Introduction
In endocrine surgery, thyroid surgery is the most
commonly performed. Complications of thyroid surgery include
bleeding, damage to the recurrent laryngeal nerve (RLN) and
superior laryngeal nerve, and hypoparathyroidism. Intraoperative
bleeding is common in thyroid surgery because of the narrow visual
field and presence of several small blood vessels (1). In such a setting, bleeding is liable to
trigger various complications; postoperative bleeding in particular
can block the airways and occasionally cause complications.
Therefore, it is imperative to perform blood vessel dissection and
hemostasis in a dry surgical field.
The Harmonic FOCUS® (HF; Ethicon
Endo-Surgery, Inc.) comprises a range of ultrasonic surgical
devices that enable simultaneous dissection and coagulation of
tissue (2). Ultrasonic waves are
created by electromagnetic energy from a generator, which undergoes
piezoelectric transduction within the hand piece. The blade of the
HF vibrates at 55 kHz, producing mechanical energy that breaks
hydrogen bonds. The HF is hand-activated, with cutting and sealing
of vessels achieved by placing the curved blade in contact with the
tissue and applying pressure (3).
Ultrasonic coagulation and incision instruments were
purchased within the purview of medical insurance coverage in 1998
following the approval of their use in laparoscopic and
thoracoscopic surgery. Subsequently, these instruments have been
used in an ever-widening range of open and laparoscopic surgeries
including those for malignant tumors. It has been claimed that the
use of the HF decreases the duration of surgery, intraoperative
blood loss, volume of drainage fluid and postoperative
complications in abdominal laparoscopic surgery (4), thoracic surgery (5) and parotid surgery (6).
Recently, some reports have demonstrated the
efficacy of their use in thyroidectomy in terms of reduction of
surgical time and other postoperative outcomes (1,7–9). Therefore, numerous surgeons who perform
thyroid surgery use the HF.
This was a retrospective clinical study based on
prospectively collected data to assess the use of the HF for open
thyroidectomy. The aim of the present study was to compare surgical
outcomes between the HF and conventional techniques in open
thyroidectomy and evaluate any significant difference in
results.
Patients and methods
A total of 45 patients with thyroid disease treated
at the Department of Surgery, Surgical Oncology and Science of the
Sapporo Medical University Hospital (Sapporo, Japan) between
February 2013 and May 2016 were retrospectively analyzed in the
present study. We examined consecutive patients aged ≥18 years who
underwent total thyroidectomy or partial thyroidectomy for thyroid
malignancy or Basedow's disease with indications for surgery,
irrespective of the presence or absence of lymph node dissection.
Patients were divided into two groups: Those who underwent surgery
with HF group (n=21) and those who underwent conventional surgery
group (n=24) performed with electric scalpel and ligation.
All the surgeries were performed by a total of three
surgeons, two of whom had 16 years of experience and one had 11
years of experience. The HF was gradually introduced from May 2015
and was used in all of the cases in 2015–2016.
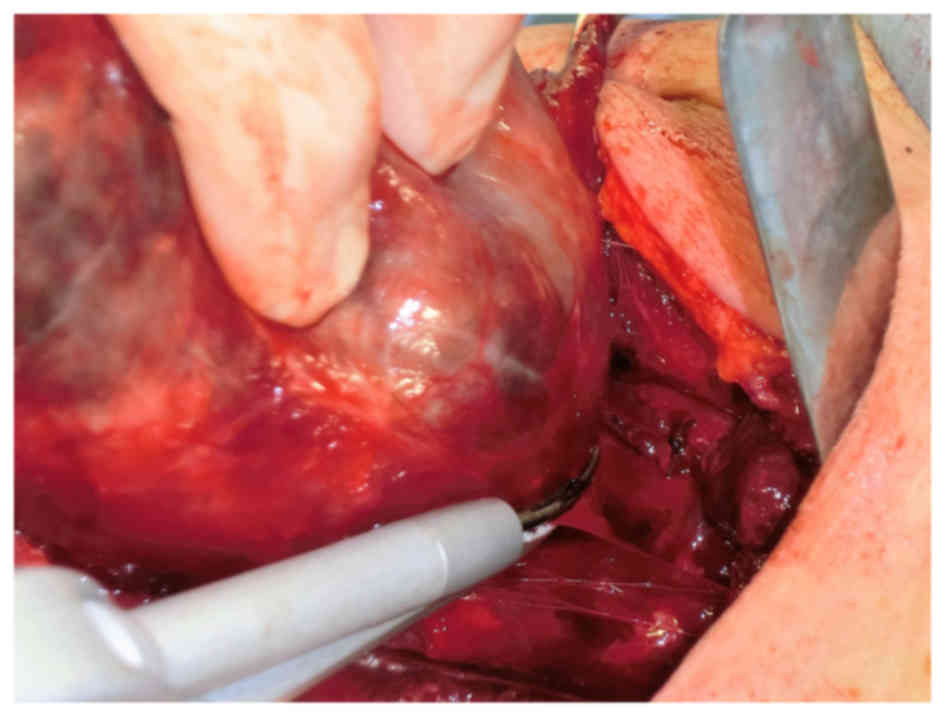
Surgical procedures were performed under general
anesthesia with endotracheal intubation. In surgeries performed
with HF, the approach to the thyroid involved transection of the
sternohyoid and the sternothyroid muscles, and most of the
dissections after skin flap creation were performed using HF
(Fig. 1). The superior and inferior
thyroid arteries and veins with diameter of ≥5 mm were ligated and
dissected; for all other blood vessels, the MIN mode of HF was
used. HF was used for dissection at the anterior surface of the
trachea including that of the Berry's ligament. For thyroid
lobectomy, coagulation and resection was performed in the MIN
mode.
The present study was performed according to the
Ethical Guidelines for Clinical Research of the Japanese Ministry
of Health, Labor and Welfare. An independent ethics committee for
each participating site approved the protocol and any
modifications. Written informed consent was obtained from all
patients or the patient's family.
Outcomes
The primary outcomes included duration of surgery
(in min) from the start of the incision until closure,
intraoperative estimated blood loss (ml), volume of drainage fluid
in the first 24 h following surgery, volume of drainage fluid until
drain removal (ml), duration of drain placement (days), and length
of hospitalization stay (days). The drain was removed once the
volume of drainage fluid was <10 ml for 1 day.
Secondary outcomes, which took safety into
consideration, included postoperative RLN paralysis, postoperative
hypocalcemia, postoperative bleeding that required surgical
intervention, and postoperative chylous fistula. Permanent RLN was
defined as paralysis that was present 1 year after surgery. RLN
paresis needed to be determined via laryngoscopy. Postoperative
hypocalcaemia was only evaluated for patients receiving a total
thyroidectomy (with or without neck dissection). Permanent
hypocalcaemia was defined as a need for vitamin D or calcium
supplementation 1 year after surgery.
Statistical analysis
Results are presented as mean values ± standard
deviation. Comparisons between the two groups were assessed with
the two-sample t test, Chi-square test. The non-parametric
Mann-Whitney U test was used to compare the operative and
postoperative parameters between the HF and CS groups. The
quantitative operative and postoperative parameters are expressed
as medians with their interquartile range (IQR). Differences were
considered significant when P<0.05. Statistical analysis was
performed using SAS, version 9.4 (SAS Institute, Cary, NC,
USA).
Results
Forty-five patients who underwent total or partial
thyroidectomy were enrolled in the present study, irrespective of
whether the disease was benign or malignant. The demographic
information of the study are summarized in Table I. No significant difference was
observed between the two groups with respect to patient attributes
[sex, age, body mass index, and nature of disease (benign or
malignant)]. With regards to the surgical procedure (total or
partial thyroidectomy), total thyroidectomy was performed with HF
in 6 patients (29%) and with CS in 10 patients (42%), whereas the
latter group had more patients; the difference was not
statistically significant.
 | Table I.Demographic parameters in the HF and
CS groups. |
Table I.
Demographic parameters in the HF and
CS groups.
| Parameter | HF (n=21) | CS (n=24) | P-value |
|---|
| Sex (%) |
|
| 0.8812a |
| Male | 4 (19) | 5 (21) |
|
|
Female | 17 (81) | 19 (79) |
|
| Age | 51.5±11.84 | 57.8±13.73 | 0.1039b |
| BMI
(kg/m2) | 23.6±3.42 | 23.7±3.93 | 0.9780b |
| Nature of disease
(%) |
|
|
|
|
Benign | 7 (33) | 8 (33) |
|
|
Malignancy | 14 (66) | 16 (66) |
|
| Extent of surgery
(%) |
|
| 0.3599a |
| Total
thyroidectomy | 6 (29) | 10 (42) |
|
| Partial
thyroidectomy | 15 (71) | 14 (58) |
|
Duration of surgery was significantly shorter in the
HF group compared with the CS group [median (IQR): 142 min
(121–160) vs. 151 min (136.8–299.3); P=0.0406] (Fig. 2A). Intraoperative blood loss was
significantly less in the HF group [median (IQR): 40 ml (0–80) vs.
125 ml (50–176.3); P=0.0054] (Fig.
2B). While there was no significant difference in the volume of
drainage fluid in the first 24 h post-surgery [median (IQR): 55 ml
(30–80) vs. 50 ml (30–90)] (Fig.
2C), the overall volume of drainage fluid until drain removal
was significantly lower in the HF group [median (IQR): 120 ml
(90–175) vs. 177.5 ml (110–288.8); P=0.0490] (Fig. 2D). There was no significant
difference between the two groups with respect to the duration of
drain placement [median (IQR): 4 days (3–4) vs. 5
days (4–5.25)] (Fig. 2E) and length
of hospitalization stay [median (IQR): 7 days (6–9) vs. 6
days (5.75–7)] (Fig. 2F).
Postoperative complications occurred in two patients
in the HF group and three in the CS group (Table II). Temporary RLN paralysis and
temporary hypocalcemia occurred in one patient in both groups. In
the CS group that underwent total thyroidectomy + neck dissection,
one patient developed postoperative chylous fistula. In this
patient, postoperative chylous fistula was diagnosed based on
increased volume and milky appearance of the drainage fluid after
recommencement of meals; however, symptoms were alleviated with one
week of fasting, continued negative pressure drainage, and total
parenteral nutrition. There was no significant difference in the
incidence of complications between the two groups (P=0.7513).
 | Table II.Postoperative surgical complications
between the HF and CS groups. |
Table II.
Postoperative surgical complications
between the HF and CS groups.
| Parameter | HF (n=21) | CS (n=24) | P-value |
|---|
| Complications | 2 (9.5%) | 3 (12.5%) | 0.7513a |
| Temporary paralysis
of RLN | 1 | 1 |
|
| Permanent paralysis
of RLN | 0 | 0 |
|
| Temporary
hypocalcaemia | 1 | 1 |
|
| Permanent
hypocalcaemia | 0 | 0 |
|
|
Hemorrhage requiring
surgery | 0 | 0 |
|
| Chyle
fistula | 0 | 1 |
|
| Surgical
site infection | 0 | 0 |
|
Discussion
In the present study, we compared the outcomes of
open thyroidectomy performed using HF with those performed using
the conventional clamp-and-tie technique. In our experience, the
use of HF is useful in shortening the duration of thyroid surgery.
This is likely attributable to the fact that tissue can be
detached, coagulated, and dissected with HF in a continuous
operation without the need to change instruments. The
characteristics of HF, i.e., the double-action jaws, shape similar
to that of the Kelly forceps used for pediatric procedures, and
curved, long, and narrow blades render it particularly suited for
thyroid surgery. On the basis of our experience, surgeons who are
generally capable of conventional thyroid surgery do not require a
particular learning period to master the use of HF.
Some negative reports indicate that routine drain
placement following thyroidectomy is not effective in reducing the
incidence of postoperative complications and that it may prolong
hospital stay and cause infection of the surgical site. However,
our surgical team placed drains in all patients who underwent
thyroidectomy. Although drain use is not routine and it is not
necessary in conventional thyroidectomy techniques as discussed in
the literature (10), it was used by
our surgical team in all the patients in the two groups.
During thyroid surgery, particular care should be
paid so as not to damage the RLN. In clinical studies, the
incidence of temporary RLN paralysis associated with the use of HF
for total thyroidectomy was 0.7–5.6% (11). Wu et al examined the effect of
use of HF on RLN in a porcine model with continuous
electrophysiological monitoring; they noted that the active blade
should be at a distance of at least 1 mm from the RLN to ensure
safety (12). Furthermore, in a
similar experimental model using porcine small intestines,
intermittent use of the harmonic operation significantly reduced
thermal damage to the surrounding tissues. A continuous activation
time of no more than 5 sec is recommended (13). With regards to treatment near the
RLN, nerve orientation is confirmed as per CS without using HF by
lifting the connective tissue of the anterior surface of the nerve
with forceps at a safe distance from the nerve followed by careful
blunt dissection.
As is the case in any type of surgery, shorter
surgical duration reduces the risk of surgical-site infection and
accelerates patient recovery (14).
The use of HF helps decrease the rate of adverse events such as RLN
paralysis and intraoperative blood loss. Furthermore, shorter
surgical duration was desirable from a cost perspective (15,16).
The present study has several limitations. The first
limitation is the small sample size. Reported outcomes are
potentially influenced by surgeon experience and other procedural
details which may have varied across the studies. Furthermore, the
underlying thyroid diseases in the study included both benign and
malignant diseases; differences with respect to tumor size and
pathological background may have influenced the level of surgical
difficulty.
Future studies should assess the areas of surgery
where HF would be effective and where it should be avoided. Further
studies should assess the level of skill required and cost
effectiveness of this surgery.
In conclusion, from this present study, the use of
HF reduced the duration of surgery, intraoperative blood loss, and
total volume of postoperative drainage fluid and did not increase
complications. Therefore, HF is a safe and reliable tool for use in
thyroid surgery and more effective than electric scalpel and
ligatures used in CS.
Acknowledgements
The present study was supported by a grant from the
Yuasa Memorial Foundation. The authors are grateful to all the
study participants.
References
|
1
|
Garas G, Okabayashi K, Ashrafian H, Shetty
K, Palazzo F, Tolley N, Darzi A, Athanasiou T and Zacharakis E:
Which hemostatic device in thyroid surgery? A network meta-analysis
of surgical technologies. Thyroid. 23:1138–1150. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Contin P, Gooßen K, Grummich K, Jensen K,
Schmitz-Winnenthal H, Büchler MW and Diener MK: ENERgized vessel
sealing systems versus CONventional hemostasis techniques in
thyroid surgery-the ENERCON systematic review and network
meta-analysis. Langenbecks Arch Surg. 398:1039–1056. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cannizzaro MA, Borzì L, Lo Bianco S,
Okatyeva V, Cavallaro A and Buffone A: Comparison between Focus
Harmonic scalpel and other hemostatic techniques in open
thyroidectomy: A systematic review and meta-analysis. Head Neck.
38:1571–1578. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Caglià P, Costa S, Tracia A, Veroux M,
Luca S, Zappulla E, Russo V, Lucifora B, Borzì L, Patanè G, et al:
Can laparoscopic cholecystectomy be safety performed in the
elderly? Ann Ital Chir. 83:1–24. 2012.PubMed/NCBI
|
|
5
|
Takagi K, Hata Y, Sasamoto S, Tamaki K,
Fukumori K, Otsuka H, Hasegawa C and Shibuya K: Late onset
postoperative pulmonary fistula following a pulmonary segmentectomy
using electrocautery or a harmonic scalpel. Ann Thorac Cardiovasc
Surg. 16:21–25. 2010.PubMed/NCBI
|
|
6
|
Prgomet D, Janjanin S, Bilić M, Prstacić
R, Kovac L, Rudes M and Katić V: A prospective observational study
of 363 cases operated with three different harmonic scalpels. Eur
Arch Otorhinolaryngol. 266:1965–1970. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Parmeggiani D, De Falco M, Avenia N,
Sanguinetti A, Fiore A, Docimo G, Ambrosino P, Madonna I, Peltrini
R and Parmeggiani U: Nerve sparing sutureless total thyroidectomy.
Preliminary study. Ann Ital Chir. 83:91–96. 2012.PubMed/NCBI
|
|
8
|
Minni A, Rosati D, Cavaliere C, De Carlo
A, Illuminati G, Scarano Catanzaro V and Bodoni M: Study on the use
of focus harmonic scalpel in thyroidectomies: Is it useful also in
preserving voice function? Eur Rev Med Pharmacol Sci. 20:3544–3551.
2016.PubMed/NCBI
|
|
9
|
Al-Dhahiry JK and Hameed HM: Total
thyroidectomy: Conventional suture ligation technique versus
sutureless techniques using harmonic scalpel or maxium. Ann Med
Surg (Lond). 5:29–34. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ozlem N, Ozdogan M, Gurer A, Gomceli I and
Aydin R: Should the thyroid bed be drained after thyroidectomy?
Langenbecks Arch Surg. 391:228–230. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lang BH, Ng SH, Lau LL, Cowling BJ and
Wong KP: A systematic review and meta-analysis comparing the
efficacy and surgical outcomes of total thyroidectomy between
harmonic scalpel versus ligasure. Ann Surg Oncol. 20:1918–1926.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wu CW, Chai YJ, Dionigi G, Chiang FY, Liu
X, Sun H, Randolph GW, Tufano RP and Kim HY: Recurrent laryngeal
nerve safety parameters of the Harmonic Focus during thyroid
surgery: Porcine model using continuous monitoring. Laryngoscope.
125:2838–2845. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pogorelić Z, Perko Z, Druzijanić N, Tomić
S and Mrklić I: How to prevent lateral thermal damage to tissue
using the harmonic scalpel: Experimental study on pig small
intestine and abdominal wall. Eur Surg Res. 43:235–240. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Elfenbein DM, Schneider DF, Chen H and
Sippel RS: Surgical site infection after thyroidectomy: A rare but
significant complication. J Surg Res. 190:170–176. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pons Y, Gauthier J, Ukkola-Pons E, Clément
P, Roguet E, Poncet JL and Conessa C: Comparison of LigaSure vessel
sealing system, harmonic scalpel and conventional hemostasis in
total thyroidectomy. Otolaryngol Head Neck Surg. 141:496–501. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Konturek A, Barczyński M, Stopa M and
Nowak W: Total thyroidectomy for non-toxic multinodular goiter with
versus without the use of harmonic FOCUS dissecting shears-a
prospective randomized study. Wideochir Inne Tech Maloinwazyjne.
7:268–274. 2012.PubMed/NCBI
|