Introduction
Vulval cancer is a rare malignancy, with ~1,300 new
cases diagnosed annually in the UK (1). The most common histological subtype is
squamous cell carcinoma, accounting for 90% of all cases. Sarcomas
encompass a group of tumours of mesenchymal origin and account for
only 3% of cancers affecting the female genital tract (2). Most sarcomas affect the uterine body;
however, 1–3% of the cases affect the vulva (3). Extraskeletal myxoid chondrosarcoma
(EMC) is a rare subtype of sarcoma, which was first described in
1972 by Enzinger and Shiraki (4).
Since that time, there have been few reported cases of this rare
tumour in the literature, and fewer still reported to affect the
female genital tract (Table I)
(5–10). EMCs tend to affect patients in the
6th decade of life and have a predilection for the deep soft tissue
of the lower extremities.
 | Table I.Literature review of reported cases of
vulval extraskeletal myxoid chondrosarcoma. |
Table I.
Literature review of reported cases of
vulval extraskeletal myxoid chondrosarcoma.
| Author (Refs.) | Year | Patient no. | Age, years | Site | Management | Margins | Adjuvant
treatment | Follow-up
(months) | Recurrence |
|---|
| Santacruz et
al (5) | 2005 | 1 | 46 |
Vulva/periclitoral | Surgical
excision | Clear | Nil | 6 | No |
| Khan et al
(6) | 2011 | 1 | 66 | Labium majus | Surgical
excision | Clear | Refused by
patient | 12 | No |
| Sawada et al
(7) | 2011 | 1 | 24 | Right labium
majus | Modified
vulvectomy | Clear | Nil | 24 | No |
| Jeh et al
(8) | 2013 | 3 | 68 | Right labium
majus | Surgical
excision | Clear | Nil | 30 | No |
|
|
|
| 52 | Left labium
majus | Surgical
excision | Clear | Nil | 24 | No |
|
|
|
| 59 | Left labium
majus | Surgical
excision | Clear | Nil | 24 | No |
| Dotlic et al
(9) | 2013 | 2 | 52 | Left labium
majus | Surgical
excision | Not mentioned | Repeated surgery due
to recurrence and 7 cycles chemotherapy | 12 | Yes - local and 12
months following diagnosis lung metastasis causing death |
|
|
|
| 52 | Left vulva | Surgical
excision | Not mentioned | Not mentioned | Not mentioned |
|
| Villert et al
(10) | 2015 | 1 | 32 | Labia majora | Surgical
excision | Not mentioned | Intraoperative
radiotherapy | 12 | 5/12 post-op inguinal
node treatment: excision/radiotherapy |
| Present case | 2018 | 1 | 42 | Right labium
majus | Surgical
excision | Close surgical deep
resection margin | Radiotherapy | 60 | No |
Histologically, these tumours are described as
having a multinodular architecture with mucoid material and foci of
haemorrhage, so that they may be initially misdiagnosed as
organised haematomas (10).
Misdiagnosis is common (8) and
preoperative diagnosis is very difficult due to the rarity of this
tumour and its presentation as a slow-growing painless lump
(6). Identifying reciprocal
translocation of t(9;22) (q22-31;q11-12) on immunohistochemistry
has characterized these tumours as a class distinct from skeletal
myxoid chondrosarcoma and aids in their diagnosis (11).
EMCs tend to be relatively chemotherapy-resistant
and, therefore, the first-line treatment is surgical resection with
adjuvant radiotherapy. Evidence suggests EMC has a high propensity
for metastasis, mainly to the lungs, lymph nodes or bone,
particularly if further characterised as high-grade, disproving
earlier beliefs that it was associated with good prognosis. The
estimated progression-free survival rates at 3, 4, 6 and 9 months
were 69, 65, 40 and 26%, respectively (12). There are limited long-term follow-up
and survival data on these patients, and even fewer on tumours
affecting the female genital tract. The survival at 5, 10 and 15
years has been reported to be 82, 65 and 58%, respectively, for
patients with EMC, irrespective of the site (12).
The aim of the present study was to present a case
of vulval EMC to add to the currently limited scientific knowledge
on this rare condition.
Case report
In 2011, a 42-year-old Caucasian woman presented
with a swelling on the right labium majus, which was initially
considered to be a Bartholin gland/duct cyst and was managed
conservatively. The patient was reviewed 7 months later and
underwent drainage and marsupialization under general anaesthesia,
resulting in extensive bruising of the vulva. The patient was
managed medically with antibiotics and non-steroidal
anti-inflammatory medication, and her condition resolved after 3
weeks. Six months later, the patient presented with another vulval
mass at the site of the previous excision and underwent exploration
and biopsy under anaesthesia. The results revealed a myxoid tumour,
potentially of sarcoid origin. A computed tomography (CT) scan of
the abdomen and pelvis did not demonstrate any evidence of
metastasis. The case was discussed at a multidisciplinary tumour
board to plan further management. The patient was referred to a
subspecialist surgeon in Gynaecological Oncology for surgical
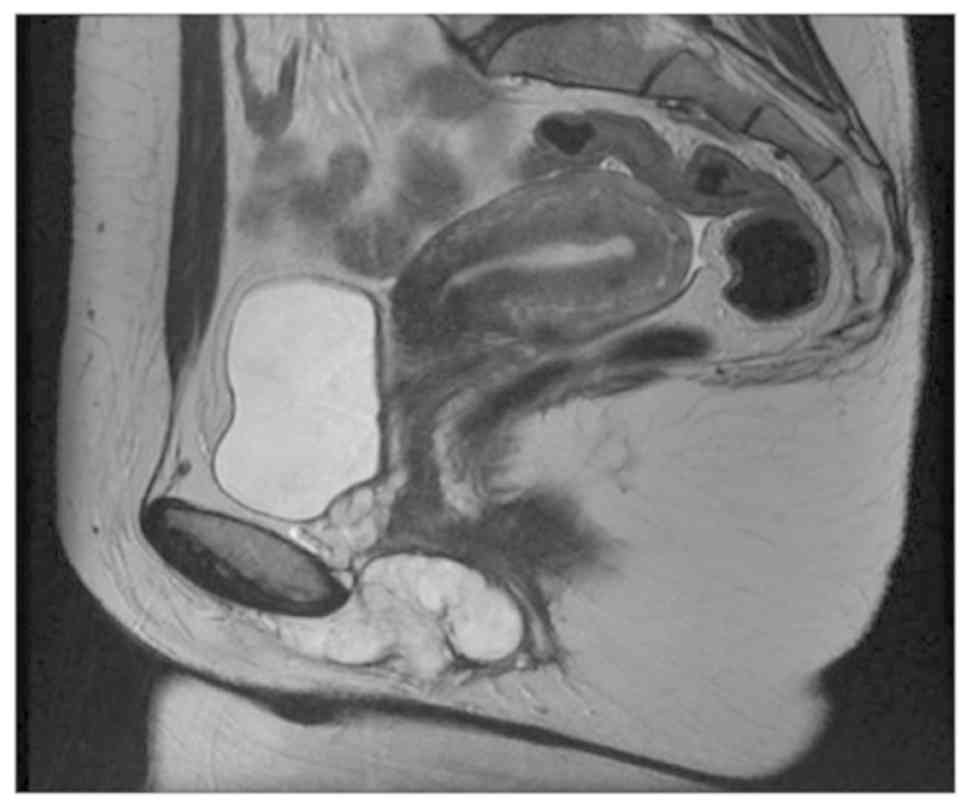
excision. A planned magnetic resonance imaging (MRI) angiogram was
performed to assess the extent and vascularity of the tumour. The
T2-weighted sagittal images showed a well-defined lobulated
high-signal mass with a low-signal capsule and an internal high
signal, similar to that of the bladder (Fig. 1).
Intraoperatively, a 7×5-cm lobulated, vascular
vulval mass was detected in the right labium majus. The tumour was
firmly adherent to the periosteum of the inferior pubic ramus. A
satisfactory resection of the tumour (including the periosteum) was
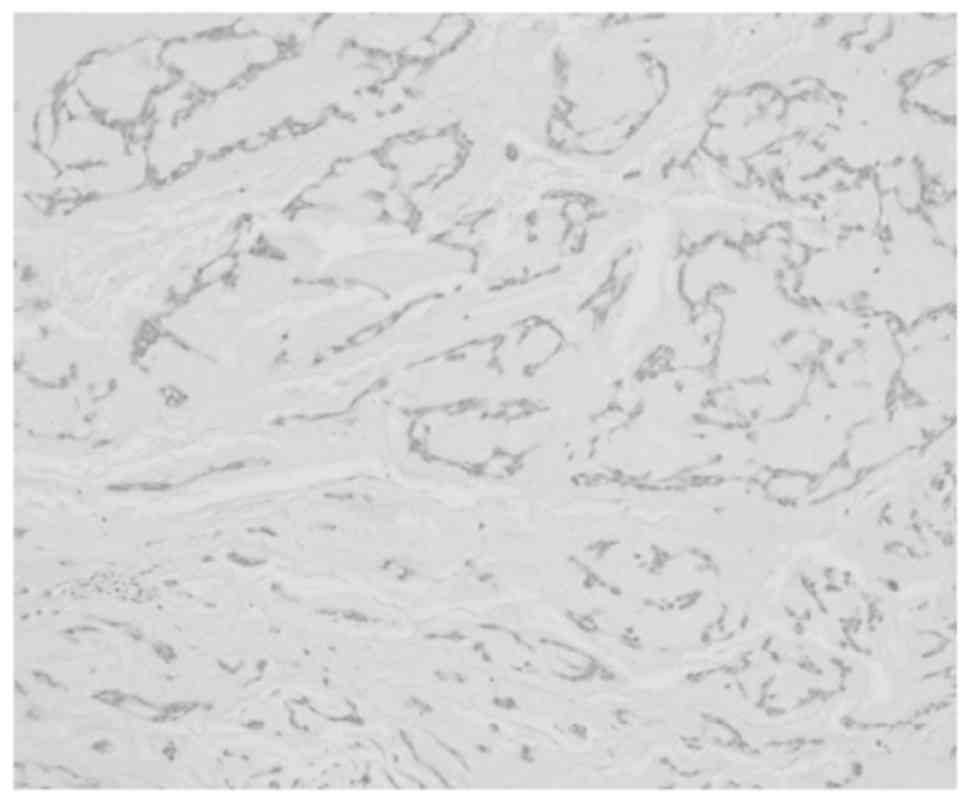
performed, with no macroscopic residual disease. Histological
examination revealed a soft tissue mass, sized 70×50×45 mm,
composed of myxoid tissue arranged in lobules with fibrous septa.
Examination under high-power magnification (×40) revealed
cord/lace-like arrangement of small rounded and spindle cells in a
myxoid-rich matrix. There was a close microscopic deep excision
margin, limited by the periosteum (Fig.
2).
Immunostaining revealed strong positivity for
vimentin; however, S-100, oestrogen receptor (ER), desmin and
smooth muscle actin were negative. FISH analysis for Ewing's
sarcoma and FUS gene (implicated in myxoid liposarcoma and
fibromyxoid sarcoma) revealed that both genes were intact. The
final histological diagnosis was low-grade EMC.
The patient's condition was further discussed at the
central and regional multi-disciplinary team meetings, and it was
recommended that she received adjuvant external-beam pelvic
radiotherapy (45 Gy in 25 sessions) due to the close deep resection
margins. A postoperative MRI demonstrated no evidence of residual
tumour. The surveillance follow-up included 6-monthly clinical
examinations and yearly CT scans. The patient remains asymptomatic
and with no evidence of recurrent disease 60 months following her
initial treatment. The last clinical follow up was 10 November
2018.
Discussion
Upon reviewing the existing literature, most cases
of vulval EMC usually present as painless, smooth, ‘globular’
mobile masses affecting the labia majora. They do not appear to
have a predilection for a specific age or menopausal status. Most
cases were treated by complete surgical resection with adequate
margins. The present case differs, as the mass was firmly adherent
to the periosteum of the inferior pubic ramus, rendering complete
surgical excision challenging and potentially debilitating. The
tumour was resected to the periosteum and the patient was offered
adjuvant radiotherapy postoperatively. The diagnosis of EMC may be
confirmed through immunohistochemical staining for vimentin,
neuron-specific enolase, S-100 protein and mucicarmine, as
described in previous cases. The present case exhibited strong
staining for vimentin. The opinion of the histopathology team was
that the negative genetic tests could be due to the extraskeletal
location of the tumour. Whilst the molecular studies performed in
this case were not suggestive of EMC, the histological appearance
and staining were consistent, confirming the diagnosis.
The decision to offer adjuvant radiotherapy was
considered as an acceptable option, as the patient was a young
woman and radical excision with microscopic clear margins could not
be guaranteed.
To the best of our knowledge, this is the longest
follow-up (60 months) of a patient with confirmed EMC in the
literature to date, and demonstrates that surgical resection with
adjuvant radiotherapy can achieve long-term remission. However,
more cases are required to assess the need for adjuvant therapy and
the required length of follow-up to detect recurrence. The
possibility of an EMC should be included in the differential
diagnosis of women presenting with a smooth, soft and vascular
vulval mass, and surgical excision with histological assessment is
advised to avoid misdiagnosis.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors contributions
AEG was involved in the conception of the study. HA
and MM were involved in the diagnosis of the patient. MEG was
involved in the literature review and writing of the article. DON
was involved in the literature review and writing of the article.
All the authors have read and approved the final version of this
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Verbal consent has been obtained for publication of
the case and associated photographs from the patient.
Competing interests
The authors declare that they have no financial
interests or industrial affiliations to disclose.
References
|
1
|
Cancer Research UK. Vulval cancer
statistics, . http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/vulval-cancerSep
14–2018
|
|
2
|
Salehin D, Haugk C, William M, Hemmerlein
B, Thill M, Diedrich K and Friedrich M: Leiomyosarcoma of the
vulva. Eur J Gynaecol Oncol. 33:306–308. 2012.PubMed/NCBI
|
|
3
|
Chokoeva AA, Tchernev G, Cardoso JC,
Patterson JW, Dechev I, Valkanov S, Zanardelli M, Lotti T and
Wollina U: Vulvar sarcomas: Short guideline for histopathological
recognition and clinical management. Part 2. Int J Immunopathol
Pharmacol. 28:178–186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Enzinger FM and Shiraki M: Extraskeletal
myxoid chondrosarcoma. An analysis of 34 cases. Hum Pathol.
3:421–435. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Santacruz MR, Proctor L, Thomas DB and
Gehrig PA: Extraskeletal myxoid chondrosarcoma: A report of a
gynecologic case. Gynecol Oncol. 98:498–501. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Khan AS, Bakhshi GD, Shaikh A, Khan AA,
Khan AA and Chitale A: Extraskeletal chondrosarcoma of labium
majus. Case Rep Pathol. 2011:4295622011.PubMed/NCBI
|
|
7
|
Sawada M, Tochigi N, Sasajima Y, Hasegawa
T, Kasamatsu T and Kitawaki J: Primary extraskeletal myxoid
chondrosarcoma of the vulva. J Obstet Gynaecol Res. 37:1706–1710.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jeh EA, Lee YJ, Kim HY, Kim A and Lee JH:
Primary extraskeletal mesenchymal chondrosarcoma of the vulva.
Obstet Gynecol Sci. 56:345–348. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dotlic S, Gatalica Z, Wen W, Ghazalpour A,
Mangham C, Babic D, Zekan J and Vranic S: Extraskeletal myxoid
chondrosarcoma of the vulva with PLAG1 gene activation: Molecular
genetic characterization of 2 cases. Appl Immunohistochem Mol
Morphol. 22:537–542. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Villert A, Kolomiets L, Vasilyev N,
Perelmuter V and Savenkova O: Extraskeletal myxoid chondrosarcoma
of the vulva: A case report. Oncol Lett. 10:2095–2099. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Antonescu CR, Argani P, Erlandson RA,
Healey JH, Ladanyi M and Huvos AG: Skeletal and extraskeletal
myxoid chondrosarcoma: A comparative clinicopathologic,
ultrastructural, and molecular study. Cancer. 83:1504–1521. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Drilon AD, Popat S, Bhuchar G, D'Adamo DR,
Keohan ML, Fisher C, Antonescu CR, Singer S, Brennan MF, Judson I,
et al: Extraskeletal myxoid chondrosarcoma: A retrospective review
from 2 referral centers emphasizing long-term outcomes with surgery
and chemotherapy. Cancer. 113:3364–3371. 2008. View Article : Google Scholar : PubMed/NCBI
|