Case report
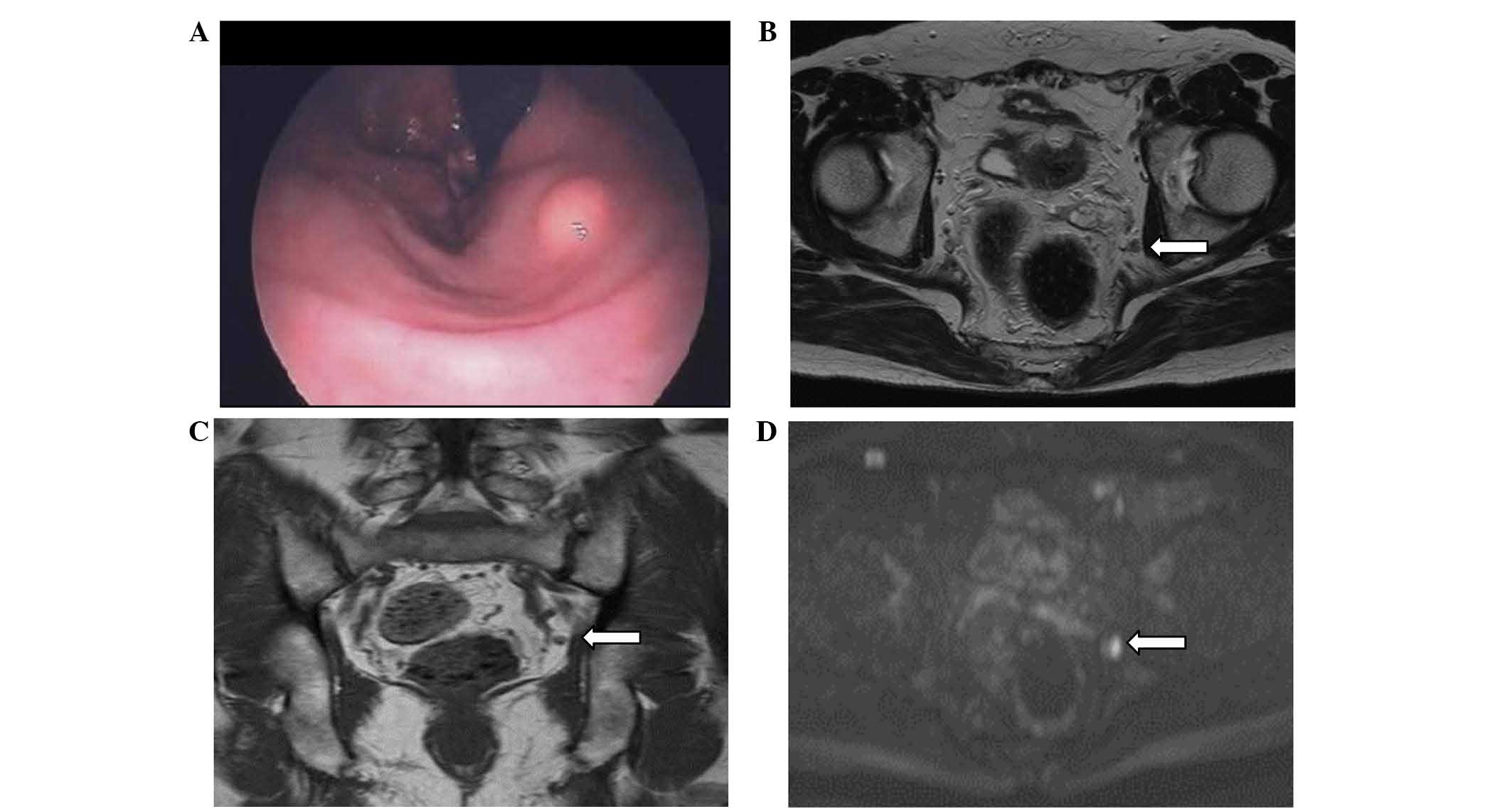
A 59-year-old man was referred to Meiwa Hospital
(Hyogo, Japan) for a routine health examination and underwent a
colonoscopy, which revealed a hemispheric submucosal tumor (7 mm in
diameter) in the lower rectum, which was located 3 cm from the anal
verge at the left side of the rectal wall (Fig. 1A). The lesion revealed no central
depression or ulceration. The pathological diagnosis of the biopsy
specimen was neuroendocrine tumor (NET). Additionally, signs and
symptoms of carcinoid syndrome, including skin flushing, facial
skin lesions and diarrhea were not observed. Abdominal computed
tomography (CT) detected no liver or lung metastasis. The patient
was further assessed by pelvic magnetic resonance imaging, which
revealed swelling in a lateral lymph node located on the left side
obturator lymph node (size, 7 mm) and the shape of the node had a
clear border and uniform detection (Fig.
1B–D). The other lymph nodes, including the mesorectum lymph
node, were not swollen. Laboratory data revealed no abnormal
findings and serum tumor markers, including carbohydrate antigen
19.9, carcinoembryonic antigen, neuron-specific enolase and urine
5-hydroxyindole acetic acid, were all negative. Based on these
findings, the patient was diagnosed with lateral lymph node
metastasis.
A laparoscopic intersphincteric resection (ISR) with
left side lateral lymphadenectomy was performed, followed by
J-pouch reconstruction without diverting stoma. Specifically, the
central lymph node was dissected around the inferior mesenteric
artery (IMA) while preserving the IMA and left colic artery. In the
pelvic space, a total mesorectal excision was performed up to the
anal canal. A left side lateral lymphadenectomy was subsequently
performed as follows: The ureter and hypogastric nerve were picked
up with forceps, and the lymph nodes and fatty tissue were
dissected from the bifurcation of the aorta extending to the common
iliac area. The internal iliac vessels were subsequently cleared
from the lymphatic tissue at a safe distance from the lateral side
of the pelvic plexus. During the dissection, the obturator nerve
and vessels were identified medial to the external iliac vein and
lateral to the superior vesical artery. Following completion of the
pelvic lymph node dissection, only the external vessels, internal
iliac vessels and their branches, the obturator nerve, and the
pelvic plexus remained. At the anal side approach, the distal
resection line was placed on the dentate line and partial-ISR was
performed to divide the intersphincteric space though the
intra-abdominal space. Finally, the surgical specimen was removed
from the anal side and was reconstructed with a colonic J-pouch.
This technique has been described previously (1).
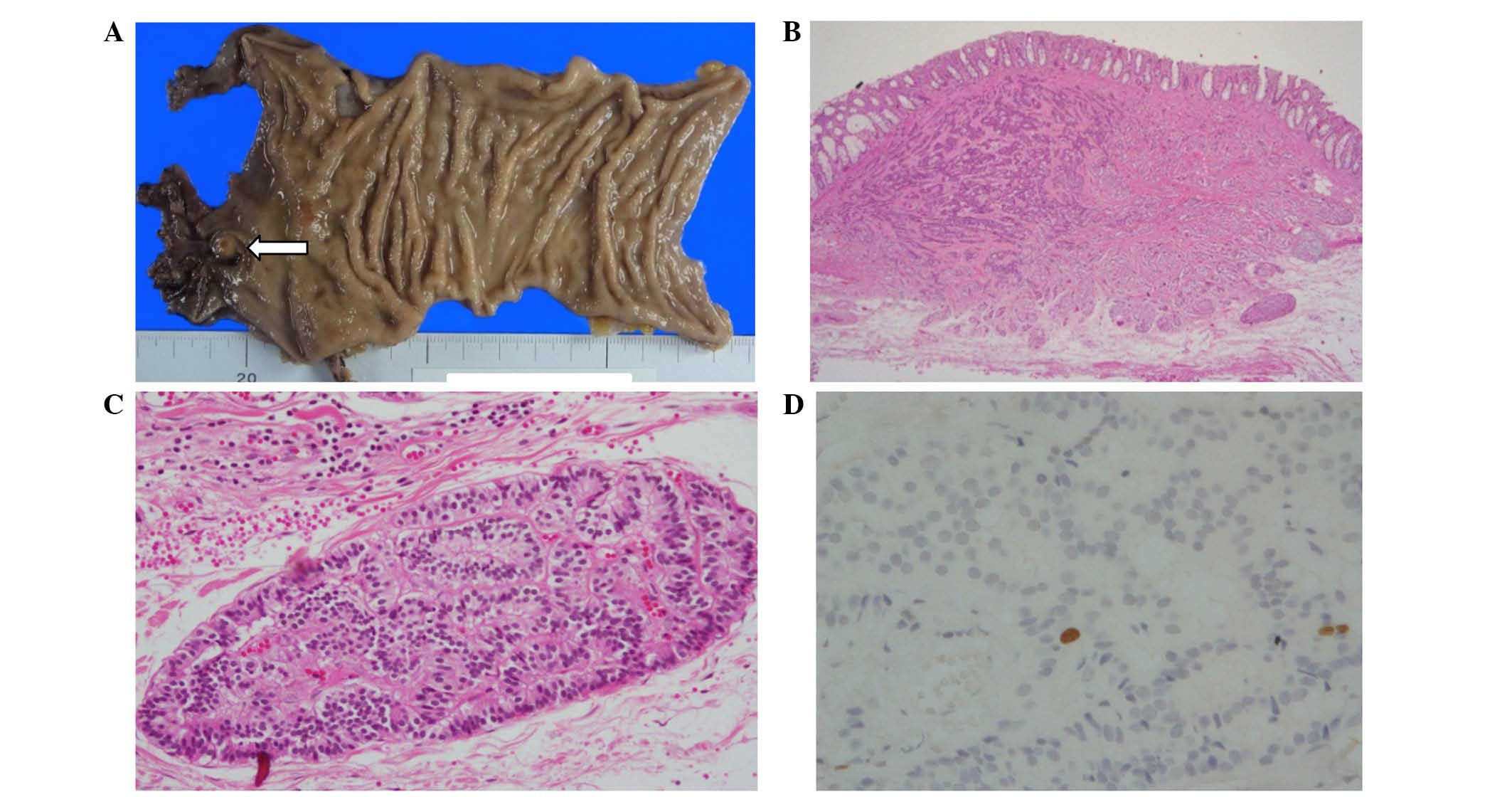
The macroscopic findings of the resected specimen
indicated that the primary tumor was 7 mm in diameter and the
surface was covered with a normal mucous membrane without central
depression or ulceration (Fig. 2A).
On the microscopic findings, a carcinoid pattern tumor was
observed, which had invaded into the perirectal tissues with a
multi-growing pattern, including ribbons, festoons and rosette-like
glands (Fig. 2B). Furthermore,
lymphatic permeation was confirmed (Fig.
2C). The present study diagnosed the tumor as NET with Grade 1
(carcinoid) and from these findings determined that the Ki-67 index
was 1.1% (Fig. 2D) without atypia or
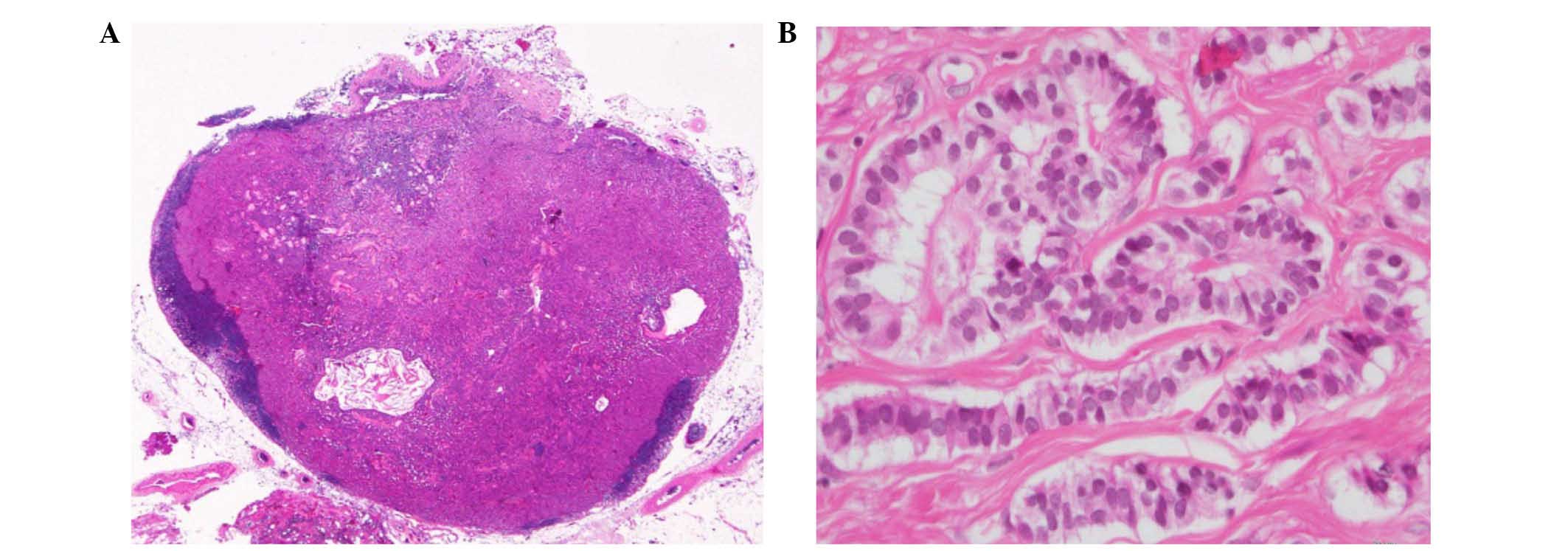
necrosis (0/10 on High Power Field). The lymph nodes at the
mesorectal fascia, including 14 lymph nodes, were all negative;
however, one of seven left side lateral lymph nodes was metastatic
(Fig. 3). Immunohistochemistry
confirmed that both the primary tumor and the metastatic lymph node
were positive for chromogranin and synaptophysin.
The patient was discharged from our hospital 8 days
following surgery, and adjuvant therapy was not performed. The
patient was followed up with chest-abdominal CT every 6 months and
colonoscopy annually. At the 3 year follow-up, recurrence was not
observed and the Wexner Fecal Incontinence Score was 3.
Discussion
Skip metastasis is diagnosed if distant nodes are
positive and regional nodes are negative. The pattern of lymph node
metastasis was decided by the lymphatic tract, which exists along
the artery. Also, the distance from the tumor, which follows
through the epicolic, paracolic, intermediate and principal lymph
nodes, respectively, although different lymphatic pathways may
exist suggesting the presence of important variables, including
tumor invasion of lymphatic channels, changes in the lymphatic
drainage pattern, or direct pressure of tumor bulk leading to
drainage by alternative lymphatic channels effecting the transport
of a single tumor cell via lymphatics (2). Our previous study detected
non-continuous nodal metastasis toward the drainage of the
lymphatic tract, which was hypothesized to be skip metastasis of
colorectal cancer and the frequency of skip metastasis is
~6.5–10.5% (3,4). In the present case study, skip
metastasis was confirmed even with the carcinoid, which is
typically very slow growing and exhibits a low grade malignant
potential.
In colorectal cancer, tumors develop from the
mucosal epithelium and growth expansively. On the other hand, in
rectal carcinoids, tumors develop from the Kultschitzky cells,
which are normally located in the deep mucosa. Therefore, these
tumors invade the submucosa from an early stage. As a result, the
genesis of metastasis is hypothesized to be different between
colorectal cancer and rectal carcinoids. At rectal carcinoid, the
incidence of lymph node metastasis, according to the tumor size,
was 5.5% (1–10 mm), 30% (10–20 mm) and 70% (21–30 mm). Based on the
depth of tumor invasion, the incidence was 12% in the submucosa and
57% in the muscularis propria. Furthermore, the incidence of
central depression and ulceration was revealed to increase in
tumors 10 mm in size (5). A
meta-analysis of factors associated with lymph node metastasis in
rectal carcinoid indicated tumor size >10 mm, an increase in the
depth of invasion, venous invasion and central depression (6). Based on those findings, minimum-invasive
surgeries were decided by the following factors: Tumor size <10
mm and the lack of central depression, ulceration or muscularis
propria invasion. Therefore, a tumor size >10 mm requires
surgical resection with lymphadenectomy (6). In the present case, the tumor size was 7
mm without central depression and ulceration; however, the tumors
had invaded the perirectal tissues. Additionally, the
lymphadenectomy cut-off size for rectal cancer in our institution
was 7 mm. Therefore, following this criteria, the present study
performed lateral lymphadenectomy. Even with the tumor size <10
mm, it was a rare case. However, the lymph node was involved;
therefore, the initial radiological finding of lymph node
metastasis was critical.
Considering previous reports, tumor size >10 mm,
invasion of muscularis propria, venous invasion and central
depression may be risk factors for lymph node invasion, which is an
indication for surgical resection with lymphadenectomy. However,
the recommended procedure for small rectal carcinoids, which are
≤10 mm in size, with lymph node metastasis is not well described.
In general, central depression, ulceration, anisonucleosis,
polymorphism, mitosis, lymph-vascular invasion, or biological
malignancies are signs of malignant potential. However, small
rectal carcinoid with lymph node metastasis are typically low grade
biological malignancies, as assessed by Ki-67 or mitosis;
therefore, previous reports have suggested that biological
malignancies, including carcinoids, are not as easily assessed
(7). The present case was also
difficult to assess since the primary tumor was a rectal
neuroendocrine tumor (Grade 1) and the size was 7 mm; however, the
tumor metastasized to the lateral lymph node and permeated the
lymphatic tract. Pathologically, the present study confirmed
lateral lymph node metastasis; however, carcinoids are typically
slow growing tumors. As a result, it may be unclear if the
pathological confirmation of lymph node metastasis had certain
benefits on the patient outcomes. Long-term outcomes were required
to confirm the usefulness of aggressive lymphadenectomy.
In conclusion, the present case study presented a
case of rectal carcinoid, 7 mm in size, with skip metastasis to the
lateral lymph node. Carcinoids are typically markedly slow growing
and exhibit low grade malignant potential, therefore, minimally
invasive therapy may be selected for non-lymph node metastatic
cases. However, the present case exhibited small carcinoids (<10
mm) with well-defined differentiation and lymph node metastasis,
including the lateral lymph node.
Acknowledgements
The authors would like to thank Dr Ayako Kakuno from
the Department of Pathology at Meiwa Hospital for performing the
pathological assessments.
References
|
1
|
Beppu N, Matsubara N, Noda M, Kimura F,
Yamanaka N, Yanagi H and Tomita N: Laparoscopic intersphincteric
resection and J-pouch reconstruction without laparotomy. Surg
Today. 45:659–662. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yagci G, Unlu A, Kurt B, Can MF,
Kaymakcioglu N, Cetiner S, Tufan T and Sen D: Detection of
micrometastases and skip metastases with ex vivo sentinel node
mapping in carcinoma of the colon and rectum. Int J Colorectal Dis.
22:167–173. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hawes D, Neville AM and Cote RJ: Occult
metastasis. Biomed Pharmacother. 55:229–242. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Merrie AE, Phillips LV, Yun K and McCall
JL: Skip metastases in colon cancer: Assessment by lymph node
mapping using molecular detection. Surgery. 129:684–691. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Soga J: Carcinoids of the rectum: An
evaluation of 1271 reported cases. Surg Today. 27:112–119. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhou X, Xie H, Xie L, Li J and Fu W:
Factors associated with lymph node metastasis in radically resected
rectal carcinoids: A systematic review and meta-analysis. J
Gastrointest Surg. 17:1689–1697. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Takaku H, Suda T, Iiai T, et al: Primary
neuroendocrine cells of the rectum-carcinoid tumor and endocrine
cell carcinoma. Niigata-igaku. 125:611–619. 2011.(In Japanese).
|