Introduction
Lung cancer is the leading cause of cancer-related
mortality worldwide, with an incidence of 1.4 million per year and
a mortality rate of 1.2 million per year (1,2).
Non-small-cell lung cancer (NSCLC) accounts for ~80% of all lung
cancer cases, and understanding the underlying mechanisms is
crucial for identifying effective means of prevention and treatment
(3).
Overexpression of epidermal growth factor receptor
(EGFR) is observed in various malignancies, including lung cancer
(4). EGFR activation is related to
cell proliferation and survival via complex intracellular
signalling pathways. The EGFR tyrosine kinase pathway, in
particular, has become an optimal therapeutic target. EGFR-tyrosine
kinase inhibitors (EGFR-TKIs), such as gefitinib and erlotinib,
have exhibited encouraging results in terms of clinical activity
against NSCLCs harboring activating EGFR mutations (5,6).
Xuanwei county has the highest lung cancer incidence
and mortality rates in China, in men as well as in women.
Environmental factors are known to play a role in cancer incidence,
and indoor air pollution from the use of smoky coal for household
purposes has been suggested to be the cause of the high rates of
lung cancer in Xuanwei, particularly in non-smoking female
patients. A previous study including a limited patient number
demonstrated that non-smoking female lung cancer patients in
Xuanwei exhibit different EGFR mutation patterns compared with the
patterns seen elsewhere in Asia (7).
The echinoderm microtubule-associated protein-like
4-anaplastic lymphoma kinase (EML4-ALK) oncogene, which was first
identified by researchers from Japan, was found to be active in
2.9–11.4% of NSCLC patients in China (8–11) and is
often present in adenocarcinomas in non-smokers. To the best of our
knowledge, no study has yet been conducted to determine the
incidence of EML4-ALK fusion protein in Xuanwei patients.
In this retrospective study, we screened 258
resection samples from lung cancer patients (90 from Xuanwei and
168 from other regions in the same province) to characterize the
EGFR expression and mutation profiles and their association with
EML4-ALK. A better understanding of the specific mutations present
in the patients from this region may lead to more effective
targeted therapeutic interventions at earlier stages of the
disease.
Materials and methods
Clinical data
This retrospective study was conducted on specimens
stored in the tissue registry of the Yunnan Provincial Tumor
Hospital, with the approval of the Institutional Review Board.
Cancer tissues were obtained from consecutive NSCLC patients who
underwent pulmonary resection at the Department of Thoracic Surgery
of our hospital between February, 2011 and February, 2014.
Amplification refractory mutation
system polymerase chain reaction (ARMS-PCR)
Genomic DNA from 3×5-mm formalin-fixed,
paraffin-embedded (FFPE) sections was isolated manually using a
QIAamp DNA FFPE Tissue kit (Qiagen, Hilden, Germany) in accordance
with the manufacturer's instructions. Polymorphisms in exons 18
(G719X), 19 (S768I), 20 (G779C, S768I, L858R, V774M) and 21 (L861Q
and L858R) were detected with the ARMS-PCR technique. DNA
amplification was performed using specific nested primer sets for
each polymorphism. PCR amplifications were performed in a total
volume of 25 µl containing 100 ng genomic DNA, 1X PCR buffer, 10
pmol of each primer, 10 nmol of each deoxyribonucleotide
triphosphate, 1.5 mM Mg2+, and 1 U TaqDNA polymerase.
The PCR conditions were as follows: Initial denaturation step (94°C
for 2 min); 10 cycles of denaturation (94°C for 15 sec) and
annealing/extension (65°C for 60 sec), followed by 20 cycles of
denaturation (94°C for 10 sec), annealing (62°C for 50 sec) and
extension (72°C for 30 sec). The PCR products were separated in a
2% agarose gel and visualized with ethidium bromide staining and
ultraviolet illumination with a gel documentation system (Gel Doc
2000; Bio-Rad, Hercules, CA, USA).
Direct DNA sequencing
To verify the ARMS-PCR results, DNA samples obtained
from 67 Xuanwei specimens were amplified, purified and sequenced
using BigDye Terminator v3.1 on an ABI 3100 Genetic Analyzer (both
from Applied Biosystems, Foster City, CA, USA).
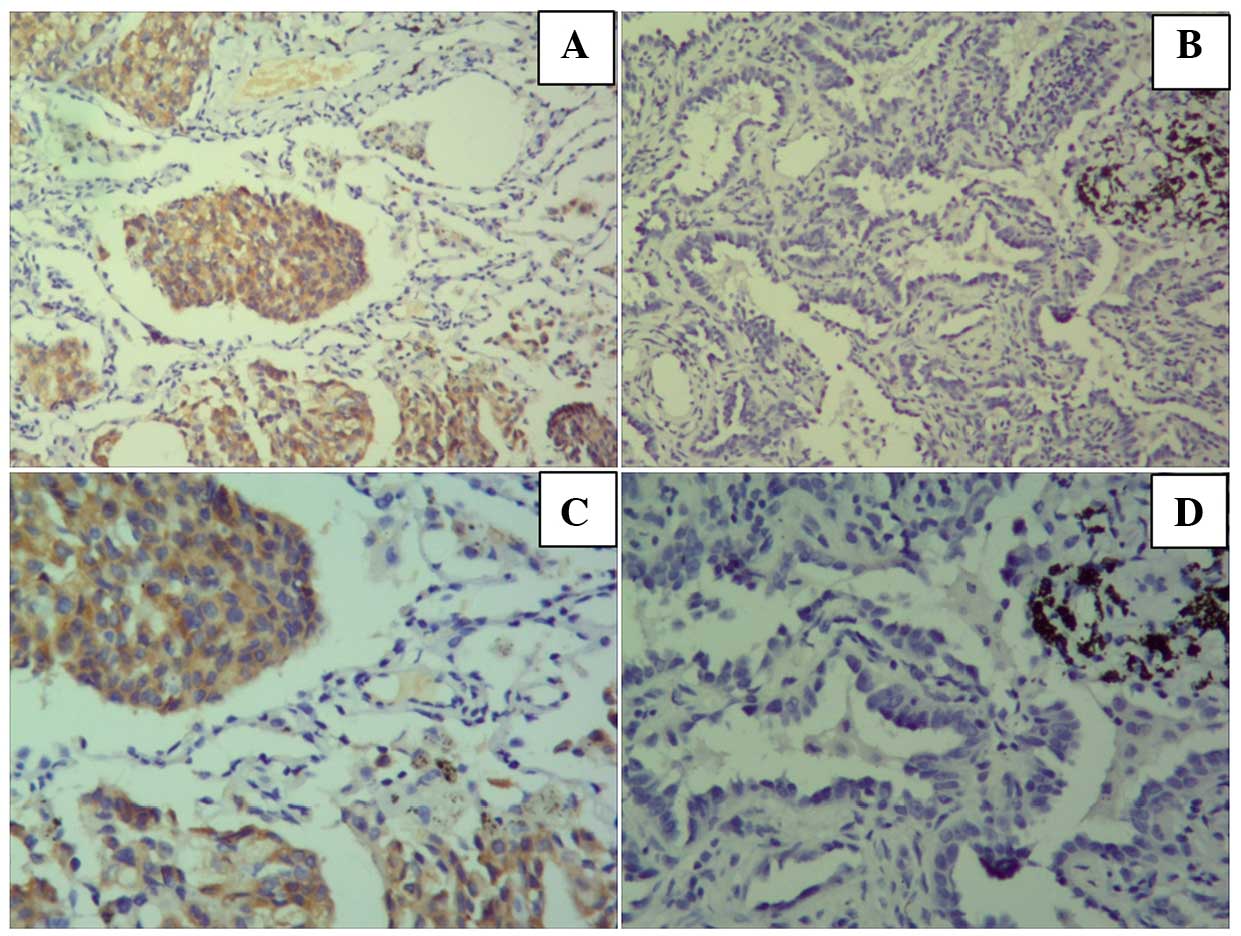
Immunohistochemistry (IHC)
All Xuanwei samples were subjected to IHC to detect
the EML4-ALK fusion protein. IHC was performed on 4-µm FFPE tissue
sections placed on silane-coated slides using the 5A4 anti-ALK
primary antibody in the ALK Detection kit (Nichirei Bioscience,
Tokyo, Japan) (12). Tumor cells that
stained more strongly in the cytoplasm compared with negative
control cells, were defined as IHC-positive. Semi-quantitative
assessment was performed by estimating the percentage of
IHC-positive tumor cells. ALK IHC scores were assigned using the
iAEP method (iScore) as follows: 0, no stained cells; 1, 0–50%
stained tumor cells; 2, 50–80% stained tumor cells or >80%
stained tumor cells with marked variability of staining intensity
(‘checkerboard pattern’); and 3, >80% stained tumor cells
without marked variability of staining intensity.
Fluorescent in situ hybridization
(FISH)
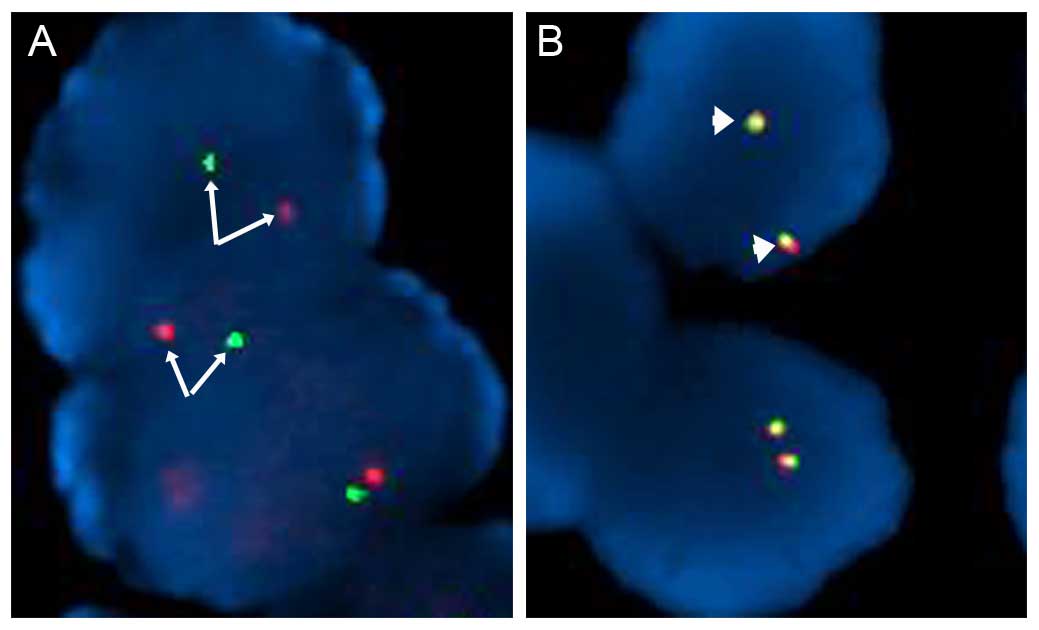
Specimens positive for the EML4-ALK fusion protein
by IHC were confirmed by FISH performed on the 4-µm FFPE tissue
sections using the Vysis ALK Break Apart FISH Probe kit (Vysis LSI
ALK Dual Color Break Apart rearrangement probe; Abbott Molecular,
Abbott Park, IL, USA) in accordance with the manufacturer's
instructions. At least 50 representative tumor cells were counted.
When ≥15% of the tumor cells exhibited separate green and red
signals or an isolated (single) red signal, the sample was
considered to contain an ALK gene rearrangement. All other samples
were classified as ALK FISH-negative.
Statistical analysis
Statistical analyses were performed using SPSS
software, version 16.0 (SPSS Inc., Chicago, IL, USA). Data were
subjected to the Pearson's Chi-square and Fisher's exact tests.
P<0.05 was considered to indicate statistically significant
differences.
Results
Patient characteristics
Cancer tissues from 258 consecutive NSCLC patients
(123 men and 135 women) who had undergone pulmonary resection at
the Department of Thoracic Surgery of our hospital between
February, 2011 and February, 2014, were obtained from the tissue
registry of our institution. Of the 258 patients, 90 were from
Xuanwei (32 men and 58 women) and 158 were from non-Xuanwei areas
in the same province (91 men and 77 women). Patient demographic and
pathological characteristics are summarized in Table I. There were significantly more women
(P<0.0059, Fisher's exact test) and younger patients
(P<0.0488, Fisher's exact test) in the Xuanwei group compared
with the non-Xuanwei control group. Lymph node metastasis was
significantly more common in the Xuanwei cohort (P<0.0001).
Furthermore, more Xuanwei patients had tumors characterized as
adenocarcinomas (P<0.0031, Chi-square test) and at lower stages
(P<0.0001, Chi-square test). However, the distribution of
patients for smoking status was similar between the two groups.
 | Table I.Patient demographic and
characteristics tumor clinicopathology. |
Table I.
Patient demographic and
characteristics tumor clinicopathology.
|
| Xuanwei (n=90) | Non-Xuanwei
(n=158) |
|
|---|
|
|
|
|
|
|---|
| Characteristics | n | % | n | % | P-value |
|---|
| Gender |
|
|
|
|
|
| Male | 32 | 35.6 | 91 | 54.38 | 0.0059 |
|
Female | 58 | 64.4 | 77 | 45.8 |
|
| Age (years) |
|
|
|
|
|
| ≤60 | 69 | 76.7 | 108 | 64.3 | 0.0488 |
|
>60 | 21 | 23.3 | 60 | 35.7 |
|
| Smoking status |
|
|
|
|
|
| Yes | 21 | 23.3 | 49 | 29.2 | 0.3785 |
| No | 69 | 76.7 | 119 | 70.8 |
|
| Lymph node
metastasis |
|
|
|
|
|
| Yes | 52 | 57.8 | 23 | 13.7 |
<0.0001 |
| No | 38 | 42.2 | 145 | 86.3 |
|
| Histology |
|
|
|
|
|
| Ad | 86 | 95.6 | 140 | 83.3 | 0.0031 |
| SCC | 3 | 3.3 | 28 | 16.7 |
|
| Sa | 1 | 1.1 | 0 |
|
|
| Stage |
|
|
|
|
|
| I | 38 | 42.2 | 23 | 13.7 |
<0.0001 |
| II | 18 | 20.0 | 15 | 8.9 |
|
| III | 11 | 12.2 | 20 | 11.9 |
|
| IV | 23 | 25.6 | 110 | 65.5 |
|
EGFR mutations in Xuanwei and
non-Xuanwei NSCLC patients
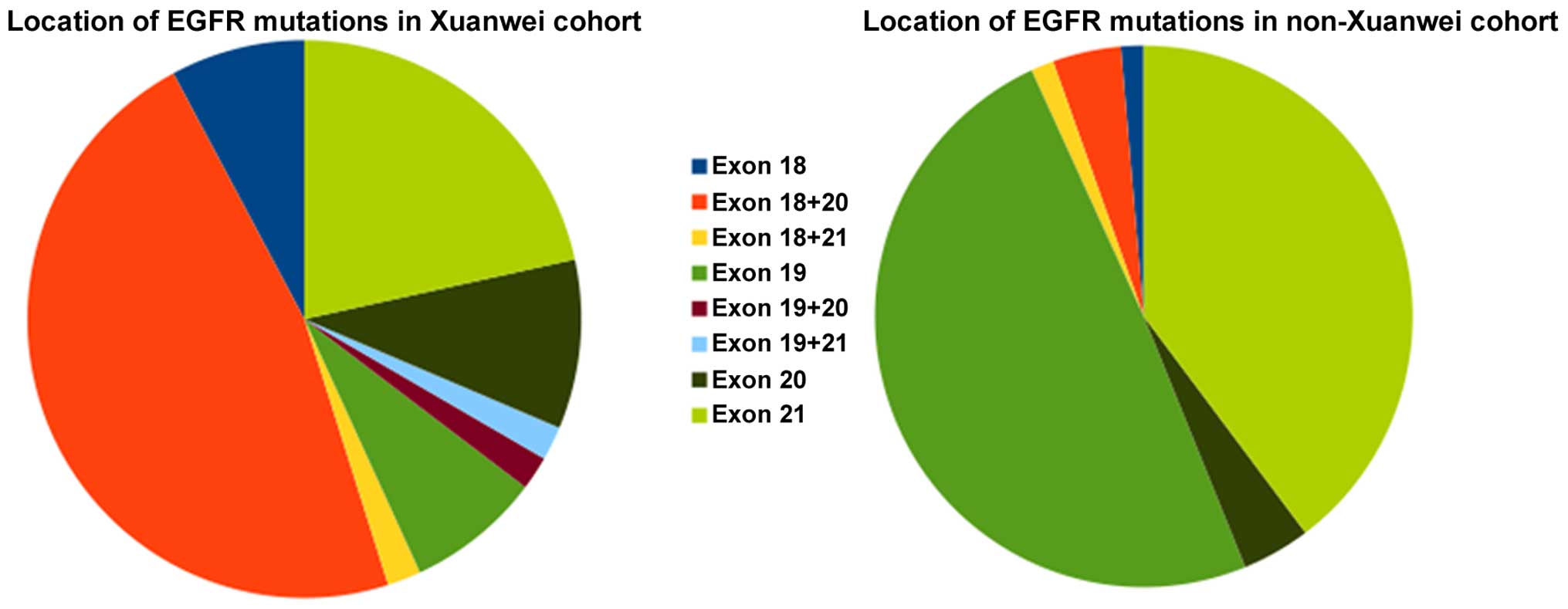
Among Xuanwei and non-Xuanwei lung cancer patients,
51 (57%) and 73 (43%) harbored EGFR mutations, respectively
(Table II). The non-Xuanwei cohort
exhibited a high frequency of deletion mutations in exon 19 (n=36,
49.3% of total mutations) and point mutations in exon 21 (n=29,
39.7% of total mutations). These mutations were identified in a
significantly smaller percentage of Xuanwei patients (exon 19: n=4,
7.8% of total mutations; and exon 21: n=11, 21.6% of total
mutations) (Fig. 1). However, the
Xuanwei cohort had more mutations in the combination of exons 18
G719X and 20 S768I (n=23, or 45.1% of total mutations), whereas
mutations in this combination were rare in the non-Xuanwei cohort
(n=3/73, 4.1%). Using the Fisher's exact test, the distribution of
patients with and without specified mutations between the Xuanwei
and non-Xuanwei regions was found to be significantly different for
deletion mutations in exon 19 and double mutations in exons 18 and
20 (Table II).
 | Table II.Characterisation and comparison of
EGFR mutations in Xuanwei and non-Xuanwei NSCLC patients. |
Table II.
Characterisation and comparison of
EGFR mutations in Xuanwei and non-Xuanwei NSCLC patients.
|
|
| Xuanwei | Non-Xuanwei |
|
|---|
|
|
|
|
|
|
|---|
| Exon | Mutation | Cases | % | Cases | % | P-value |
|---|
| 18 | G719X | 4 | 7.8 | 1 | 1.4 | NA |
| 18+20 | G719X+G779C | 1 |
2.0 | – |
| NA |
|
| G719X+S768I | 23 |
45.1 | 3 |
4.1 | <0.0001 |
| 18+21 | G719X+L861Q | 1 |
2.0 | 1 |
1.4 | NA |
| 19 | Deletion | 4 |
7.8 | 36 |
49.3 | <0.0001 |
| 19+21 | Deletion+L858R | 1 |
2.0 | – |
| NA |
| 20 | P772_H773
insertion | 1 |
2.0 | – |
| NA |
|
| S768I | 2 |
3.9 | 2 |
2.7 | NA |
|
| S768I+V774M
insertion | 2 |
3.9 | 1 |
1.4 | NA |
| 20+21 | S768I+L858R | 1 |
2.0 | – |
| NA |
| 21 | L858R | 10 |
19.6 | 27 |
37.0 |
0.1496 |
|
| L861Q | 1 |
2.0 | 2 |
2.7 |
|
| Total |
| 51 |
100.0 | 73 |
100.0 |
|
Differences in exonal localization of
EGFR mutations between Xuanwei and non-Xuanwei patients
We further compared the exonal localization of EGFR
mutations (Table III), and found
significant differences for exons 18/20, as well as for the
combination of exons 19 and 21 or the combination of exons 18 and
20, the latter mutations being less frequently detected in general
lung cancer patients (13).
 | Table III.Differences in exonal localization of
EGFR mutations between Xuanwei and non-Xuanwei patients. |
Table III.
Differences in exonal localization of
EGFR mutations between Xuanwei and non-Xuanwei patients.
| Exon | Mutation | Xuanwei | Non-Xuanwei |
P-valuea |
|---|
| 19 | Yes | 5 | 36 | 0.0003 | 0.0005 |
|
| No | 85 | 122 |
|
|
| 21 | Yes | 14 | 30 | 0.6046 |
|
|
| No | 76 | 128 |
|
|
| 18 | Yes | 35 | 5 | 0.0001 | 0.0001 |
|
| No | 55 | 153 |
|
|
| 20 | Yes | 30 | 6 | 0.0001 |
|
|
| No | 60 | 152 |
|
|
Association between
clinicopathological characteristics and EGFR events in Xuanwei and
non-Xuanwei patients
The distributions of EFGR mutations were similar by
age, histology, and lymph node involvement (Table IV). However, Xuanwei patients were
significantly more likely to be non-smokers rather than smokers
(P<0.05), which was not the case for non-Xuanwei patients
(Table IV). In the Xuanwei as well
as the non-Xuanwei cohort, the distribution of patients was
significantly different between the two genders (P<0.05), in
accordance with a previous study (8).
 | Table IV.Association between
clinicopathological characteristics and EGFR events in Xuanwei and
non-Xuanwei lung cancer patients. |
Table IV.
Association between
clinicopathological characteristics and EGFR events in Xuanwei and
non-Xuanwei lung cancer patients.
|
| Xuanwei
patients | Non-Xuanwei
patients |
|---|
|
|
|
|
|---|
|
| Wild-type | EGFR mutation |
| Wild-type | EGFR mutation |
|
|---|
|
|
|
|
|
|
|
|
|---|
|
Characteristics | n | % | n | % | P-value | n | % | n | % | P-value |
|---|
| Age (years) |
|
|
|
| 0.80 |
|
|
|
| 0.07 |
|
≤60 | 29 | 74.4 | 40 | 78.4 |
| 67 | 70.5 | 41 | 56.2 |
|
|
>60 | 10 | 25.6 | 11 | 21.6 |
| 28 | 29.5 | 32 | 43.8 |
|
| Gender |
|
|
|
| <0.01 |
|
|
|
| <0.02 |
|
Male | 20 | 51.3 | 12 | 23.5 |
| 59 | 62.1 | 32 | 43.8 |
|
|
Female | 19 | 48.7 | 39 | 76.5 |
| 36 | 37.9 | 41 | 56.2 |
|
| Smoking
history |
|
|
|
| <0.02 |
|
|
|
| 0.17 |
|
Yes | 14 | 35.9 | 7 | 13.7 |
| 32 | 33.7 | 17 | 23.3 |
|
| No | 25 | 64.1 | 44 | 86.3 |
| 63 | 66.3 | 56 | 76.7 |
|
| Histology |
|
|
|
| <0.03 |
|
|
|
| <0.001 |
|
Adenocarcinoma | 35 | 89.7 | 51 | 100.0 |
| 71 | 74.7 | 69 | 94.5 |
|
|
Others | 4 | 10.3 | 0 |
|
| 24 | 25.3 | 4 | 5.5 |
|
| Stage |
|
|
|
| 1.00 |
|
|
|
| 1.00 |
|
I–II | 24 | 61.5 | 32 | 62.7 |
| 22 | 23.2 | 16 | 21.9 |
|
|
III–IV | 15 | 39.5 | 19 | 37.3 |
| 73 | 76.8 | 57 | 78.1 |
|
| Lymph nodes |
|
|
|
| 1.00 |
|
|
|
| 0.38 |
|
Yes | 23 | 59.0 | 29 | 56.9 |
| 11 | 11.6 | 12 | 16.4 |
|
| No | 16 | 41.0 | 22 | 43.1 |
| 84 | 88.4 | 61 | 83.6 |
|
Detection of EGFR mutations with the
ARMS and direct sequencing methods
Direct DNA sequencing of a subset of samples from
the Xuanwei cohort (n=67) confirmed almost all the ARMS results,
with the exception of one deletion mutation in exon 19. The
sequencing also identified 4 point mutations in exon 20 [P772-H773
(insGNP), S768I, V774M and G779C] (Table
V), which had not been previously reported in the
literature.
 | Table V.Number of EGFR mutations found with
the ARMS and direct sequencing methods. |
Table V.
Number of EGFR mutations found with
the ARMS and direct sequencing methods.
| Method | Exon 18 | Exon 19 | Exon 20 | Exon 21 |
|---|
| ARMS | 24 | 4 | 20 | 10 |
| Direct
sequencing | 24 | 3 | 24 | 10 |
EML4-ALK detection by IHC and
FISH
Two specimens from Xuanwei patients were found to be
positive for EML4-ALK by IHC (Fig.
2), and this result was confirmed by FISH (Fig. 3). The patients who were positive for
EML4-ALK did not harbor EGFR mutations (data not shown).
Discussion
Xuanwei county in the province of Yunnan, located in
Southwest China, is known to have very high rates of lung cancer
compared with the general population of China (7). In order to gain a better understanding
of the potential drug sensitivities within this population, we
screened samples from our tissue registry for EGFR mutations, a
known cause of NSCLC. Our large sample consisted of tissue from 258
consecutive lung cancer patients, 90 from Xuanwei and 168 from
other areas of Yunnan. To the best of our knowledge, this study is
the first comprehensive profile of EGFR mutations in the Xuanwei
area using patients from the same province as controls.
EGFR mutation rates were found to be higher in
specimens from Xuanwei compared with other areas. These numbers are
marginally higher compared with those for the general Asian
population (8). In addition to the
high frequency of occurrence, Xuanwei patients carrying EGFR
mutations also exhibit distinct demographic and pathological
characteristics. EGFR mutations are more likely detected in women
and younger patients in the Xuanwei area compared with non-Xuanwei
areas. Clinicopathologically, Xuanwei patients carrying EGFR
mutations are more likely to be classified as adenocarcinomas or
have lymph node metastasis, but less likely to be diagnosed at more
advanced stages. These results suggest that the factors causing
EGFR mutations and subsequent pathogenesis are likely different
between the two patient groups.
Consistent with previous studies (7,8), we found
reciprocal patterns of mutations in patients from different
regions: Non-Xuanwei patients most frequently exhibited deletion
mutations in exon 19 and L858R point mutations in exon 21 (the
‘classical’ mutations), whereas the majority of mutations in
Xuanwei patients were in exon 18. However, we also found a
strikingly higher number of co-mutations in exon 18 (mainly G719X)
and exon 20 (S768I) in Xuanwei patients when compared with
non-Xuanwei patients, a result that has not been previously
reported. Intriguingly, 18 of the 23 patients with G719X and S768I
double mutations were women (data not shown). This is likely due to
the exposure of women to increased household coal burning, since
the women in the Xuanwei area are more likely to stay at home doing
household work (7). These distinctive
molecular characteristics in EGFR mutations observed in Xuanwei
patients may have contributed to the abovementioned
clinicopathological characteristics that are specific to this group
of patients.
Direct DNA sequencing confirmed almost all EGFR
mutations identified by ARMS. The only exception was a deletion
mutation in exon 19, which may have been the result of loading an
insufficient amount of sample. Direct DNA sequencing also
identified 4 additional point mutations (Table V). Thus, direct DNA sequencing
described a more detailed mutation profile compared with ARMS in
our study.
The EML4-ALK fusion protein was positive in 2.2% of
Xuanwei patients (2 of 90). This is lower compared with the
percentage reported for other Asian regions (10). It is possible that the increased lung
cancer incidence in the Xuanwei area is exclusively associated with
EGFR mutations, thus resulting in the lower prevalence of EML4-ALK
fusions. None of the specimens that were positive for the EML4-ALK
fusion protein harboured any EGFR mutations. This is consistent
with a previous study suggesting that EML4-ALK and EGFR mutations
are independent events and are mutually exclusive (14). Due to the small number of
EML4-ALK-positive specimens in this study (2 samples out of 90),
further investigation is required to draw any conclusions regarding
this finding in the Xuanwei population, but would suggest that
treatment of this group with crizotinib is contraindicated.
In conclusion, this study provides a comprehensive
profile of EGFR gene mutations in Xuanwei patients and patients
from other areas in Yunnan province. Particularly since a high
percentage of the Xuanwei patients were never smokers, a status
associated with EGFR mutations (15),
it offers an excellent model to study environmental or genetic
factors, or interactions between them, in lung cancer biology.
Mutations in the EGFR are known to either sensitize tumors to TKIs,
or to make them refractory to such treatments (16). Furthermore, the efficacy of EGFR-TKI
and ALK inhibitors is known to decrease in some initially
responsive patients. The detailed evaluation of mutations found in
the Xuanwei subpopulation of NSCLC patients presented in this study
holds the potential for improvements in targeted therapies. Further
studies in this group, regarding responsiveness to TKIs and other
targeted therapies, are required.
Glossary
Abbreviations
Abbreviations:
|
EGFR
|
epidermal growth factor receptor
|
|
ALK
|
anaplastic lymphoma kinase
|
|
EML4
|
echinoderm microtubule-associated
protein-like 4
|
|
NSCLC
|
non-small-cell lung cancer
|
|
ARMS-PCR
|
amplification refractory mutation
system polymerase chain reaction
|
|
IHC
|
immunohistochemistry
|
|
TKI
|
tyrosine kinase inhibitor
|
|
RT-PCR
|
reverse transcription polymerase chain
reaction
|
|
FISH
|
fluorescence in situ
hybridization
|
|
FFPE
|
formalin-fixed paraffin-embedded
|
References
|
1
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jemal A, Siegel R, Ward E, Murray T, Xu J
and Thun MJ: Cancer statistics, 2007. CA Cancer J Clin. 57:43–66.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Buettner R, Wolf J and Thomas RK: Lessons
learned from lung cancer genomics: The emerging concept of
individualized diagnostics and treatment. J Clin Oncol.
31:1858–1865. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Normanno N, Maiello MR and De Luca A:
Epidermal growth factor receptor tyrosine kinase inhibitors
(EGFR-TKIs): Simple drugs with a complex mechanism of action? J
Cell Physiol. 194:13–19. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Maemondo M, Inoue A, Kobayashi K, Sugawara
S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I,
et al: North-East Japan Study Group: Gefitinib or chemotherapy for
non-small-cell lung cancer with mutated EGFR. N Engl J Med.
362:2380–2388. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rosell R, Carcereny E, Gervais R,
Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R,
Pallares C, Sanchez JM, et al: Spanish Lung Cancer Group in
collaboration with Groupe Français de Pneumo-Cancérologie and
Associazione Italiana Oncologia Toracica: Erlotinib versus standard
chemotherapy as first-line treatment for European patients with
advanced EGFR mutation-positive non-small-cell lung cancer
(EURTAC): A multicentre, open-label, randomised phase 3 trial.
Lancet Oncol. 13:239–246. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hosgood HD III, Pao W, Rothman N, Hu W,
Pan YH, Kuchinsky K, Jones KD, Xu J, Vermeulen R, Simko J, et al:
Driver mutations among never smoking female lung cancer tissues in
China identify unique EGFR and KRAS mutation pattern associated
with household coal burning. Respir Med. 107:1755–1762. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shigematsu H and Gazdar AF: Somatic
mutations of epidermal growth factor receptor signaling pathway in
lung cancers. Int J Cancer. 118:257–262. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sun Y, Ren Y, Fang Z, Li C, Fang R, Gao B,
Han X, Tian W, Pao W, Chen H, et al: Lung adenocarcinoma from East
Asian never-smokers is a disease largely defined by targetable
oncogenic mutant kinases. J Clin Oncol. 28:4616–4620. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wong DW, Leung EL, So KK, Tam IY, Sihoe
AD, Cheng LC, Ho KK, Au JS, Chung LP and Wong Pik M: University of
Hong Kong Lung Cancer Study Group: The EML4-ALK fusion gene is
involved in various histologic types of lung cancers from
nonsmokers with wild-type EGFR and KRAS. Cancer. 115:1723–1733.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rikova K, Guo A, Zeng Q, Possemato A, Yu
J, Haack H, Nardone J, Lee K, Reeves C, Li Y, et al: Global survey
of phosphotyrosine signaling identifies oncogenic kinases in lung
cancer. Cell. 131:1190–1203. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Takeuchi K, Choi YL, Togashi Y, Soda M,
Hatano S, Inamura K, Takada S, Ueno T, Yamashita Y, Satoh Y, et al:
KIF5B-ALK, a novel fusion oncokinase identified by an
immunohistochemistry-based diagnostic system for ALK-positive lung
cancer. Clin Cancer Res. 15:3143–3149. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Siegelin MD and Borczuk AC: Epidermal
growth factor receptor mutations in lung adenocarcinoma. Lab
Invest. 94:129–137. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang Y, Wang S, Xu S, Qu J and Liu B:
Clinicopathologic features of patients with non-small cell lung
cancer harboring the EML4-ALK fusion gene: A meta-analysis. PLoS
One. 9:e1106172014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pao W, Miller V, Zakowski M, Doherty J,
Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, et al:
EGF receptor gene mutations are common in lung cancers from ‘never
smokers’ and are associated with sensitivity of tumors to gefitinib
and erlotinib. Proc Natl Acad Sci USA. 101:13306–13311. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sharma SV, Bell DW, Settleman J and Haber
DA: Epidermal growth factor receptor mutations in lung cancer. Nat
Rev Cancer. 7:169–181. 2007. View
Article : Google Scholar : PubMed/NCBI
|