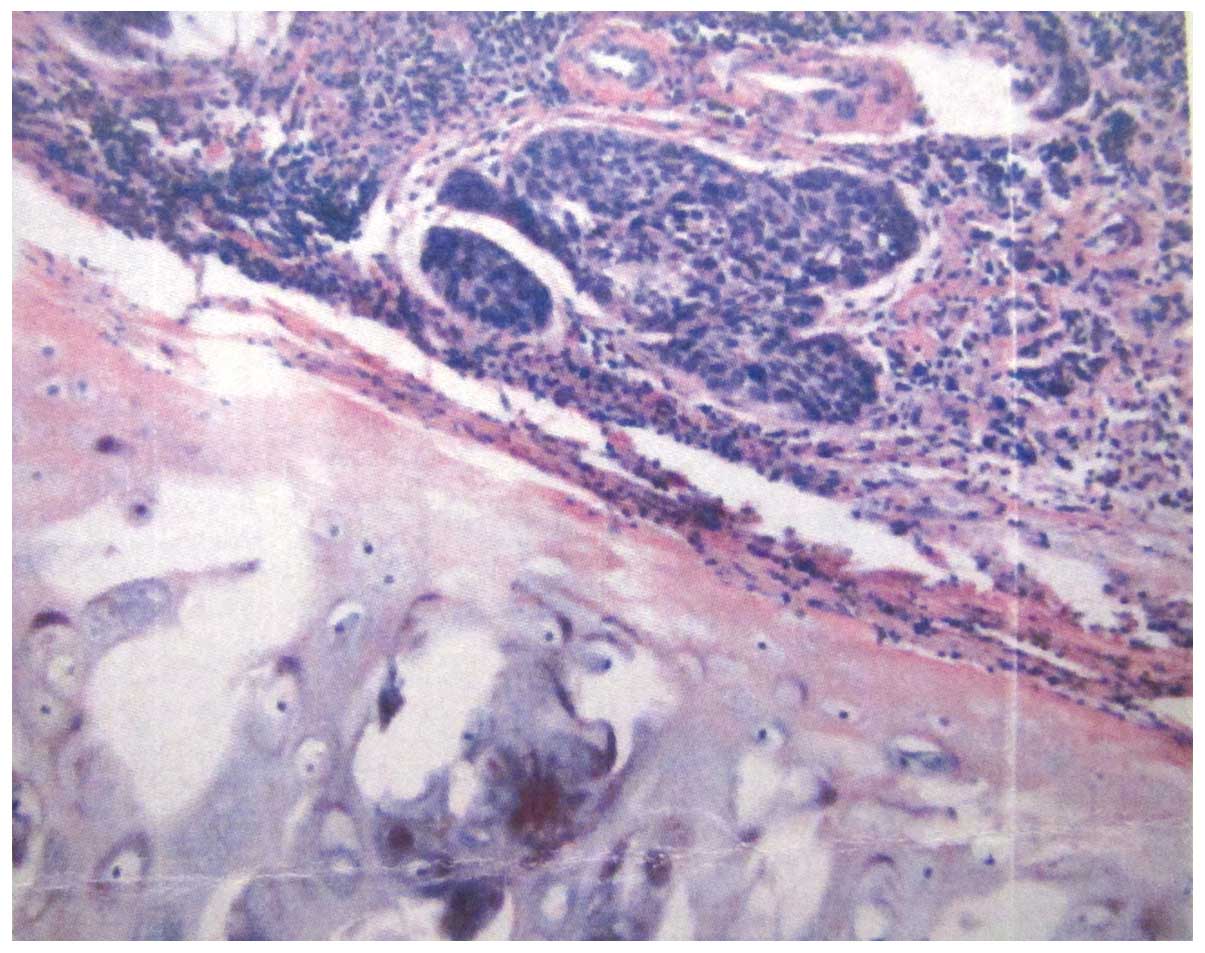
The intraoperative bleeding volume was 120 ml, and
no intraoperative complications occurred. The pathological
examination revealed a 2.6×1.7×2.7 cm solid carcinoma, which the
resultant microscopic examination identified as SCC (Fig. 3) with one hilar lymph node
involvement (a total of seven lymph nodes were studied), leading us
to consider that the postoperative stage was pT2, N1, M0, IIB.
Thoracic drainage tubes were removed on the eighth postoperative
day, and the patient was discharged from the hospital on the ninth
postoperative day.
Discussion
It is now well established that, with the
improvements in technique and instrumentation, VATS has become a
replacement method of choice for a number of procedures that were
formerly carried out via thoracotomy (1). The advantages of VATS for lobectomy
have been previously reported, including reduced perioperative
pain, shorter hospital stays, a more rapid resumption of normal
daily activities, less impairment of pulmonary and shoulder
function, reduced rates of cytokine release, and an improved
delivery of adjuvant chemotherapy (2). Central bronchogenic carcinoma often
invades the bronchus and pulmonary artery, and sleeve lobectomy
with pulmonary arterioplasty or bronchoplasty were traditionally
performed with a posterolateral thoracotomy (3). Formerly, sleeve resection has been
viewed as a contraindication to VATS lobectomy. However, recently
VATS sleeve lobectomy was considered as the preferred minimally
invasive method in view of its higher operation safety, lower
complications, decreased pain and improved quality of life,
particularly when the patients presented with long-term smoking,
chronic obstructive pulmonary disease and poor pulmonary function,
as previously described (4).
Han et al (5,6)
hypothesized that, compared with the open surgery, the VATS
procedure would generally be likely to be more technically
challenging for the transmission from the direct view to a local
two-dimensional screen, and from multi-angle, multi-direction
operational field to one directional operation field. Therefore, in
comparative terms, a markedly clearer anatomical view of the
travel, distribution and variation of the pulmonary vessels was
required. In addition, others have argued that, in VATS lobectomy,
when all the five lobes are considered, the biggest difficulty of
the operation resides with a VATS left upper lobectomy due to the
deep location, special operation angle and predominant vessel
invasion of the tumor, particularly central-type pulmonary tumors
(7). However, as with all other
procedures, VATS sleeve lobectomy has had its own learning curve
for surgeons. With the accumulation of experience, continuous
suture has been able to be used to complete both membranous
bronchus and cartilage anastomosis at one time through thoractomy.
Consequently, surgeons have been able to perform continuous suture
to complete end-to-end anastomosis using VATS, and to avoid
tangling the untied ends.
Additionally, it was our opinion that the left
pulmonary artery could more easily be prone to tumor invasion since
the left pulmonary artery trunk is shorter, although it has more
branches with more fissions and cross-sections. The left pulmonary
artery is not shielded by other vessels lying ahead of it, but the
right pulmonary artery is shielded by the superior vena cava. In
comparison with the right pulmonary artery, the left pulmonary
artery is more readily exposed to invasion by the central type
pulmonary carcinoma in the left upper lobe. In order to reserve
more pulmonary tissue, it was necessary to perform a pulmonary
angioplasty. Routinely, pulmonary arterioplasty comprises four
operational modes, namely, direct suture, pericardial patch
angioplasty, end-to-end anastomosis and pericardial tube
replacement (8). From the technical
perspective, direct suture appeared to be the most feasible to
perform. However, the principle of a successful direct suture is to
guarantee that there are no obstructions, and no stenosis for the
distal section of the artery; otherwise, pericardial patch
angioplasty or end-to-end anastomosis ought to be performed instead
(9). However, it was our opinion
that, courtesy of the improvements in operational proficiency and
surgical instruments, the other three operational modes are also
able to be completed using VATS.
The success of totally VATS bronchial sleeve
lobectomy and pulmonary angioplasty for the left upper lobe would
offer more central type lung carcinoma patients the opportunity to
accept the minimally invasive operation, and expand the operation
indication of totally VATS lobectomy. Our hope is that total VATS
bronchial sleeve and pulmonary angioplasty lobectomy will obtain a
more widespread application for the surgical treatment of central
type lung carcinoma in the future.
Two major conclusions may be drawn from the present
case report: i) Simultaneous end-to-end anastomosis of bronchus and
pulmonary angioplasty may be completed using VATS. This indicates
that VATS is applicable for the treatment of central bronchogenic
carcinoma with invasion of the main bronchus and pulmonary artery;
and ii) with the improvements in operational proficiency and
surgical instruments, more complicated surgical procedures may also
be completed using VATS; therefore, the surgical indications are
that the applicability of VATS lobectomy as a technique will be
expanded in the future.
References
|
1
|
Schmid T, Augustin F, Kainz G, Pratschke J
and Bodner J: Hybrid video-assisted thoracic surgery-robotic
minimally invasive right upper lobe sleeve lobectomy. Ann Thorac
Surg. 91:1961–1965. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yamashita Y, Harada H and Misumi K:
Video-assisted thoracic surgery lobectomy for lung cancer: The
point at issue. Gen Thorac Cardiovasc Surg. 59:164–168. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nakanishi R, Fujino Y, Oka S and Odate S:
Video-assisted thoracic surgery involving major pulmonary resection
for central tumors. Surg Endosc. 24:161–169. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Predina JD, Kunkala M, Aliperti LA,
Singhal AK and Singhal S: Sleeve lobectomy: Current indications and
future directions. Ann Thorac Cardiovasc Surg. 16:310–318.
2010.PubMed/NCBI
|
|
5
|
Han Y, Zhou S, Yu D, Song X and Liu Z:
Video-assisted left upper bronchial sleeve lobectomy. J Thorac Dis.
5(Suppl 3): S304–S631. 2013.PubMed/NCBI
|
|
6
|
Han Y, Zhou S, Yu D, Song X and Liu Z:
Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy
with partial pulmonary artery resection. J Thorac Dis. 5(Suppl 3):
S301–S331. 2013.PubMed/NCBI
|
|
7
|
Gonzalez-Rivas D, de la Torre M, Fernandez
R and Mosquera VX: Single-port video- assisted thoracoscopic left
upper lobectomy. Interact Cardiovasc Thorac Surg. 13:539–541. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
de Leyn P and Decker G: Surgical treatment
of non-small cell lung cancer. Rev Mal Respir. 21(5)1971–982. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Okada M, Tsubota N, Yoshimura M, Miyamoto
Y, Matsuoka H, Satake S and Yamagishi H: Extended sleeve lobectomy
for lung cancer: The avoidance of pneumonectomy. J Thorac
Cardiovasc Surg. 118:710–714. 1999. View Article : Google Scholar : PubMed/NCBI
|