Introduction
Solitary fibrous tumors (SFT), a rare mesenchymal
neoplasm originally described in the pleura by Klempere and Rabin
in 1931 (1), are uncommon spindle
cell neoplasms of mesenchymal origin, but more recently reported at
a wide range of anatomic sites.
Hemangiopericytoma (HPC) is a very rare vascular
tumor and originates from small pericapillary spindle cells called
Zimmermann's pericytes, which was first described by Stout and
Murray in 1942 as a tumor of the retroperitoneum, buttock, and
thigh (2). HPC has been considered
as a cellular variant of SFT. In the 2013 World Health Organization
(WHO) classification of tumors of the soft tissue, HPC was removed
as a synonym for SFT (3).
The predilection sites of this tumor are the lower
limbs, axilla, and pelvis as well as the head and neck (4). The head and neck area is the third most
common site, accounting for 15–30% of all occurrences. In the head
and neck region, the tumor usually involves the orbit, nasal
cavity, oral cavity, jaw, parotid gland, parapharyngeal space or
jugular foramen (5).
Numb chin syndrome (NCS) is a rare neurological
symptom and an indicator of various diseases. It describes a
condition presenting as orofacial sensory disturbance especially
localized to the lower lip and chin. The condition manifests
spontaneously without history of trauma, infection or obvious
dental cause. NCS is an important finding as it may be the initial
symptom of Multiple Sclerosis or metastatic malignancy (6).
In this paper, we report a case of a large SFT in
the infratemporal fossa which manifested NCS as the initial
symptom, and was treated with intensity modulated radiation therapy
alone.
Case report
An otherwise healthy 39-year-old female patient was
referred to our hospital having experienced right lower lip
numbness for one month. She had no past medical history. Initial
findings indicated no facial swelling or trismus. Intra-oral
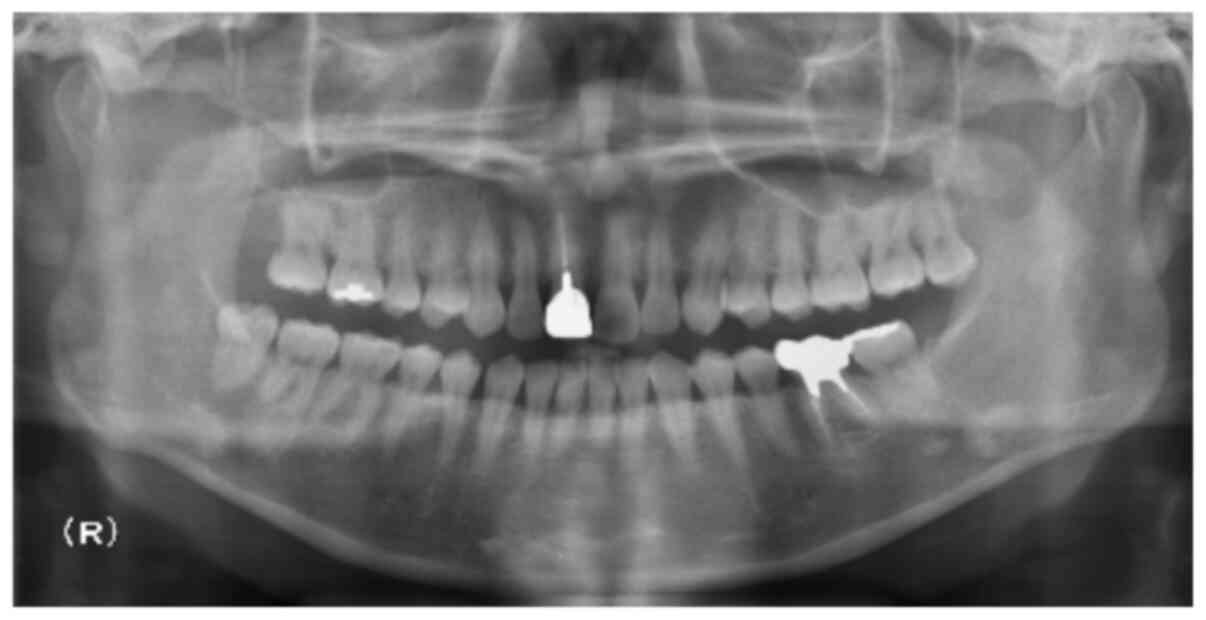
findings revealed no abnormal observation. Panoramic radiography
showed that there were no bony lesions at the mandible. However,
the right lower wisdom tooth showed signs of pericoronitis
(Fig. 1). The patient received
medication with antibiotics and Vitamin B12 to improve the
pericoronitis and right lower lip numbness. Two weeks following
referral, in spite of these medications, right lower lip numbness
was not improved. Three months later, the right lower wisdom tooth
was extracted, and subsequently right lower lip numbness was
slightly improved.
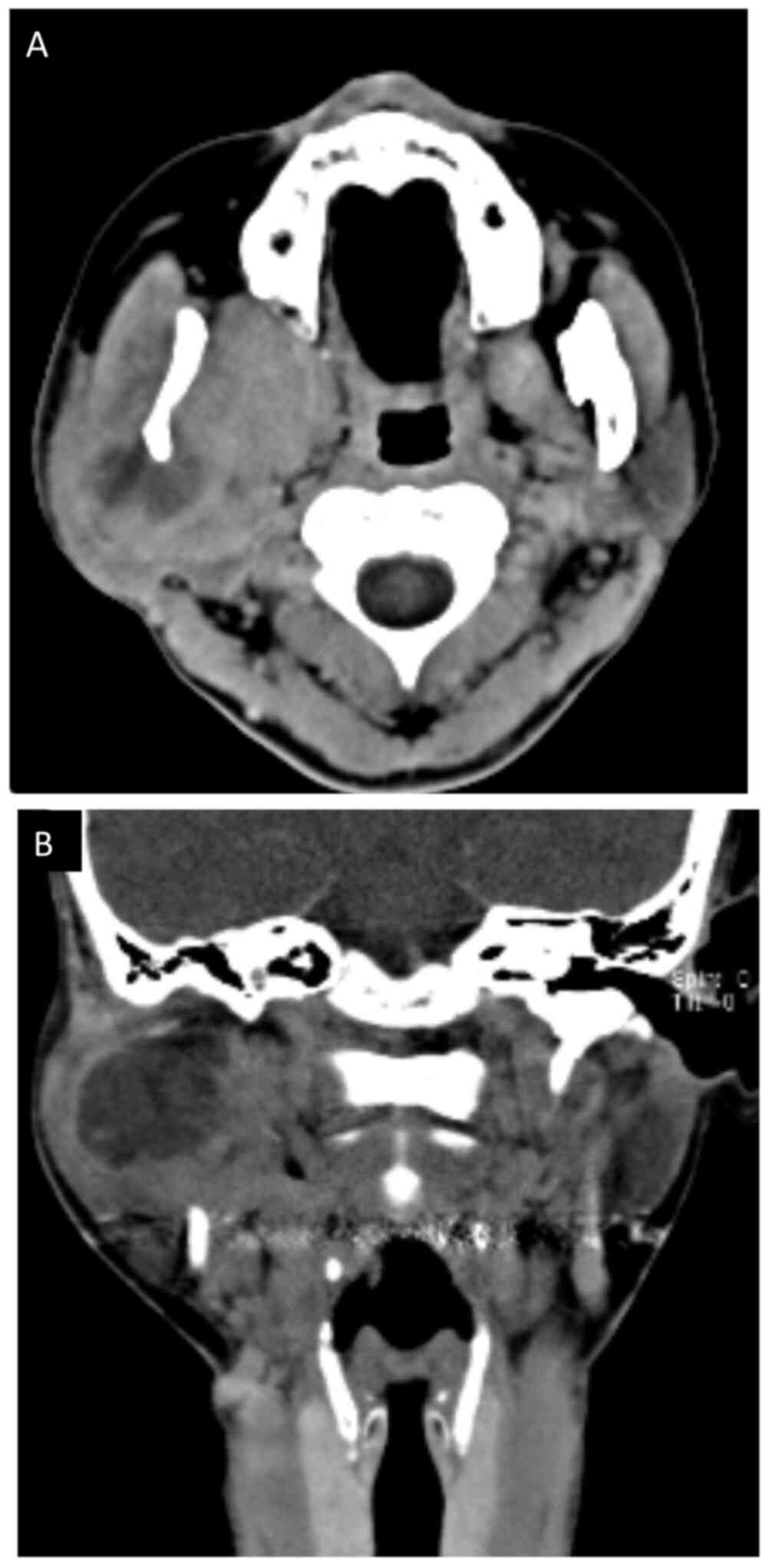
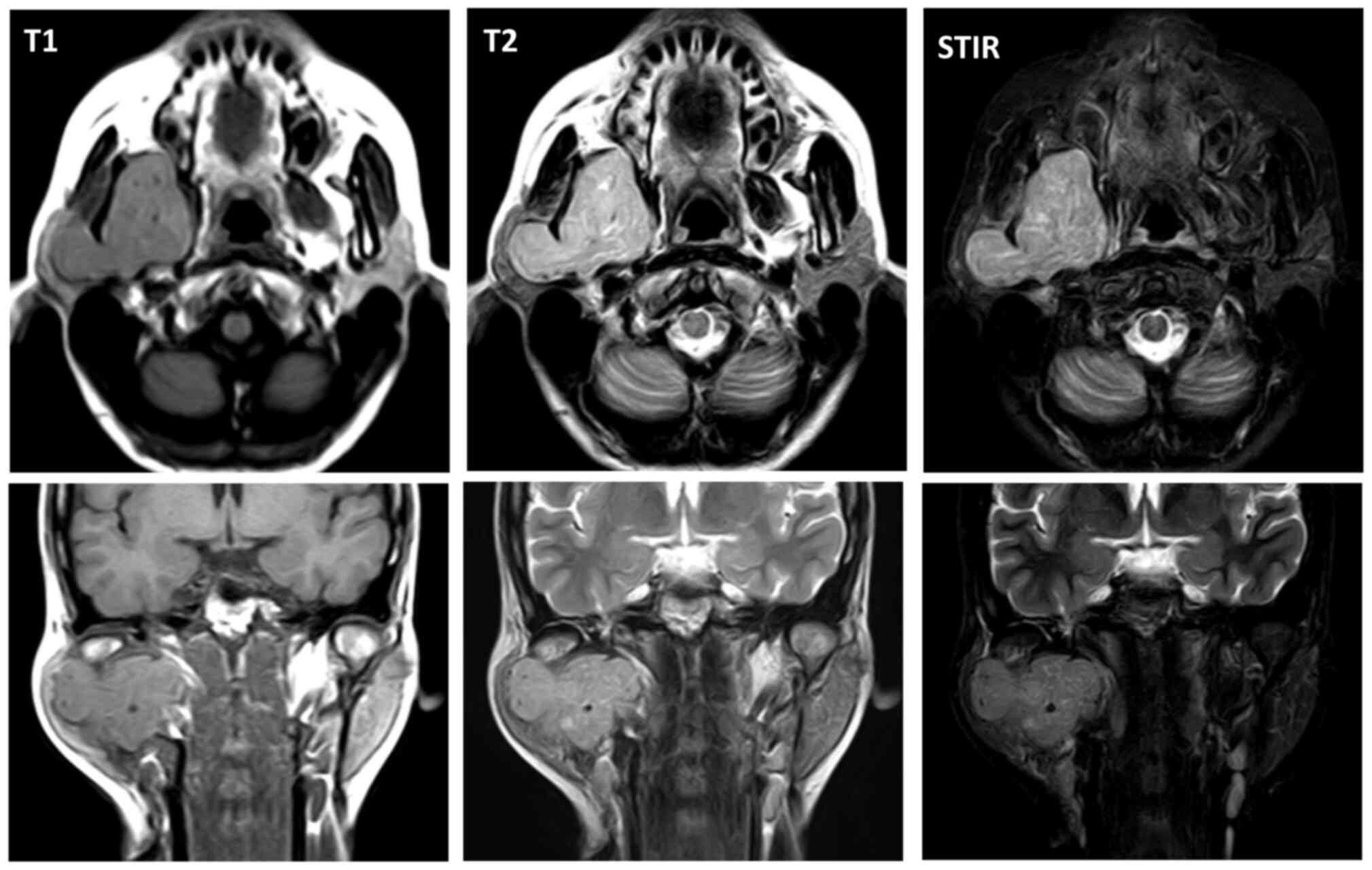
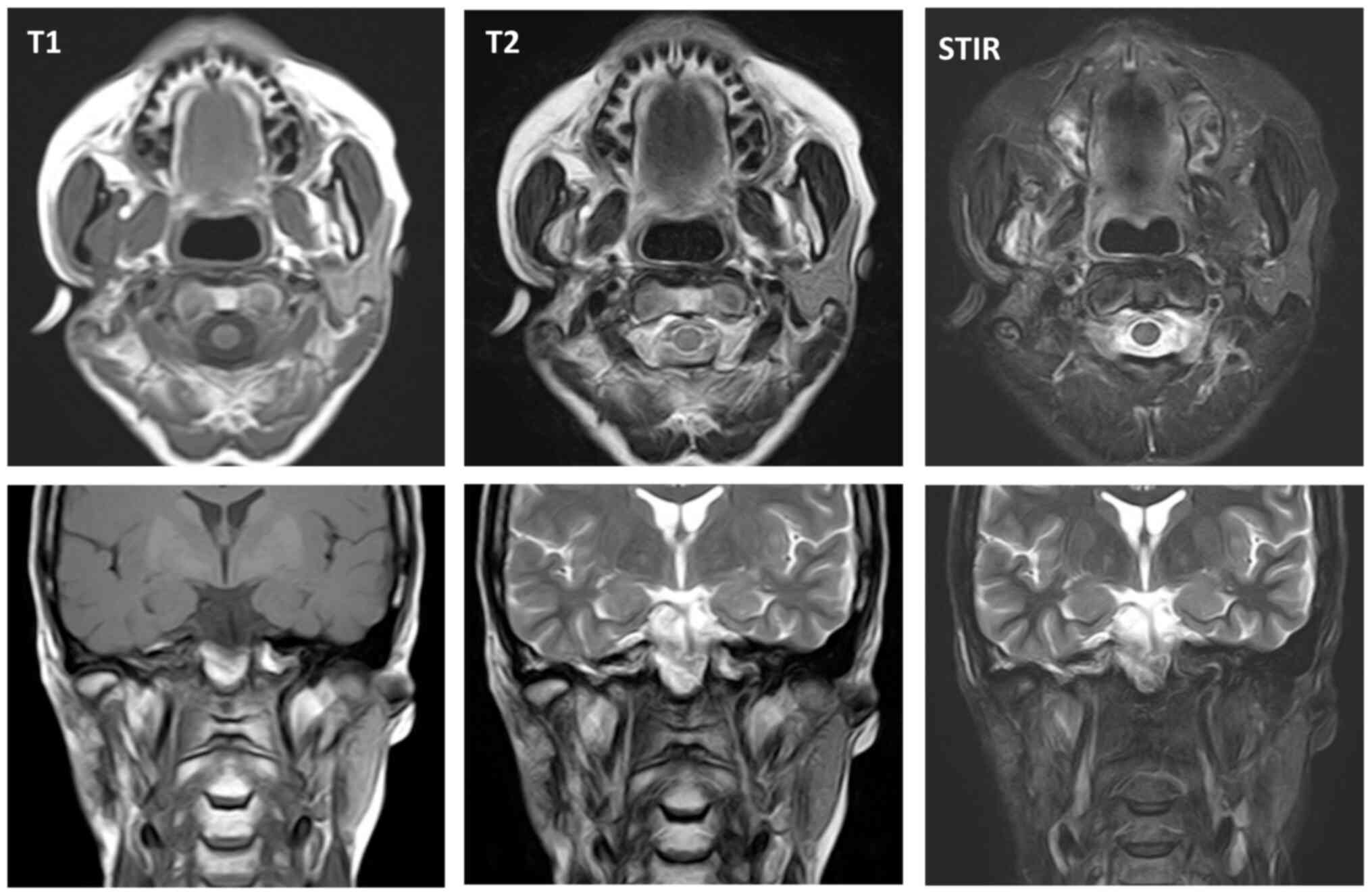
At five months post referral the lower part of the
right auricula displayed swelling. Computed tomography (CT) and
magnetic resonance imaging (MRI) revealed a space occupying mass
(52×50×40 mm) in the infratemporal fossa (Figs. 2 and 3). Fine needle aspiration biopsy (FNAB) was
performed at this site and hemoid gelatinous fluid was withdrawn.
However, pathological examination of the sample did not lead to
final diagnosis. Parotid gland tumor, neurilemoma, primitive
neuroectodermal tumor (PNET), conventional HPC, and SFT were cited
as differential diagnoses.
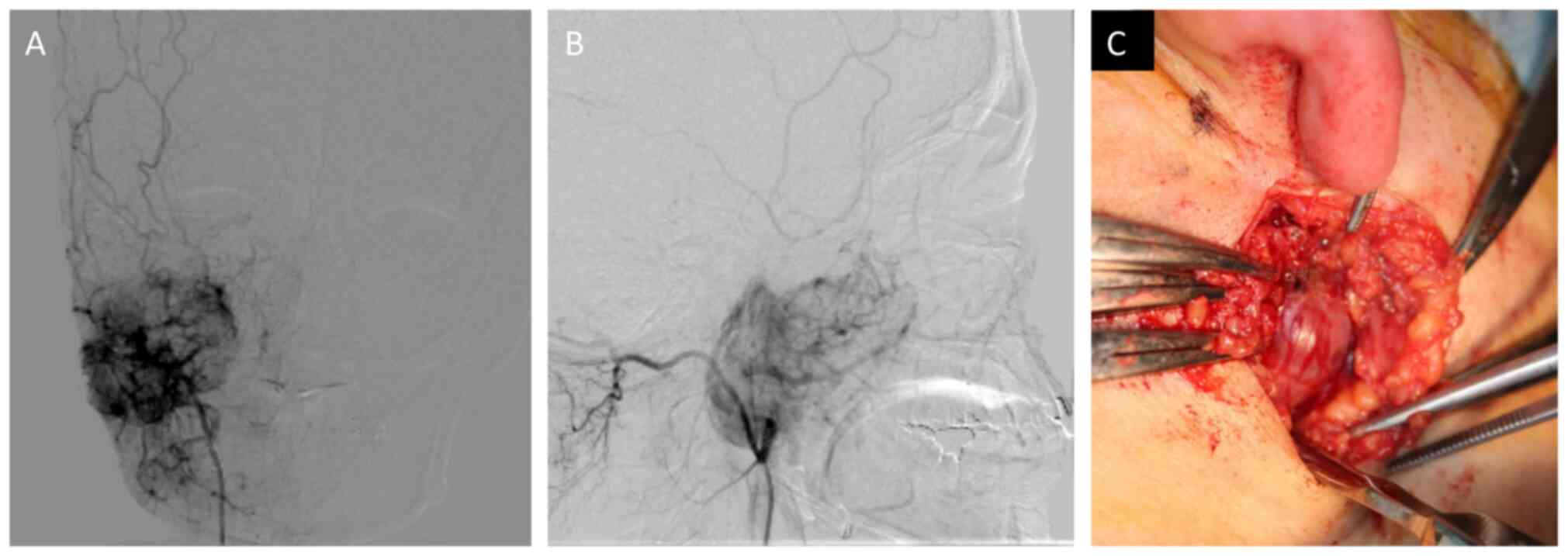
An open biopsy was performed on the lower part of
the right auricula following angiography assisted vascular
embolization of the maxillary artery (Fig. 4A and B). The tumor was found in
deeper layers than the parotid gland, and bleeding was not observed
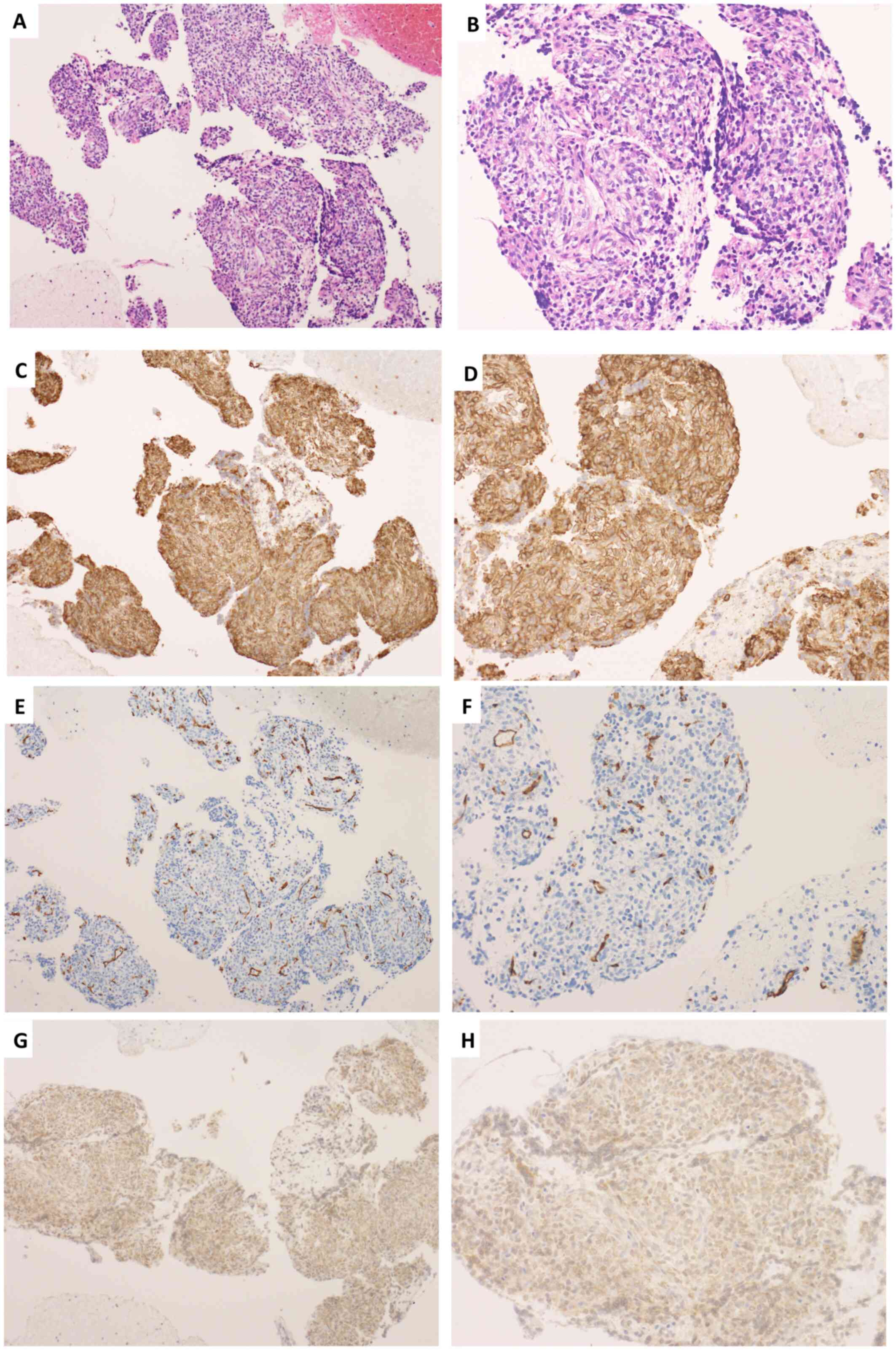
during biopsy due to the effect of vascular embolization (Fig. 4C). Immunohistologically, CD99 was
positive, CD34 was positive only for vascular endothelium, and B
cell lymphoma 2 (Bcl-2) was weakly positive. These findings
suggested SFT. Then, athological diagnosis was confirmed as SFT
(Fig. 5A-H).
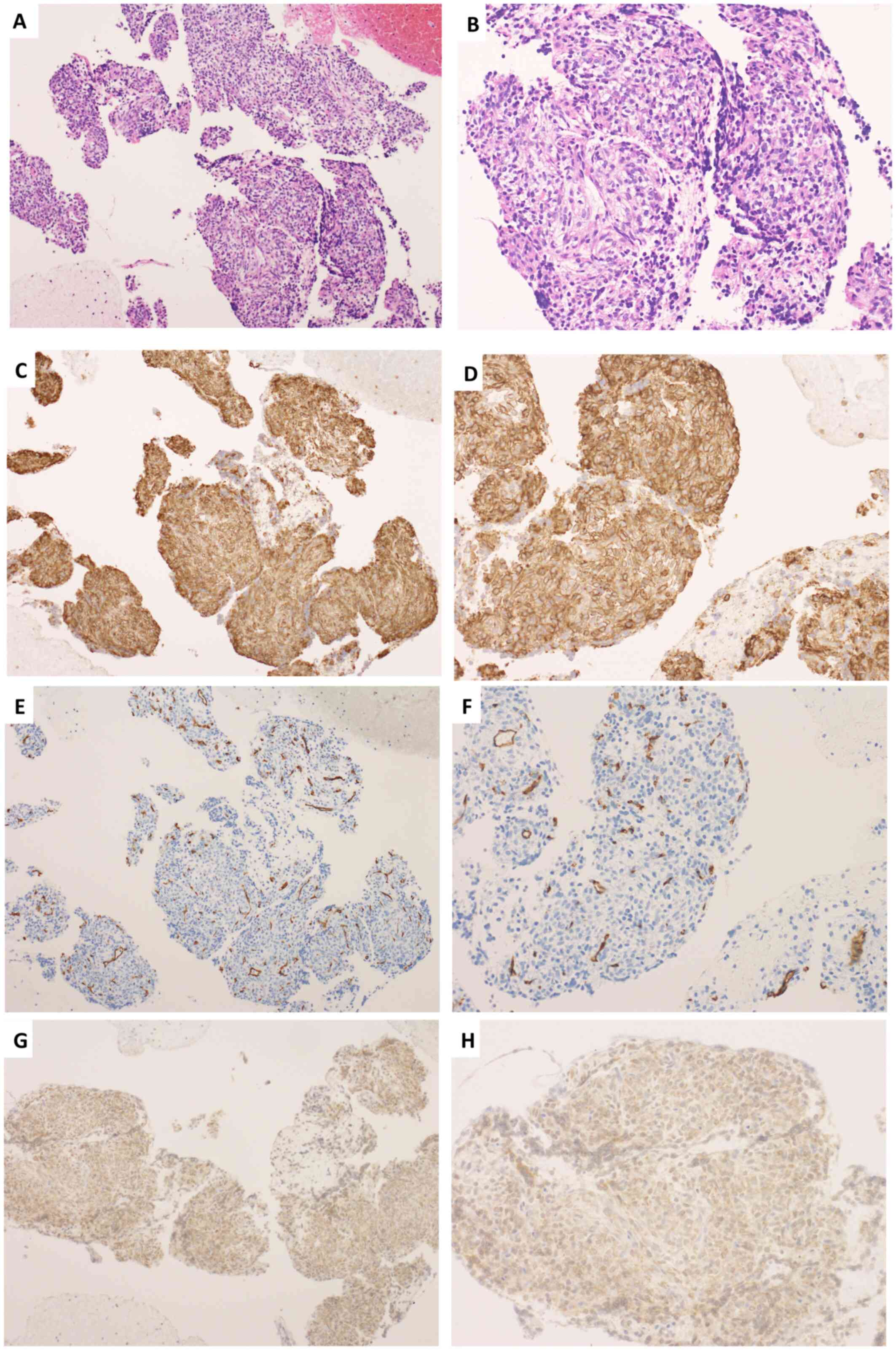 | Figure 5.Pathological findings. (A) Hematoxylin
and eosin staining (original magnification, ×10), (B) Hematoxylin
and eosin staining (original magnification, ×20). (C) CD99 staining
(original magnification, ×10), (D) CD99 staining (original
magnification, ×20), (E) CD34 staining (original magnification,
×10), (F) CD34 staining (original magnification, ×20), (G) Bcl-2
staining (original magnification, ×10), (H) Bcl-2 staining
(original magnification, ×20). |
We offered the patient intensity modulated radiation
therapy (IMRT) and obtained written informed consent. IMRT of the
primary lesion was performed five times per week at two Gray (Gy)
per fraction, for a total of 66 Gy. The treatment was continued,
with radiation being administered for about six weeks. The patient
developed grade two stomatitis, dry mouth, grade two dermatitis,
grade two alopecia, and grade two dysgeusia (National Cancer
Institute common toxicity criteria, version 4.0).
Successful shrinkage of the tumor was seen in MRI 3
years after treatment without recurrence (Fig. 6). Slight numbness of the lower lip,
trismus, occasional light dizziness and sustained tinnitus remained
as problematic disorders.
Discussion
SFT originating in the infratemporal fossa was first
described by Buchanan (7), followed
by several reports showing SFT arising from the infra temporal
fossa (8–10). These case reports showed swelling in
the temporal region without pain, and they did not show nerve palsy
as a first manifestation. In the case presented, the patient with a
huge SFT at the infratemporal fossa displayed numb chin syndrome as
a first manifestation and the period from first presentation to
final diagnosis took approximately 6 months. NCS is mostly caused
by odontogenic lesions, commonly recognized as symptoms of
Vincent's disease. NCS can also be caused by malignant tumor,
infectious disease, degenerative disease or metabolic disease in an
area supplied by the submandibular nerve (6). NCS should be differentially diagnosed
not only for odontogenic diseases but also the possibility of
various other causes, and sufficient image examination should be
considered.
SFT are a heterogeneous group of rare spindle-cell
tumors including benign and malignant neoplasms (11). In this case, NCS may be due to the
expansion of the tumor and compression of the trigeminal nerve
third branch.
SFT originate from mesothelial mesenchymal cells,
whereas HPC originates from capillary pericytes. These tumors have
much in common in clinical behavior, pathological findings and
image findings. HPC is now considered to be a cellular variant of
SFT. The 2006 WHO fascicle of soft tissue tumors stated the
histological appearance and clinical behavior of HPC and SFT are
similar, a view also shared by others (12). In the 2013 WHO classification of soft
tissue tumors, the terminology is unified as SFT only (13). In the case presented, the tumor was
diagnosed as HPC by histopathological examination including
immunostaining, but it was difficult to distinguish from SFT using
image findings alone.
The standard treatment of SFT is still
controversial. The optimal treatment for SFT is considered to be
radical resection of the tumor (14). SFT is considered to be a
radiosensitive tumor (10). The
combination of radical surgery and post-operative radiation therapy
was suggested to reduce the rate of local recurrence (15). Cytotoxic chemotherapy such as
doxorubicin-based, gemcitabine-based, and paclitaxel-based are used
for patients with locally advanced, recurrent, or metastatic SFT,
and show a poor response (16).
Recent novel targeted agents such as temozolomide-bevacizumab
combination therapy (17), sunitinib
(18), sorafenib (19), pazopanib (20) and anti-insulin-like growth factor I
agents (21) showed more favorable
results than conventional cytotoxic chemotherapy in advanced SFT
patients. In our case, we opted for a single treatment by IMRT to
the SFT at the infratemporal fossa because surgical access may be
difficult as this area includes the lower cranial nerve, internal
carotid artery, and internal jugular vein.
Despite the tumor size and anatomical site, tumor
shrinkage was obtained successfully without relapse/recurrence.
IMRT alone may be effective as a future potential treatment option
for locally advanced head and neck SFT.
References
|
1
|
Klemperer P and Rabin C: Primary neoplasms
of the pleura. A report of five cases. Am J Ind Med. 22:1–31. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Stout AP and Murray MR:
Hemangiopericytoma: A vascular tumor featuring zimmermann's
pericytes. Ann Surg. 116:26–33. 1942. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Doyle LA: Sarcoma classification: An
update based on the 2013 World Health Organization Classification
of Tumors of Soft Tissue and Bone. Cancer. 120:1763–1774. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koch M, Nielsen GP and Yoon SS: Malignant
tumors of blood vessels: Angiosarcomas, hemangioendotheliomas, and
hemangioperictyomas. J Surg Oncol. 97:321–329. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fareed MM, Al Amro AS, Akasha R, Al Assiry
M, Al Asiri M, Tonio M and Bayoumi Y: Parapharyngeal space
hemangiopericytoma treated with surgery and postoperative
radiation-a case report. Head Neck Oncol. 4:102012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Smith RM, Hassan A and Robertson CE: Numb
chin syndrome. Curr Pain Headache Rep. 19:442015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Buchanan G: Two rare tumours involving the
infratemporal fossa: Alveolar soft part sarcoma and
haemangiopericytoma. J Laryngol Otol. 89:375–389. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kanazawa T, Nishino H, Miyata M, Kuriki K,
Abe K and Ichimura K: Haemangiopericytoma of infratemporal fossa. J
Laryngol Otol. 115:77–79. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Brucoli M, Giarda M, Valente G and Benech
A: Hemangiopericytoma of the infratemporal fossa: Progression
toward malignancy in a 30-year history. J Craniofac Surg.
16:1146–1150. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bianchi B, Poli T, Bertolini F and Sesenna
E: Malignant hemangiopericytoma of the infratemporal fossa: Report
of a case. J Oral Maxillofac Surg. 60:309–312. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Penel N, Amela EY, Decanter G, Robin YM
and Marec-Berard P: Solitary fibrous tumors and so-called
hemangiopericytoma. Sarcoma. 2012:6902512012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ambrosini-Spaltro A and Eusebi V:
Meningeal hemangiopericytomas and hemangiopericytoma/solitary
fibrous tumors of extracranial soft tissues: A comparison. Virchows
Arch. 456:343–354. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fletcher CD, Bridge J and Lee J: World
Health Organization Classification of Tumours of Soft Tissue and
Bone. IARC Press; Lyon, France: 2013
|
|
14
|
Koscielny S, Bräuer B and Förster G:
Hemangiopericytoma: A rare head and neck tumor. Eur Arch
Otorhinolaryngol. 260:450–453. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Schirmer CM and Heilman CB:
Hemangiopericytomas of the skull base. Neurosurg Focus. 30:E102011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Park MS, Ravi V, Conley A, Patel SR, Trent
JC, Lev DC, Lazar AJ, Wang WL, Benjamin RS and Araujo DM: The role
of chemotherapy in advanced solitary fibrous tumors: A
retrospective analysis. Clin Sarcoma Res. 3:72013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park MS, Patel SR, Ludwig JA, Trent JC,
Conrad CA, Lazar AJ, Wang WL, Boonsirikamchai P, Choi H, Wang X, et
al: Activity of temozolomide and bevacizumab in the treatment of
locally advanced, recurrent, and metastatic hemangiopericytoma and
malignant solitary fibrous tumor. Cancer. 117:4939–4947. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stacchiotti S, Negri T, Palassini E, Conca
E, Gronchi A, Morosi C, Messina A, Pastorino U, Pierotti MA, Casali
PG and Pilotti S: Sunitinib malate and figitumumab in solitary
fibrous tumor: Patterns and molecular bases of tumor response. Mol
Cancer Ther. 9:1286–1297. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Domont J, Massard C, Lassau N, Armand JP,
Le Cesne A and Soria JC: Hemangiopericytoma and antiangiogenic
therapy: Clinical benefit of antiangiogenic therapy (sorafenib and
sunitinib) in relapsed malignant haemangioperyctoma/solitary
fibrous tumour. Invest New Drugs. 28:199–202. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sleijfer S, Ray-Coquard I, Papai Z, Le
Cesne A, Scurr M, Schöffski P, Collin F, Pandite L, Marreaud S, De
Brauwer A, et al: Pazopanib, a multikinase angiogenesis inhibitor,
in patients with relapsed or refractory advanced soft tissue
sarcoma: A phase II study from the European organisation for
research and treatment of cancer-soft tissue and bone sarcoma group
(EORTC study 62043). J Clin Oncol. 27:3126–3132. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Quek R, Wang Q, Morgan JA, Shapiro GI,
Butrynski JE, Ramaiya N, Huftalen T, Jederlinic N, Manola J, Wagner
AJ, et al: Combination mTOR and IGF-1R inhibition: Phase I trial of
everolimus and figitumumab in patients with advanced sarcomas and
other solid tumors. Clin Cancer Res. 17:871–879. 2011. View Article : Google Scholar : PubMed/NCBI
|