Introduction
Patients with prostate cancer have multiple options
for radical treatment modalities for their localized disease,
ranging from radical prostatectomy to radiotherapy, which includes
external beam radiotherapy (EBRT), low-dose-rate
(LDR)-brachytherapy (BT) and high-dose-rate (HDR)-BT. These
treatments offer similar rates of biochemical control.
BT has the ability to deliver an intense radiation
dose to the target, with minimal normal tissue toxicity, and
achieves excellent outcomes for patients with prostate cancer
(1,2).
LDR-BT is most frequently used for the low-risk group and HDR-BT is
predominantly combined with EBRT to treat the intermediate- or
high-risk groups (3–6). Certain disadvantages of HDR-BT are known
when compared with LDR-BT. HDR-BT is more labor intensive and less
convenient for the patients, and medical staff, due to its
multi-fraction schedule. Additionally, it takes a longer period to
complete the treatment, since HDR is usually performed in
combination with EBRT.
In our institute, HDR-BT in combination with EBRT
was initiated in July 1999. Initially, prostate cancer patients
were treated with three fractions of 6 Gy within 2 days and
subsequently EBRT (2 Gy, ×20). To overcome the disadvantages of
HDR-BT described above, reducing the number of fractions was
attempted since November 2004, as the patients had been treated
with two fractions (9 Gy, ×2) within 1 day, combined with EBRT (2
Gy, ×20 or 3 Gy, ×13). Since July 2011, in order to make HDR-BT
more convenient and more efficient, HDR-BT as a monotherapy with
two fractions of 13.5 Gy delivered in 1 day was developed.
An increasing number of articles on HDR monotherapy
have been reported (7). However,
little is reported about high or very high-risk cases treated with
1-day HDR monotherapy. The present study reported valuable data on
the feasibility and the early outcome of two-fraction 1-day HDR
monotherapy for localized prostate cancer, including high-/very
high-risk cases.
Materials and methods
Patient characteristics
Between July 2011 and December 2014, 68 patients
with prostate cancer were treated with HDR Ir-192 BT as a
two-fraction 1-day schedule. Of these patients, 65 had a minimum
follow-up of 12 months without taking adjuvant androgen deprivation
therapy (ADT) and were enrolled in the present study. Patients with
localized prostate cancers (T1c to T4) based on pelvic magnetic
resonance imaging were included. This study was approved by
institutional review board.
HDR Ir-192 BT schedule
The patients were placed in the lithotomy position
under epidural anesthesia. The 7.5-MHz biplanar TRUS transducer was
inserted into the rectum, and the prostate and urethra were
identified. The flexible applicator needles (OncoSmart®
ProGuide SharpNeedle; Elekta AB, Stockholm, Sweden) were implanted
from the anterior to the posterior rows in the periphery of the
prostate to minimize rotation or deformation. The remaining needles
for the internal regions were subsequently implanted. All needles
were inserted, penetrating 4 cm beyond the bladder wall to prevent
needle displacement, and secured to the peritoneal region with
resin and glue. Computed tomography (CT)-based planning was
obtained using Oncentra® Brachy ver. 4.0 (Elekta AB).
The clinical target volume (CTV) was defined by the whole prostate
with a 3 mm margin, with the exception of the posterior region,
where a 2 mm margin was included due to the proximity of the rectal
wall. If seminal vesicle invasion was observed, the applicator
needles were placed, and the seminal vesicle was included in the
CTV. The planning target volume was defined as equal to the CTV.
The dosimetric goals were as follows: Percentage of the prostate
receiving 100 and 150% of the prescribed dose, >90 and <30%,
respectively; minimal dose delivered to 90% of the prostate volume,
>13.5 Gy; volume of the urethra receiving 110% of the prescribed
dose, <1 cc; and volume of the rectum receiving 75% of the
prescribed dose, <1 cc. The patients received the first fraction
of the 13.5 Gy (×2)-schedule using the microSelectron®
Digital HDR-V2 (Elekta AB). The second fraction was delivered on
the same day, with a minimum interval of 6 h. CT was repeated and
CT-based planning was repeatedly obtained for the second fraction
to prevent inaccurate delivery due to needle displacement and/or
deformation. If needle displacement into the prostate occurred,
which affected an area not covered by effective dose, the needles
were reinserted penetrating beyond the bladder wall and CT was
repeated.
Assessment of adverse events (AEs) and
statistical analysis
AEs were scored, according to the Common Terminology
Criteria for Adverse Events (version 4), and the highest score
encountered during each period was reported.
Biochemical failure was assessed using the Radiation
Therapy Oncology Group/American Society for Therapeutic Radiology
and Oncology Phoenix definition of 2 ng/ml or more above nadir
prostate-specific antigen (PSA) (8).
The follow-ups were 4 weeks after the treatment, every 3 months for
the first 2 or 3 years for low-/intermediate- or high-/very
high-risk patients, respectively, the every 6 months until 5 years,
and annually thereafter. Biochemical failure-free survival (bFFS)
was estimated by the Kaplan-Meier method and compared between
groups using the log-rank test. All statistical analyses were
performed using JMP® (SAS Institute Inc., Cary, NC,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
The characteristics of the patients are listed in
Table I. The median follow-up was
30.1 months (12.0–42.7 months) and the median patient age was 72
years (57–81 years). Overall, 42/65 (64.6%) patients exhibited
high-/very high-risk prostate cancers of the National Comprehensive
Cancer Network risk group classification (http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf).
Neoadjuvant ADT was administered to 50 (76.9%) of the patients.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristic | Value |
|---|
| Total patients | 65 |
| Median age, years
(range) | 72 (57–81) |
| Median initial PSA,
ng/ml (range) | 13.1 (4.1–57.8) |
| Initial PSA, n
(%) |
|
| <10
ng/ml | 24 (36.9) |
| 10–20
ng/ml | 23 (35.4) |
| >20
ng/ml | 18 (27.7) |
| Gleason score, n
(%) |
|
| 6 | 7 (10.8) |
| 7 | 29 (44.6) |
| 8–10 | 29 (44.6) |
| Clinical T stage, n
(%) |
|
| T1c | 17 (26.2) |
| T2a | 14 (21.5) |
| T2b | 9 (13.8) |
| T2c | 3 (4.6) |
| T3a | 18 (27.7) |
| T3b | 3 (4.6) |
| T4 | 1 (1.5) |
| Risk
groupa, n (%) |
|
| Low | 2 (3.1) |
|
Intermediate | 21 (32.3) |
| High | 38 (58.5) |
| Very
high | 4 (6.2) |
| Neoadjuvant ADT, n
(%) |
|
| Not
administered | 15 (23.1) |
|
Administered | 50 (76.9) |
| Follow-up, months
(range) | 30.1 (12.0–42.7) |
The majority of patients exhibited mild acute
genitourinary (GU) AEs (Table II),
the most common acute GU AEs being Grade 1 frequency (47.7%),
urgency (41.5%), urethral pain (33.8%) and urinary incontinence
(33.8%). The rate of Grade 2 acute GU AEs was <10%, with the
exception of frequency (12.3%). A total of four patients (6.2%) had
urinary retention, requiring a temporary Foley catheter, and 3
patients developed Grade 3 AEs: Of those, 2 (3.1%) with frequency
and one (1.5%) with hematuria. No other Grade 3 acute GU AEs were
reported. As for acute gastrointestinal (GI) AEs, only 5 patients
experienced mild diarrhea, rectal hemorrhage, proctitis or fecal
incontinence, and no Grade 2 or 3 acute GI AEs occurred.
 | Table II.Acute adverse events occurring within
6 months of treatment. |
Table II.
Acute adverse events occurring within
6 months of treatment.
|
|
| Grade |
|---|
|
|
|
|
|---|
| Adverse event | n | 0 | 1 | 2 | 3 | 4 |
|---|
| Genitourinary, n
(%) |
|
|
|
|
|
|
|
Frequency | 65 | 24 (36.9) | 31 (47.7) | 8 (12.3) | 2 (3.1) | 0 (0) |
|
Urgency | 65 | 35 (53.9) | 27 (41.5) | 3 (4.6) | 0 (0) | 0 (0) |
| Urethral
pain | 65 | 40 (61.6) | 22 (33.8) | 3 (4.6) | 0 (0) | 0 (0) |
|
Retention | 65 | 51 (78.4) | 10 (15.4) | 4 (6.2) | 0 (0) | 0 (0) |
| Urinary
incontinence | 65 | 38 (58.5) | 22 (33.8) | 5 (7.7) | 0 (0) | 0 (0) |
|
Hematuria | 65 | 56 (86.2) | 8 (12.3) | 0 (0) | 1 (1.5) | 0 (0) |
| Urinary
tract obstruction | 65 | 61 (93.9) | 1 (1.5) | 3 (4.6) | 0 (0) | 0 (0) |
| Cystitis
non-infective | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Gastrointestinal, n
(%) |
|
|
|
|
|
|
|
Diarrhea | 65 | 64 (98.5) | 1(1.5) | 0 (0) | 0 (0) | 0 (0) |
| Rectal
hemorrhage | 65 | 63 (96.9) | 2 (3.1) | 0 (0) | 0 (0) | 0 (0) |
|
Proctitis | 65 | 64 (98.5) | 1(1.5) | 0 (0) | 0 (0) | 0 (0) |
| Rectal
pain | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Fecal
incontinence | 65 | 63 (96.9) | 2 (3.1) | 0 (0) | 0 (0) | 0 (0) |
| Rectal
fistula | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
With regards to chronic AEs, 1 patient (1.5%)
exhibited the Grade 3 GU AE of frequency (Table III). This patient developed Grade 3
urinary stricture 9 months after HDR-BT and required endoscopic
treatment. Other than Grade 2 GU urinary incontinence (9.2%) and
urinary tract obstruction (6.2%), the rate of Grade 2 GU AEs was
<5%. No Grade 2 or 3 chronic GI AEs developed, with the
exception of one patient with chronic Grade 2 fecal
incontinence.
 | Table III.Chronic adverse events that developed
after 6 months of treatment. |
Table III.
Chronic adverse events that developed
after 6 months of treatment.
|
|
| Grade |
|---|
|
|
|
|
|---|
| Adverse event | n | 0 | 1 | 2 | 3 | 4 |
|---|
| Genitourinary, n
(%) |
|
|
|
|
| 0 (0) |
|
Frequency | 65 | 37 (57.0) | 26 (40.0) | 1 (1.5) | 1 (1.5) | 0 (0) |
|
Urgency | 65 | 38 (58.5) | 26 (40.0) | 1 (1.5) | 0 (0) | 0 (0) |
|
Urethral pain | 65 | 50 (76.9) | 14 (21.6) | 1 (1.5) | 0 (0) | 0 (0) |
|
Retention | 65 | 57 (87.7) | 6 (9.2) | 2 (3.1) | 0 (0) | 0 (0) |
| Urinary
incontinence | 65 | 45 (69.2) | 14 (21.6) | 6 (9.2) | 0 (0) | 0 (0) |
|
Hematuria | 65 | 62 (95.4) | 2 (3.1) | 1 (1.5) | 0 (0) | 0 (0) |
| Urinary
tract obstruction | 65 | 60 (92.3) | 0 (0) | 4 (6.2) | 1 (1.5) | 0 (0) |
|
Cystitis non-infective | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Gastrointestinal, n
(%) |
|
|
|
|
|
|
|
Diarrhea | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Rectal
hemorrhage | 65 | 63 (96.9) | 2 (3.1) | 0 (0) | 0 (0) | 0 (0) |
|
Proctitis | 65 | 63 (96.9) | 2 (3.1) | 0 (0) | 0 (0) | 0 (0) |
| Rectal
pain | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Fecal
incontinence | 65 | 62 (95.4) | 2 (3.1) | 1 (1.5) | 0 (0) | 0 (0) |
| Rectal
fistula | 65 | 65 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
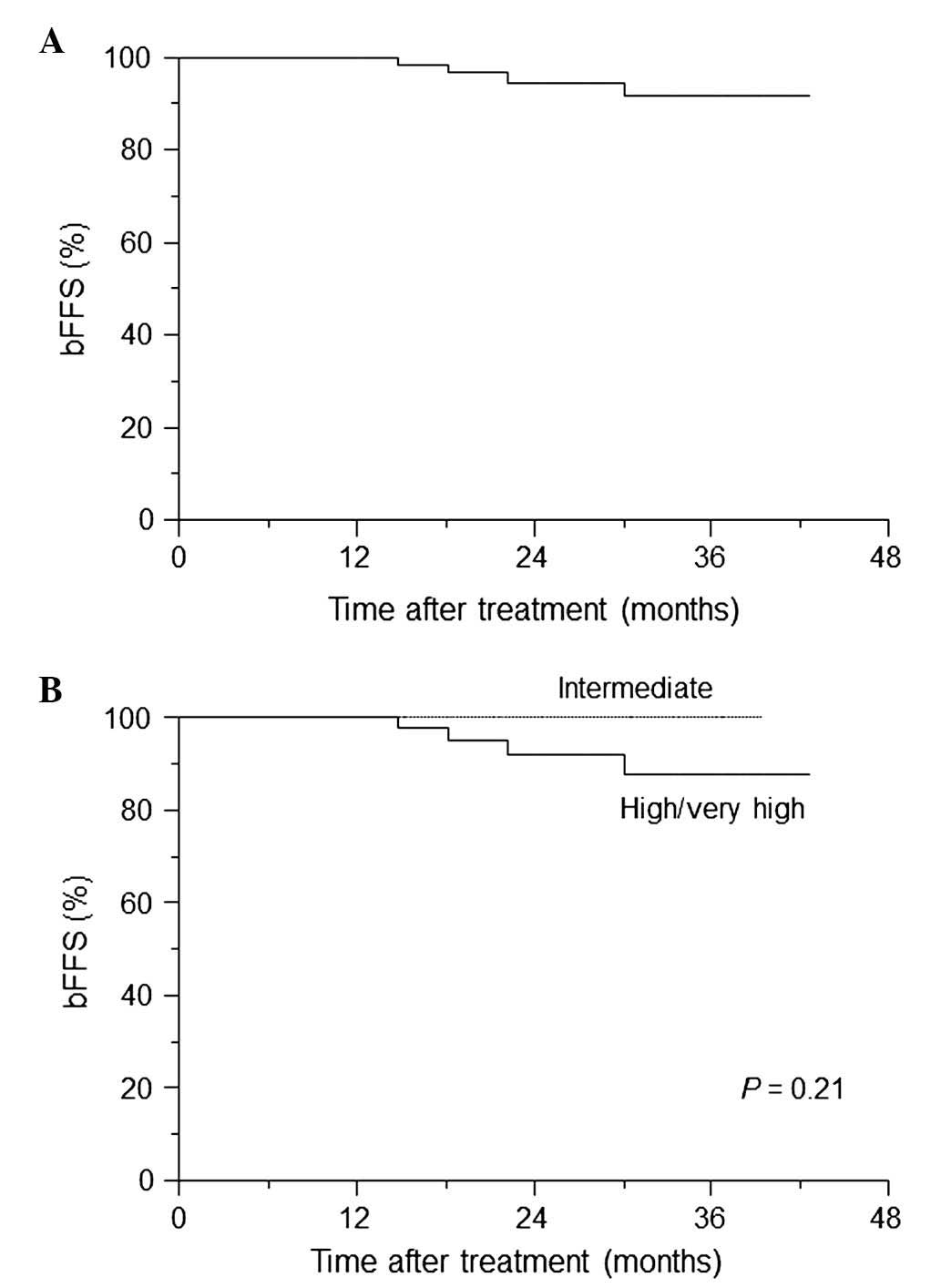
A total of 4 patients (6.2%) had PSA failure, 3 had
high-risk cancers, and 1 patient had very high-risk cancer that
recurred 14.8 months after the treatment (Table IV). Fig.
1 demonstrates the estimates of freedom from biochemical
failure for HDR-BT as monotherapy. The rates of 3-year bFFS were
91.6% overall (Fig. 1A) and 88.0% in
high-/very high-risk patients (Fig.
1B). Excluding the 2 patients with low-risk disease, no
significant difference in bFFS between the intermediate- and
high-/very high-risk groups existed (P=0.21; Fig. 1B).
 | Table IV.Characteristics of four patients with
biochemical failure. |
Table IV.
Characteristics of four patients with
biochemical failure.
| Age (years) | Initial PSA
(ng/ml) | Gleason score | Clinical T
stage | Risk
groupa | Neoadjuvant
ADT | Time to biochemical
failure (months) |
|---|
| 62 | 33.6 | 4+4 | 2b | High | Administered | 30.1 |
| 72 | 12.5 | 4+4 | 2b | High | Administered | 22.2 |
| 67 | 54.9 | 4+3 | 3b | Very high | Administered | 14.8 |
| 75 | 17.2 | 5+4 | 2a | High | Administered | 18.3 |
Discussion
HDR-BT was first introduced at Kiel University,
Germany in 1986 (9). HDR-BT was
initially performed as a boost in combination with EBRT. In 1995,
the first trial of HDR-BT as a monotherapy was introduced at Osaka
University, Japan (10). Since then,
>80 articles and abstracts on HDR monotherapy have been
published, with a variety of doses and fractionations (7).
From the perspective of the radiobiology of HDR-BT
schedules and biologic equivalent dose (BED), the radiation
schedule of 13.5 Gy (×2) was used in the present study. Notably,
when applying the standard linear quadratic model [BED = number of
fractions × dose per fraction (1+d/α/β)], with an α/β ratio of 1.5,
the BED of the 13.5 Gy (×2) schedule was 261 Gy, which is markedly
higher compared with the BED of the EBRT schedule of 1.8 Gy (×45;
BED = 178 Gy) (11).
In the present study, the data indicated the low
toxicity of HDR-BT as monotherapy in two fractions within one day.
The AE data presented are similar to the data from a previously
published HDR monotherapy series (11), which favorably compared with those
from an LDR-BT series (12–15). Zelefsky et al (16) reported that the 5 year likelihood of
urethral stricture development was 10%, and the median duration
until stricture development was 18 months. The median follow-up of
the present series was 30.1 months. Therefore, it is unlikely that
the rate of urethral strictures will significantly change with
longer follow-up (Tables II and
III). Zamboglou et al
(17) recently reported a large
series in which 718 patients were treated with HDR monotherapy.
This previous study showed that late Grade 3 GU toxicity was 3.5%,
which compared favorably with 3.1% in the present series. Yoshioka
et al (18,19) reported that the rate of Grade 2–3
chronic rectal bleeding was ~10% after HDR monotherapy was
delivered with a total dose of 54 Gy in nine fractions within 5
days. The GI toxicity of the present two-fraction schedule was
minimal, and no Grade 2 or greater GI AEs developed, with the
exception of one patient with chronic Grade 2 fecal incontinence.
The present study hypothesized that the reproducibility of
dosimetry is most important to prevent AEs, and repeated CT
planning prior to the second treatment is necessary.
The majority of patients received neoadjuvant ADT
for 3–6 months. Certain patients with a median follow up of 30.1
months may still be under the influence of ADT, as well as HDR-BT.
Therefore, the present biochemical outcome data remains relatively
early. However, the data are important as an early indicator of the
efficacy of this technique. The American Brachytherapy Society
(ABS) guidelines for HDR prostate BT support the use of HDR
monotherapy for localized prostate cancer and quote biochemical
control rates of 85–100, 81–100 and 43–93% for low-, intermediate-
and high-risk prostate cancers, respectively (20). Yoshioka et al (21) recently reported that the three-year
PSA failure-free rates of intermediate- and high-risk patients were
96 and 90%, respectively, for the 45.5 Gy/7 fractions regimen, and
93 and 85%, respectively, for the 54 Gy/9 fractions regimen.
Zamboglou et al (17) showed
that the 3, 5 and 8 year biochemical control rates were 97, 94 and
90%, with no significant differences between the risk groups. In
our cohort, 91.6% of patients overall were free of biochemical
relapse at 3 years. Of those, 100 and 88.0% exhibited intermediate-
and high-/very high-risk diseases. The technique reported in the
present study achieves excellent bFFS rates, similar to the
published data and at the upper end of data quoted by the ABS
guidelines. Finally, HDR monotherapy is not associated with any
significant increase in AEs or reductions in efficacy when compared
with our conventional HDR-BT with EBRT, which achieved bFFSs of
91.7 and 82.5% for 3 and 5 years, respectively, in the high-risk
group (data not shown).
References
|
1
|
Crook J: The role of brachytherapy in the
definitive management of prostate cancer. Cancer Radiother.
15:230–237. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ghilezan M: Role of high dose rate
brachytherapy in the treatment of prostate cancer. Cancer
Radiother. 16:418–422. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hoskin PJ, Colombo A, Henry A, Niehoff P,
Hellebust Paulsen T, Siebert FA and Kovacs G: GEC/ESTRO
recommendations on high dose rate afterloading brachytherapy for
localised prostate cancer: An update. Radiother Oncol. 107:325–332.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hoskin PJ, Rojas AM, Bownes PJ, Lowe GJ,
Ostler PJ and Bryant L: Randomised trial of external beam
radiotherapy alone or combined with high-dose-rate brachytherapy
boost for localised prostate cancer. Radiother Oncol. 103:217–222.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Langley S, Laing R, Henderson A, Aaltomaa
S, Kataja V, Palmgren JE, Bladou F, Salem N, Serment G, Nava L, et
al: European collaborative group on prostate brachytherapy:
Preliminary report in 1175 patients. Eur Urol. 46:565–570;
discussion 570. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zwahlen DR, Andrianopoulos N, Matheson B,
Duchesne GM and Millar JL: High-dose-rate brachytherapy in
combination with conformal external beam radiotherapy in the
treatment of prostate cancer. Brachytherapy. 9:27–35. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Demanes DJ and Ghilezan MI: High-dose-rate
brachytherapy as monotherapy for prostate cancer. Brachytherapy.
13:529–541. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Roach M III, Hanks G, Thames H Jr,
Schellhammer P, Shipley WU, Sokol GH and Sandler H: Defining
biochemical failure following radiotherapy with or without hormonal
therapy in men with clinically localized prostate cancer:
Recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int
J Radiat Oncol Biol Phys. 65:965–974. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kovács G, Galalae R, Loch T, Bertermann H,
Kohr P, Schneider R and Kimming B: Prostate preservation by
combined external beam and HDR brachytherapy in nodal negative
prostate cancer. Strahlenther Onkol. 175(Suppl 2): S87–S88. 1999.
View Article : Google Scholar
|
|
10
|
Yoshioka Y, Nose T, Yoshida K and Inoue T,
Yamazaki H, Tanaka E, Shiomi H, Imai A, Nakamura S, Shimamoto S and
Inoue T: High-dose-rate interstitial brachytherapy as a monotherapy
for localized prostate cancer: Treatment description and
preliminary results of a phase I/II clinical trial. Int J Radiat
Oncol Biol Phys. 48:675–681. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ghilezan M, Martinez A, Gustason G, Krauss
D, Antonucci JV, Chen P, Fontanesi J, Wallace M, Ye H, Casey A, et
al: High-dose-rate brachytherapy as monotherapy delivered in two
fractions within one day for favorable/intermediate-risk prostate
cancer: Preliminary toxicity data. Int J Radiat Oncol Biol Phys.
83:927–932. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Anderson JF, Swanson DA, Levy LB, Kuban
DA, Lee AK, Kudchadker R, Phan J, Bruno T and Frank SJ: Urinary
side effects and complications after permanent prostate
brachytherapy: The MD Anderson cancer center experience. Urology.
74:601–605. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Crook J, Fleshner N, Roberts C and Pond G:
Long-term urinary sequelae following 125 iodine prostate
brachytherapy. J Urol. 179:141–145; discussion 146. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Keyes M, Miller S, Moravan V, Pickles T,
McKenzie M, Pai H, Liu M, Kwan W, Agranovich A, Spadinger I, et al:
Predictive factors for acute and late urinary toxicity after
permanent prostate brachytherapy: Long-term outcome in 712
consecutive patients. Int J Radiat Oncol Biol Phys. 73:1023–1032.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Merrick GS, Butler WM, Wallner KE,
Galbreath RW, Allen ZA, Gutman S and Lief J: Long-term rectal
function after permanent prostate brachytherapy. Cancer J.
13:95–104. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zelefsky MJ, Hollister T, Raben A,
Matthews S and Wallner KE: Five-year biochemical outcome and
toxicity with transperineal CT-planned permanent I-125 prostate
implantation for patients with localized prostate cancer. Int J
Radiat Oncol Biol Phys. 47:1261–1266. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zamboglou N, Tselis N, Baltas D, Buhleier
T, Martin T, Milickovic N, Papaioannou S, Ackermann H and Tunn UW:
High-dose-rate interstitial brachytherapy as monotherapy for
clinically localized prostate cancer: Treatment evolution and
mature results. Int J Radiat Oncol Biol Phys. 85:672–678. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yoshioka Y, Konishi K, Sumida I, Takahashi
Y, Isohashi F, Ogata T, Koizumi M, Yamazaki H, Nonomura N, Okuyama
A and Inoue T: Monotherapeutic high-dose-rate brachytherapy for
prostate cancer: Five-year results of an extreme hypofractionation
regimen with 54 Gy in nine fractions. Int J Radiat Oncol Biol Phys.
80:469–475. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yoshioka Y, Nose T, Yoshida K, Oh RJ,
Yamada Y, Tanaka E, Yamazaki H and Inoue T and Inoue T:
High-dose-rate brachytherapy as monotherapy for localized prostate
cancer: A retrospective analysis with special focus on tolerance
and chronic toxicity. Int J Radiat Oncol Biol Phys. 56:213–220.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yamada Y, Rogers L, Demanes DJ, Morton G,
Prestidge BR, Pouliot J, Cohen GN, Zaider M, Ghilezan M and Hsu IC:
American Brachytherapy Society: American brachytherapy society
consensus guidelines for high-dose-rate prostate brachytherapy.
Brachytherapy. 11:20–32. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yoshioka Y, Konishi K, Suzuki O, Nakai Y,
Isohashi F, Seo Y, Otani Y, Koizumi M, Yoshida K, Yamazaki H, et
al: Monotherapeutic high-dose-rate brachytherapy for prostate
cancer: A dose reduction trial. Radiother Oncol. 110:114–119. 2014.
View Article : Google Scholar : PubMed/NCBI
|