Introduction
Features of right- and left-sided breast cancer (BC)
have been poorly studied to date. Publications on lateral
differences and the incidence of BC are few, and only a single
study has been published on lateral differences and survival
following BC (1–3). Results from population studies have
indicated that the frequency of occurrence of left-sided BC is
higher compared with right-sided BC (4–6). The
distinction is not great (4–8%), although the difference is not
considered to be trivial, and may be associated with unidentified
etiological factors (7).
The laterality of BC does not belong to recognized
predictive factors. In a study performed by the Israeli Cancer
Register, it was suggested that the survival of patients with BC is
not dependent on tumor laterality (8). However, the results of other previous
studies showed that the survival of patients with left-sided BC is
higher compared with patients with the right-sided BC (9,10).
Studies on morphological differences of right-and
left-sided BC are also few. Erendeeva et al (9) performed a comparative analysis of right-
and left-sided BC on 45 clinico-morphological parameters. Results
from this analysis revealed a number of statistically significant
characteristics, including size of the primary center, histological
type of tumor, existence of metastasis in regional lymph nodes and
background pathology. This study established that primary tumors
localized on the right side were significantly more in size
compared with tumors of the left side, and had a significant
tendency to metastasize in regional lymph nodes. Among the various
forms of a mastopathy (background pathology), a particular emphasis
was placed on the existence of mazoplasia, the significant
processes of proliferation in breast tissue. It was noted that
mazoplasia associated with right-side tumors was observed five
times more often compared with left-side tumors. The authors
considered that asymmetry of hormonal and immune influences in a
human body could be the predominant reason for asymmetry of the
clinico-morphological parameters of BC. Nouh et al (11) showed that metastases in regional lymph
nodes of left-sided BC were observed less frequently compared with
right-sided BC. The authors hypothesized that this may be
associated with the greater activity of the right hand.
Proliferative activity of a tumor defines its
aggression, and is an indicator of the prognosis (12). A number of indicators of proliferative
activity are known. The greatest interest in recent years has
focused on the biomarker, Ki-67, as an index of proliferative
activity. Numerous previous studies have shown that Ki-67 is an
independent predictive marker for a local relapse, and for overall
and disease-free survival (13–23). No
previous studies, to the best of our knowledge, have shown lateral
differences in Ki-67 in BC. Research in this area may enrich our
knowledge of the natural history of BC and assist in creating
personalized treatment for this disease.
Materials and methods
Following the protocols of immunohistochemical
research of the Rostov Regional Morphological Bureau (2008–2010),
an analysis of biopsy material from 500 patients was performed.
Four BC parameters were investigated: The expression levels of the
estrogen receptors (ERs), of the progesterone receptors (PRs), of
Ki-67 and the epidermal growth factor receptor, C-erbB-2
(Her-2-neu). From these 500 BC cases, right-sided localization of
the BC was observed in 238 (47.6%) patients; that of left-sided BC
was observed in 262 (52.4%) patients. The present study aimed to do
the following: i) Perform comparative analysis of Ki-67 levels in
groups of patients with right- or left-sided BC; ii) to define
lateral differences of Ki-67 levels in three different age groups
(≤49, 50–59 and ≥60 years); and iii) to estimate changes in Ki-67
levels, depending on other parameters (ER, PR, Her-2-neu).
The statistical analysis was performed with the use
of Statistics 8.0 software (StatSoft, Inc., Tulsa, OK, USA). To
define interrelations, correlation matrixes were created.
Comparison of different groups was performed using Student's
t-test. In the case of the small size of groups, Fisher's exact
test was used. Comparison of averages was performed by analysis of
variance. The data are shown as percentages, with 95% confidence
intervals (95% CI) ± the standard error of the mean. P<0.05 was
considered to indicate a statistically significant difference.
Production of immunohistochemical reactions and
interpretation of the results were performed, according to a
previous study (24). For the light
optical and immunohistochemical experiments, biopsy material was
fixed in 10% buffering (neutral) formalin (BlikMedicalProduction,
Taganrog, Russia) within 24 h at room temperature. Following
treatment with paraffin (BlikMedicalProduction), serial cuts 4
µm-thick were performed. The cut sections were mounted onto the
subject glasses and were loaded or covered with poly-L-lysine
(Sigma-Aldrich, St. Louis, MO, USA). For the light optical
experiments, the cut sections were stained with hematoxylin and
eosin (DakoCytomation, Hamburg, Germany). For the
immunohistochemical experiments, the cut sections made from
paraffin blocks were placed in the thermostat for 30 min at 56°C.
Paraffin was removed from the sections by incubating in xylol
(BlikMedicalProduction) five times. The duration of one incubation
was between 5 and 10 min. The sections were subsequently dehydrated
in three changes of absolute ethanol for 3 min, prior to placement
in distilled water. To visualize the proteins, the sections were
incubated with buffered solution (DakoCytomation) of primary
antibodies (DakoCytomation, Hamburg, Germany) in a water bath for
20 min at 95°C. The tissue sections were subsequently washed in the
buffer. Endogenous peroxidase activity was suppressed using a
hydrogen peroxide-based blocking solution (DakoCytomation) for 5–7
min at room temperature. Immunohistochemical reactions were
performed in an automatic robotized device (Autostainer Plus;
DakoCytomation) according to the following protocol: Incubation
with primary antibodies (15–30 min, according to antibody
protocol), incubation with secondary antibodies (30 min),
incubation with a substratum chromogen (8 min) and staining of
kernels with Mayer's hematoxylin (5 min). A Dako EnVision system
and peroxidase (antirabbit, antimouse) was used. The sections were
washed using Tris-HCl, containing Triton-X, to reduce background
coloring and promote penetration of solutions into the tissue. For
each studied gene, a negative control was used instead of primary
antibodies, and also a positive control, the fabric which
containing this antigen. The following mouse monoclonal antibodies
were used: Anti-progesterone receptor (Clone PgR 636; Target
Retrieval S 1700 pH 6.0; dilution 2:100), anti-Human Ki-67 (Clone
MIB-1; Target Retrieval S 1700 pH 6.0; dilution 1:100), all from
DakoCytomation. HER-2/neu protein expression was performed using
the HercepTest, according to the manufacturers instructions
(DakoCytomation).
Results
The proliferative activity of Ki-67 significantly
correlated with the BC laterality (r=−0.08; P=0.046). A higher
Ki-67 index corresponded with right-side localization of the BC.
The Ki-67 median for the right-sided BC was 18.1% (95%
CI=15.3–21.0) and for the left-sided BC was 14.5% (95%
CI=12.2–16.8). A t-test revealed the significance of differences
(P=0.046).
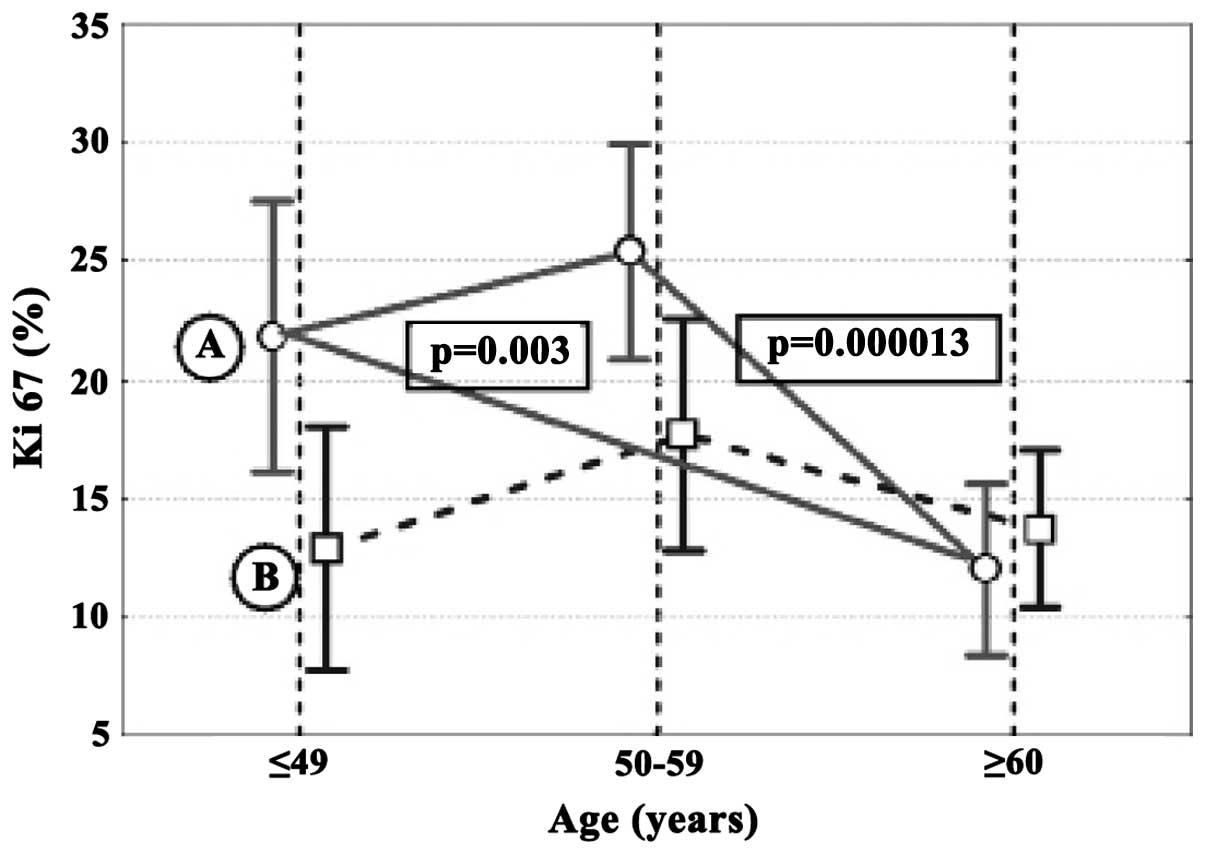
Correlation of Ki-67 with the age of the patients
was characteristic only for right-sided BC (r=−0.28; P<0.001).
The maximum Ki-67 values for right-sided BC were observed in the
age interval of 50–59 years (25.3%; 95% CI=19.4–31.3) and the
minimum Ki-67 values were observed in the age interval ≥60 years
(12.0%; 95% CI = 9.1–14.8; Fig. 1).
The comparative analysis revealed that tumors of patients with
right-sided BC of an age interval ≥60 years had a Ki-67 index
significantly lower compared with tumors of patients at the age of
≤49 (P=0.003) and 50–59 years (P=0.000013). In the left-sided BC,
the Ki-67 index in age intervals did not significantly differ. An
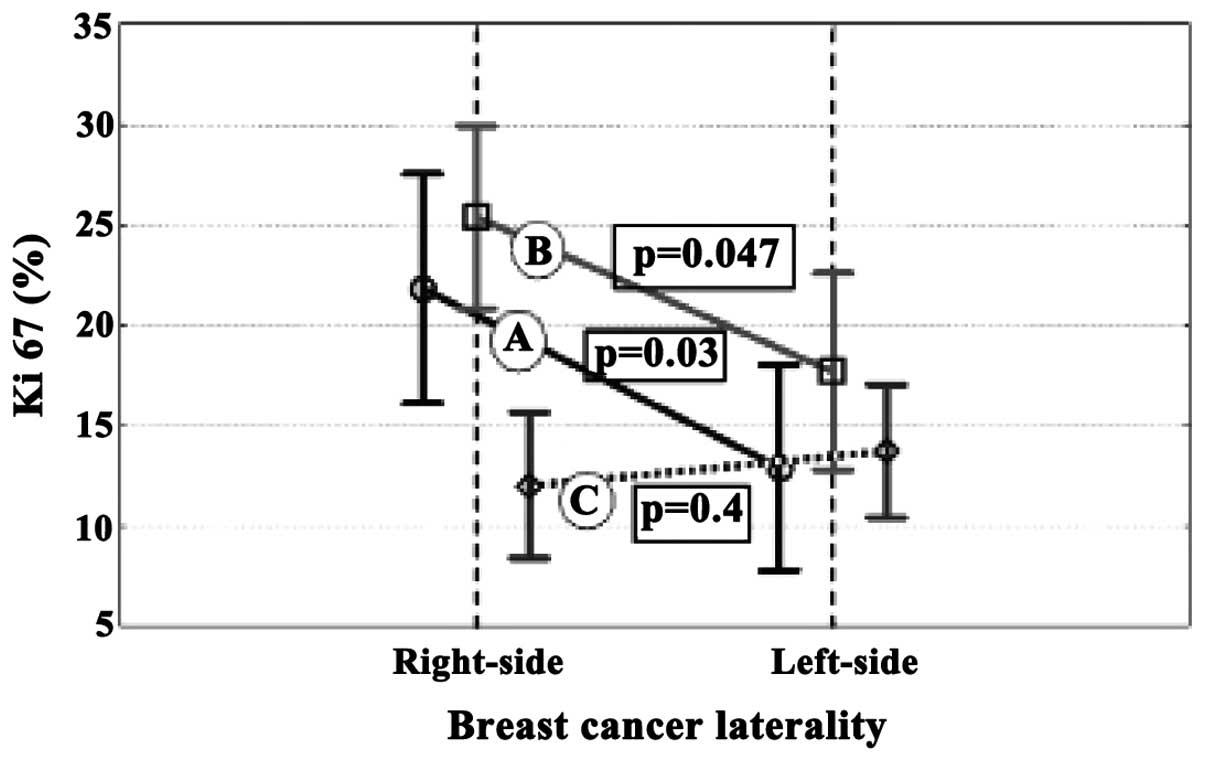
assessment of the lateral differences in age intervals established
that the Ki-67 index of right-sided BC was significantly higher
compared with left-sided BC in two age groups, ≤49 (P=0.038) and
50–59 (P=0.047) years. For the ≥60 years age group, lateral
differences in Ki-67 were not observed (P=0.4; Fig. 2).
The analysis of lateral differences of Ki-67 in
tumors of different receptor profiles revealed significant
differences in Ki-67 of the right- and left-sided BC under
ER+ PR− (P=0.007) and ER−
PR− (P=0.016) conditions, therefore, when there is no
expression of PR. In these cases, the Ki-67 index was higher in
right-sided BC (Table I). In general,
the maximum Ki-67 index was found in the group of right-sided
tumors with the ER− PR− receptor profile,
where the Ki-67 index reached 33.7±5.1%.
 | Table I.Ki-67 expression in right- and
left-sided BC in different receptor profiles. |
Table I.
Ki-67 expression in right- and
left-sided BC in different receptor profiles.
|
| Right-side | Left-side |
|
|---|
|
|
|
|
|
|---|
| Receptor profile | n | Ki-67 (%) | n | Ki-67 (%) | P-value |
|---|
| ER+
PR+ | 136 | 11.4±3.2 | 155 | 12.3±3.0 | 0.610 |
| ER+
PR− | 39 | 21.4±5.9 | 37 | 9.5±6.1 | 0.007 |
| ER−
PR+ | 10 | – | 1 | – | – |
| ER−
PR− | 53 | 33.7±5.1 | 69 | 22.2±4.5 | 0.016 |
In tumors with the ER+ PR+
receptor profile, lateral differences of the BC on the Ki-67 index
were absent (r=0.61). The assessment of the ER−
PR+ receptor profile was not performed due to
insignificant numbers of samples.
Expression of the epidermal growth factor receptor,
C-erbB-2 (Her-2-neu), positively correlated with the Ki-67 index
(right-side, r=0.27; P<0.001; left-side, r=0.17; P=0.006).
Discussion
Features of right-sided BC, including the bigger
size of primary tumor and more frequent metastasis in regional
lymph nodes (9,11), as revealed by previous studies, can be
partly explained by the results of the present research. It is
known that the Ki-67 index is directly connected with certain
biological characteristics, including aggressive growth and
metastatic potential.
Notably, the significantly higher rate of Ki-67 for
the right-sided BC, in comparison with the left-sided BC, was
observed only up until 60 years. In women who developed BC at ≥60
years, lateral differences in Ki-67 index were not observed. It is
also necessary to note that, in patients with right-sided BC, those
women who became ill at ≥60 years were characterized by
significantly lower Ki-67 levels compared with patients of the two
other age groups. This suggested a dependence of the proliferative
activity of the BC on the functioning mechanisms and the cessation
of the menstrual cycle. In the ≥60 years group, Ki-67 was at a
markedly low level and exhibited no lateral differences.
Results of the present study demonstrated the
differences in the expression of Ki-67 of right- and left-side
tumors of the breast. Age dynamics of lateral differences of Ki-67
in BC is a reflection of age dynamics of structural-functional
asymmetry of a human body (25–27). In
turn, asymmetry of neurohumoral regulation of the organism can be
directly connected with mechanisms of the menstrual cycle (28).
Acknowledgements
The author would like to thank Dr Poroshenko for
assistance in the interpretation of the results.
Glossary
Abbreviations
Abbreviations:
|
BC
|
breast cancer
|
|
ER
|
estrogen receptor
|
|
PR
|
progesterone receptor
|
|
CI
|
confidence interval
|
References
|
1
|
Fatima N, Zaman MU, Maqbool A, Khan SH and
Riaz N: Lower incidence but more aggressive behavior of right sided
breast cancer in pakistani women: does right deserve more respect?
Asian Pac J Cancer Prev. 14:43–45. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Borisenkov MF and Bazhenov SM: Survival in
human breast cancer: effects of tumor laterality and the time of
year of surgery. Human Physiology. 27:631–634. 2001.(In Russian).
View Article : Google Scholar
|
|
3
|
Bao J, Yu K-D, Jiang Y-Z, Shao Z-M and Di
G-H: The effect of laterality and primary tumor site on
cancer-specific mortality in breast cancer: a SEER population-based
study. PLoS ONE. 9:e948152014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Aareleĭd TP and Khint EK: Prevalence of
tumors in the left breast. Vopr Onkol. 33:37–42. 1987.(In
Russian).
|
|
5
|
Tulinius H, Sigvaldason H and Olafsdóttir
G: Left and right sided breast cancer. Pathol Res Pract. 186:92–94.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Weiss HA, Devesa SS and Brinton LA:
Laterality of breast cancer in the United States. Cancer Causes
Control. 7:539–543. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Perkins CI, Hotes J, Kohler BA and Howe
HL: Association between breast cancer laterality and tumor
location, United States, 1994–1998. Cancer Causes Control.
15:637–645. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Melnik Y, Slater PE, Steinitz R and Davies
AM: Breast cancer in Israel: Laterality and survival. J Cancer Res
Clin Oncol. 95:291–293. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Erendeeva LE, Zav'yalova MB, Slonimskaya
EM and Perelmuter VM: Influence of functional asymmetry on the
forecast of a breast cancer. Byul Sib Med. 1:36–39. 2002.(In
Russian).
|
|
10
|
Hartveit F, Tangen M and Hartveit E: Side
and survival in breast cancer. Oncology. 41:149–154. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nouh MA, Ismail H, El-Din NH and
El-Bolkainy MN: Lymph node metastasis in breast carcinoma:
Clinicopathologic correlations in 3747 patients. J Egypt Natl Canc
Inst. 16:50–56. 2004.PubMed/NCBI
|
|
12
|
Mandard AM, Denoux Y, Herlin P, Duigou F,
van De Vijver MJ, Clahsen PC, van Den Broek L, Sahmoud TM,
Henry-Amar M and van De Velde CJ: Prognostic value of DNA cytometry
in 281 premenopausal patients with lymph node negative breast
carcinoma randomized in a control trial: Multivariate analysis with
Ki-67 index, mitotic count and microvessel density. Cancer.
89:1748–1757. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Trihia H, Murray S, Price K, Gelber RD,
Golouh R, Goldhirsch A, Coates AS, Collins J, Castiglione-Gertsch M
and Gusterson BA: International Breast Cancer Study Group: Ki-67
expression in breast carcinoma: Its association with grading
systems, clinical parameters, and other prognostic factors-a
surrogate marker? Cancer. 97:1321–1331. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ponzone R, Montemurro F, Maggiorotto F,
Robba C, Gregori D, Jacomuzzi ME, Kubatzki F, Marenco D, Dominguez
A, Biglia N and Sismondi P: Clinical outcome of adjuvant endocrine
treatment according to PR and HER-2 status in early breast cancer.
Ann Oncol. 17:1631–1636. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Viale G, Regan MM, Mastropasqua MG,
Maffini F, Maiorano E, Colleoni M, Price KN, Golouh R, Perin T,
Brown RW, et al: Predictive value of tumor Ki-67 expression in two
randomized trials of adjuvant chemoendocrine therapy for
node-negative breast cancer. J Natl Cancer Inst. 100:207–212. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Penault-Llorca F, Abrial C, Raoelfils I,
Cholletac P, Cayrea A, Mouret-Reynier M, Thivat E, Mishellany F,
Gimbergues P and Durando X: Changes and predictive and prognostic
value of the mitotic index, Ki-67, cyclin D1, and cyclo-oxygenase-2
in 710 operable breast cancer patients treated with neoadjuvant
chemotherapy. Oncologist. 13:1235–1245. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li L, Mu K, Zhou G, Lan L, Auer G and
Zetterberg A: Genomic instability and proliferative activity as
risk factors for distant metastases in breast cancer. Br J Cancer.
99:513–519. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Darb-Esfahani S, Loibl S, Müller BM,
Roller M, Denkert C, Komor M, Schlüns K, Blohmer JU, Budczies J,
Gerber B, et al: Identification of biology-based breast cancer
types with distinct predictive and prognostic features: Role of
steroid hormone and HER2 receptor expression in patients treated
with neoadjuvant anthracycline/taxane-based chemotherapy. Breast
Cancer Res. 11:R692009. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sharma S, Hiran KR, Pavithran K and
Vijaykumar DK: A pilot study to assess the feasibility of
evaluation of markers of response to chemotherapy at one day &
21 days after first cycle of chemotherapy in carcinoma of breast: A
prospective non-randomized observational study. World J Surg Oncol.
7:352009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dowsett M, A'Hern R, Salter J, Zabaglo L
and Smith IE: Who would have thought a single Ki67 measurement
would predict long-term outcome? Breast Cancer Res. 11(Suppl 3):
S152009. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rodger A: Who would have thought it!
Influence on outcome of radiotherapy, Ki67 and stroma. Introduction
to Session 5. Breast Cancer Res. 11(Suppl 3): S132009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yerushalmi R, Woods R, Ravdin PM, Hayes MM
and Gelmon KA: Ki67 in breast cancer: Prognostic and predictive
potential. Lancet Oncol. 11:174–183. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shokouh TZ, Ezatollah A and Barand P:
Interrelationships between Ki67, HER2/neu, p53, ER and PR status
and their associations with tumor grade and lymph node involvement
in breast carcinoma subtypes: Retrospective-observational
analytical study. Medicine (Baltimore). 94:e13592015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dabbs D: Diagnostic Immunohistochemistry
(2nd). Philadelphia: Elsevier. 699–746. 2006. View Article : Google Scholar
|
|
25
|
Jung P, Baumgärtner U, Stoeter P and
Treede R-D: Structural and Functional Asymmetry in the Human
Parietal Opercular Cortex. Journal of Neurophysiology.
101:3246–3257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cabeza R: Hemispheric asymmetry reduction
in older adults: the HAROLD model. Psychol Aging. 17:85–100. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dolcos F, Rice HJ and Cabeza R:
Hemispheric asymmetry and aging: right hemisphere decline or
asymmetry reduction. Neurosci Biobehav Rev. 26:819–825. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Poroshenko AB: About the nature of
deficiency of anticancer resistance of an organism. Sbornik
nauchnykh trudov RNIOI. Sposoby i mekhanizmy povysheniya
protivoopukholevoi zashchity v onkologii (Moskva). 211–257.
1993.(In Russian).
|