Introduction
Since the introduction of laparoscopic surgery in
gynecology, there have been significant advances in minimally
invasive surgery (MIS), and laparoscopic surgery is becoming the
gold standard approach for malignancies as well as benign
conditions in gynecology. Laparoscopic surgery for patients with
endometrial cancer has been covered by insurance from April 2014
onwards, and laparoscopic radical hysterectomy for patients with
cervical cancer was approved as advanced medical treatment in
December 2014 in Japan. However, laparoscopic surgery requires
special skills, and education of the operator is necessary in the
context of human resource development. Moreover, skill-enhancing
laparoscopic training programs are urgently needed.
Among the various training tools, dry box training
is not suitable for dissection, incision and coagulation with an
electric scalpel. In addition, live animals, such as pigs, differ
from humans anatomically as they have a bicornuate uterus.
Moreover, anesthesiology personnel is required for laparoscopic
training using a live anesthetized pig, adding to the total cost of
training. Human cadavers have recently been introduced in
laparoscopic training (1–7). In particular, the human cadaver appears
to be the best anatomic and clinical-like model for surgical
procedure training (8), and the
validity of laparoscopic training using fresh-frozen cadavers has
been previously reported (7).
However, fresh-frozen cadavers are very costly, as they must be
preserved in a large freezer, and are also associated with the risk
of infections.
Thiel et al developed a low-odor embalming
technique in which the color, consistency and transparency of the
tissues are very well preserved. Furthermore, the efficacy of the
method for disinfection was confirmed by bacteriological tests
(9). Giger et al reporting on
laparoscopic training on Thiel-embalmed human cadavers (THCs)
suggested that this may be an excellent additional model to teach
advanced skills for bariatric, hernia and colon surgery (10). In this report, the assessment was
focused on the authenticity, consistency and tactility of the THCs
through the use of questionnaires.
Hands-on training using THCs was introduced in our
center in December 2012. Studies using cadavers in our center are
conducted according to Guidelines for Cadaver Dissection in
Education and Research of Clinical Medicine (Japan Surgical Society
and Japanese Association of Anatomists) (11). Laparoscopic training for
gynecological surgery using THCs was initiated in 2014. To evaluate
the usefulness of THCs, we analyzed the authenticity of tissue
color, consistency and operative tactility of THCs compared with
in vivo laparoscopic training for advanced gynecological
surgery using a similar method to that previously reported by Giger
et al (10).
Materials and methods
Hands-on training courses using THCs were held at
Ehime University Graduate School of Medicine between March 2014 and
October 2017. Obstetricians and gynecologists from Ehime University
Hospital and the main district hospital participated in the
training. The training on THCs included advanced laparoscopic
procedures, such as laparoscopic radical hysterectomy type III,
involving the identification of the ureter, and lymphadenectomy, as
well as hysterectomy and bilateral salpingo-oophorectomy. One THC
was used by two participants, and the set-up time was 6 h.
At the end of the training, data were collected
using a standardized, anonymous questionnaire termed Likert scale
(1, strongly disagree; 2, disagree; 3, neither agree nor disagree;
4, agree; and 5, strongly agree). The survey items on the
questionnaire included color of tissues and organs, consistency,
authenticity of anatomical condition, operative tactility compared
with in vivo surgery, disturbance by odors and overall
satisfaction with the training course. Data are provided as mean ±
standard deviation. The training using THCs described above was
undertaken with the approval of the Ethics Committee of our
institution. Informed consent was also obtained from the
participants prior to enrolling.
Results
Hands-on training courses using THCs were held a
total of 11 times at Ehime University Graduate School of Medicine
between March 2014 and October 2017. The participants from our
hospital and five other medical facilities included 17
obstetricians and gynecologists who had been performing
laparoscopic surgery with >10 years of expertise and experience
as a doctor.
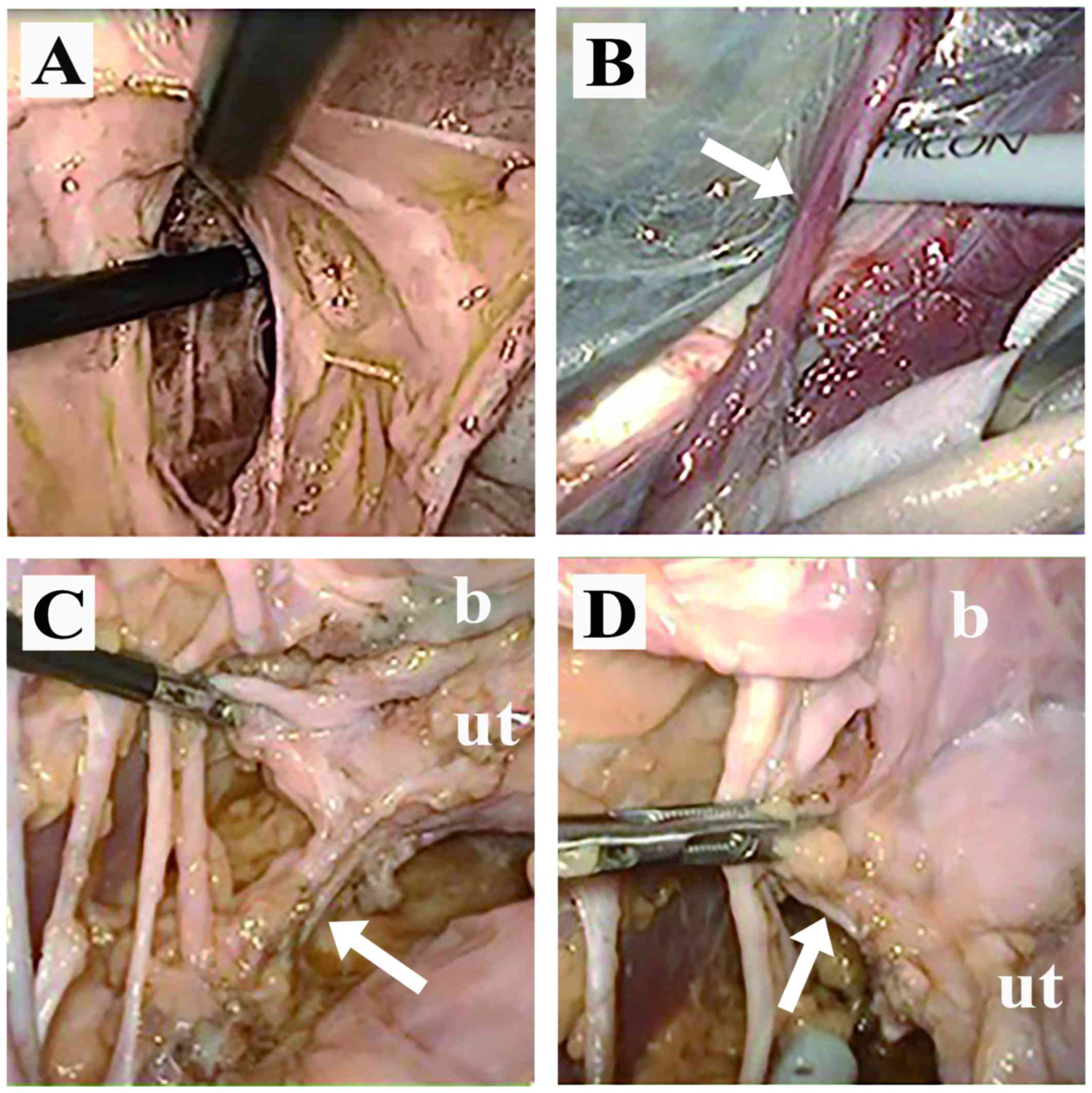
Laparoscopic training comprised hands-on training on
laparoscopic radical hysterectomy type III as follows:
Identification and isolation of the ureter, opening of the left
paravesical space and pelvic lymphadenectomy, dissection of the
posterior leaf of the vesicouterine ligament and isolation of the
left cardinal ligament, as well as hysterectomy and bilateral
salpingo-oophorectomy (Fig. 1).
Assessment of each organ of the
THCs
When analyzing the quality of tissue or organ color
compared with in vivo conditions, agreement or strong
agreement was stated by the majority of the participants regarding
the uterus (3.8±0.7), adnexa (3.8±0.8) and ureter (3.7±0.7), but
not for large blood vessels (2.9±0.8). Furthermore, equivalent
results were obtained regarding tissue and organ consistency
compared with in vivo conditions as follows: Uterus
(3.9±1.0), adnexa (4.1±0.8) and ureter (3.6±1.0); however, strong
agreement was not stated for large blood vessels (2.8±0.7). The
highest scores were observed regarding the authenticity of
anatomical condition compared with in vivo surgery: Uterus
(4.6±0.6), adnexa (4.6±0.6), ureter (4.5±0.6) and large blood
vessels (4.2±0.7). Moreover, when asking whether operative
tactility during training was comparable with in vivo
surgery, equivalent results were obtained for color and
consistency: Uterus (4.1±0.9), adnexa (4.1±0.8) and ureter
(3.6±0.9); however, there were no strong agreement statements for
large blood vessels (2.7±0.7). The assessment of each organ of the
THCs is summarized in Table I.
 | Table I.Assessment of each organ of the
THCs. |
Table I.
Assessment of each organ of the
THCs.
| Questions | Uterus (n=17) | Adnexa (n=17) | Ureter (n=17) | Large blood vessels
(n=17) |
|---|
| Is the quality of
organ color of THCs comparable to in vivo surgery? | 3.8±0.7 | 3.8±0.8 | 3.7±0.7 | 2.9±0.8 |
| Is the quality of
organ consistency of THCs comparable to in vivo
surgery? | 3.9±1.0 | 4.1±0.8 | 3.6±1.0 | 2.8±0.7 |
| Is the anatomical
condition on THCs authentic to in vivo findings? | 4.6±0.6 | 4.6±0.6 | 4.5±0.6 | 4.2±0.7 |
| Is the operative
tactility during training on THCs comparable to in vivo
surgery? | 4.1±0.9 | 4.1±0.8 | 3.6±0.9 | 2.7±0.7 |
Assessment of laparoscopic training
using THCs
No offensive odors by THCs were reported by any of
the participants during training; in addition, there were no
disagreement or strong disagreement statements regarding offensive
odors (3.9±0.6). Additionally, the majority of the participants
strongly agreed that the training using THCs would help improve
their laparoscopic skills (4.8±0.4) with a high level of
satisfaction (4.8±0.4). Furthermore, most participants also
reported that they would recommend this training to other
obstetrician-gynecologists (4.7±0.5). The assessment of
laparoscopic training using THCs is summarized in Table II.
 | Table II.Assessment of laparoscopic training
using THCs (n=17). |
Table II.
Assessment of laparoscopic training
using THCs (n=17).
| Statement | Agreement (Likert
scale) |
|---|
| I was not disturbed
by odors during training on THCs | 3.9±0.6 |
| The training will
help me to improve my laparoscopic skills | 4.8±0.4 |
| I am very satisfied
with the training | 4.8±0.4 |
| I will recommend the
training to other obstetrician-gynecologists | 4.7±0.5 |
Discussion
Since the introduction of laparoscopic surgery,
there has been an increasing need for laparoscopic interventions
over the last few decades with the advances in surgical practice
and medical equipment. Laparoscopic surgery has recently become the
gold standard approach for malignancies as well as benign
conditions in gynecology. Laparoscopic surgery requires special
skills, and laparoscopic training programs to improve technical
skills are urgently needed. Moreover, education of the operator is
necessary in the context of human resource development. In addition
to training tools, such as dry box training and live animals, human
cadavers were recently introduced in laparoscopic training
(1–7). Due to the anatomy and tissue fidelity,
human cadaver models appear to be optimal for surgical procedure
training (8), and the validity of
laparoscopic training using fresh-frozen cadavers has been
previously reported (7).
In particular, Thiel et al developed a
low-odor embalming technique with which the color, consistency and
transparency of the tissue are well-preserved. High standards of
preservation were confirmed without releasing harmful substances
into the environment. The concentration of formaldehyde in room air
remained under the limit of detection. The efficacy for
disinfection when using this method has been confirmed with
bacteriological tests (9). The
tissue quality, elasticity and handling of THCs are satisfactory,
and they have been previously used for teaching and urological
skills training (12). The efficacy
and role of training using THCs were also reported in other
departments (12–17). Furthermore, the validity and
reliability of THCs have also been reported in transperitoneal
laparoscopic nephrectomy training (18), as well as in various advanced
laparoscopic training courses for colon, hernia and bariatric
surgery (10).
THCs ensure excellent conditions, with flexibility
and plasticity of tissues and organs. Enough working space was
provided, similar to in vivo conditions under
pneumoperitoneum. The authenticity of organ color was comparable to
in vivo findings in the uterus, adnexa, and ureter, but not
in large blood vessels. Similar results were reported for the
authenticity of organ consistency and operative tactility. The
highest scores were obtained for the authenticity of the anatomical
condition of each organ. The high anatomical authenticity of THCs
was confirmed as none of the participants stated disagree or
strongly disagree. Alternatively, large blood vessels, such as the
inferior vena cava and iliac vein, were relaxed and there was no
pulse or bleeding following injury. Hence, a lower agreement rate
was observed regarding the authenticity of large blood vessels
other than the anatomical condition.
None of the participants answered disagree or
strongly disagree regarding offensive odors during training. These
results support one of the characteristics of THCs, namely that the
concentration of formaldehyde in room air remains under the limit
of detection. Furthermore, the level of satisfaction with the
training using THCs was high; in addition, most participants stated
agree or strongly agree that the training using THCs will help
improve their laparoscopic skills, and that they would recommend
this training to other obstetrician-gynecologists.
However, there remain other issues: First, the
number of THCs available for training is limited and uncertain,
since all cadavers were personal donations by will to the Anatomy
of the Ehime University. Furthermore, the cost per cadaver for
embalming and preservation is high (~1,000 USD). Finally, the
medical equipment used in laparoscopic surgery must also be
rented.
In our experience, training using THCs is an
excellent tool enabling advanced laparoscopic training for
gynecological malignancies. However, it is necessary to reduce the
total cost of this type of training for it to be held periodically
and continuously.
In conclusion, laparoscopic training for
gynecological malignancies using THCs was comparable to the in
vivo conditions in terms of surgical view and operative
tactility. Therefore, THCs constitute a valuable training tool for
improving the laparoscopic surgical skills for gynecological
malignancies. However, is necessary to reduce the total costs of
training using THCs to make it sustainable.
References
|
1
|
Fernandes CF, Ruano JM, Kati LM, Noguti
AS, Girão MJ and Sartori MG: Assessment of laparoscopic skills of
gynecology and obstetrics residents after a training program.
Einstein (Sao Paulo). 14:468–472. 2016.(In English, Portuguese).
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Antosh DD, Auguste T, George EA, Sokol AI,
Gutman RE, Iglesia CB, Desale SY and Park AJ: Blinded assessment of
operative performance after fundamentals of laparoscopic surgery in
gynecology training. J Minim Invasive Gynecol. 20:353–359. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Botchorishvili R, Rabischong B, Larraín D,
Khoo CK, Gaia G, Jardon K, Pouly JL, Jaffeux P, Aublet-Cuvelier B,
Canis M and Mage G: Educational value of an intensive and
structured interval practice laparoscopic training course for
residents in obstetrics and gynecology: A four-year prospective,
multi-institutional recruitment study. J Surg Educ. 69:173–179.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Urwitz-Lane RS, Lee RH, Peyre S, Rahman S,
Kwok L and Muderspach L: Impact of laparoscopic experience on
performance on laparoscopic training drills among obstetrics and
gynecology residents: A pilot study. J Minim Invasive Gynecol.
16:72–75. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kirby TO, Numnum TM, Kilgore LC and
Straughn JM: A prospective evaluation of a simulator-based
laparoscopic training program for gynecology residents. J Am Coll
Surg. 206:343–348. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kirwan WO, Kaar TK and Waldron R: Starting
laparoscopic cholecystectomy-the pig as a training model. Ir J Med
Sci. 160:243–246. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sharma M and Horgan A: Comparison of
fresh-frozen cadaver and high-fidelity virtual reality simulator as
methods of laparoscopic training. World J Surg. 36:1732–1737. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lam F, Jankova L, Dent OF, Molloy MP, Kwun
SY, Clarke C, Chapuis P, Robertson G, Beale P, Clarke S, et al:
Identification of distinctive protein expression patterns in
colorectal adenoma. Proteomics Clin Appl. 4:60–70. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Thiel W: The preservation of the whole
corpse with natural color. Ann Anat. 174:185–195. 1992.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Giger U, Frésard I, Häfliger A, Bergmann M
and Krähenbühl L: Laparoscopic training on Thiel human cadavers: A
model to teach advanced laparoscopic procedures. Surg Endosc.
22:901–906. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Japan Surgical Society and Japanese
Association of Anatomists: Guidelines for cadaver dissection in
education and research of clinical medicine. Kaibogaku Zasshi.
87:21–23. 2012.(In Japanese). PubMed/NCBI
|
|
12
|
Healy SE, Rai BP, Biyani CS, Eisma R,
Soames RW and Nabi G: Thiel embalming method for cadaver
preservation: A review of new training model for urologic skills
training. Urology. 85:499–504. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Charbonney E, Delisle S, Savary D,
Bronchti G, Rigollot M, Drouet A, Badat B, Ouellet P, Gosselin P,
Mercat A, et al: A new physiological model for studying the effect
of chest compression and ventilation during cardiopulmonary
resuscitation: The Thiel cadaver. Resuscitation. 125:135–142. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Munirama S, Zealley K, Schwab A, Columb M,
Corner GA, Eisma R and McLeod GA: Trainee anaesthetist diagnosis of
intraneural injection-a study comparing B-mode ultrasound with the
fusion of B-mode and elastography in the soft embalmed Thiel
cadaver model. Br J Anaesth. 117:792–800. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Maruyama D, Chaki T, Omote M, Hirata N,
Yamauchi M and Yamakage M: Movements of the double-lumen
endotracheal tube due to lateral position with head rotation and
tube fixation: A Thiel-embalmed cadaver study. Surg Radiol Anat.
37:841–844. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Munirama S, Satapathy AR, Schwab A, Eisma
R, Corner GA, Cochran S, Soames R and McLeod GA: Translation of
sonoelastography from Thiel cadaver to patients for peripheral
nerve blocks. Anaesthesia. 67:721–728. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Alberty J, Filler TJ, Schmal F and Peuker
ET: Thiel method fixed cadaver ears. A new procedure for graduate
and continuing education in middle ear surgery. HNO. 50:739–742.
2002.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rai BP, Stolzenburg JU, Healy S, Tang B,
Jones P, Sweeney C, Somani BK, Biyani CS and Nabi G: Preliminary
validation of Thiel embalmed cadavers for laparoscopic radical
nephrectomy. J Endourol. 29:595–603. 2015. View Article : Google Scholar : PubMed/NCBI
|