Introduction
The aging trend in Japan and Korea has been
significant, with >30% of gastric cancer patients in these
countries being aged >70 years (1,2). Elderly
patients are often considered as high-risk for major abdominal
surgery due to reduced functional reserve and increased
comorbidities (3).
Since the first published report of
laparoscopy-assisted distal gastrectomy (LADG) for early gastric
cancer in 1994 (4), the number of
patients who have undergone LADG in Japan has significantly
increased; according to a Japanese nationwide survey of endoscopic
surgery, >9,000 cases of LADG were performed in 2013 (5). It has been reported that LADG for early
gastric cancer has long-term oncological outcomes equivalent to
those of conventional open distal gastrectomy (CODG) (6). In addition, several meta-analyses have
demonstrated short-term advantages for LADG over CODG in terms of
intraoperative blood loss, postoperative analgesic consumption and
length of hospital stay, as well as a better cosmetic outcome
(7–9).
Recent advances in laparoscopic techniques have facilitated the
development of several intracorporeal anastomosis methods, which
enabled totally laparoscopic gastrectomy to be performed without
additional incisions for anastomosis (10–14).
In this study, we evaluated the efficacy of totally
laparoscopic distal gastrectomy (TLDG) in elderly patients with
gastric cancer through measuring postoperative systemic responses
and postoperative analgesic consumption.
Patients and methods
Patients
A total of 102 consecutive patients with gastric
cancer underwent laparoscopic distal gastrectomy at the Department
of Surgery, National Defense Medical College Hospital (Tokorozawa,
Japan) between 2010 and 2014. Prior to August, 2012, LADG was
performed in 45 patients; after that time, TLDG was performed in 57
patients among all eligible cases. The patients were classified
into elderly (aged ≥75 years) and non-elderly (aged <75 years)
groups. The clinicopathological characteristics of the patients
were evaluated on the basis of the Japanese Classification of
Gastric Carcinoma (3rd English edition) published by the Japanese
Gastric Cancer Association (15).
There was no change in the delivery of postoperative care during
this period. The medical and nursing charts of the patients were
retrospectively evaluated for preoperative status, type of surgical
procedure, analgesic consumption and postoperative systemic
response, including white blood cell (WBC) count, body temperature,
heart rate, levels of C-reactive protein (CRP) and all laboratory
data up to postoperative day (POD) 7.
This was a non-randomized study and informed consent
was obtained from all the participants prior to study
initiation.
Operative procedures
Following induction of general anesthesia with an
epidural catheter, each patient was placed in the supine position.
The surgeon was positioned on the left side of the patient, the
first assistant was on the right, and the laparoscopist was located
between the abducted legs of the patient. A camera port was
inserted into a median umbilical incision. Following this, a
pneumoperitoneum of 12 mmHg was created and 4 additional ports (2
ports of 12 mm in diameter and 2 ports of 5 mm in diameter) were
inserted under laparoscopic imaging into the left upper, right
lower, left lower, and right upper quadrants. An
ultrasonically-activated sealing device (Harmonic Scalpel Ace;
Ethicon, Tokyo, Japan) and a vessel-sealing device (LigaSure V;
Tyco Healthcare, Tokyo, Japan) were used in the dissecting
procedures.
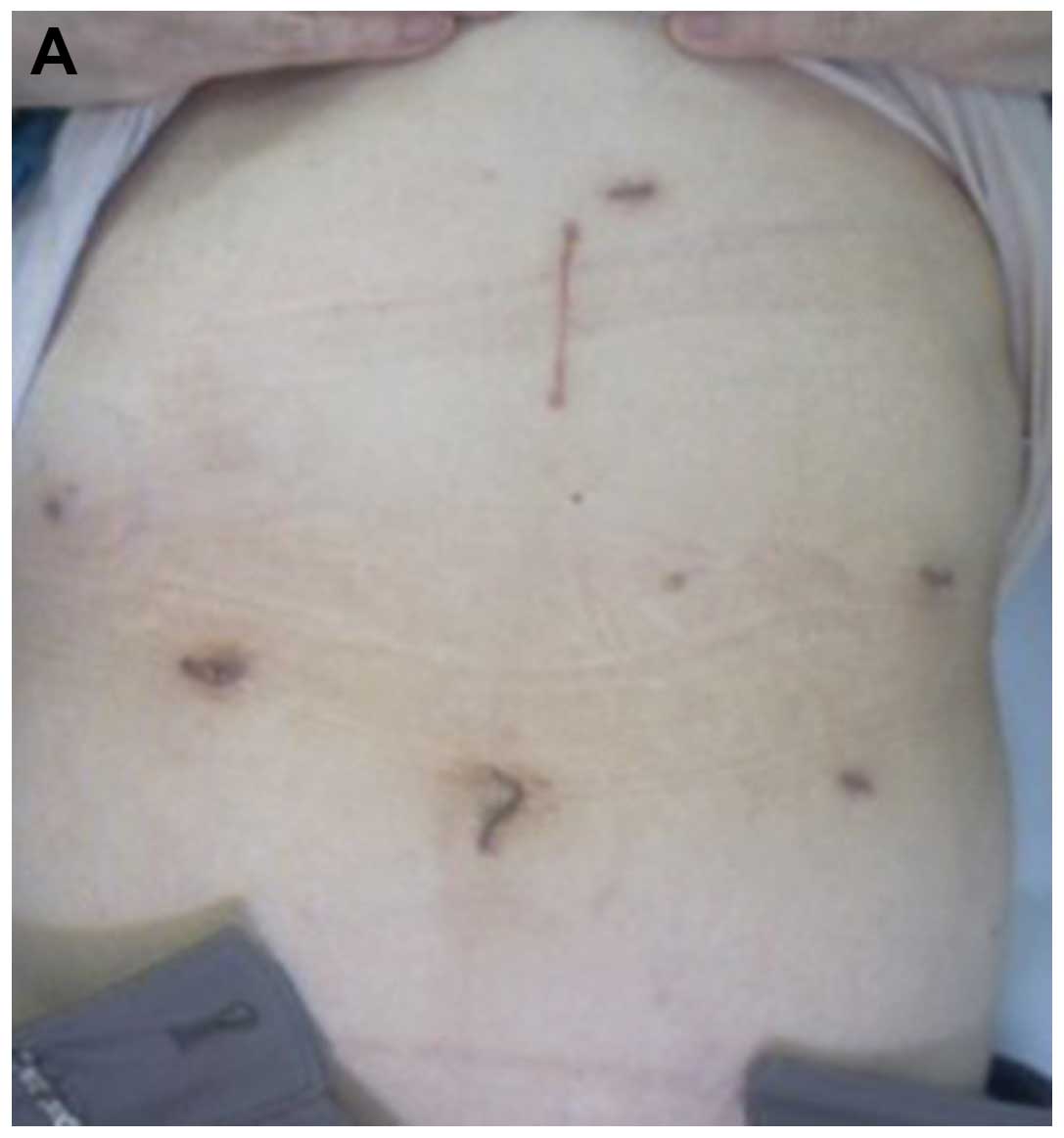
For the LADG cases, following gastrectomy with
lymphadenectomy, depending on the tumor stage, a median superior
abdominal incision ~4 cm in length was created (Fig. 1A). A Billroth I reconstruction was
then usually performed by the hemi-double stapling technique using
a 25-mm circular stapler (Covidien, Tokyo, Japan), as previously
described (16). The stomach was
transected with a linear stapler and the specimen was collected
through a mini-laparotomy. When the extracorporeal Billroth I
reconstruction was expected to be strained, a Roux-en-Y
reconstruction was selected and anastomoses were performed through
mini-laparotomy.
For cases with TLDG, following gastrectomy, the
umbilical trocar incision was extended to ~2 cm by enlarging the
median fascia and skin incisions; tumors and surrounding tissues
were pulled out through the umbilical incision (Fig. 1B). Intracorporeal Billroth I
anastomosis was performed using the δ-shaped anastomosis, as
previously described (13). When a
Roux-en-Y reconstruction was employed, all anastomoses were
performed using laparoscopic linear staplers and/or a
hand-suturing technique.
Postoperative analgesia
Postoperative pain was controlled by epidural
anesthesia, and patients were allowed to have additional analgesia
when necessary. The surgeon in charge determined the time of
epidural catheter removal, while managing the patient's pain. Oral
or intravenous non-steroidal anti-inflammatory drugs or intravenous
pentazocine hydrochloride were employed as rescue medications.
Statistical analysis
The statistical analyses were performed using the
JMP 10.0.0 software package (SAS Institute, Cary, NC, USA). The
data are expressed as the mean ± standard error. Statistical
analyses were performed using the Student's t-test or Chi-square
test with the Fisher's exact test, whichever was considered
appropriate. P<0.05 was considered to indicate a statistically
significant difference.
Results
Demographic data and surgical outcomes
of the elderly and non-elderly groups
The elderly and non-elderly groups were matched for
age, gender, location and size of tumor, histological
differentiation, pathological tumor depth, nodal involvement and
stage, except for body mass index (BMI) (Table I). In addition, there were no
differences in age, gender, location and size of tumor,
histological differentiation, nodal involvement, BMI or tumor stage
among the patients who underwent TLDG and those who underwent LADG
for both groups (data not shown). When compared with the
non-elderly group, the elderly group exhibited a higher frequency
of comorbidities, such as cardiovascular and respiratory diseases
(Table I). There was no difference in
operative outcome between the two groups, such as extent of
lymphadenectomy, total number of harvested lymph nodes and type of
reconstruction (Table II). Although
there was no difference in the occurrence of postoperative
complications, it required a significantly longer time for the
elderly group to start oral intake and be discharged from the
hospital; in addition, the elderly group had more intraoperative
bleeding compared with the non-elderly group. There were no cases
of conversion to open surgery in either group.
 | Table I.Demographic data of the elderly and
non-elderly groups. |
Table I.
Demographic data of the elderly and
non-elderly groups.
| Characteristics | Non-elderly group
(n=77) | Elderly group
(n=25) | P-value |
|---|
| Gender, n (%) |
|
|
|
| Male | 56 (72.7) | 20 (80.0) | 0.469 |
|
Female | 21 (27.3) | 5 (20.0) |
|
| Body mass index
(kg/m2) | 22.3±3.1 | 20.4±2.1 | 0.003 |
| Tumor location, n
(%) |
|
|
|
| Middle
third | 22 (28.6) | 8 (32.0) | 0.772 |
| Lower
third | 55 (71.4) | 17 (68.0) |
|
| Maximal tumor size
(mm) | 38.5±23.2 | 35.3±16.6 | 0.523 |
| Histological
classification, n (%) |
|
|
|
|
Intestinal | 44 (57.1) | 14 (56.0) | 0.920 |
|
Diffuse | 33 (42.9) | 11 (44.0) |
|
| Tumor depth |
|
|
|
| pT1 | 49 (63.6) | 21(84.0) | 0.057 |
|
pT2-T4 | 28 (36.4) | 4 (16.0) |
|
| Lymph node
metastasis, n (%) |
|
|
|
| pN0 | 60 (77.9) | 20 (80.0) | 0.826 |
|
pN1–3 | 17 (22.1) | 5 (20.0) |
|
| pStage, n (%) |
|
|
|
| I | 59 (76.6) | 21 (84.0) | 0.474 |
| II | 12 (15.6) | 2 (8.0) |
|
| III | 6 (7.8) | 1 (4.0) |
|
| Comorbidity, n
(%) |
|
|
|
| Yes | 32 (41.6) | 21 (84.0) | <0.001 |
| No | 45 (58.4) | 4 (16.0) |
|
| Number of
comorbidities, (%) |
|
|
|
| 0 | 45 (58.4) | 4 (16.0) | <0.001 |
| 1 | 23 (29.9) | 12 (48.0) |
|
| 2 | 9 (11.7) | 9 (36.0) |
|
| Comorbid diseases, n
(%) |
|
|
|
|
Cardiovascular | 24 (31.2) | 15 (60.0) | 0.010 |
|
Respiratory | 3 (3.9) | 4 (16.0) | 0.038 |
|
Liver | 1 (1.3) | 0 (0.0) | 0.567 |
|
Renal | 1 (1.3) | 1 (4.0) | 0.397 |
|
Diabetes mellitus | 6 (7.8) | 5 (20.0) | 0.087 |
|
Collagen disease | 3 (3.9) | 0 (0.0) | 0.317 |
| Thyroid
disease | 0 (0.0) | 1 (4.0) | 0.078 |
 | Table II.Surgical outcomes of the elderly and
non-elderly groups. |
Table II.
Surgical outcomes of the elderly and
non-elderly groups.
| Variables | Non-elderly group
(n=77) | Elderly group
(n=25) | P-value |
|---|
| Lymphadenectomy, n
(%) |
|
|
|
| D1,
D1+ | 39 (50.6) | 18 (72.0) | 0.062 |
| D2 | 38 (49.4) | 7 (28.0) |
|
| Surgery, n (%) |
|
|
|
|
LADG | 35 (45.5) | 10 (40.0) | 0.633 |
|
TLDG | 42 (54.5) | 15 (60.0) |
|
| Total number of
harvested LNs | 34.9±17.1 | 34.6±19.3 | 0.932 |
| Reconstruction, n
(%) |
|
|
|
|
Billroth I | 45 (58.4) | 19 (76.0) | 0.115 |
|
Roux-en-Y | 32 (41.6) | 6 (24.0) |
|
| Time until start of
oral intake (days) | 3.3±0.6 | 4.6±3.7 | 0.005 |
| Hospital stay
(days) | 9.8±13.2 | 13.2±10.6 | 0.022 |
| Operative time
(min) | 247.6±48.7 | 243.5±60.5 | 0.839 |
| Intraoperative
bleeding (ml) | 54.1±108.9 | 109.8±151.7 | 0.048 |
| Conversion to open
surgery, n (%) | 0 (0.0) | 0 (0.0) | >0.99 |
| Postoperative
complications, n (%) |
|
|
|
|
Yes | 11 (14.3) | 5 (20.0) | 0.495 |
| No | 66 (85.7) | 20 (80.0) |
|
Pneumonia | 2 (2.6) | 0 (0.0) | 0.416 |
|
Leakage | 2 (2.6) | 3 (12.0) | 0.059 |
|
SSI | 2 (2.6) | 1 (4.0) | 0.718 |
|
DGE | 2 (2.6) | 0 (0.0) | 0.416 |
|
Pancreatic fistula | 1 (1.3) | 0 (0.0) | 0.567 |
|
Bleeding | 1 (1.3) | 0 (0.0) | 0.567 |
|
Cholangitis | 0 (0.0) | 1 (4.0) | 0.078 |
|
UTI | 1 (1.3) | 0 (0.0) | 0.567 |
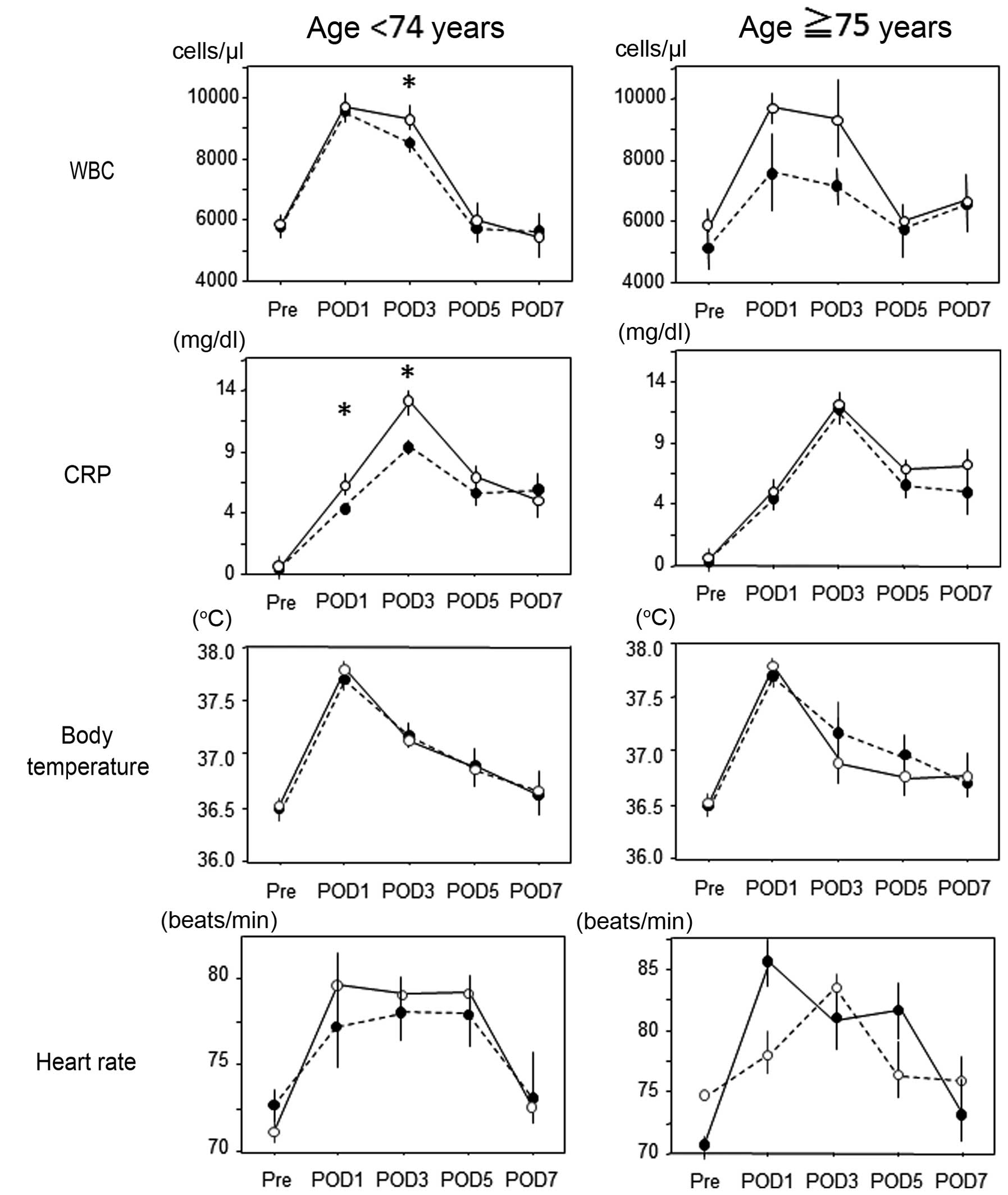
Postoperative systemic responses of
the elderly and non-elderly groups
There was no difference in the postoperative WBC,
CRP, body temperature or heart rate between the two groups (data
not shown). In the non-elderly group, the WBC levels on POD3 and
the CRP levels on POD1 and 3 in patients who underwent TLDG were
significantly higher compared with those in patients who underwent
LADG; these differences were not observed in the elderly group
(Fig. 2).
Postoperative analgesic
consumption
No difference was observed in the duration of
epidural anesthesia between the two groups (Table III). The elderly group required less
frequent additional analgesia postoperatively, albeit not
significantly. We next compared the postoperative analgesia
consumption according to surgical procedure between the two groups
(Table IV). In both groups, the
duration of epidural anesthesia in patients who underwent TLDG was
shorter compared with that in patients who underwent LADG. The
frequencies of additional analgesia use on POD1 and 2 in patients
who underwent TLDG were lower compared with that in patients who
underwent LADG in the elderly group, and the total consumption of
additional analgesics until POD5 in patients who underwent TLDG was
significantly lower compared with that in patients who underwent
LADG in the elderly group; there was no such trend in the
non-elderly group. In addition, as compared with the patients in
the non-elderly group on POD1 and 2, the consumption and the need
for additional analgesia for patients who underwent TLDG in the
elderly group were significantly lower.
 | Table III.Postoperative analgesia consumption
in the elderly and non-elderly groups. |
Table III.
Postoperative analgesia consumption
in the elderly and non-elderly groups.
| Variables | Non-elderly group
(n=77) | Elderly group
(n=25) | P-value |
|---|
| Duration of
epidural anesthesia (days) | 2.8±0.8 | 2.8±0.8 | 0.971 |
| Frequency of
additional analgesia use |
|
|
|
|
POD1 | 0.51±0.75 | 0.24±0.60 | 0.111 |
|
POD2 | 1.00±1.01 | 0.64±0.86 | 0.113 |
|
POD3 | 0.82±0.90 | 0.64±0.86 | 0.387 |
|
POD4 | 0.53±0.87 | 0.28±0.61 | 0.181 |
|
POD5 | 0.26±0.55 | 0.20±0.41 | 0.617 |
|
Total | 3.12±2.85 | 2.00±2.57 | 0.085 |
| Incidence of using
additional analgesia, n (%) |
|
|
|
|
POD1 | 15 (35.7) | 1 (6.7) | 0.106 |
|
POD2 | 25 (59.5) | 5 (33.3) | 0.147 |
|
POD3 | 22 (52.4) | 4 (26.7) | 0.072 |
|
POD4 | 14 (33.3) | 2 (13.3) | 0.280 |
|
POD5 | 9 (21.4) | 2 (13.3) | 0.280 |
 | Table IV.Postoperative analgesia consumption
according to the surgical procedure in the elderly and non-elderly
groups. |
Table IV.
Postoperative analgesia consumption
according to the surgical procedure in the elderly and non-elderly
groups.
|
| Non-elderly
group |
| Elderly group |
|
|---|
|
|
|
|
|
|
|---|
| Variables | TLDG (n=42) | LADG (n=35) | P-value | TLDG (n=15) | LADG (n=10) | P-value |
|---|
| Duration of
epidural anesthesia (days) | 2.5±0.8 | 2.8±0.7 | 0.084 | 2.6±0.6 | 3.1±0.8 | 0.135 |
| Frequency of
additional analgesia use |
|
|
POD1 | 0.45±0.67 | 0.57±0.85 | 0.656 |
0.07±0.26a | 0.50±0.84 | 0.108 |
|
POD2 | 1.04±0.99 | 0.94±1.06 | 0.476 |
0.40±0.63a | 1.00±1.05 | 0.122 |
|
POD3 | 0.83±0.88 | 0.80±0.93 | 0.800 | 0.40±0.74 | 1.00±0.94 | 0.087 |
|
POD4 | 0.50±0.80 | 0.57±0.95 | 0.879 | 0.20±0.56 | 0.40±0.70 | 0.340 |
|
POD5 | 0.26±0.54 | 0.26±0.56 | 0.902 | 0.13±0.35 | 0.30±0.48 | 0.317 |
|
Total | 3.10±2.64 | 3.14±3.13 | 0.840 |
1.20±2.11a | 3.20±2.82 | 0.015 |
| Incidence of
additional analgesia use, n (%) |
|
|
POD1 | 15 (35.7) | 14 (40.0) | 0.331 | 1
(6.7)a | 3 (30) | 0.106 |
|
POD2 | 25 (59.5) | 22 (62.9) | 0.494 | 5 (33.3) | 6 (60) | 0.147 |
|
POD3 | 22 (52.4) | 18 (51.4) | 0.534 | 4 (26.7) | 6 (60) | 0.072 |
|
POD4 | 14 (33.3) | 12 (34.3) | 0.927 | 2 (13.3) | 3 (30) | 0.280 |
|
POD5 | 9 (21.4) | 7 (20) | 0.614 | 2 (13.3) | 3 (30) | 0.280 |
Discussion
As elderly individuals are currently representing a
rapidly increasing percentage of the population, the mean age and
number of patients with various malignancies have increased
(1). The functional capacity of
organs decreases with age, resulting in a decreased reserve and
lower ability to endure stress (17);
therefore, advanced age is a significant risk factor for increased
mortality (18). However, advances in
surgical and anesthesiology techniques have reportedly reduced
surgical complications and have, consequently, improved the
short-term surgical outcomes in elderly patients (19,20).
In this study, there were no differences in
postoperative systemic responses (WBC, CRP, body temperature and
heart rate) between the TLDG and LADG procedures in the elderly
group, and the total consumption of additional analgesics until
POD5 in patients who underwent TLDG was significantly lower
compared with that in patients who underwent LADG in the elderly
group; the patients who underwent TLDG had a relatively shorter
duration of epidural anesthesia. Our present data pose a question
regarding the mechanism(s) of differential postoperative pain
between elderly and non-elderly patients that may be explained as
follows: i) It has been reported that aging-related anatomic
changes may affect the spreading pattern of the local anesthetic
injected into the epidural space (21), which may decrease the anesthesia of
the upper abdomen; and ii) there may be a different susceptibility
to pain and/or analgesic agents between the elderly and
non-elderly patients; a negative correlation with age was observed
for postoperative pain intensity, as well as analgesic consumption
(22–24). Moreover, Sommer et al (25) demonstrated that patients aged ≥65
years experienced less pain compared with patients aged 41–64 years
following major surgery.
Jin et al (26)
reported that persistent postoperative pain may cause cardiac,
respiratory and cerebrovascular complications, resulting in an
increase in the risk of an adverse outcome. Adequate postoperative
pain management is not only indispensable for patient comfort, but
it has also been reported that there is a strong association
between effective postoperative pain management and the prevention
of postoperative complications (22,27). In
this regard, TLDG for gastric cancer in the elderly may be the
optimal surgical approach in terms of postoperative pain management
to improve short-term outcome.
In conclusion, TLDG is suitable for treating elderly
patients with gastric cancer, who exhibit the highest mortality
rate in the adult surgical population, in terms of postoperative
pain.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
|
1
|
Levi F, Lucchini F, Negri E, Boyle P and
La Vecchia C: Changed trends of cancer mortality in the elderly.
Ann Oncol. 12:1467–1477. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim MG, Kim HS, Kim BS and Kwon SJ: The
impact of old age on surgical outcomes of totally laparoscopic
gastrectomy for gastric cancer. Surg Endosc. 27:3990–3997. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Creditor MC: Hazards of hospitalization of
the elderly. Ann Intern Med. 118:219–223. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kitano S, Iso Y, Moriyama M and Sugimachi
K: Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc
Endosc. 4:146–148. 1994.PubMed/NCBI
|
|
5
|
Lu C, Zhou S, Peng Z and Chen L: Quality
of D2 lymphadenectomy for advanced gastric cancer: Is
laparoscopic-assisted distal gastrectomy as effective as open
distal gastrectomy? Surg Endosc. 29:1537–1544. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kitano S, Shiraishi N, Uyama I, Sugihara K
and Tanigawa N: Japanese Laparoscopic Surgery Study Group: A
multicenter study on oncologic outcome of laparoscopic gastrectomy
for early cancer in Japan. Ann Surg. 245:68–72. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zeng YK, Yang ZL, Peng JS, Lin HS and Cai
L: Laparoscopy-assisted versus open distal gastrectomy for early
gastric cancer: Evidence from randomized and nonrandomized clinical
trials. Ann Surg. 256:39–52. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen XZ, Hu JK, Yang K, Wang L and Lu QC:
Short-term evaluation of laparoscopy-assisted distal gastrectomy
for predictive early gastric cancer: A meta-analysis of randomized
controlled trials. Surg Laparosc Endosc Percutan Tech. 19:277–284.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cheng Q, Pang TC, Hollands MJ, Richardson
AJ, Pleass H, Johnston ES and Lam VW: Systematic review and
meta-analysis of laparoscopic versus open distal gastrectomy. J
Gastrointest Surg. 18:1087–1099. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim DG, Choi YY, An JY, Kwon IG, Cho I,
Kim YM, Bae JM, Song MG and Noh SH: Comparing the short-term
outcomes of totally intracorporeal gastroduodenostomy with
extracorporeal gastroduodenostomy after laparoscopic distal
gastrectomy for gastric cancer: A single surgeon's experience and a
rapid systematic review with meta-analysis. Surg Endosc.
27:3153–3161. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tsujimoto H, Uyama I, Yaguchi Y, Kumano I,
Takahata R, Matsumoto Y, Yoshida K, Horiguchi H, Aosasa S, Ono S,
et al: Outcome of overlap anastomosis using a linear stapler after
laparoscopic total and proximal gastrectomy. Langenbecks Arch Surg.
397:833–840. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Inaba K, Satoh S, Ishida Y, Taniguchi K,
Isogaki J, Kanaya S and Uyama I: Overlap method: Novel
intracorporeal esophagojejunostomy after laparoscopic total
gastrectomy. J Am Coll Surg. 211:e25–e29. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kanaya S, Kawamura Y, Kawada H, Iwasaki H,
Gomi T, Satoh S and Uyama I: The delta-shaped anastomosis in
laparoscopic distal gastrectomy: Analysis of the initial 100
consecutive procedures of intracorporeal gastroduodenostomy.
Gastric Cancer. 14:365–371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N,
Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T, et al:
Advantages of totally laparoscopic distal gastrectomy over
laparoscopically assisted distal gastrectomy for gastric cancer.
Surg Endosc. 23:2374–2379. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Japanese Gastric Cancer Association:
Japanese classification of gastric carcinoma: 3rd English edition.
Gastric Cancer. 14:101–112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Omori T, Oyama T, Akamatsu H, Tori M,
Ueshima S, Nakahara M and Toshirou N: A simple and safe method for
gastrojejunostomy in laparoscopic distal gastrectomy using the
hemidouble-stapling technique: Efficient purse-string stapling
technique. Dig Surg. 26:441–445. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jones AG and Hunter JM: Anaesthesia in the
elderly. Special considerations. Drugs Aging. 9:319–331. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Takeshita H, Ichikawa D, Komatsu S, Kubota
T, Okamoto K, Shiozaki A, Fujiwara H and Otsuji E: Surgical
outcomes of gastrectomy for elderly patients with gastric cancer.
World J Surg. 37:2891–2898. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fujiwara S, Noguchi T, Harada K, Noguchi
T, Wada S and Moriyama H: How should we treat gastric cancer in the
very elderly? Hepatogastroenterology. 59:620–622. 2012.PubMed/NCBI
|
|
20
|
Dittmar Y, Rauchfuss F, Götz M,
Scheuerlein H, Jandt K and Settmacher U: Impact of clinical and
pathohistological characteristics on the incidence of recurrence
and survival in elderly patients with gastric cancer. World J Surg.
36:338–345. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sharrock NE: Epidural anesthetic dose
responses in patients 20 to 80 years old. Anesthesiology.
49:425–428. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gagliese L and Katz J: Age differences in
postoperative pain are scale dependent: A comparison of measures of
pain intensity and quality in younger and older surgical patients.
Pain. 103:11–20. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ip HY, Abrishami A, Peng PW, Wong J and
Chung F: Predictors of postoperative pain and analgesic
consumption: A qualitative systematic review. Anesthesiology.
111:657–677. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shafer SL: The pharmacology of anesthetic
drugs in elderly patients. Anesthesiol Clin North America. 18:1–29.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sommer M, de Rijke JM, van Kleef M,
Kessels AG, Peters ML, Geurts JW, Patijn J, Gramke HF and Marcus
MA: Predictors of acute postoperative pain after elective surgery.
Clin J Pain. 26:87–94. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jin F and Chung F: Minimizing
perioperative adverse events in the elderly. Br J Anaesth.
87:608–624. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Joshi GP and Ogunnaike BO: Consequences of
inadequate postoperative pain relief and chronic persistent
postoperative pain. Anesthesiol Clin North America. 23:21–36. 2005.
View Article : Google Scholar : PubMed/NCBI
|