Introduction
Eosinophilic pancreatitis (EP) is a rare form of
chronic pancreatitis characterized by localized or diffuse
eosinophilic infiltration of the pancreas and elevated serum
immunoglobulin (Ig) E levels. EP is difficult to distinguish from
pancreatic cancer on the basis of clinical symptoms and the results
of auxiliary examination alone. Therefore, the majority of the
patients undergo pancreatic surgery to confirm the diagnosis. We
herein describe 3 cases of EP patients who underwent
pancreatoduodenectomy due to a preoperative diagnosis of cancer of
the pancreatic head or choledochal cancer. The clinicopathological
characteristics or these EP patients were investigated in the
present study to improve our understanding of this disease and
reduce the rates of misdiagnosis and missed diagnosis.
Case report
Case 1
A 39-year-old man was admitted to The First
Affiliated Hospital of Harbin Medical University (Harbin, China) in
February, 2006 with a 2-week history of jaundice. The patient
denied drug and alcohol use, and had a negative history of
allergies. The physical examination was unremarkable, expect for
the yellowish skin and sclerae. The laboratory findings included a
percentage of peripheral blood eosinophils of 11%, total bilirubin
(TB) of 147.5 µmol/l and direct bilirubin (DB) of 87.4 µmol/l. The
B-ultrasound and computed tomography (CT) results revealed diffuse
enlargement of the pancreatic head, expansion of the intrahepatic
and extrahepatic bile ducts, and pancreatic duct dilatation. The
patient was diagnosed with pancreatic head cancer and underwent
pancreatoduodenectomy. Postoperatively, the pancreatic specimens
were enlarged and had a diffusely hard texture on cross section. A
gray mass measuring 2×2.3×1.5 cm with indistinct boundaries
appeared to constrict the pancreatic duct and common bile duct. On
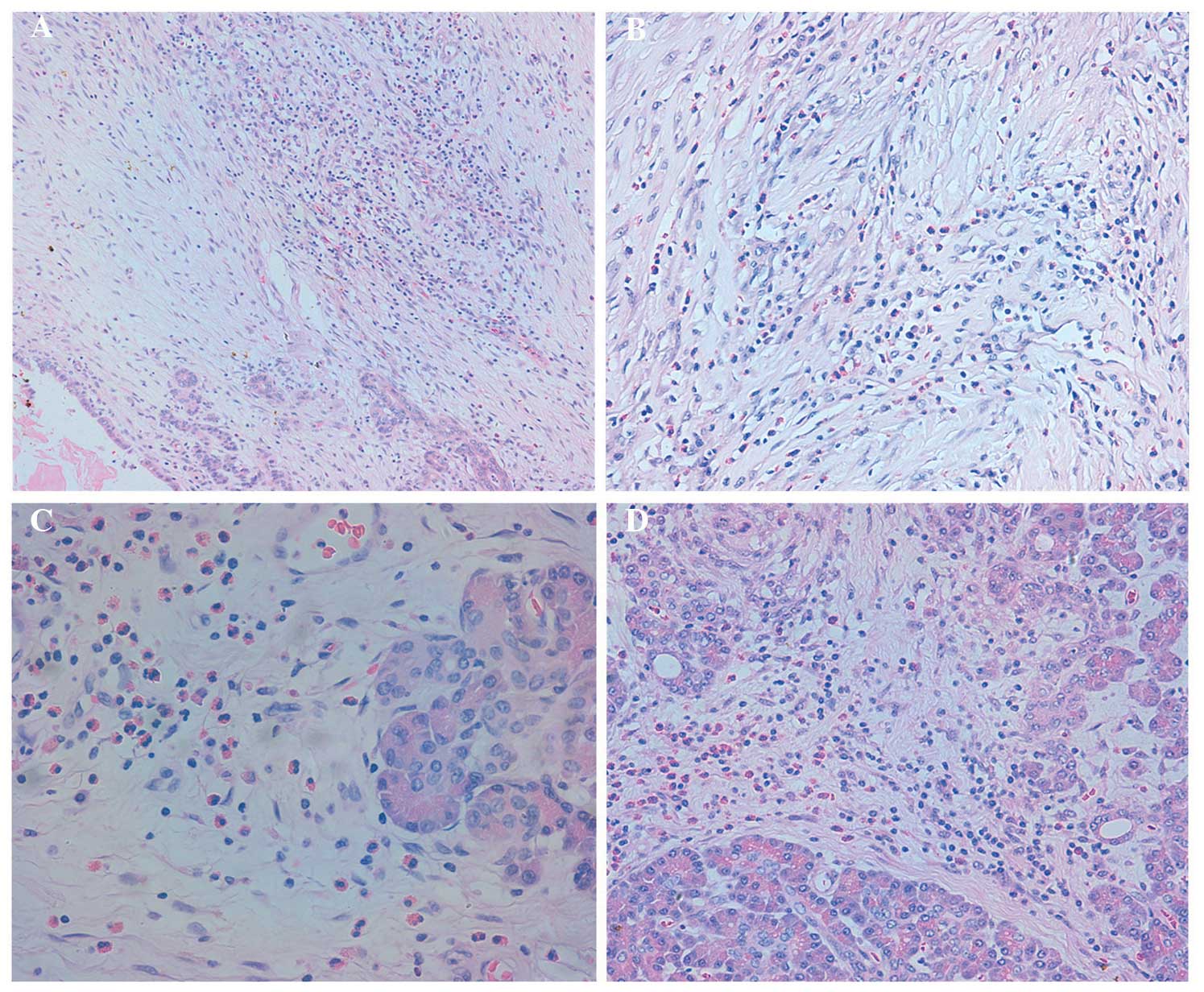
microscopic examination, there was diffuse inflammatory cell
infiltration of the pancreatic duct, acini and interstitium, mostly
by eosinophils and a few lymphocytes and plasma cells (Fig. 1A, C and D). Fibrous connective tissue
hyperplasia and collagenation were also observed (Fig. 1A and B). The patient tested negative
for parasites, rheumatism and autoimmune antibodies, which excluded
the possibility of autoimmune pancreatitis and parasitic infection.
A diagnosis of EP was made. The patient presented 2 months after
surgery with jaundice, TB of 116.5 µmol/l, DB of 82.6 µmol/l,
elevated serum IgE and normal IgG levels. The patient was treated
with 40 mg/day prednisone for 6 days, after which the jaundice
subsided.
Case 2
A 46-year-old man was admitted to our hospital in
June, 2010 with an 8-day history of jaundice and mild abdominal
pain. The patient had a history of asthma and denied alcohol and
medication use. The laboratory findings included a percentage of
peripheral blood eosinophils of 10%, TB of 127.2 µmol/l and DB of
77.6 µmol/l. The B-ultrasound and CT results revealed diffuse
enlargement of the pancreas and a low-density shadow in the
pancreatic head. Endoscopic retrograde cholangiopancreatography
(ERCP) revealed stenosis of the distal bile duct and pancreatic
duct at the head of the pancreas, and pancreatic duct dilatation
adjacent to the area of stenosis. The proposed diagnosis was
pancreatic head carcinoma and the patient underwent
pancreatoduodenectomy. Postoperatively, the pancreatic specimens
displayed an enlarged pancreatic head, with a diffusely hard
texture on cross section. A gray mass measuring 2×2.3×1.5 cm with
indistinct boundaries was detected, which appeared to constrict the
common bile duct. On microscopic examination, there was a diffuse
inflammatory cell infiltration of the pancreatic parenchyma and
interstitium, mostly consisting of eosinophils and a few
lymphocytes and plasma cells. Fibrous connective tissue hyperplasia
and collagenation were also observed. The patient tested negative
for parasites, rheumatism and autoimmune antibodies, which excluded
the possibility of autoimmune pancreatitis and parasite infection.
A diagnosis of EP was made.
Case 3
A 41-year-old woman was admitted to our institution
in June, 2013 with a 4-day history of abdominal pain, fatigue, loss
of appetite, weight loss, nausea, vomiting and jaundice. The
patient denied alcohol and medication use and had a negative
history of allergic diseases. The laboratory findings included a
peripheral blood eosinophil percentage of 3%, TB of 127.2 µmol/l
and DB of 97.6 µmol/l. The CT scan revealed intrahepatic and
extrahepatic bile duct dilatation and delayed enhancement of the
lower end of the common bile duct, A diagnosis of choledochal
cancer was made and the patient underwent pancreatoduodenectomy.
Postoperatively, the pancreatic specimens exhibited stenosis of the
intrapancreatic portion of the common bile duct, with a smooth
mucosa and absence of masses, surrounded by hardened pancreatic
tissue exhibiting a coarse granular texture on cross section.
Constriction of the common bile duct was observed. On microscopic
examination, there was an inflammatory cell infiltration of the
pancreatic parenchyma and interstitium, mostly by eosinophils and a
few lymphocytes and plasma cells. Fibrous connective tissue
hyperplasia and collagenation were also observed. The IgE and IgG
levels were within the normal range and the patient tested negative
for parasites, rheumatism and autoimmune antibodies. A diagnosis of
EP was made.
Discussion
EP is a rare form of chronic pancreatitis
characterized by localized or diffuse eosinophilic infiltration of
the pancreas, accompanied by an increase in IgE levels. Abraham
et al (1) analyzed 3,375
patients with pancreatic disease; among those, 26 exhibited
eosinophilic infiltration of the pancreas, of whom only 3 patients
were diagnosed with EP. This disease has been reported in animals,
including nematode-infected horses, Toxocara canis-infected
dogs, mice injected with purified scorpion venom, horses with
T-cell lymphoma and ferrets with Hodgkins disease (2–7).
A diagnosis of EP is often made following exclusion
of parasitic infection in patients presenting with abdominal pain,
vomiting, diarrhea and other gastrointestinal symptoms, who exhibit
marked eosinophilic infiltration in pathological samples (despite
the lack of a standard for eosinophil counts) and no organ
involvement outside the digestive system (8,9).
The clinical symptoms and characteristics of the
patients during the course of the EP are as follows: A peripheral
eosinophil count of >1.5×109 for >6 months; a
history of rhinitis, bronchial asthma and other allergic diseases;
eosinophilic infiltration of other organs, such as the heart, skin
and gastrointestinal tract; exclusion of other causes of
eosinophilia, such as leukemia and parasitic infections; and a
diagnosis of hypereosinophilic syndrome according to the
international standards (10). An
increase in blood eosinophil count may not be present in patients
with other diseases associated with eosinophilia during the early
stages; therefore, close observation is mandatory.
Pancreatic diseases associated with eosinophilia
include EP, pancreatic cancer, autoimmune pancreatitis and
alcoholic pancreatitis. EP and autoimmune pancreatitis are easily
misdiagnosed as pancreatic cancer and are often treated surgically
due to the similarity in their clinical symptoms and imaging
findings, such as pancreatic enlargement; furthermore, a proportion
of cases of pancreatic cancer are associated with eosinophilia
(11). The differential diagnosis
mainly depends on the histopathological findings and the
measurement of serum tumor marker levels, as well as differences in
the results of ERCP, history of asthma and allergy, increased IgE
and IgG levels, and the effectiveness of glucocorticoid
treatment.
EP is difficult to distinguish from autoimmune
pancreatitis, which exhibits similar clinical manifestations and CT
and ERCP results compared with those of EP. The main
characteristics that may be helpful for the differential diagnosis
of these two conditions are as follows (1,12): i) The
histopathological changes of EP include diffuse eosinophilic
infiltration of the pancreatic ducts, acini and interstitium,
accompanied with eosinophilic phlebitis; the inflammatory
infiltrate of the pancreas is mainly composed by eosinophils, or
may be exclusively eosinophilic in a few cases, with localized
high-density infiltration observed in cases with pancreatic
pseudocysts; ii) the lesions of autoimmune pancreatitis are mainly
infiltrated by lymphocytes rather than eosinophils; iii) EP is
associated with an increase in IgE levels in the peripheral blood,
whereas patients with autoimmune pancreatitis exhibit elevated IgG4
levels; iv) autoimmune pancreatitis patients generally test
positive for autoimmune and antinuclear antibodies; and v)
autoimmune pancreatitis patients exhibit an evenly enlarged
(sausage-like) pancreas, rather than enlargement of the pancreatic
head or tail.
The morphological manifestations in the 3 patients
described in the present study were consistent with those of EP.
Autoimmune pancreatitis and parasitic infections were excluded
based on the postoperative pathological changes and additional
clinical history and laboratory examination, including a negative
history of alcohol and medication use, leading to a diagnosis of
EP. The 3 patients did not meet the diagnostic criteria of
eosinophilic gastroenteritis or eosinophilic syndrome; however, the
increased eosinophil count and IgE levels in the peripheral blood
indicate the need for close observation, considering that a
proportion of cases of eosinophilia combined with other diseases do
not exhibit an elevated eosinophil count in the early stages of the
disease. Although a diagnosis of EP was made in the 3 cases based
on the results of postoperative pathology, EP was not suspected
preoperatively, underscoring the need to improve our knowledge of
EP to prevent misdiagnosis. In our cases, the medical history was
incomplete and eosinophilia in routine blood tests was overlooked,
with no preoperative detection of autoantibodies or increased serum
IgE levels, which led to misdiagnosing EP for cancer. In patients
with chronic inflammation of the pancreas, a frozen section biopsy
of the mass during surgery may prevent misdiagnosis and unnecessary
surgical interventions.
A diagnosis of EP remains difficult for the
following reasons: i) Low incidence and, consequently, limited
information in the available literature; ii) no specific clinical
symptoms; iii) high technical requirements for diagnosis, as
neither IgE measurements nor endoscopic ultrasound-guided
pancreatic biopsy may be performed in a General Hospital; and iv)
the presence of tumor-like changes, which may lead to a
misdiagnosis of pancreatic cancer.
In summary, EP is a rare disease that is easily
misdiagnosed in clinical practice. This is partly due to the
increasing incidence of pancreatic cancer and autoimmune
pancreatitis, combined with a difficulty in differential diagnosis
among these three conditions. Laboratory tests, including
eosinophil counts and IgE levels, combined with CT and ERCP, as
well as pathological examination of the biopsy specimens, are
necessary for the diagnosis of EP. Glucocorticoid diagnostic
treatment may be used when these tests are not possible, with rapid
shrinkage of the pancreatic mass and a decrease of the eosinophil
count suggesting EP. Non-invasive treatments that preserve
pancreatic function are preferred, as they minimize the impact on
the patients' quality of life. An accurate diagnosis of EP is
crucial, as it is considered to be a hypereosinophilic syndrome.
Surgical intervention may be used to alleviate the biliary duct
obstruction and resect the pancreatic head lesion; however, other
pathological changes of the pancreatic body and tail, as well as
the involvement of other organs, such as the skin, liver, spleen,
lymph nodes, cardiovascular system and respiratory system, require
close follow-up.
Acknowledgements
Acknowledgements
The present study was supported by the Natural
Science Foundation of Heilongjiang Province (grant no. H201445 to
Hong Zhu).
References
|
1
|
Abraham SC, Leach S, Yeo CJ, Cameron JL,
Murakata LA, Boitnott JK, Albores-Saavedra J and Hruban RH:
Eosinophilic pancreatitis and increased eosinophils in the
pancreas. Am J Surg Pathol. 27:334–342. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Breider MA, Kiely RG and Edwards JF:
Chronic eosinophilic pancreatitis and ulcerative colitis in a
horse. J Am Vet Assoc. 186:809–811. 1985.
|
|
3
|
Petty DP, Lange AL, Verster A and Hattingh
J: Necropsies of eight horses infected with Strongylus
equinus and Strongylus edentatus. J S AfrVet Assoc.
63:66–69. 1992.
|
|
4
|
Hayden DW and Kruiningen HJ:
Experimentally induced canine toxocariasis: Laboratory examinations
and pathologic changes, with emphasis on the gastrointestinal
tract. Am J Vet Res. 36:1605–11614. 1975.PubMed/NCBI
|
|
5
|
Novaes G, Cde Cardozo C, Costa NM, de
Falco CN, de Carvalho MH and de Queiroz AC: Experimental chronic
interstitial pancreatitis induced by scorpion toxin in rats. Arq
Gastroenterol. 27:187–190. 1990.PubMed/NCBI
|
|
6
|
La Perle KM, Peircy RJ, Long JF and Blomme
EA: Multisystemic, eosinophilic, epitheliotropic disease with
intestinal lymphosarcoma in a horse. Vet Pathol. 35:144–146. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Blomme EA, Foy SH, Chappell KH and La
Perle KM: Hypereosinophilic syndrome with Hodgkin's-like lymphoma
in a ferret. J Comp Pathol. 120:211–217. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Le Connie D and Nguyen H: Eosinophilic
gastroenteritis and pancreatitis: A case report and review of the
literature. South Med J. 97:905–906. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bhat Javid K, Bhat S, Dutt K, Gupta S and
Samoon Jeelani H: Chronic diarrhea, eosinophilic ascites, acute
pancreatitis and deep venous thrombosis: A case report. Caspian J
Intern Med. 5:182–185. 2014.PubMed/NCBI
|
|
10
|
Valent P, Klion AD, Horny HP, Roufosse F,
Gotlib J, Weller PF, Hellmann A, Metzgeroth G, Leiferman KM, Arock
M, et al: Contemporary consensus proposal on criteria and
classification of eosinophilic disorders and related syndromes. J
Allergy Clin Immunol. 130:607–612. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Euscher E, Vaswani K and Frankel W:
Eosinophilic pancreatitis: A rare entity that can mimic a
pancreatic neoplasm. Ann Diagn Pathol. 4:379–385. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shimosegawa T, Chari ST, Frulloni L,
Kamisawa T, Kawa S, Mino-Kenudson M, Kim MH, Klöppel G, Lerch MM,
Löhr M, et al: International consensus diagnostic criteria for
autoimmune pancreatitis: Guidelines of the International
Association of Pancreatology. Pancreas. 40:352–358. 2011.
View Article : Google Scholar : PubMed/NCBI
|