Introduction
DF of the bone is an extremely rare, lytic, locally
aggressive but non-metastatic primary bone tumor. Histologically,
DF consists of wavy fibroblasts and abundant collagenous tissue,
bears a close resemblance to a desmoid tumor of the soft tissues
and exhibits a characteristic production of collagen fibers
(1). DF may involve any bone, but is
most often found in the mandible (22%) and less frequently in the
femur (15%), pelvic bones (13%), radius (12%) and tibia (9%)
(2,3).
The incidence of DF is estimated to be 0.06% among
all bone tumors and 0.3% among benign bone tumors (1,3–5). DF of the bone most often occurs during
the first three decades of life and exhibits no gender predilection
(6). The most common symptoms
include pain and swelling, and 12% of the patients present with
pathological fractures. However, a number of patients may be
asymptomatic; thus, the tumor is often incidentally identified
(7).
On radiographs, the lesion is lytic, occasionally
with poorly defined borders, while on computed tomography (CT) it
is mildly hyperdense, with thin sclerotic margins, with or without
destruction of the contiguous cortex, and exhibits low signal
intensity on T2-weighted magnetic resonance imaging (MRI). The
diagnosis of DF is predominantly based on pathological examination.
The recurrence rates in patients treated with and without resection
are 17 and 55–72%, respectively (7).
This disease was first identified by Jaffe in 1958
(8). To date, ~200 cases of
desmoplastic fibroma of the bone have been reported in the
literature; of these, 13 have been reported in the femur (9–20), with
only 2 in the proximal femur (9,14) and
the remaining in the distal femur (10–13,15–18,20,21).
Image-guided percutaneous biopsy is becoming an
increasingly accepted modality for initial diagnosis in the
majority of musculoskeletal tumors. However, despite its
well-documented specificity and sensitivity (22,23),
there has been continued reluctance on the part of orthopedic
oncologists to accept this technique as the modality of choice for
initial biopsy in primary bone tumors. Detractors of percutaneous
needle biopsy suggest that sufficient material cannot be obtained
to ensure an accurate diagnosis, particularly in patients with
sclerotic bone lesions (24).
Historically, all biopsies to date were performed via an open
surgical biopsy, which remains the gold standard for a proportion
of physicians. The reported accuracy of an open surgical biopsy,
whether incisional or excisional, is 98% (23,25),
whereas needle biopsy under CT guidance has a reported accuracy
estimated between 78 and 98.4% (26).
The needle pathway is determined on the basis of the
expected definitive treatment, in order to avoid intercompartmental
contamination, minimize the amount of biopsy tract to be removed at
the time of definitive surgery in case of malignancy, and avoid
neurovascular structures. The choice of CT vs. fluoroscopy is
generally determined on the basis of three factors, namely size,
location and attenuation (27).
To the best of our knowledge, this study presents
the only published case of minimally invasive diagnosis of DF of
the bone. Written informed consent was obtained from the patient
for the publication of the case details.
Case report
In August 2015, a 36-year-old African female patient
presented to the Emergency Room of Arcispedale Santa Maria
Nuova-IRCCS (Reggio Emilia, Italy), which is a medium-sized general
hospital, complaining of pain in the rib cage, knees and lower
thighs following a mild trauma she had suffered a few days earlier
after a fall, for which she had not been hospitalized. There were
no evident abnormalities on physical examination, with the
exception of pain on percussion. Radiography showed a well-defined,
eccentric, low-density lesion in the distal metaphysis of the left
tibia (Fig. 1), adherent to the
external cortex. The contiguous cortex was apparently not eroded,
but minimally thinned due to compression by the expanding tumor.
The margins were intact and sclerotic. The initial diagnosis on
admission, based on radiological evidence, was bone fibroma. The
patient was advised on an outpatient basis to undergo a magnetic
resonance imaging (MRI) scan and a subsequent orthopedic
evaluation.
Due to the X-ray and bone MRI results, the
orthopedic surgeon suggested an image-guided bone biopsy.
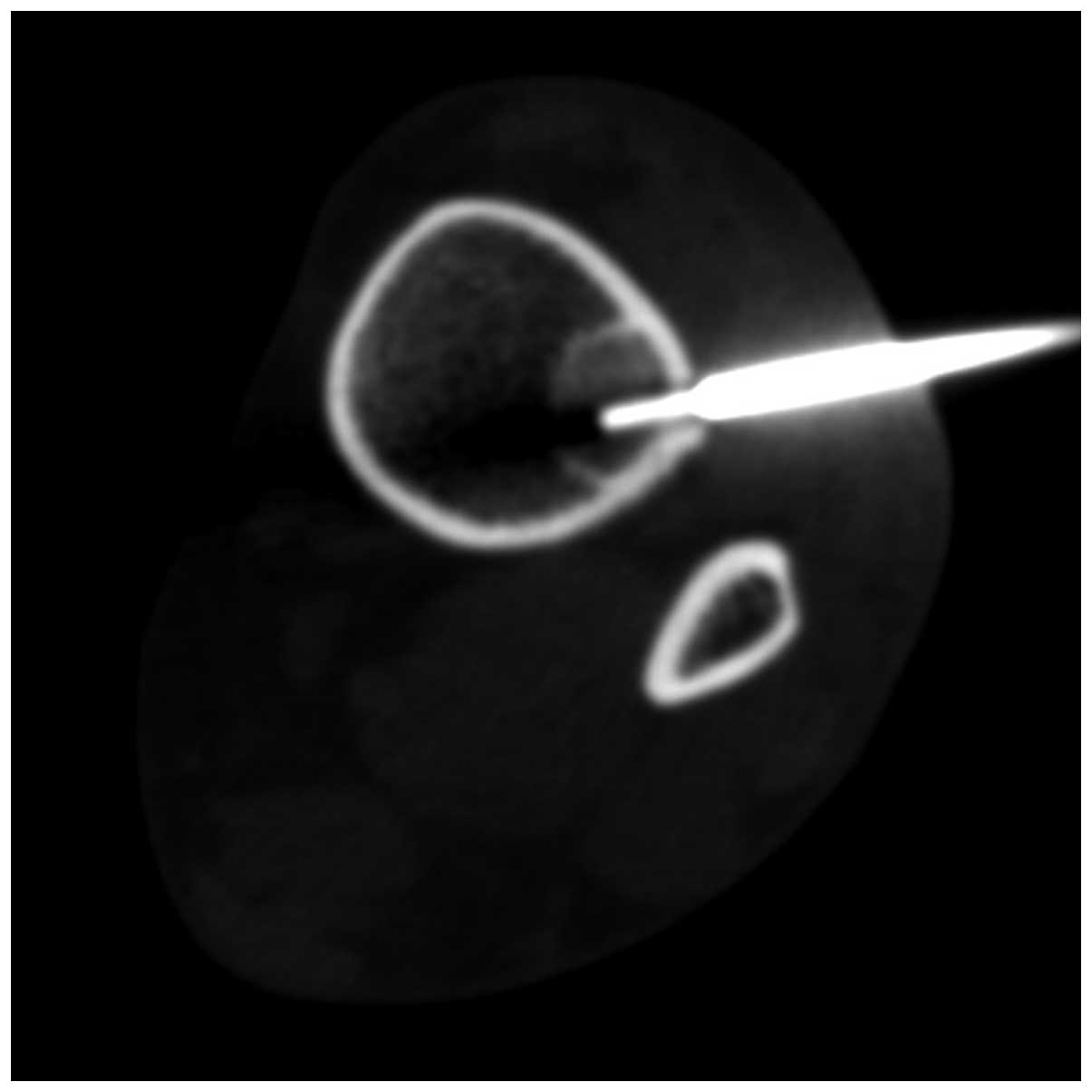
After a CT scan confirmed the location and imaging
characteristics of the lesion (solid, well-circumscribed, no cortex
erosions), local anesthesia with lidocaine was administered, a
17-gauge bone biopsy needle (Osteo-Site Ratchet; Cook Medical,
Limerick, Ireland) was inserted, passing through the anterolateral
face of the skin overlying the tibia, the tibialis anterior muscle
and, finally, the cortex, into the core of the lesion (Fig. 2) and a single specimen was extracted.
Since no peri-procedural complications occurred, the patient was
discharged after a few hours in good health and without the need
for oral pain medication, with the recommendation to refer to her
general practitioner in case of any discomfort. Histological
examination of the bone specimen revealed focal peripheral
proliferation of spindle-shaped cells resembling fibroblasts,
showing strong reactivity for anti-vimentin antibody; the
appearance was in accordance with a fibroblastic desmoid tumor of
the bone.
Discussion
Percutaneous needle bone biopsy is a safe and
accurate method (22,25,27–29) for
obtaining a tissue diagnosis. In general, better results are
obtained with lesions of the extremities or pelvis compared with
those in the spine (30).
Percutaneous needle biopsies have a very low complication rate
(1.1%), whereas open biopsy has a complication rate of ≤16%
(31).
A serious complication of percutaneous biopsy is the
risk of seeding malignant cells along the needle track,
particularly if the lesion is a sarcoma, which would necessitate
resection of the needle track en bloc with the tumor in
limb-sparing reconstructive surgery (32). Thus, selecting the appropriate needle
path is critical for limb-salvaging procedures. Fine-needle
aspiration (FNA) may differentiate between a metastasis and a
benign lesion; however, core biopsy is superior to FNA in
determining cell type and tumor grade, which is necessary for the
diagnosis of primary bone tumor. In our experience, of the various
options that are available for bone biopsy (33), the Osteo-Site Ratchet (Cook Medical)
13-gauge coaxial bone biopsy system is effective in obtaining
tissue from sclerotic lesions where normal bone cortex needs to be
traversed. In general, all bone biopsies are performed under local
anesthesia; however, conscious sedation may be required in children
or uncooperative patients. An adequate biopsy sample is considered
to be that providing adequate abnormal tissue for the pathologist
to reliably make a diagnosis. We have found that, despite the low
incidence of DF, a single long core of abnormal tissue obtained
with a 13-gauge needle is sufficient.
In conclusion, this study reported the case of a
36-year-old African female patient with a DF of the bone
incidentally detected by an X-ray and diagnosed by means of
percutaneous CT-guided bone biopsy. This case differs from other
published studies due to the minimally invasive, preoperative,
image-guided histological diagnosis. This type of diagnosis is
commonly made based on a resection sample obtained through
incisional biopsy under general anesthesia. The results of
image-guided biopsy in terms of cost-to-benefit ratio are similar
to those of open biopsy, with reduced comparable morbidity.
References
|
1
|
Böhm P, Kröber S, Greschniok A, Laniado M
and Kaiserling E: Desmoplastic fibroma of the bone. A report of two
patients, review of the literature, and therapeutic implications.
Cancer. 78:1011–1023. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fletcher CDM, Uni KK and Mertens F:
Pathology and genetics of tumors of soft tissue and boneWHO
classification of tumors. IARC Press; Lyon: pp. 2882002
|
|
3
|
Said-Al-Naief N, Fernandes R, Louis P,
Bell W and Siegal GP: Desmoplastic fibroma of the jaw: A case
report and review of literature. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 101:82–94. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rabin D, Ang LC, Megyesi J, Lee DH and
Duggal N: Desmoplastic fibroma of the cranium: Case report and
review of the literature. Neurosurgery. 52:950–954; discussion 954.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ikeshima A and Utsunomiya T: Case report
of intra-osseous fibroma: A study on odontogenic and desmoplastic
fibromas with a review of the literature. J Oral Sci. 47:149–157.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Crim JR, Gold RH, Mirra JM, Eckardt JJ and
Bassett LW: Desmoplastic fibroma of bone: Radiographic analysis.
Radiology. 172:827–832. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hauben E and Cleton-Jansen AM: Fibrogenic
tumours: Desmoplastic fibroma of boneWHO Classification of Tumours
of Soft Tissue and Bone. Fletcher CDM, Bridge JA, Hogendoorn P and
Mertens F: 4th. IARC; Lyon: pp. 2982013
|
|
8
|
Jaffe HL: Tumors and tumorous conditions
of the bones and jointsThe American Journal of the Medical
Sciences. Lea & Febiger; Philadelphia: 1958
|
|
9
|
Lichtman EA and Klein MJ: Case report 302.
Desmoplastic fibroma of the proximal end of the left femur.
Skeletal Radiol. 13:160–163. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wadhwa V, Suh KJ, Yi JH and Chhabra A:
Incidental lesion in the femoral metaphysis. Desmoplastic fibroma
of the bone. Skeletal Radiol. 42:1739–1740, 1775–1776. 2013.
View Article : Google Scholar
|
|
11
|
Clayer M and Oakeshott R: Allograft bone
in the treatment of desmoplastic fibroma. A case report. Clin
Orthop Relat Res. 219–224. 1994.PubMed/NCBI
|
|
12
|
Rastogi S, Varshney MK, Trikha V, Khan SA
and Mittal R: Desmoplastic fibroma: A report of three cases at
unusual locations. Joint Bone Spine. 75:222–225. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chan KW, Pun WK and Choi CH: Desmoplastic
fibroma of bone. Pathology. 19:201–203. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Grube-Pagola P and Valle-Landa JC:
Desmoplastic fibroma of the femur. Radiologia. 55:359–361. 2013.(In
Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Doya H and Yaoita M: Case of desmoplastic
fibroma in the femur. Seikei Geka. 17:754–756. 1966.(In Japanese).
PubMed/NCBI
|
|
16
|
Matsumori S, Watabe E, Toyoshima Y and
Yagi Y: Primary desmoplastic fibroma of the femur. Seikei Geka.
23:275–281. 1972.(In Japanese). PubMed/NCBI
|
|
17
|
Bertoni F, Calderoni P, Bacchini P and
Campanacci M: Desmoplastic fibroma of bone. A report of six cases.
J Bone Joint Surg Br. 66:265–268. 1984.PubMed/NCBI
|
|
18
|
Petrovichev NN, Filippova NA,
Annamukhammedov A and Karapetian RM: Case of desmoplastic fibroma
of the femur. Arkh Patol. 47:55–58. 1985.(In Russian). PubMed/NCBI
|
|
19
|
Nielsen GP, O'Connell JX, Dickersin GR and
Rosenberg AE: Collagenous fibroma (desmoplastic fibroblastoma): A
report of seven cases. Mod Pathol. 9:781–785. 1996.PubMed/NCBI
|
|
20
|
Gao S, Cai Q, Yao W, Wang J, Zhang P and
Wang X: Desmoplastic (collagenous) fibroma of the femur: A case
report and review of the literature. Oncol Lett. 6:1285–1288.
2013.PubMed/NCBI
|
|
21
|
Yokouchi M, Ueno Y, Nagano S, Shimada H,
Nakamura S, Setoguchi T, Kawamura I, Ishidou Y and Komiya S:
Extended curettage and heat ablation for desmoplastic fibroma of
the distal femur with a 12-year follow-up period: A case report.
Oncol Lett. 8:1103–1106. 2014.PubMed/NCBI
|
|
22
|
Fraser-Hill MA and Renfrew DL:
Percutaneous needle biopsy of musculoskeletal lesions. 1. Effective
accuracy and diagnostic utility. AJR Am J Roentgenol. 158:809–812.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dupuy DE, Rosenberg AE, Punyaratabandu T,
Han MH and Mankin HJ: Accuracy of CT-guided needle biopsy of
musculoskeletal neoplasms. AJR Am J Roentgenol. 171:759–762. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mankin HJ, Mankin CJ and Simon MA: The
hazards of biopsy, revisited. Members of the musculoskeletal tumor
society. J Bone Joint Surg Am. 78:656–663. 1996.PubMed/NCBI
|
|
25
|
Altuntas AO, Slavin J, Smith PJ, Schlict
SM, Powell GJ, Ngan S, Toner G and Choong PF: Accuracy of computed
tomography guided core needle biopsy of musculoskeletal tumours.
ANZ J Surg. 75:187–191. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Rimondi E, Rossi G, Bartalena T, Ciminari
R, Alberghini A, Ruggieri P, Errani C, Angelini A, Calabrò T, Abati
CN, et al: Percutaneous CT-guide biopsy of the musculoskeletal
system: Results of 2027 cases. Eur J Radiol. 77:34–42. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jelinek JS, Murphey MD, Welker JA, Henshaw
RM, Kransdorf MJ, Shmookler BM and Malawer MM: Diagnosis of primary
bone tumors with image-guided percutaneous biopsy: Experience with
110 tumors. Radiology. 223:731–737. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Leffler SG and Chew FS: CT-guided
percutaneous biopsy of sclerotic bone lesions: Diagnostic yield and
accuracy. AJR. 172:1389–1392. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ashford RU, McCarthy SW, Scolyer RA, Bonar
SF, Karim RZ and Stalley PD: Surgical biopsy with intraoperative
frozen section. An accurate and cost-effective method for diagnosis
of musculoskeletal sarcomas. J Bone Joint Surg Br. 88:1207–1211.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hau A, Kim I, Kattapuram S, Hornicek FJ,
Rosenberg AE, Gebhardt MC and Mankin HJ: Accuracy of CT-guided
biopsies in 359 patients with musculoskeletal lesions. Skeletal
Radiol. 31:349–353. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Welker JA, Henshaw RM, Jelinek J,
Shmookler BM and Malawer MM: The percutaneous needle biopsy is safe
and recommended in the diagnosis of musculoskeletal masses. Cancer.
89:2677–2686. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Anderson MW, Temple HT, Dussault RG and
Kaplan PA: Compartmental anatomy: Relevance to staging and biopsy
of musculoskeletal tumors. AJR Am J Roentgenol. 173:1663–1671.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Roberts CC, Morrison WB, Leslie KO,
Carrino JA, Lozevski JL and Liu PT: Assessment of bone biopsy
needles for sample size, specimen quality and ease of use. Skeletal
Radiol. 34:329–335. 2005. View Article : Google Scholar : PubMed/NCBI
|