|
1
|
Ueno M, Oya M, Azekura K, Yamaguchi T and
Muto T: Incidence and prognostic significance of lateral lymph node
metastasis in patients with advanced low rectal cancer. Br J Surg.
92:756–763. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sugihara K, Kobayashi H, Kato T, Mori T,
Mochizuki H, Kameoka S, Shirouzu K and Muto T: Indication and
benefit of pelvic sidewall dissection for rectal cancer. Dis Colon
Rectum. 49:1663–1672. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ueno H, Mochizuki H, Hashiguchi Y,
Ishiguro M, Miyoshi M, Kajiwara Y, Sato T, Shimazaki H and Hase K:
Potential prognostic benefit of lateral pelvic node dissection for
rectal cancer located below the peritoneal reflection. Ann Surg.
245:80–87. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kobayashi H, Mochizuki H, Kato T, Mori T,
Kameoka S, Shirouzu K and Sugihara K: Outcomes of surgery alone for
lower rectal cancer with and without pelvic sidewall dissection.
Dis Colon Rectum. 52:567–576. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Akiyoshi T, Watanabe T, Miyata S, Kotake
K, Muto T and Sugihara K: Japanese Society for Cancer of the Colon
and Rectum: Results of a Japanese nationwide multi-institutional
study on lateral pelvic lymph node metastasis in low rectal cancer:
Is it regional or distant disease? Ann Surg. 255:1129–1134. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Watanabe T, Tsurita G, Muto T, Sawada T,
Sunouchi K, Higuchi Y, Komuro Y, Kanazawa T, Iijima T, Miyaki M and
Nagawa H: Extended lymphadenectomy and preoperative radiotherapy
for lower rectal cancers. Surgery. 132:27–33. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yano H, Saito Y, Takeshita E, Miyake O and
Ishizuka N: Prediction of lateral pelvic node involvement in low
rectal cancer by conventional computed tomography. Br J Surg.
94:1014–1019. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dharmarajan S, Shuai D, Fajardo AD,
Birnbaum EH, Hunt SR, Mutch MG, Fleshman JW and Lin AY: Clinically
enlarged lateral pelvic lymph nodes do not influence prognosis
after neoadjuvant therapy and TME in stage III rectal cancer. J
Gastrointest Surg. 15:1368–1374. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Akiyoshi T, Ueno M, Matsueda K, Konishi T,
Fujimoto Y, Nagayama S, Fukunaga Y, Unno T, Kano A, Kuroyanagi H,
et al: Selective lateral pelvic lymph node dissection in patients
with advanced low rectal cancer treated with preoperative
chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol.
21:189–196. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lim SB, Yu CS, Kim CW, Yoon YS, Park SH,
Kim TW, Kim JH and Kim JC: Clinical implication of additional
selective lateral lymph node excision in patients with locally
advanced rectal cancer who underwent preoperative
chemoradiotherapy. Int J Colorectal Dis. 28:1667–1674. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Japanese Society for Cancer of the Colon
and Rectum: Japanese classification of colorectal carcinoma. (2nd
English). (Tokyo). Kanehara & Co. Ltd. 7–10. 2009.
|
|
12
|
Yoshikawa R, Kusunoki M, Yanagi H, Noda M,
Furuyama JI, Yamamura T and Hashimoto-Tamaoki T: Dual antitumor
effects of 5-fluorouracil on the cell cycle in colorectal carcinoma
cells: A novel target mechanism concept for pharmacokinetic
modulating chemotherapy. Cancer Res. 61:1029–1037. 2001.PubMed/NCBI
|
|
13
|
Inoue Y, Okigami M, Kawamoto A, Okugawa Y,
Hiro J, Saigusa S, Toiyama Y, Tanaka K, Mohri Y and Kusunoki M:
Phase I study of 5-fluorouracil, leucovorin and bevacizumab in
combination with radiation therapy in patients with locally
advanced rectal cancer. Mol Clin Oncol. 1:511–516. 2013.PubMed/NCBI
|
|
14
|
Saigusa S, Tanaka K, Toiyama Y, Matsushita
K, Kawamura M, Okugawa Y, Hiro J, Inoue Y, Uchida K, Mohri Y and
Kusunoki M: Gene expression profiles of tumor regression grade in
locally advanced rectal cancer after neoadjuvant chemoradiotherapy.
Oncol Rep. 28:855–861. 2012.PubMed/NCBI
|
|
15
|
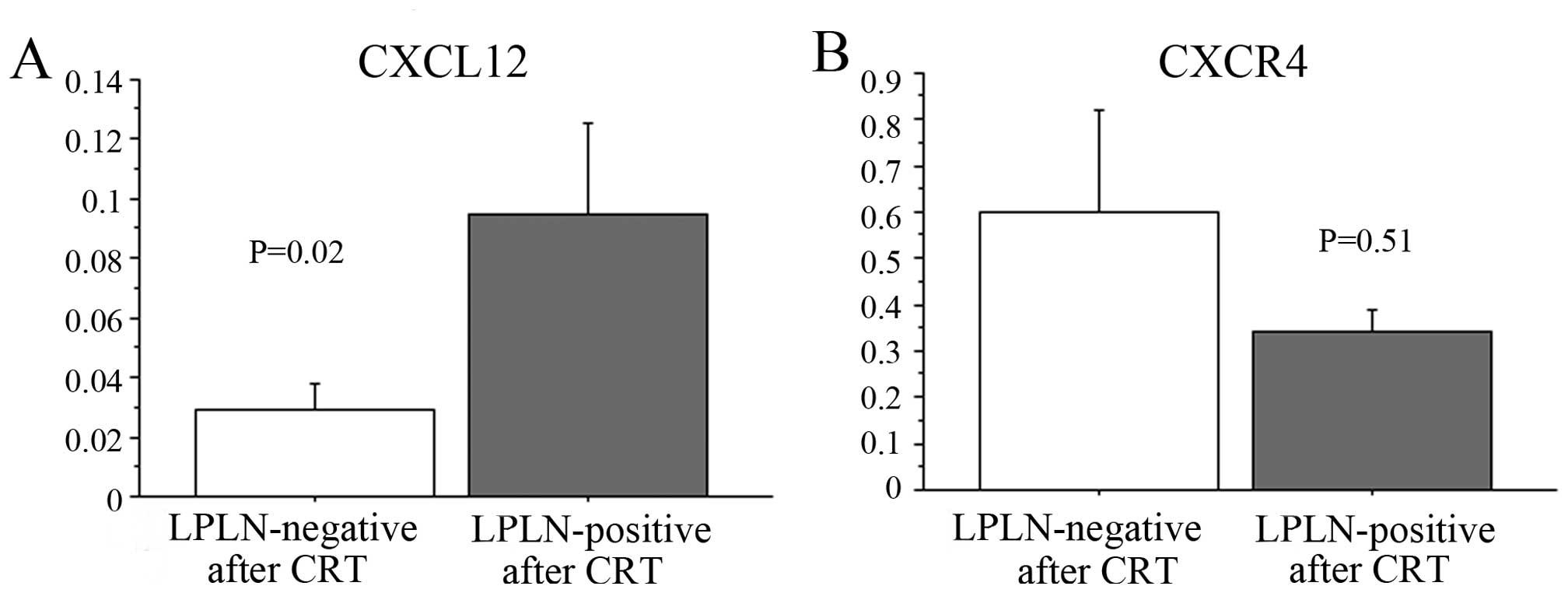
Saigusa S, Toiyama Y, Tanaka K, Yokoe T,
Okugawa Y, Kawamoto A, Yasuda H, Inoue Y, Miki C and Kusunoki M:
Stromal CXCR4 and CXCL12 expression is associated with distant
recurrence and poor prognosis in rectal cancer after
chemoradiotherapy. Ann Surg Oncol. 17:2051–2058. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moriya Y, Sugihara K, Akasu T and Fujita
S: Importance of extende lymphadenectomy with lateral node
dissection for advanced lower rectal cancer. World J Surg.
21:728–732. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sugihara K, Moriya Y, Akasu T and Fujita
S: Pelvic autonomic nerve preservation for patients with rectal
carcinoma. Oncologic and functional outcome. Cancer. 78:1871–1880.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Beyond TME Collaborative: Consensus
statement on the multidisciplinary management of patients with
recurrent and primary rectal cancer beyond total mesorectal
excision planes. Br J Surg. 100:1009–1014. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Benson AB III, Bekaii-Saab T, Chan E, Chen
YJ, Choti MA, Cooper HS, Engstrom PF, Enzinger PC, Fakih MG, Fuchs
CS, et al: Rectal cancer. J Natl Compr Canc Netw. 10:1528–1564.
2012.PubMed/NCBI
|
|
20
|
Quadros CA, Falcão MF, Carvalho ME and
Ladeia PA: Metastases to retroperitoneal or lateral pelvic lymph
nodes indicated unfavorable survival and high pelvic recurrence
rates in a cohort of 102 patients with low rectal adenocarcinoma. J
Surg Oncol. 106:653–658. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Salvucci O, Yao L, Villalba S, Sajewicz A,
Pittaluga S and Tosato G: Regulation of endothelial cell branching
morphogenesis by endogenous chemokine stromal-derived factor-1.
Blood. 99:2703–2711. 2001. View Article : Google Scholar
|
|
22
|
Müller A, Homey B, Soto H, Ge N, Catron D,
Buchanan ME, McClanahan T, Murphy E, Yuan W, Wagner SN, et al:
Involvement of chemokine receptors in breast cancer metastasis.
Nature. 410:50–56. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kim J, Takeuchi H, Lam ST, Turner RR, Wang
HJ, Kuo C, Foshag L, Bilchik AJ and Hoon DS: Chemokine receptor
CXCR4 expression in colorectal cancer patients increases the risk
for recurrence and for poor survival. J Clin Oncol. 23:2744–2753.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Matsusue R, Kubo H, Hisamori S, Okoshi K,
Takagi H, Hida K, Nakano K, Itami A, Kawada K, Nagayama S and Sakai
Y: Hepatic stellate cells promote liver metastasis of colon cancer
cells by the action of SDF-1/CXCR4 axis. Ann Surg Oncol.
16:2645–2653. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ottaiano A, Franco R, Aiello Talamanca A,
Liguori G, Tatangelo F, Delrio P, Nasti G, Barletta E, Facchini G,
Daniele B, et al: Overexpression of both CXC chemokine receptor 4
and vascular endothelial growth factor proteins predicts early
distant relapse in stage II-III colorectal cancer patients. Clin
Cancer Res. 12:2795–2803. 2006. View Article : Google Scholar : PubMed/NCBI
|