Introduction
Radiotherapy plays an important role in the
treatment of several patients with pelvic malignancies, such as
anorectal, urological and gynecological cancers (1). Approximately 70% of cancer patients
undergo radiotherapy for these malignancies to prolong disease-free
survival and reduce local recurrence (2,3).
However, radiotherapy may also lead to significant injury of the
normal tissues in the radiation field. The gastrointestinal tract
is a radiosensitive organ in the pelvis and often proves to be the
major limiting factor when determining tolerance to radiation
therapy (4).
One of the long-term complications of radiotherapy
for pelvic malignancies is the development of large bowel cancer
(3,5). Although the exact incidence of this
complication and the mechanisms of tumorigenesis have not been
fully elucidated, a close association between radiation and the
development of colorectal cancer (CRC) has been demonstrated
(6,7). Post-irradiation cancer is currently
termed radiation-associated cancer, as other predisposing factors,
such as lymphedema, adjuvant chemotherapy and genetic abnormalities
may be involved (8).
As most radiation treatments are directed to the
pelvis, the rectum is at particular risk of injury. The sigmoid
colon is also a common site of involvement due to its fixed
position at the pelvic brim, and is likely to receive a higher dose
of radiation (9). The occurrence of
colon and anorectal cancer following pelvic irradiation has been
reported, and the majority of the cases were encountered among
women who had undergone previous radiation therapy for
gynecological cancers, such as uterine cervical cancer (5,6,8,10).
Although preoperative chemoradiotherapy (CRT) is currently the
standard therapy for locally advanced rectal cancer (11), little attention has been paid to the
occurrence of colon cancer following CRT for rectal cancer. We
herein describe a case of suspected radiation-associated sigmoid
colon cancer following radiotherapy for locally advanced rectal
cancer.
Case report
A 48-year-old man presented at the University of
Tokyo Hospital with severe anal pain and frequent defecation. The
patient had undergone low anterior resection for rectal cancer
following preoperative radiotherapy at a total dose of 50 Gy at the
age of 29 years. Six years after surgery, contrast-enhanced
computed tomography (CT) revealed a fistula between the sigmoid
colon and presacral tissue, which subsequently recovered following
conservative management. The patient had been followed up regularly
without evidence of recurrence for 7 years, after which time he was
lost to follow-up. On admission, the results of the general
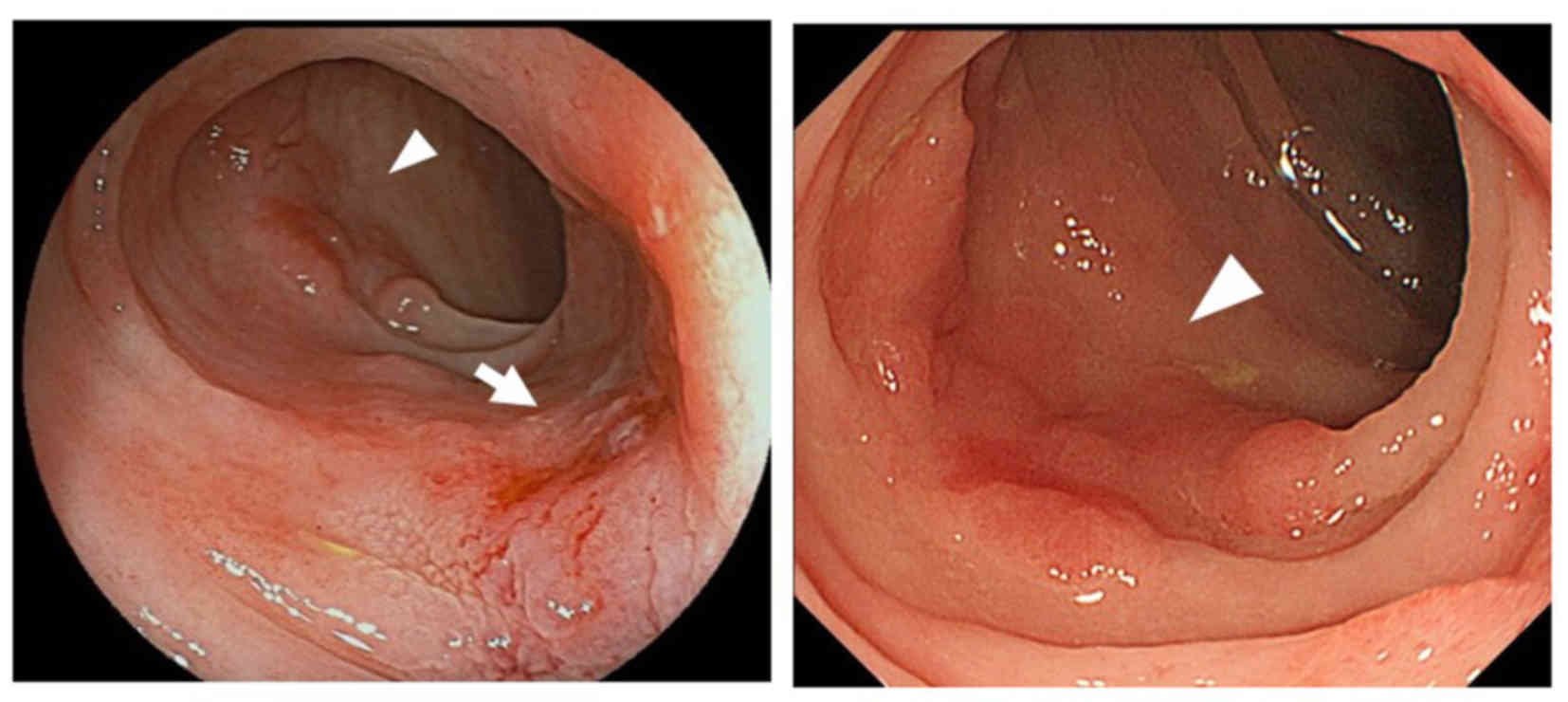
physical examination were normal. On colonoscopic examination, two
flat tumors of the sigmoid colon were identified at a distance of
14 cm from the anal margin, whereas the anastomosis site was
located at a distance of 4 cm from the anal margin (Fig. 1). Biopsies from both lesions revealed
well-differentiated adenocarcinomas. In addition, colonoscopy
identified five flat polyps near the tumor site; these flat polyps
were resected endoscopically and were diagnosed as tubular
adenomas. Colonoscopic findings of radiation proctocolitis were not
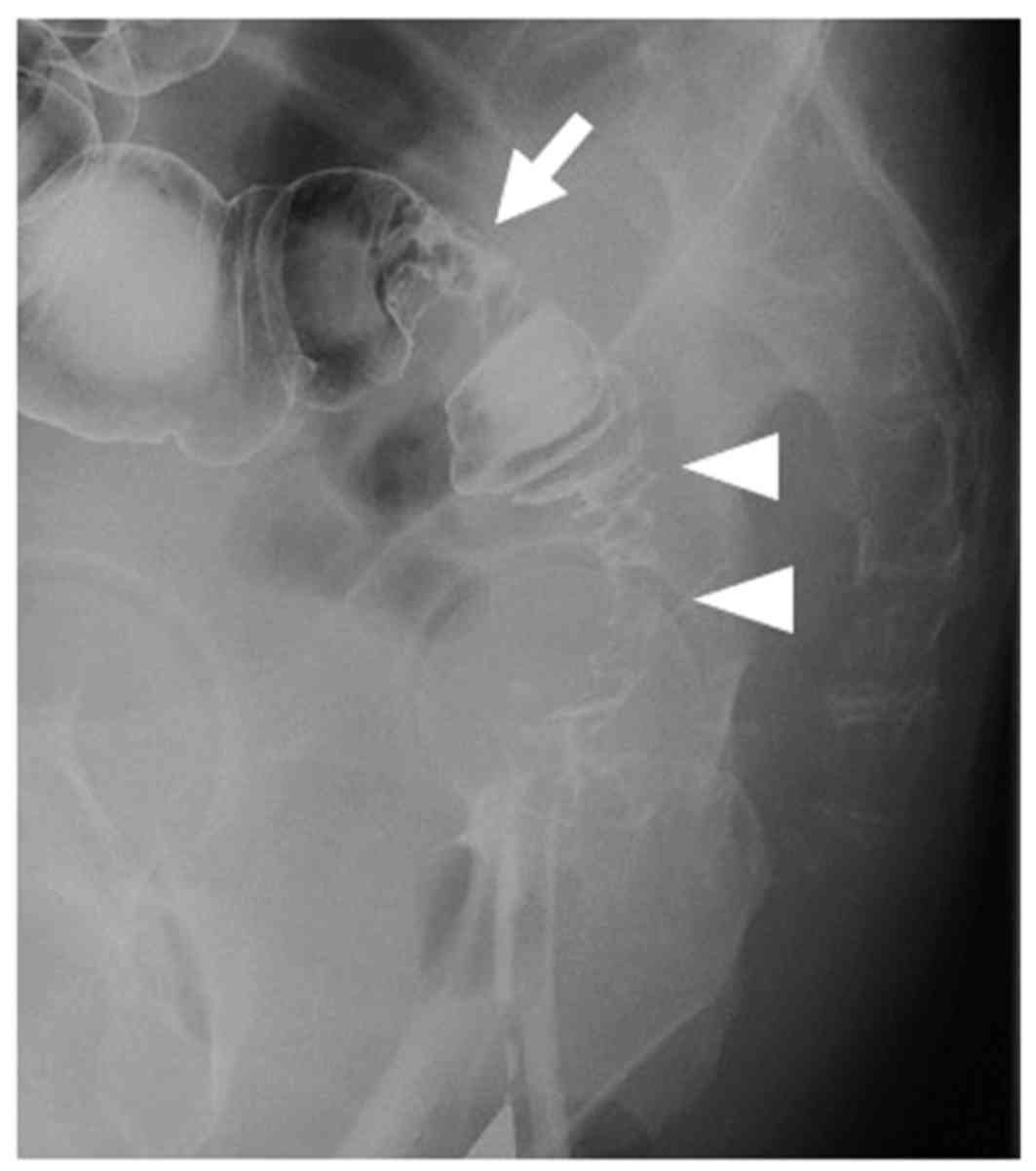
observed. A water-soluble contrast enema revealed an irregular
stricture of the sigmoid colon extending from the tumor to the
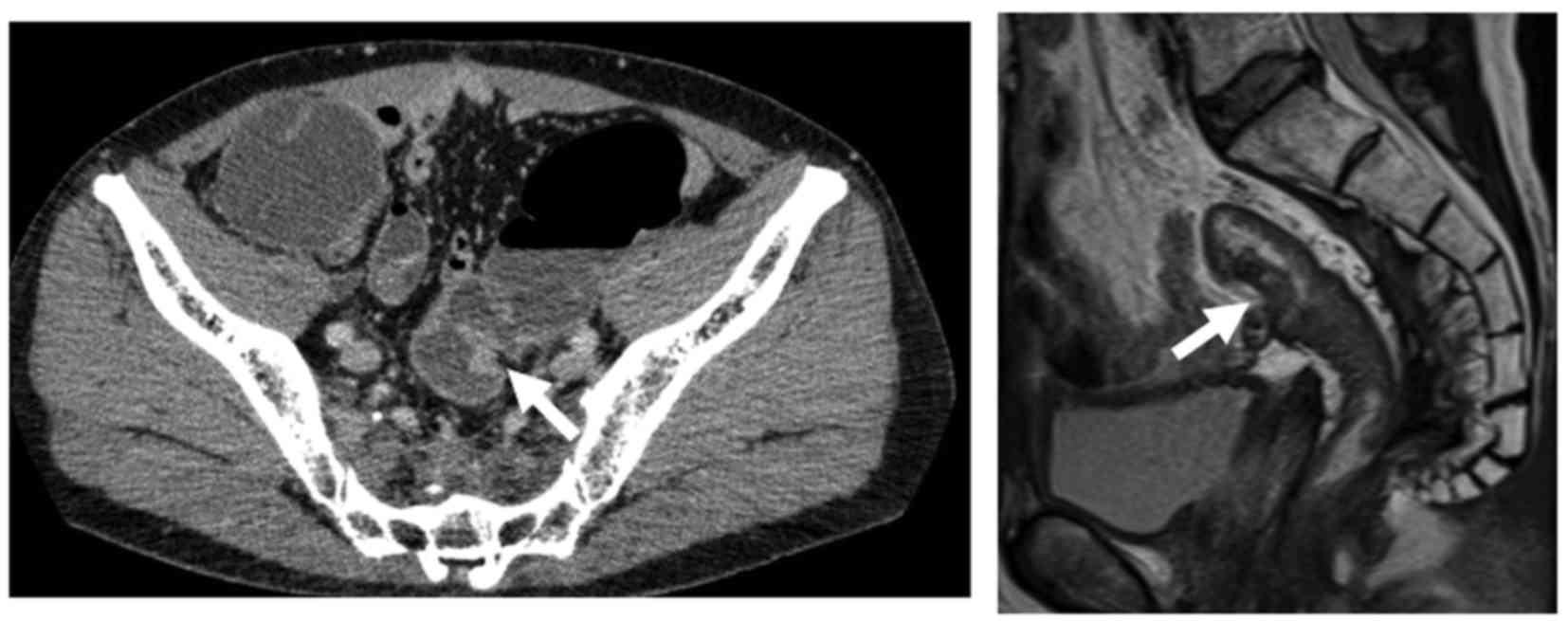
anastomosis (Fig. 2). CT and
magnetic resonance imaging revealed a mass in the sigmoid colon
with no evidence of distant metastasis (Fig. 3). Laparoscopic-assisted
intersphincteric resection of the rectum and the sigmoid colon with
diverting ileostomy was performed. There were no specific
complications postoperatively and the patient was discharged from
the hospital on the 20th postoperative day.
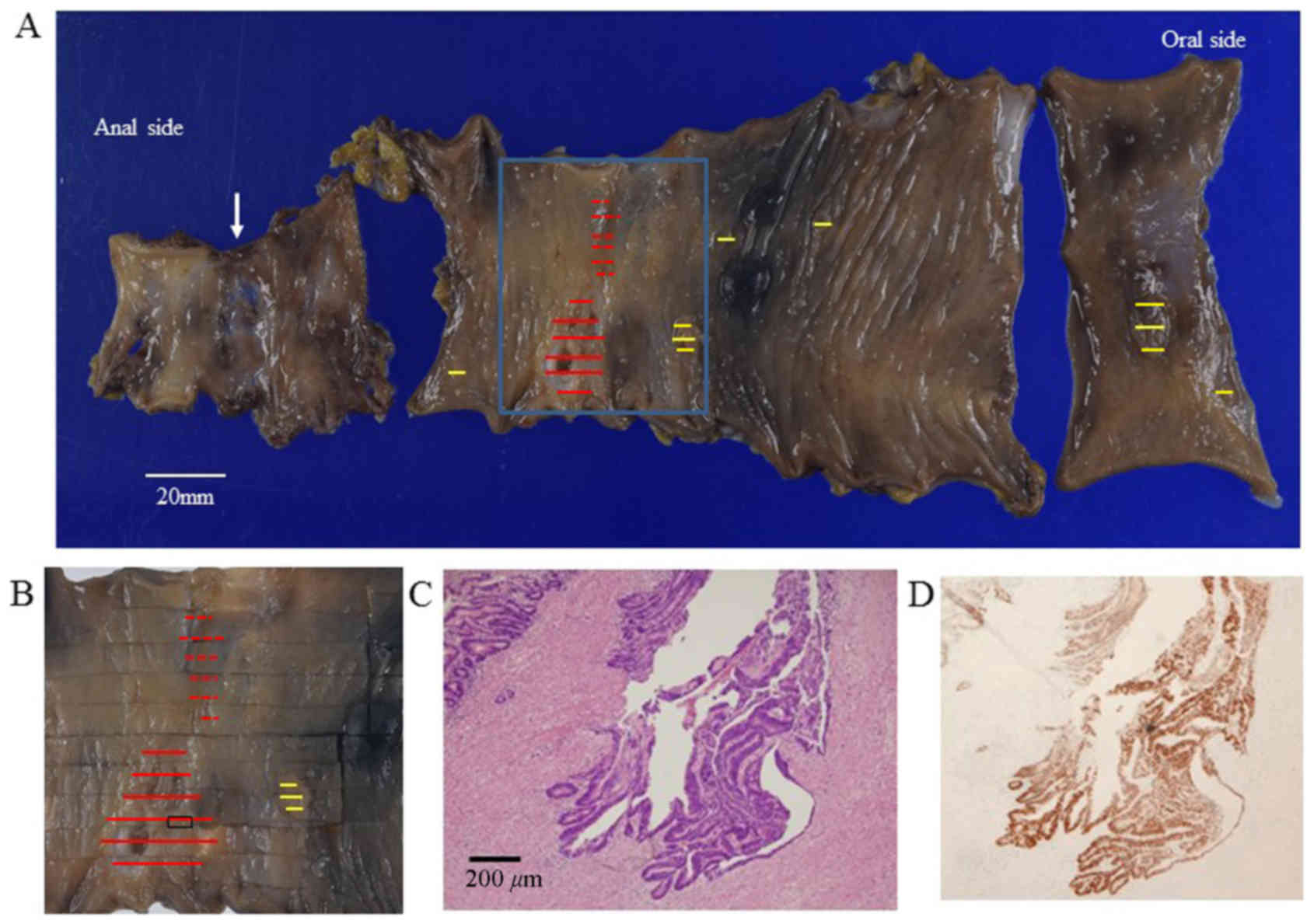
On pathological examination, the resected rectum and
sigmoid colon contained two separate tumors and six flat polyps
(Fig. 4A and B). The first tumor was
located at 8 cm from the distal margin and measured 3.5×1.5 cm; the
tumor was pathologically diagnosed as well-differentiated
adenocarcinoma with invasion of the subserosa (Fig. 4C). Another tumor was located near the
first and measured 2.5×2.2 cm; this tumor was pathologically
diagnosed as well-differentiated adenocarcinoma with invasion of
the submucosa. In addition, 17 regional lymph nodes without
metastasis were resected. Microsatellite instability (MSI) was not
observed on genetic analysis; however, p53 overexpression was
detected using immunohistochemical examination of the first tumor
(Fig. 4D). All six flat polyps were
diagnosed as tubular adenomas. Pathological findings of radiation
proctocolitis, such as submucosal fibrosis and hyalinization of the
blood vessels, were not observed in the sigmoid colon surrounding
the tumor.
Discussion
The clinicopathological characteristics of
radiation-associated CRC are as follows: i) Prior history of
radiation therapy and development of a malignancy in the radiation
field; ii) clinically chronic radiation proctocolitis at the site
of the subsequent tumor; iii) a long interval of ≥10 years between
irradiation and the appearance of the malignancy; iv)
histopathological evidence of intestinal radiation damage; and v)
mucinous carcinoma as the most common type (5). In the present case, all these
characteristics, apart from histological findings of intestinal
radiation damage and mucinous histology, were observed. Castro
et al (5) reported that, in
12 of 26 tumors, there was no mucin production and, among the 26
cases, 4 exhibited no histological evidence of radiation
damage.
Radiation proctocolitis has been reported in 5–11%
of patients treated for gynecological cancers (12,13).
Colonic strictures, erosions and fistulae are common sequelae of
radiation therapy of the gastrointestinal tract, and may result in
refractory pain, tenesmus and changes in bowel habits (4). From these findings, such as the fistula
of the sigmoid colon 6 years after surgery, colonic stricture and
erosions, as well as the clinical symptoms, such as anal pain and
frequent defecation, the suspicion of chronic radiation
proctocolitis was raised in the present case.
Considering the macroscopic type, as compared to
typical CRCs, radiation-associated CRCs often have a non-polypoid,
diffusely infiltrating appearance rather than a polypoid or
localized ulcerative appearance with a well-defined tumor margin
(8). In the present case, the two
flat sigmoid tumors had a diffusely infiltrating appearance,
without a well-defined tumor margin. Levitt et al (7) found synchronous multiple rectal cancers
within the radiation fields in 2 of 5 patients with rectal cancer
following pelvic irradiation, and hypothesized that radiation
exerted a ‘field effect’ for carcinogenesis on the rectal mucosa.
In the present case, the two flat tumors and 6 flat polyps were all
observed in the resected specimens and, thus, the radiation field
effect may be involved in our case. Therefore, based on the
macroscopic findings and clinical characteristics of chronic
radiation colitis, the two flat tumors in the present case were
considered to be radiation-associated sigmoid colon cancer.
The histopathological characteristics of late
radiation injury of the colorectum are characterized by severe
vascular changes, such as subintimal fibrosis and hyaline
sclerosis. The majority of the cases reported these findings in
women with cervical cancer who received high-dose irradiation, with
a dose ranging from 50 to 82 Gy (8,10,13).
None of these vascular changes were observed in the present case;
thus, we consider our case to have received lower-dose irradiation
compared with previously reported cases. The dose applied in our
case was 50 Gy and was focused on the rectal cancer, which had
already been resected. Of note, Palmer et al reported that
patients who received low-dose irradiation for benign gynecological
conditions had a higher rate (3.32%) of rectal cancer compared with
those who had received high-dose irradiation (1.4%) for cervical
cancer; they suggested that the relatively low irradiation dose
exerted a growth-stimulating effect that the high dose did not.
However, similar to the present case, the minority
of early-onset cases may be attributed to common hereditary CRC
syndromes (14). At present, two
independent genetic pathways are known to be involved in colorectal
carcinogenesis: One is the mutator phenotype pathway, which
involves dysfunction of DNA mismatch repair machinery; tumors in
this pathway frequently exhibit MSI (15). The other pathway is multistep
carcinogenesis, in which accumulation of mutations in the
adenomatous polyposis coli, KRAS, p53 and DPC
genes contributes to tumorigenesis (16). In the present case, there was no
detected hereditary tendency for malignancy, and there was no MSI,
although the first flat tumor harbored a p53 mutation.
Similar to the present case, Minami et al (17) reported that p53 protein
overexpression was detected using immunohistochemistry in 7 of 9
patients with radiation-associated colon cancer; however, they
found no definite correlation between the overexpression of p53 in
radiation-associated and spontaneous colon cancers. This suggested
that the occurrence of p53 gene mutations was not specific
to the carcinogenesis of radiation-associated colon cancers
compared with spontaneous colon cancers.
In the present case, the interval from radiation
treatment to diagnosis of sigmoid colon cancer was 19 years. In the
largest published series, the peak incidence of post-irradiation
CRC was between 5 and 10 years after the completion of
radiotherapy, while 1 carcinoma was diagnosed 45 years after
irradiation (5). However, the effect
of the radiation dose on the interval period has not been
investigated. It is therefore possible that higher doses of
irradiation may be associated with an earlier incidence of CRC
(7). From these findings, the
increased risk of CRC may start at 5 years and persist for >40
years after irradiation.
Clinically, the presenting symptoms of abnormal
bowel movement, diarrhea and dyschezia are similar between
radiation proctocolitis and radiation-associated colon cancer.
Additionally, it is difficult to detect curable CRC using
laboratory parameters. These factors may account for the delayed
diagnosis and advanced stage of colon cancer at the time of
detection (18,19). In the present case, colonoscopy was
performed to diagnose the cause of the anal pain, and sigmoid colon
cancer was detected incidentally. Therefore, there is a need for
earlier detection of CRC that develops in the setting of
proctocolitis following irradiation. Patients with radiation
colitis involving frequent diarrhea, dyschezia and tenesmus,
similar to the present case, require long-term surveillance to
prevent the growth of radiation-associated cancer.
We herein present a case of a radiation-associated
colon cancer in a patient who had undergone low anterior resection
for rectal cancer following preoperative radiotherapy 19 years
prior. The increased risk of CRC may start at 5 years and persist
for >40 years after irradiation. For cases of chronic
proctocolitis, such as colonic stricture, fistulae and abnormal
bowel movement, long-term surveillance with a colonoscope should be
considered after irradiation in patients undergoing previous pelvic
radiotherapy.
References
|
1
|
Wang J, Boerma M, Fu Q and Hauer-Jensen M:
Significance of endothelial dysfunction in the pathogenesis of
early and delayed radiation enteropathy. World J Gastroenterol.
13:3047–3055. 2007.PubMed/NCBI
|
|
2
|
Andreyev HJ: Gastrointestinal problems
after pelvic radiotherapy: The past, the present and the future.
Clin Oncol (R Coll Radiol). 19:790–799. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Birgisson H, Påhlman L, Gunnarsson U and
Glimelius B: Occurrence of second cancers in patients treated with
radiotherapy for rectal cancer. J Clin Oncol. 23:6126–6131. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ashburn JH and Kalady MF:
Radiation-induced problems in colorectal surgery. Clin Colon Rectal
Surg. 29:85–91. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Castro EB, Rosen PP and Quan SH: Carcinoma
of large intestine in patients irradiated for carcinoma of cervix
and uterus. Cancer. 31:45–52. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jao SW, Beart RW Jr, Reiman HM, Gunderson
LL and Ilstrup DM: Colon and anorectal cancer after pelvic
irradiation. Dis Colon Rectum. 30:953–958. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Levitt MD, Millar DM and Stewart JO:
Rectal cancer after pelvic irradiation. J R Soc Med. 83:152–154.
1990.PubMed/NCBI
|
|
8
|
Tamai O, Nozato E, Miyazato H, Isa T,
Hiroyasu S, Shiraishi M, Kusano T, Muto Y and Higashi M:
Radiation-associated rectal cancer: Report of four cases. Dig Surg.
16:238–243. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shadad AK, Sullivan FJ, Martin JD and Egan
LJ: Gastrointestinal radiation injury: Symptoms, risk factors and
mechanisms. World J Gastroenterol. 19:185–198. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tsuji T, Sawai T, Nakagoe T, Hidaka S,
Shibasaki S, Tanaka K, Nanashima A, Yamaguchi H, Yasutake T and
Tagawa Y: Genetic analysis of radiation-associated rectal cancer. J
Gastroenterol. 38:1185–1188. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hotchi M, Shimada M, Kurita N, Iwata T,
Sato H, Morimoto S, Yoshikawa K, Higashijima J, Miyatani T, Mikami
C and Kashihara H: Short-term results of laparoscopic surgery after
preoperative chemoradiation for clinically staged T3 and T4 rectal
cancer. Asian J Endosc Surg. 5:157–163. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Perez CA, Breaux S, Bedwinek JM,
Madoc-Jones H, Camel HM, Purdy JA and Walz BJ: Radiation therapy
alone in the treatment of carcinoma of the uterine cervix. II.
Analysis of complications. Cancer. 54:235–246. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tomori H, Yasuda T, Shiraishi M, Isa T,
Muto Y and Egawa H: Radiation-associated ischemic coloproctitis:
Report of two cases. Surg Today. 29:1088–1092. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yurgelun MB, Masciari S, Joshi VA, Mercado
RC, Lindor NM, Gallinger S, Hopper JL, Jenkins MA, Buchanan DD,
Newcomb PA, et al: Germline TP53 mutations in patients with
early-onset colorectal cancer in the colon cancer family registry.
JAMA Oncol. 1:214–221. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Malkhosyan S, Rampino N, Yamamoto H and
Perucho M: Frameshift mutator mutations. Nature. 382:499–500. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fearon ER and Vogelstein B: A genetic
model for colorectal tumorigenesis. Cell. 61:759–767. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Minami K, Matsuzaki S, Hayashi N, Mokarim
A, Ito M and Sekine I: Immunohistochemical study of p53
overexpression in radiation-induced colon cancers. J Radiat Res.
39:1–10. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shirouzu K, Isomoto H, Morodomi T, Ogata
Y, Araki Y and Kakegawa T: Clinicopathologic characteristics of
large bowel cancer developing after radiotherapy for uterine
cervical cancer. Dis Colon Rectum. 37:1245–1249. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Arai T, Nakano T, Fukuhisa K, Kasamatsu T,
Tsunematsu R, Masubuchi K, Yamauchi K, Hamada T, Fukuda T, Noguchi
H, et al: Second cancer after radiation therapy for cancer of the
uterine cervix. Cancer. 67:398–405. 1991. View Article : Google Scholar : PubMed/NCBI
|