Introduction
Desmoid tumor (DT), a locally invasive form of
fibromatosis, comprises only 0.03% of all tumors (1). DT may develop in the extremities, chest
wall, abdominal wall and intra-abdominally (2). DTs are benign tumors exhibiting
infiltrative growth and a tendency for recurrence (1,3).
Intra-abdominal DTs are rare and seldom reported in the literature.
There is a frequent association of DTs with familiar adenomatous
polyposis (FAP) and Gardner's syndrome (1). In patients with FAP and Gardner's
syndrome, the tumors are more likely to be intra-abdominal or
located in the anterior abdominal wall (4). By contrast, sporadic DTs are more
likely to be extra-abdominal (4),
with only 5% of sporadic DTs located intra-abdominally (5). Other possible triggers for the
development of intra-abdominal DTs mentioned in the literature
include female gender, childbirth, prior trauma or surgery and
estrogen exposure (1,6,7).
Case report
A 28-year-old woman, without any previous systemic
disease, was referred to the Department of Diagnostic and
Intervention Radiology, University Hospital Merkur (Zagreb,
Croatia) in November, 2016, for abdominal computed tomography (CT)
due to occasional abdominal pain of varying intensity for 6 months.
There were no other reported symptoms. The patient had no past
history of colonic polyps, abdominal trauma or surgical therapy.
The family history was negative for FAP. The general physical
examination was unremarkable. The analysed blood parameters were
within the normal ranges and the tumor markers were negative.
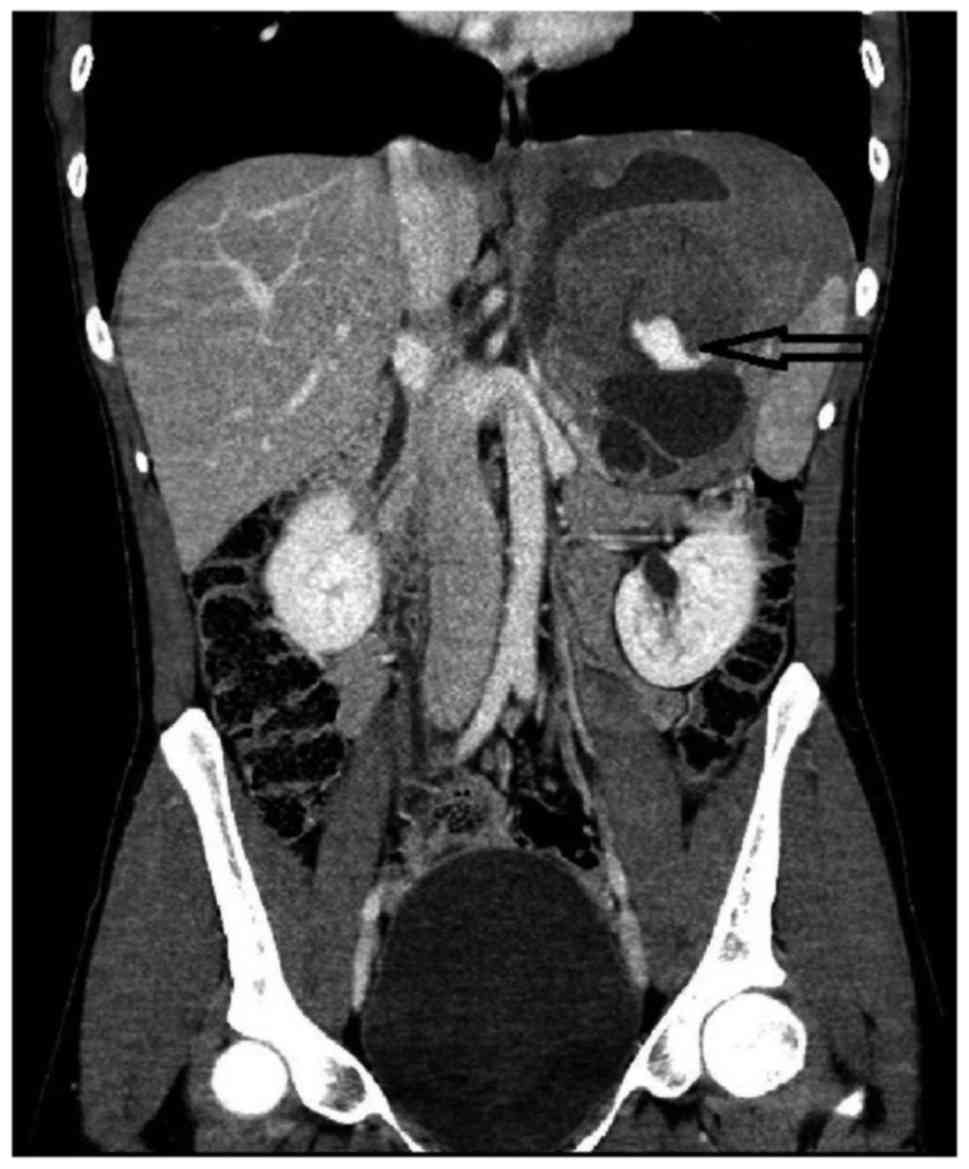
Ultrasound (US) examination revealed a large
solid-cystic heterogeneous hypoechoic mass in the upper left
abdomen. A contrast-enhanced CT of the abdomen revealed a large
heterogeneous solid-cystic intraperitoneal mass (18×14×11 cm)
occupying most of the left upper abdomen, extending from the left
hemidiaphragm to the upper pole of the left kidney, with partially
well-defined margins. The left adrenal gland and left kidney were
displaced downward. The mass was inseparable from the adjacent
greater curvature of the stomach, left hemidiaphragm, transverse
colon, pancreatic tail and spleen. Hyperdense areas of fresh
hemorrhage were observed within the tumor tissue (Figs. 1–3).
Hypointense infarcted areas were also identified in the spleen.
A subsequent laparotomy revealed a giant tumor
located in the left upper abdomen fixed to the greater curvature of
the stomach, pancreas, transverse colon, left adrenal gland, left
part of the diaphragm and spleen. An en bloc resection of the tumor
with the adherent spleen and left adrenal gland, with partial
resection of the stomach, pancreas, left hemidiaphragm and
transverse colon was performed. The patient tolerated the procedure
well and was discharged on the 7th postoperative day.
Histopathological examination of the mass confirmed
the diagnosis of solid-cystic DT, with negative surgical margins
and hemorrhagic areas. Immunohistochemical analysis revealed that
the tumor cells were positive for β-catenin. Follow-up details are
not yet available.
Discussion
DT is a rare benign tumor with a high propensity for
infiltrative growth and local invasion, which tends to recur
following local excision, but does not metastasize (1–6). Women
are more commonly affected compared with men, with a female:male
ratio of 3:1 (8). Two-thirds of the
patients are aged 20–40 years (8).
Associated conditions include FAP, Gardner's syndrome, trauma,
hormonal imbalance and prior surgery (8). DTs are usually solitary, but in 10–15%
of the cases they are multiple (8).
Intra-abdominal DTs are able to grow to a large size prior to
becoming symptomatic (9).
Imaging studies, such as CT and magnetic resonance
imaging (MRI), are used for preoperative diagnosis and for the
planning of the surgery. Following surgery, CT and MRI are used for
detecting recurrence and to monitor tumor response to radiotherapy
or medical therapy for unresectable or recurrent tumors (4,9). The CT
and MRI characteristics of intra-abdominal DTs are associated with
their histological characteristics and vascularity (9). The typical appearance of an
intra-abdominal DT on CT is that of a well-circumscribed solid soft
tissue mass, without calcifications (9). Although intra-abdominal DTs may appear
to be mostly well-circumscribed on CT and MRI, they are often
infiltrative (10). The US
characteristics of intra-abdominal DTs are often non-specific
(10).
Complete surgical resection with negative
pathological margins is the first line of management (10), and careful follow-up is recommended
due to the high rate of recurrence (11). Colonoscopy and examination of the eye
to exclude Gardner's syndrome are also recommended (11).
In conclusion, we herein presented a case of
intra-abdominal DT in a female patient who was negative for the
most well-known predisposing factors. The aim of this study was to
highlight the importance of including DT in the differential
diagnosis of a huge intra-abdominal mass.
References
|
1
|
Palladino E, Nsenda J, Siboni R and
Lechner C: A giant mesenteric desmoid tumor revealed by acute
pulmonary embolism due to compression of the inferior vena cava. Am
J Case Rep. 15:374–377. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kasper B, Ströbel P and Hohenberger P:
Desmoid tumors: Clinical features and treatment options for
advanced disease. Oncologist. 16:682–693. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kreuzberg B, Koudelova J, Ferda J, Treska
V, Spidlen V and Mukensnabl P: Diagnostic problems of abdominal
desmoid tumors in various locations. Eur J Radiol. 62:180–185.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sakorafas GH, Nissotakis C and Peros G:
Abdominal desmoid tumors. Surg Oncol. 16:131–142. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Efthimiopoulos GA, Chatzifotiou D,
Drogouti M and Zafiriou G: Primary asymptomatic desmoid tumor of
the mesentery. Am J Case Rep. 16:160–163. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mangat C, Inoue S, Kader M, Debelenko L
and Onwuzurike N: Sudden progressive abdominal pain due to large
peritoneal desmoid tumor: A case report with review of literature.
J Ped Surg Case Reports. 1:241–243. 2013. View Article : Google Scholar
|
|
7
|
Koshariya M, Shukla S, Khan Z, Vikas V,
Singh A Pratap, Baghel P, Pendro V, Jain V Kirti, Jai S Jagdish,
Kumar S and Songra MC: Giant desmoid tumor of the anterior
abdominal wall in a young female: A case report. Case Rep Surg.
2013:7808622013.PubMed/NCBI
|
|
8
|
Mirza RA, Ghesani MV and Enker WE:
Radiological case: Intra-abdominal desmoid tumor. Appl Radiol.
43:20–21. 2014.
|
|
9
|
Chen CB, Chiou YY, Chen CH, Chou YH,
Chiang JH and Chang CY: Sonographic and computed tomography
findings of intra-abdominal desmoid tumor. J Chin Med Assoc.
73:393–395. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gari MK, Guraya SY, Hussein AM and Hego
MM: Giant mesenteric fibromatosis: Report of a case and review of
the literature. World J Gastrointest Surg. 4:79–82. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shah M and Azam B: Case report of an
intra-abdominal desmoid tumour presenting with bowel perforation.
Mcgill J Med. 10:90–92. 2007.PubMed/NCBI
|