Introduction
Gastrointestinal stromal tumors (GISTs) are the most
common mesenchymal neoplasms of the gastrointestinal tract, and
mesenchymal tumors are thought to constitute ~1% of primary
gastrointestinal cancers (1,2). Between 50–70% of GISTs arise from the
stomach, which is the most common site of origin (1,3). The
National Institutes of Health (NIH) 2002 consensus stratified GIST
risk according to tumor size and mitotic rate (3). It has been proposed that these
stratification guidelines should be widely used to predict
recurrent risk factors, and modifications have also been proposed
(4); however, certain factors
regarding the criteria remain to be elucidated, such as the impact
of tumor location, which may lead to an overestimation of the risk
of large gastric GISTs (5,6). Another risk stratification schema that
incorporates the impact of tumor location has been supported by
three large retrospective studies conducted by the Armed Forced
Institute of Pathology (7–9). However, some questions remain regarding
the rare clinical settings that lack proposed parameters of risk
assessment, as the data was too insufficient to lead to a
convincing definition (5,6). Therefore, finding a reliable
immunohistochemical predictor would be helpful for clinical
practice.
Positive transcriptional elongation factor b
(P-TEFb) contains the catalytic subunit cyclin-dependent kinase 9
(Cdk9) and the regulatory subunit cyclin T. Cyclin T contains
subunits T1, T2a and T2b. Cdk9 is complexed with T1, T2a and T2b in
~80, 10 and 10% of cases, respectively (10–12). The
expression pattern of cyclin T2a almost completely overlapped the
pattern described for cyclin T1 (12). The expression of cyclin T1 increased
the Cdk9 kinase activity and the phosphorylation of RNA polymerase
II (RNAPII). The hypophosphorylation of the carboxyl-terminal
repeat domain of RNAPII promotes and starts the elongation phase of
transcription (13). This enables
RNAPII to escape promoter-proximal pausing in order to engage the
factors for pre-mRNA processing (14).
P-TEFb has been proficiently investigated in cardiac
hypertrophy and human immunodeficiency virus (HIV) infection. The
transcriptional activation for HIV-1 requires Tat interaction with
human cyclin T1 and involves the formation of a complex with P-TEFb
to increase the amount of RNAPII (15). In addition, the Cdk inhibitor,
flavopiridol, has been reported to have a mitigating effect on
RNAPII levels (16). By contrast,
hypertrophic signals may activate Cdk9 and consequently cause
phosphorylation of RNAPII. This effect not only increases RNA
synthesis but also enlarges myocyte size and may result in cardiac
hypertrophy (13,14). In previous years, certain studies have
reported that P-TEFb and transcriptional elongation exhibited key
roles in protecting normal and cancerous cells from apoptosis
(17). Cdk9 inhibitors have been
thought to be potential therapeutic agents for chronic lymphocytic
leukemia (18) and lung
adenocarcinoma (19). Cyclin T1 and
Cdk9 are also overexpressed in the human head and neck carcinoma
cell lines (10).
The expression of cyclins A, B, D and E appear to be
associated with high-grade disease but not with the clinical
outcome (20–22). In addition, cyclin H-positive patients
have a poor prognosis when they have high-risk GIST and when they
exhibit metastasis or recurrent disease (23). However, there are few effective
clinical predictors for gastric GIST. The aim of the present study
was to assess the association of cyclin T1 and Cdk9, and the
clinical parameters of gastric GISTs.
Materials and methods
Tissues and patients
The study included 30 gastric GIST patients who
underwent either laparoscopic or laparotomic partial gastrectomy
between 2008 and 2011 by the same surgical team at Tungs' Taichung
MetroHarbor Hospital (Taiwan, China). Fifteen of the patients who
were at a high risk of recurrence according to the NIH consensus
received postoperative adjuvant chemotherapy with imatinib, and 1
patient received sunitinib. The medical charts, pathological
reports, and surgical notes of all the study participants were
retrospectively reviewed. The pathological diagnoses were reviewed
by at least two experienced pathologists.
Ethics statement
The study was granted approval from the
Institutional Review Board of the Tungs' Taichung MetroHarbor
Hospital. All the patients included in the study received a full
explanation of the procedures involved and provided written
informed consent prior to collection of the specimens and clinical
information.
Immunohistochemical staining
Using the Bond-Max autostainer (Leica Microsystems,
Buffalo Grove, IL, USA), the slides were stained with Cdk9
monoclonal antibody and cyclin T1 polyclonal antibody. The details
of these immunomarkers, including methods of pretreatment for
antigen retrieval, are provided in Table
I. Briefly, formalin-fixed and paraffin-embedded tissue
specimens were placed in Tris-buffered saline and Tween 20,
rehydrated through serial dilutions of alcohol, and washed in
phosphate-buffered saline (pH 7.2), which was the buffer that was
used for all subsequent washes, according to the manufacturer's
recommended protocol. The coated slides were stained with the
previously mentioned antibodies, and the immunostaining procedure
was performed on the fully-automated Bond-Max system using the
onboard heat-induced antigen retrieval and a Leica Refine Polymer
Detection System (Leica Microsystems). Diaminobenzidine was used as
the chromogen (Leica Microsystems) in all these immunostainings.
Negative controls were obtained by excluding the primary antibody.
Appropriate positive controls were used throughout the study. These
slides were mounted with gum for microscopic examination, and the
images were captured by the Olympus BX51 microscopic/DP71 Digital
Camera System (Olympus, Ina, Japan) for study comparisons.
 | Table I.Antibodies used in the present
study. |
Table I.
Antibodies used in the present
study.
| Antigen | Clone | Product code | Antibody class | Supplier | Dilution | Antigen | Retrieval, min |
|---|
| CyclinT1 | Rabbit
polyclonal | ab2098 | IgG | Abcam | 1:500 | ER1 | 20 |
| Cdk9 | Rabbit
monoclonal | 2454–1 | IgG | Epitomics | 1:500 | ER2 | 20 |
For the assessment of Cdk9 and cyclin T1 expression,
the intensity of immunostaining was scored on a scale of 0 (no
staining) to 4 (strongest intensity), and the percentage of cell
staining at each intensity was estimated from 0 to 100. The
percentage of cells at each intensity level was multiplied by the
corresponding intensity value, and these products were combined to
obtain an immunostaining score ranging from 0 to 400.
Statistical analysis
The disease-free survival (DFS) rates of patients
were analyzed by Kaplan-Meier estimates and compared using the
log-rank test. The DFS was defined as the interval between the date
of surgery and the date of tumor recurrence or distant metastasis.
Cox regression methods were used to investigate the association
between survival, clinical parameters and immunohistochemical
variables in multivariate models. Differences between positive and
negative cyclin T1 staining were analyzed using the Mann-Whitney
U-test. All the statistical tests were two-sided. The difference
between the groups was considered statistically significant when
P<0.05. All the analyses were performed using the SPSS 16.0
(SPSS, Inc., Chicago, IL, USA) software package.
Results
Patient variables
A total of 30 patients were examined in the study
(15 male and 15 female). The mean age was 60.3 years; 14 patients
were <60 years old and 16 were >60. Eleven patients developed
tumor recurrence or distant metastases during the study. Fifteen of
the patients who were at high risk of recurrence according to the
NIH consensus received postoperative adjuvant chemotherapy with
imatinib, and 1 patient received sunitinib. The other 14 patients
did not receive postoperative adjuvant chemotherapy. The scores of
Ki67 staining for 6 and 8 patients were > and <5%,
respectively. The results of the other 16 patients were not
recorded.
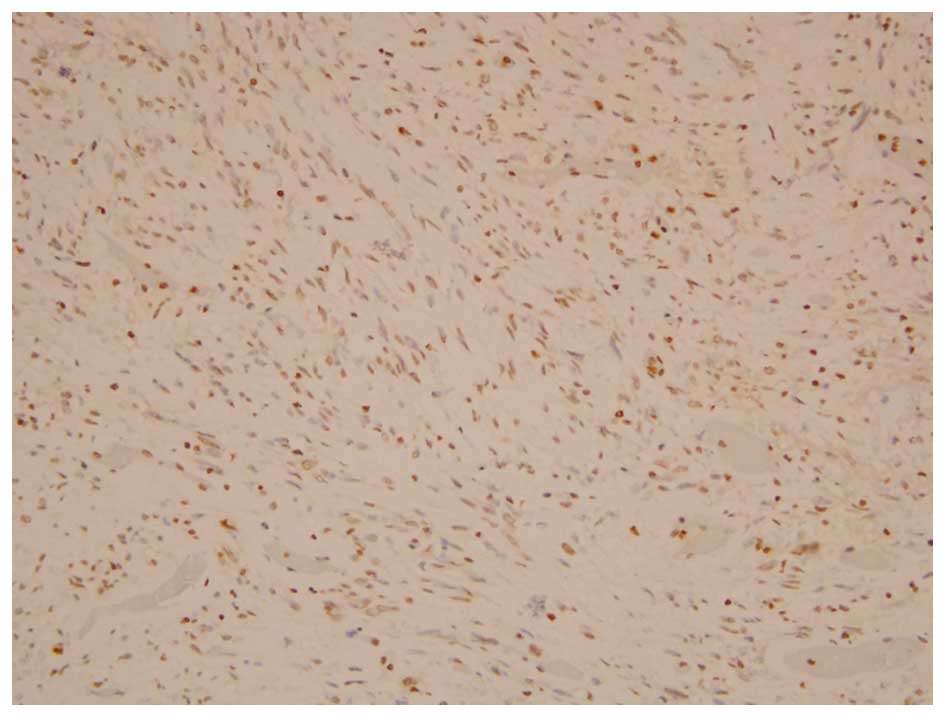
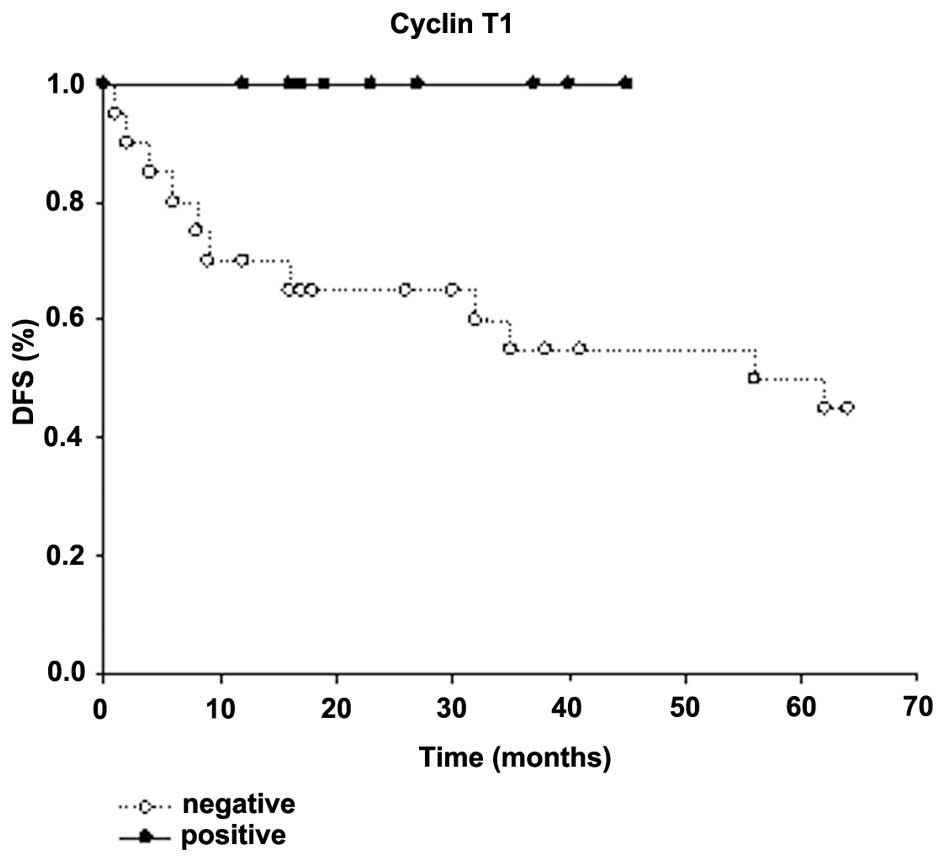
Ten patients were cyclin T1-positive (Fig. 1), and 20 were negative. All 11
patients with recurrent tumors or distant metastases were cyclin
T1-negative patients. The DFS was analyzed using univariate
log-rank test and multivariate stepwise Cox-regression test. Old
age, large tumor size, higher Ki67 staining, high mitotic count and
negative cyclin T1 staining were associated with clinical outcomes
in univariate analysis. The Kaplan-Meier survival curve illustrated
the DFS of the patients with negative cyclin T1 staining was
significantly lower than that of the patients with positive cyclin
T1 staining (P=0.031, Fig. 2).
However, no significant difference was observed in the DFS between
different ages, genders, tumor size, pathological type, Ki67
staining and cyclin T1 staining using the multivariate analysis.
The clinicopathological features and univariate and multivariate
analyses are summarized in Table
II.
 | Table II.Univariate log-rank and multivariate
Cox analyses for prognostic factors with respect to disease-free
survival. |
Table II.
Univariate log-rank and multivariate
Cox analyses for prognostic factors with respect to disease-free
survival.
|
|
|
| P-value |
|---|
|
|
|
|
|
|---|
| Parameters | Cases, n | Events, n | Univariate | Multivariate |
|---|
| Gender |
|
|
|
|
|
Male | 15 | 5 | 0.404 |
|
|
Female | 15 | 6 |
|
|
| Age, years |
|
|
|
|
|
≤60 | 14 | 2 | 0.026a | 0.765 |
|
>60 | 16 | 9 |
|
|
| Type |
|
|
|
|
|
Spindle | 26 | 9 | 0.088 | 0.834 |
|
Epitheloid/mixed | 4 | 2 |
|
|
| Tumor size, cm |
|
|
|
|
| ≤5 | 11 | 2 | 0.023a | 0.959 |
|
>5 | 19 | 9 |
|
|
| Ki67 |
|
|
|
|
|
≤5b | 8 | 0 | 0.018a | 0.675 |
|
>5b | 6 | 3 |
|
|
| Mitosis, HPF |
|
|
|
|
|
≤5/50 | 23 | 6 | 0.021a | 0.894 |
|
>5/50 | 7 | 5 |
|
|
| Cdk9 |
|
|
|
|
|
≤270b | 14 | 5 | 0.928 |
|
|
>270b | 16 | 6 |
|
|
| Cyclin T1 |
|
|
|
|
| − | 20 | 11 | 0.031a | 0.874 |
| + | 10 | 0 |
|
|
Subgroup analysis for cyclin T1
The patients were also divided into two subgroups on
the basis of positive and negative staining for cyclin T1. Cyclin
T1 staining was analyzed with the other clinicopathological
factors. No significant differences were observed between the two
subgroups. However, patients with negative cyclin T1 staining
appeared to have poorer results than those with positive cyclin T1
staining. Among the 30 patients, 23 patients had low mitotic rates,
and 7 had high rates. All 7 patients with high mitotic rates were
cyclin T1-negative. A summary of the association between cyclin T1
staining and other clinicopathological factors are shown in
Table III.
 | Table III.Association of cyclin T1 with various
clinicopathological parameters. |
Table III.
Association of cyclin T1 with various
clinicopathological parameters.
|
|
| Cyclin T1 |
|
|---|
|
|
|
|
|
|---|
| Parameters | Cases, n | − | + | P-value |
|---|
| Age, years |
|
|
|
|
|
≤60 | 14 | 8 | 6 | 0.442 |
|
>60 | 16 | 12 | 4 |
|
| Gender |
|
|
|
|
|
Male | 15 | 9 | 6 | 0.699 |
|
Female | 15 | 11 | 4 |
|
| Tumor size, cm |
|
|
|
|
| ≤5 | 11 | 7 | 4 | >0.9999 |
|
>5 | 19 | 13 | 6 |
|
| Type |
|
|
|
|
|
Spindle | 26 | 17 | 9 | >0.9999 |
|
Epitheloid/mixed | 4 | 3 | 1 |
|
| Ki67 |
|
|
|
|
|
≤5% | 8 | 5 | 3 | >0.9999 |
|
>5% | 6 | 4 | 2 |
|
| Mitosis, HPF |
|
|
|
|
|
≤5/50 | 23 | 13 | 10 | 0.064 |
|
>5/50 | 7 | 7 | 0 |
|
| Cdk9 |
|
|
|
|
|
≤270 | 14 | 10 | 4 | 0.709 |
|
>270 | 16 | 10 | 6 |
|
Discussion
In the present study, age, tumor size, percentage of
Ki-67 staining, mitotic rate and cyclin T1 staining were the
prognostic factors associated with recurrence in patients with
gastric GIST following surgical resection. The results showed a
significant difference in the univariate analysis but not in the
multivariate analysis. Along with the factors of large tumor size
and high mitotic rate presented in the NIH consensus, several
studies have defined other poor prognostic factors, such as
epithelioid type, increased expression of cytoplasmic HuR and
cyclin A, and a high Ki67 ratio (24–27).
Increased expression of cyclin H was also a poor prognostic factor
in high-risk GIST patients (23). The
present results showed that cyclin T1 may be another potential
prognostic predictor for gastric GIST patients.
The association between cyclin T1 staining and other
factors was also analyzed. Although no statistical significance was
observed in the difference in mitotic rates between the cyclin
T1-positive and -negative patients, all 10 patients with positive
cyclin T1 staining had low mitotic rates, and all 7 patients with
high mitotic rates were negative for cyclin T1. Cyclin T1 may be a
potential regulator of mitosis and may contribute to tumor
recurrence.
In a previous study, Cdk9/cyclin T1 complex
upregulation contributed to T lymphocyte differentiation and
malignant transformation (28).
Regulation of the Cdk9/cyclin T1 complex is dependent on a
tissue-specific signaling pathway (29), and the complex response to certain
cytokines such as tumor necrosis factor and interleukin-6 (30,31).
Cyclin T1 and Cdk9 may promote the expression of anti-apoptotic
factors and cause proliferation (32–34). A
deregulated Cdk9-related pathway has been observed in several human
tumors, including lymphoma (29,35,36),
neuroblastoma (37), prostate cancer
(38) and several hematopoietic
malignancies (29). By contrast,
certain studies have demonstrated that cyclin T1, but not Cdk9,
induced transformation in vitro in head and neck tumors
(10). Upregulation of cyclin T1 is
the main mechanism for activation of the complex during T-cell
activation, and cyclin T1 acts as a rate-limiting regulatory
subunit (39). A previous study also
suggested that the cyclin-dependent kinase inhibitor had no
correlation with the malignant potential of GIST and did not serve
as a predictor of DFS (40). The
present results demonstrated that cyclin T1, but not Cdk9, was a
prognostic factor for DFS, and that cyclin T1 was associated with
the mitotic rate. The study confirmed that cyclin T1 has a
regulatory role in the Cdk9/cyclin T complex, and that upregulation
of cyclin T1 was the main mechanism for the activation of this
complex. These results also supported that cyclin T1 acted as a
rate-limited regulatory subunit (39).
Certain previous studies have shown that cyclin T1
overexpression was a poor prognostic factor (10,28,29,39).
However, the present results demonstrated that negative staining
for cyclin T1 was a poor prognostic factor. Cdk9 and cyclin T1 were
expressed in a similar pattern in certain normal tissues, but
varied in other tissues (12). The
tissues of mesenchymal organs, such as connective tissue, skeletal
muscle, blood and lymphoid tissue, exhibited high cyclin T1
expression levels (11,12). It is also believed that cyclin T1 is
not a typical cell cycle regulator, as its levels do not oscillate
at any phase during the cell cycle (11). Additionally, the upregulation of
cyclin T1 is not linked directly to cell cycle entry and
progression (11). In different
tissues, the expression of cyclin T1 has different roles in tumor
behavior. Deregulation of cyclin T1 contributes to poor outcomes,
and negative cyclin T1 expression is potentially associated with a
worse prognosis.
The present study had several limitations. The
subgroups of patients were too small for individual analysis. A
study with a larger sample size will be necessary for further
investigation of the predictors of gastric GISTs. In addition,
in vitro cell molecular studies would help to identify the
pathway of cyclin T1. This was a pilot study to determine whether
cyclin T1 could be considered for further studies including more
patients and cell lines to confirm the role of the Cdk9/cyclin T1
complex in GIST.
In conclusion, it is reasonable to consider cyclin
T1 immunohistochemical staining as a predictor of the prognosis of
gastric GIST following surgical resection. The pathway of cyclin T1
was also demonstrated to potentially be associated with the mitotic
rate.
Acknowledgements
The present study was supported by a grant from
Tungs' Taichung MetroHarbor Hospital (no. TTMHH-100R0004).
References
|
1
|
Scarpa M, Bertin M, Ruffolo C, Polese L,
D'Amico DF and Angriman I: A systemic review on the clinical
diagnosis of gastrointestinal stromal tumors. J Surg Oncol.
98:384–392. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Miettinen M, Sarlomo-Rikala M and Lasota
J: Gastrointestinal stromal tumors: Recent advances in
understanding of their biology. Hum Pathol. 30:1213–1220. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fletcher CD, Berman JJ, Corless C,
Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti
H, Rubin BP, et al: Diagnosis of gastrointestinal stromal tumors: A
consensus approach. Int J Surg pathol. 10:81–99. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang HY, Li CF, Huang WW, Hu TH, Lin CN,
Uen YH, Hsiung CY and Lu D: A modification of NIH consensus
criteria to better distinguish the highly lethal subset of primary
localized gastrointestinal stromal tumors: A subdivision of the
original high-risk group on the basis of outcome. Surgery.
141:748–756. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Demetri GD, von Mehren M, Antonescu CR,
DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF,
Schuetze S, et al: NCCN task force report: Update on the management
of patients with gastrointestinal stromal tumors. J Natl Compr Canc
Netw. 8(Suppl 2): S1–S41. 2010.PubMed/NCBI
|
|
6
|
Joensuu H: Risk stratification of patients
diagnosed with gastro-intestinal stromal tumor. Hum Pathol.
39:1411–1419. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors-definition, clinical, histological,
immunohistochemical and molecular genetic features and differential
diagnosis. Virchows Arch. 438:1–12. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Miettinen M, Sobin LH and Lasota J:
Gastrointestinal stromal tumors of the stomach: A
clinicopathologic, immunohistochemical and molecular genetic study
of 1765 cases with long-term follow-up. Am J Surg Pathol. 29:52–68.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Miettinen M, Makhlouf H, Sobin LH and
Lasota J: Gastrointestinal stromal tumors of the jejunum and ileum:
A clinicopathologic, immunohistochemical and molecular genetic
study of 906 cases before imatinib with long-term follow-up. Am J
Surg Pathol. 30:477–489. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Moiola C, De Luca P, Gardner K, Vazquez E
and De Siervi A: Cyclin T1 overexpression induces malignant
transformation and tumor growth. Cell Cycle. 9:3119–3126. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Luca A, De Falco M, Baldi A and Paggi
MG: Cyclin T: Three forms for different roles in physiological and
pathological functions. J Cell Physiol. 194:101–107. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
De Luca A, Russo P, Severino A, Baldi A,
Battista T, Cavallotti I, De Luca L, Baldi F, Giordano A and Paggi
MG: Pattern of expression of cyclin T1 in human tissues. J
Histochem Cytochem. 49:685–692. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sano M and Schneider MD: Cyclin-dependent
kinase-9: An RNAPII kinase at the nexus of cardiac growth and death
cascades. Circ Res. 95:867–876. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sano M, Wang SC, Shirai M, Scaglia F, Xie
M, Sakai S, Tanaka T, Kulkarni PA, Barger PM, Youker KA, et al:
Activation of cardiac Cdk9 represses PGC-1 and confers a
predisposition to heart failure. EMBO J. 23:3559–3569. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chiu YL, Cao H, Jacque JM, Stevenson M and
Rana TM: Inhibition of human immunodeficiency virus type 1
replication by RNA interference directed against human
transcription elongation factor P-TEFb (CDK9/CyclinT1). J Virol.
78:2517–2529. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chao SH and Price DH: Flavopiridol
inactivates P-TEFb and blocks most RNA polymerase II transcription
in vivo. J Biol Chem. 276:31793–31799. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Napolitano G, Majello B and Lania L: Role
of cyclinT/Cdk9 complex in basal and regulated transcription
(review). Int J Oncol. 21:171–177. 2002.PubMed/NCBI
|
|
18
|
Chen R, Keating MJ, Gandhi V and Plunkett
W: Transcription inhibition by flavopiridol: Mechanism of chronic
lymphocytic leukemia cell death. Blood. 106:2513–2519. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shan B, Zhuo Y, Chin D, Morris CA, Morris
GF and Lasky JA: Cyclin-dependent kinase 9 is required for tumor
necrosis factor-alpha-stimulated matrix metalloproteinase-9
expression in human lung adenocarcinoma cells. J Biol Chem.
280:1103–1111. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nemoto Y, Mikami T, Hana K, Kikuchi S,
Kobayashi N, Watanabe M and Okayasu I: Correlation of enhanced cell
turnover with prognosis of gastrointestinal stromal tumors of the
stomach: relevance of cellularity and p27kip1. Pathol Int.
56:724–731. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu FY, Qi JP, Xu FL and Wu AP:
Clinicopathological and immunohistochemical analysis of
gastrointestinal stromal tumor. World J Gastroenterol.
12:4161–4165. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Koon N, Schneider-Stock R, Sarlomo-Rikala
M, Lasota J, Smolkin M, Petroni G, Zaika A, Boltze C, Meyer F,
Andersson L, et al: Molecular targets for tumour progression in
gastrointestinal stromal tumours. Gut. 53:235–240. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dorn J, Spatz H, Schmieder M, Barth TF,
Blatz A, Henne-Bruns D, Knippschild U and Kramer K: Cyclin H
expression is increased in GIST with very-high risk of malignancy.
BMC Cancer. 10:3502010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wei YC, Chou FF, Li CF, Li WM, Chen YY,
Lan J, Li SH, Fang FM, Hu TH, Yu SC, et al: HuR cytoplasmic
expression is associated with increased cyclin A expression and
inferior disease-free survival in patients with gastrointestinal
stromal tumours (GISTs). Histopathology. 63:445–454.
2013.PubMed/NCBI
|
|
25
|
Rubin BP: Gastrointestinal stromal
tumours: An update. Histopathology. 48:83–96. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wong NA: Gastrointestinal stromal
tumours-an update for histopathologists. Histopathology.
59:807–821. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
ESMO/European Sarcoma Network Working
Group: Gastrointestinal stromal tumors: ESMO clinical practice
guidelines for diagnosis, treatment and follow-up. Ann Oncol.
23(Suppl 7): vii. S49–S55. 2012.
|
|
28
|
Leucci E, De Falco G, Onnis A, Cerino G,
Cocco M, Luzzi A, Crupi D, Tigli C, Bellan C, Tosi P, et al: The
role of the Cdk9/cyclin T1 complex in T cell differentiation. J
Cell Physiol. 212:411–415. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bellan C, De Falco G, Lazzi S, Micheli P,
Vicidomini S, Schürfeld K, Amato T, Palumbo A, Bagella L, Sabattini
E, et al: CDK9/CYCLIN T1 expression during normal lymphoid
differentiation and malignant transformation. J Pathol.
203:946–952. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
De Luca A, Russo P, Severino A, Baldi A,
Battista T, Cavallotti I, De Luca L, Baldi F, Giordano A and Paggi
MG: Pattern of expression of cyclin T1 in human tissues. J
Histochem Cytochem. 49:685–692. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
MacLachlan TK, Sang N, De Luca A, Puri PL,
Levrero M and Giordano A: Binding of CDK9 to TRAF2. J Cell Biochem.
71:467–478. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Peng J, Zhu Y, Milton JT and Price DH:
Identification of multiple cyclin subunits of human P-TEFb. Genes
Dev. 12:755–762. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Napolitano G, Majello B, Licciardo P,
Giordano A and Lania L: Transcriptional activity of positive
transcription elongation factor b kinase in vivo requires the
C-terminal domain of RNA polymerase II. Gene. 254:139–145. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chen R, Keating MJ, Gandhi V and Plunkett
W: Transcription inhibition by flavopiridol: Mechanism of chronic
lymphocytic leukemia cell death. Blood. 106:2513–2519. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Fu TJ, Peng J, Lee G, Price DH and Flores
O: Cyclin K functions as a CDK9 regulatory subunit and
partici-pates in RNA polymerase II transcription. J Biol Chem.
274:34527–34530. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bettayeb K, Tirado OM, Marionneau-Lambot
S, Ferandin Y, Lozach O, Morris JC, Mateo-Lozano S, Drueckes P,
Schächtele C, Kubbutat MH, et al: Meriolins, a new class of cell
death inducing kinase inhibitors with enhanced selectivity for
cyclin-dependent kinases. Cancer Res. 67:8325–8334. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
De Falco G and Giordano A: CDK9: From
basal transcription to cancer and AIDS. Cancer Biol Ther.
1:342–347. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lee DK, Duan HO and Chang C: Androgen
receptor interacts with the positive elongation factor P-TEFb and
enhances the efficiency of transcriptional elongation. J Biol Chem.
276:9978–9984. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Garriga J, Peng J, Parreño M, Price DH,
Henderson EE and Graña X: Upregulation of cyclin T1/CDK9 complexes
during T cell activation. Oncogene. 17:3093–3102. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shirin H, Kravtsov V, Shahmurov M, Shabat
VS, Krinshpon I, Alin A, Avinoach I and Avni Y: The
cyclin-dependent kinase inhibitor, p27, has no correlation with the
malignant potential of GIST. Digestion. 75:4–9. 2007. View Article : Google Scholar : PubMed/NCBI
|