Introduction
Vaginal melanoma is a rare tumor that accounts for
<1% of all melanomas and ~5% of all vaginal malignant tumors
(1–4). The etiology of vaginal melanoma remains
unknown at present as, given its location, ultraviolet radiation is
unlikely to be involved in the tumorigenic process.
The prognosis of vaginal melanoma is extremely poor,
with a 5-year overall survival (OS) rate of only ~18%, which is
significantly lower compared with that of vulvar melanoma (47%) and
cutaneous melanoma (81%) (5). The
occult nature of the anatomical location contributes to the late
presentation and late diagnosis. In addition, the diffuse lymphatic
vascular plexus in the vagina promotes early metastasis of vaginal
melanoma.
There are currently no established guidelines for
the treatment of vaginal melanoma due to its rarity; therefore,
physicians may find deciding on the treatment method challenging.
Complete resection may be difficult due to its anatomical location,
and vaginal melanoma is often resistant to chemotherapy and
radiotherapy (6). We herein present
a retrospective clinical analysis of 5 cases of vaginal
melanoma.
Patients and methods
Patients
A total of 5 patients with vaginal melanoma, treated
at the Department of Gynecology of Osaka City University Hospital
(Osaka, Japan) between October, 2000 and April, 2014, were
investigated. This is a retrospective study of the patient
characteristics and treatment outcomes. Ethics approval and written
informed consent have been obtained. A staging system of vaginal
melanoma has not been fully established to date; thus, the
International Federation of Gynecology classification for vaginal
cancer (7) was used to determine
disease stage. In all 5 patients, the diagnosis of malignant
melanoma was histologically confirmed, and staging was based on
pelvic examination, computed tomography and magnetic resonance
imaging.
The patients' medical records were consulted for
information on patient characteristics, treatment, histological
findings, presence of recurrence, site of recurrence, treatment for
recurrence, OS and disease-free survival (DFS).
Results
Patient characteristics
The characteristics of the 5 cases are summarized in
Tables I and II. All the cases presented with abnormal
genital bleeding as the main complaint. Notably, in 3 of the 5
cases, the tumors appeared as non-pigmented polyps. In all 5 cases,
local resection was performed as primary treatment.
 | Table I.Summary of all cases (n=5) with
vaginal melanoma. |
Table I.
Summary of all cases (n=5) with
vaginal melanoma.
| Patient no. | Age, years | Main complaint | Stage | Initial
diagnosis | Surgery | Adjuvant therapy | Recurrence | Site of
recurrence | Outcome | DFS, days | OS, days |
|---|
| 1 | 62 | AGB | IIc | Vaginal polyp
(non-pigmented) | Local resection | DAVFeron | + | Uterine cervix,
pelvic LN | AWD | 392 | 772 |
| 2 | 78 | AGB | IIa | MM | Local resection | IFN-β | + | Liver | DOD | 102 | 427 |
| 3 | 78 | AGB | IIa | Vaginal polyp
(non-pigmented) | Local resection | IFN-β | + | Brain | DOD | 235 | 294 |
| 4 | 79 | AGB | IIc | MM | Local resection | − | + | Vagina | DOD | 115 | 177 |
| 5 | 82 | AGB | IIc | Vaginal polyp
(non-pigmented) | Local resection | IFN-β | + | Vagina, lung | DOD | 117 | 419 |
 | Table II.Patient characteristics (n=5). |
Table II.
Patient characteristics (n=5).
| Characteristics | No. (%) |
|---|
| Age, years [median
(range)] | 78 (62–82) |
| Main complaint |
|
| Abnormal
genital bleeding | 5 (100) |
| Initial
diagnosis |
|
| Malignant
melanoma | 2 (40) |
| Vaginal
polyp | 2 (40) |
| Vaginal
carcinoma | 1 (20) |
| Stage |
|
| IIa | 2 (40) |
| IIc | 3 (60) |
| Primary
treatment |
|
| Local
resection | 5 (100) |
| Adjuvant therapy |
|
| Local
injection of IFN-β | 3 (60) |
|
DAVFeron | 1 (20) |
| Not
performed | 1 (20) |
Treatment and recurrence
All 5 cases recurred within 1 year. The site of
recurrence varied and included the vaginal wall, liver, brain and
lung. Treatment for recurrence was as follows: An extended
hysterectomy was performed in case 1, which recurred in the uterine
cervix; X-Knife radiosurgery was used in case 3 for a brain
metastasis; local resection was performed in case 5 for a
recurrence in the vagina, and dacarbazine and nivolumab [an
anti-programmed cell death protein-1 (PD-1) antibody] were
administered to treat the second recurrence in the vagina and the
multiple lung metastases; in case 2, nivolumab was administered for
a liver metastasis; and in case 4, the patient declined additional
treatment for the recurrence.
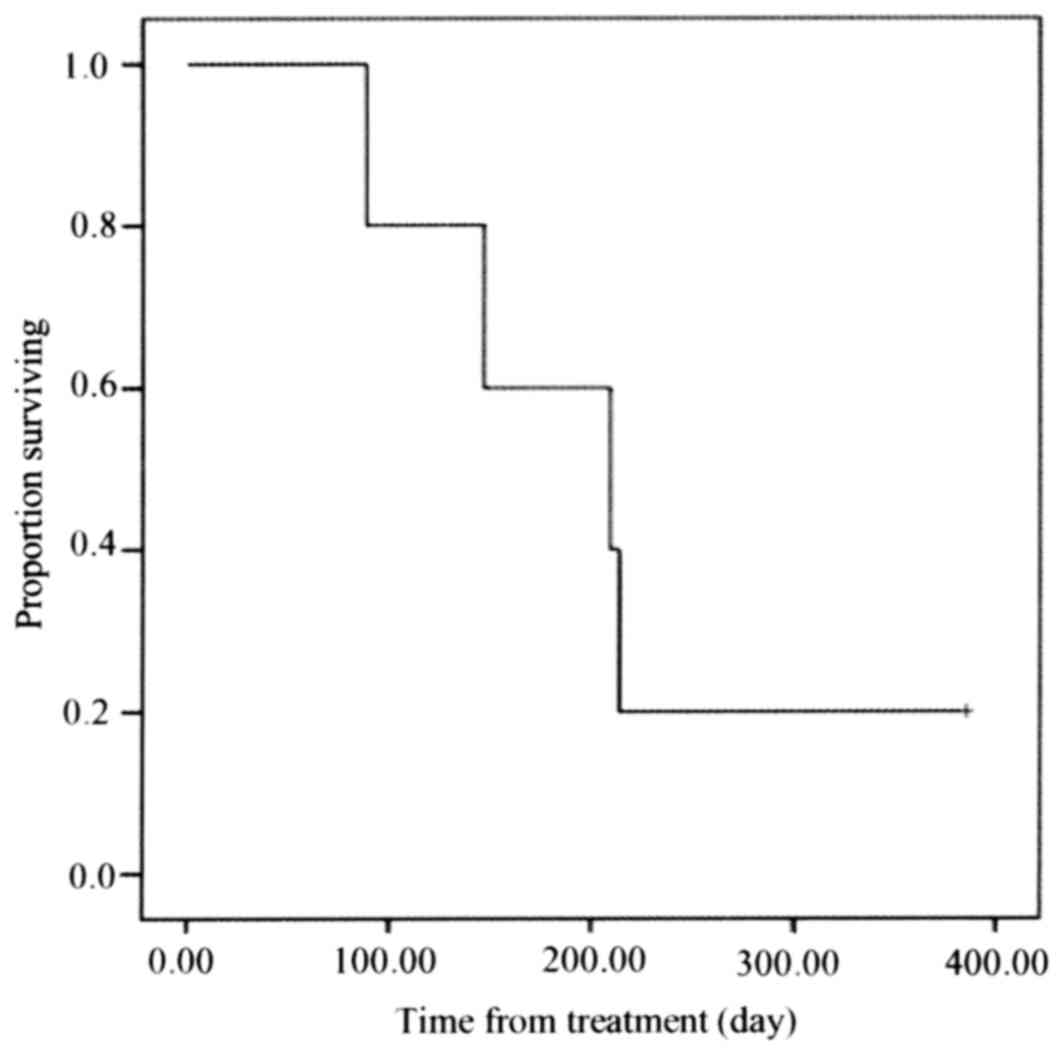
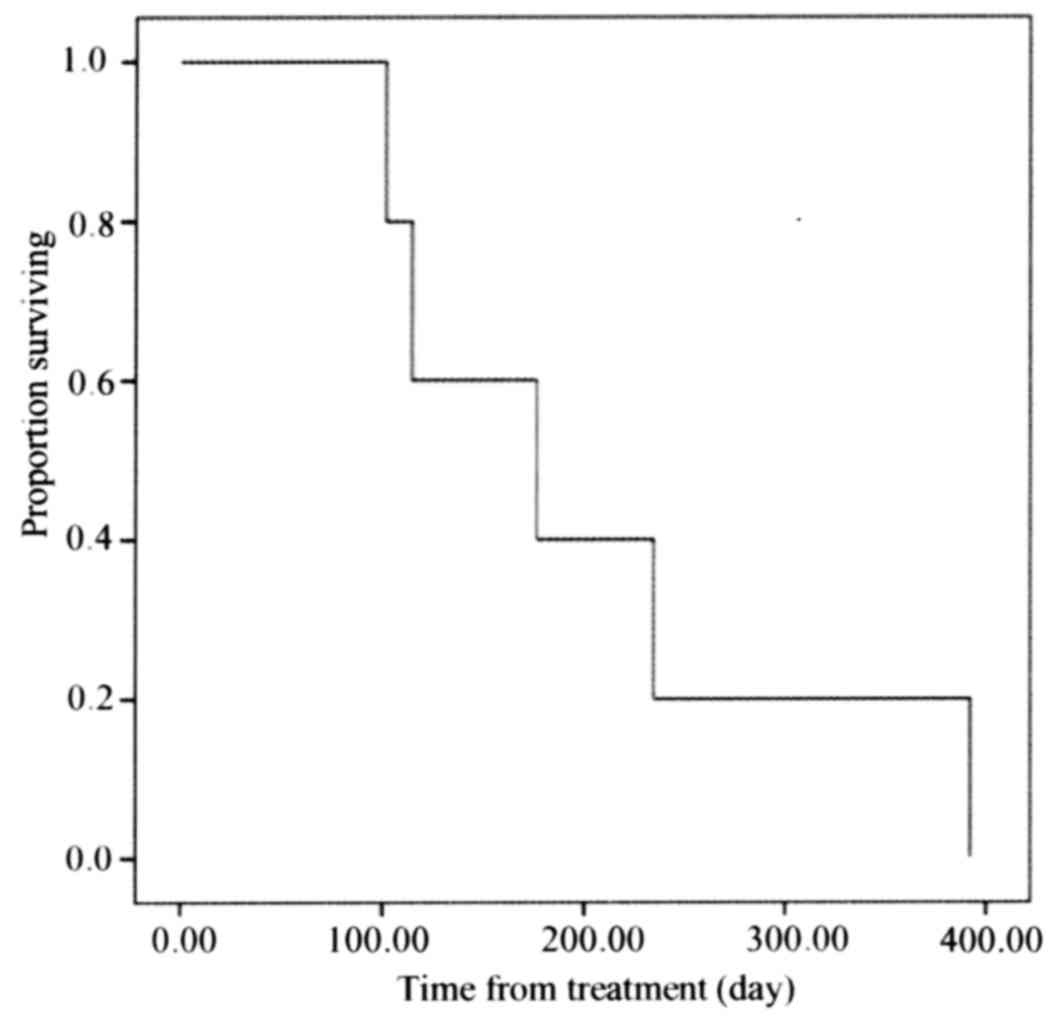
The survival curves for OS and DFS are illustrated
in Figs. 1 and 2, respectively. The median OS was 419 days
and the median DFS was 177 days.
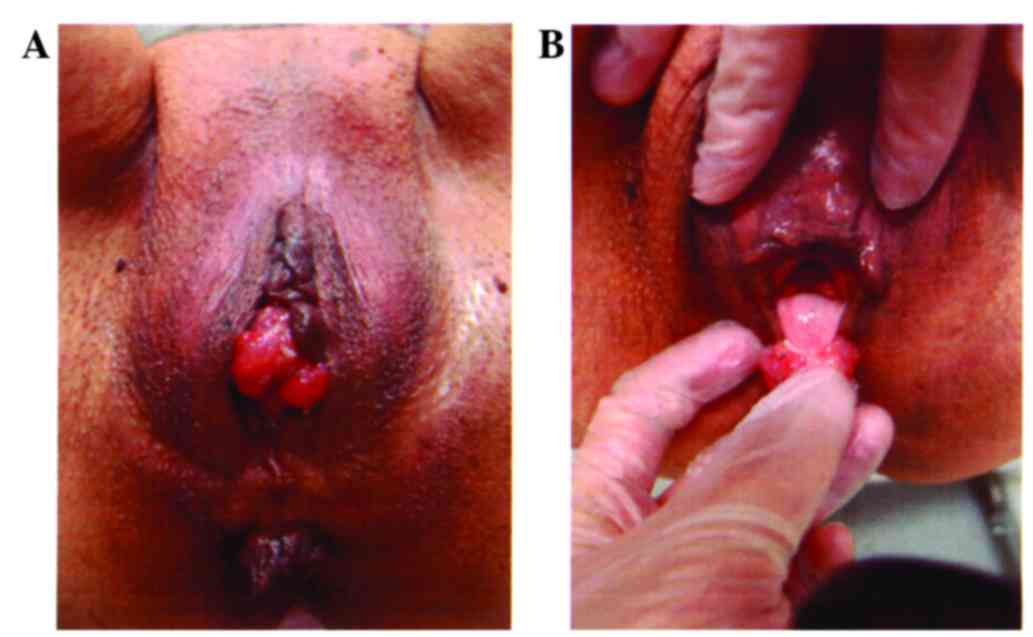
The non-pigmented lesion of case 5 is presented in
Fig. 3. At the first visit, the
possibility of melanoma was not taken into consideration, and a
biopsy of the tumor suggested the diagnosis of squamous cell
carcinoma. The histopathological examination following local
resection established the diagnosis of malignant melanoma.
Discussion
The prognosis of vaginal melanoma is worse compared
with that of cutaneous melanoma, vulvar melanoma, and other vaginal
malignancies (5,8–10). The
occult nature of its anatomical location may contribute to the late
presentation and late diagnosis of vaginal melanoma, and the
diffuse lymphatic vascular plexus in the vagina contributes to the
early metastasis of vaginal melanomas.
The prognostic factors of vaginal melanoma have not
been definitely determined. From the previous literature, tumor
size, depth of invasion, lymph node status, extent of surgery and
adjuvant therapy may affect the prognosis of vaginal melanoma
(1).
Primary treatment protocols for vaginal melanoma
remain to be established. Surgery, radiotherapy, chemotherapy and
immunotherapy are recommended as individual and combined therapies.
Surgery is the optimal treatment and is considered to be the only
potentially curative treatment for vaginal melanoma (1). Surgical procedures for the primary
disease range from conservative local excision to a more radical
approach, including vaginectomy and pelvic exenteration. Since an
association between the extent of surgery and survival has not been
proven for vaginal melanoma, there has been significant controversy
regarding the optimal surgical method. Therefore, local resection
was performed in all the cases presented herein.
There is currently no standard approach to adjuvant
therapy. The limited case series available suggest an improvement
in local control with the use of radiotherapy in the adjuvant
setting for vulvar and vaginal melanomas. Additionally, for
patients with limited treatment options, radiotherapy may also
provide some palliative benefit in terms of symptomatic control
(6). For advanced and recurrent
disease, palliative systemic therapy may be an option. The authors
of a retrospective case series of vulvar or vaginal lesions
reported that, with treatment with a variety of biochemotherapy
regimens (dacarbazine, cisplatin, interferon-α and interleukin-2),
a partial response was achieved in 36% of the patients (11).
Systemic therapy for advanced cutaneous melanoma has
changed significantly. There have been reports of significant OS
improvement in response to agents such as anticytotoxic
T-lymphocyte-associated antigen-4 antibodies (ipilimumab) (12,13),
antibodies against BRAF (vemurafenib and dabrafenib), MEK
inhibitors (trametinib) (14–16) and
an anti-PD-1 antibody (nivolumab) (17). Nivolumab may result in significant
improvements in OS and progression-free survival as compared with
dacarbazine for previously untreated patients with metastatic
melanoma without a BRAF mutation (17); thus, it may be helpful in the
treatment of vaginal melanoma.
In the present study, all 5 cases presented with
abnormal genital bleeding as the main complaint. Therefore,
malignant melanoma of the vagina must be considered along with
other gynecological malignancies in patients presenting with
abnormal genital bleeding. In this study, 3 of the 5 cases had a
non-pigmented polypoid lesion of the vagina. Therefore, the
possibility of malignant melanoma of the vagina must be taken into
consideration in patients with a polypoid lesion on the vaginal
wall.
References
|
1
|
Xia L, Han D, Yang W, Li J, Chuang L and
Wu X: Primary malignant melanoma of the vagina: A retrospective
clinicopathologic study of 44 cases. Int J Gynecol Cancer.
24:149–155. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bishop KD and Olszewski AJ: Epidemiology
and survival outcomes of ocular and mucosal melanomas: A
population-based analysis. Int J Cancer. 134:2961–2971. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Frumovitz M, Etchepareborda M, Sun CC,
Soliman PT, Eifel PJ, Levenback CF and Ramirez PT: Primary
malignant melanoma of the vagina. Obstet Gynecol. 116:1358–1365.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Das P, Kumar N, Ahuja A, Jain A, Ray R,
Sarkar C and Gupta SD: Primary malignant melanoma at unusual sites:
An institutional experience with review of literature. Melanoma
Res. 20:233–239. 2010.PubMed/NCBI
|
|
5
|
Ragnarsson-Olding B, Johansson H, Rutqvist
LE and Ringborg U: Malignant melanoma of the vulva and vagina:
Trends in incidence, age distribution, and long-term survival among
245 consecutive cases in Sweden 1960–1984. Cancer. 71:1893–1897.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nobbenhuis MA, Lalondrelle S, Larkin J and
Banerjee S: Management of melanomas of the gynaecological tract.
Curr Opin Oncol. 26:508–513. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
FIGO Committee on Gynecologic Oncology, .
Current FIGO staging for cancer of the vagina, fallopian tube,
ovary, and gestational trophoblastic neoplasia. Int J Gynaecol
Obstet. 105:3–4. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Creasman WT, Phillips JL and Menck HR: The
National Cancer Data Base report on cancer of the vagina. Cancer.
83:1033–1040. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Piura B: Management of primary melanoma of
the female urogenital tract. Lancet Oncol. 9:973–981. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Weinstock MA: Malignant melanoma of the
vulva and vagina in the United States: Patterns of incidence and
population-based estimates of survival. Am J Obstet Gynecol.
171:1225–1230. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Harting MS and Kim KB: Biochemotherapy in
patients with advanced vulvovaginal mucosal melanoma. Melanoma Res.
14:517–520. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hodi FS, O'Day SJ, McDermott DF, Weber RW,
Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel
JC, et al: Improved survival with ipilimumab in patients with
metastatic melanoma. N Engl J Med. 363:711–723. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Robert C, Thomas L, Bondarenko I, O'Day S,
Weber J, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, et al:
Ipilimumab plus dacarbazine for previously untreated metastatic
melanoma. N Engl J Med. 364:2517–2526. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hauschild A, Grob JJ, Demidov LV, Jouary
T, Gutzmer R, Millward M, Rutkowski P, Blank CU, Miller WH Jr,
Kaempgen E, et al: Dabrafenib in BRAF-mutated metastatic melanoma:
A multicentre, open-label, phase 3 randomised controlled trial.
Lancet. 380:358–365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chapman PB, Hauschild A, Robert C, Haanen
JB, Ascierto P, Larkin J, Dummer R, Garbe C, Testori A, Maio M, et
al: Improved survival with vemurafenib in melanoma with BRAF V600E
mutation. N Engl J Med. 364:2507–2516. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Flaherty KT, Infante JR, Daud A, Gonzalez
R, Kefford RF, Sosman J, Hamid O, Schuchter L, Cebon J, Ibrahim N,
et al: Combined BRAF and MEK inhibition in melanoma with BRAF V600
mutations. N Engl J Med. 367:1694–1703. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Robert C, Long GV, Brady B, Dutriaux C,
Maio M, Mortier L, Hassel JC, Rutkowski P, McNeil C,
Kalinka-Warzocha E, et al: Nivolumab in previously untreated
melanoma without BRAF mutation. N Engl J Med. 372:320–330. 2015.
View Article : Google Scholar : PubMed/NCBI
|