Introduction
Dermatomyositis (DM) represents an idiopathic
inflammatory connective tissue disease, characterized by
inflammation of the muscles and the skin. The skin manifestations
include a heliotrope rash (blue-purple discoloration) of the upper
eyelids, red patches on the face and upper trunk, Gottron's papules
and a raised scaly eruption of the knuckles (1). The first case of DM associated with
gastric cancer was reported by Stertz in 1916 (2). A number of studies have been conducted
to investigate the association between DM and malignancy.
Approximately 10–25% of DM cases are associated with various
malignancies and are classed as paraneoplastic syndromes (1). We herein report the case of a patient
with small-cell lung cancer accompanied by paraneoplastic DM.
Case report
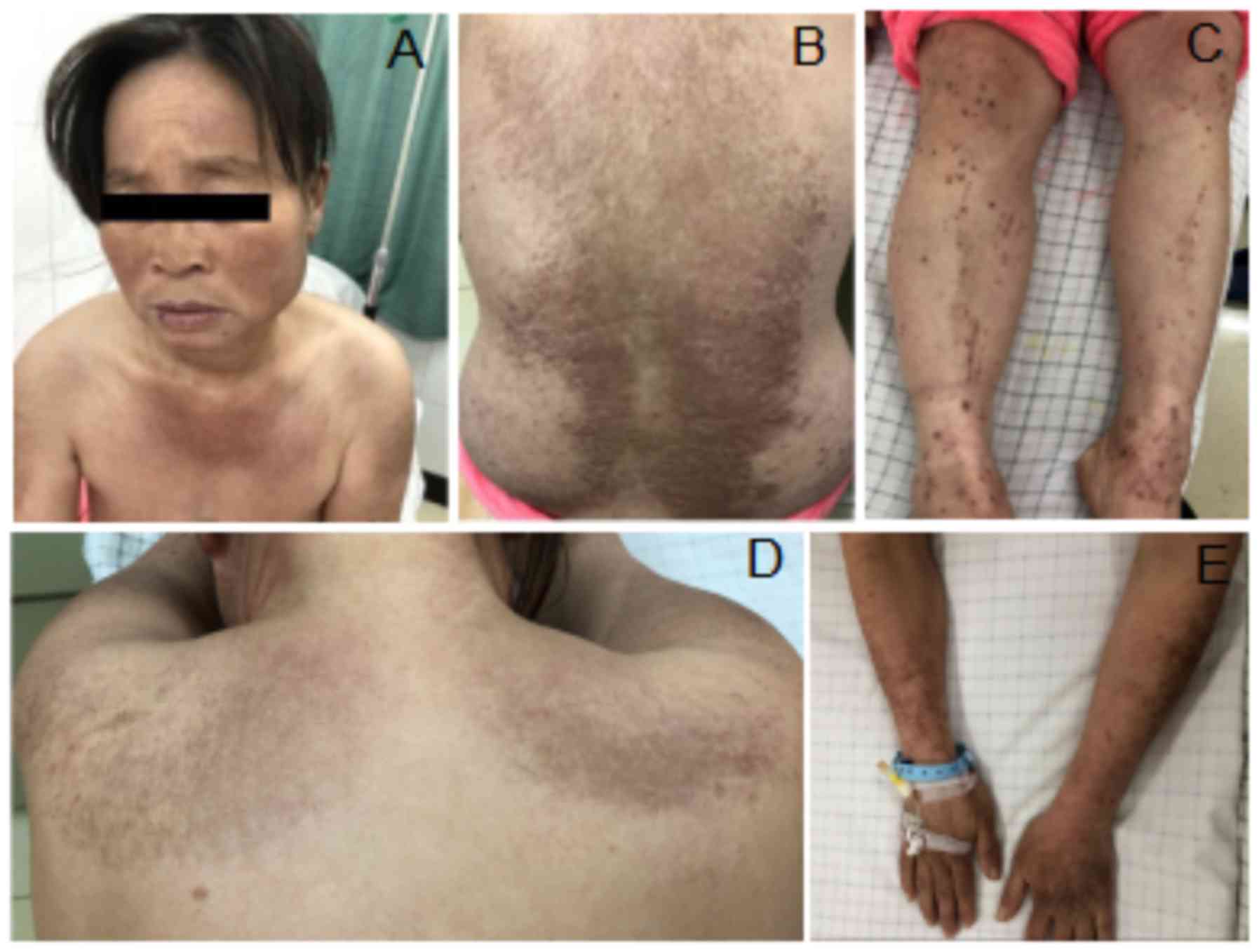
The patient was a 48-year-old woman without a
history of smoking or drinking, who developed symmetrical erythema
and numerous papules on the cheeks, chest and back, without an
obvious inducing factor. The skin lesions were accompanied by
intense pruritus. The patient was diagnosed with eczema at a local
hospital, but no significant improvement was observed after
antiallergic treatment with oral levcetirizine for 1 month. There
was progressive chest tightness, asthma, heart palpitations and
enlargement of the skin lesions. Extensive erythema was observed on
the trunk and limbs. Skin erythema and papules were also observed
on the dorsum of the hands and extensor surfaces of the knuckles.
The patient also exhibited symmetrical progressive weakness of both
upper and lower (muscle strength was assessed as level 4),
characterized by difficulty in lifting the upper limb, a small
angle (<90°) between the abducted arms and the trunk, difficulty
in standing up after crouching, and symmetric involvement of the
limbs (Fig. 1). In addition, the
patient developed cough and aggravation of the chest congestion,
asthma and dyspnea. The patient was admitted to the Department of
Dermatology of the First Affiliated Hospital of Bengbu Medical
College (Bengbu, China) on February 19, 2018. The results of
electromyography (EMG) revealed normal motor nerve conduction
velocity (MCV) and sensory nerve conduction velocity of the right
median, bilateral ulnar, right peroneal and right tibial nerves.
Positive sharp waves were observed in the left and right anterior
tibialis muscles and the right deltoid muscle. Spontaneous
potentials were observed when the muscles were at rest. The
amplitude of the motor units was normal, but the duration was
shortened. The conclusion of the MCV assessment was myogenic
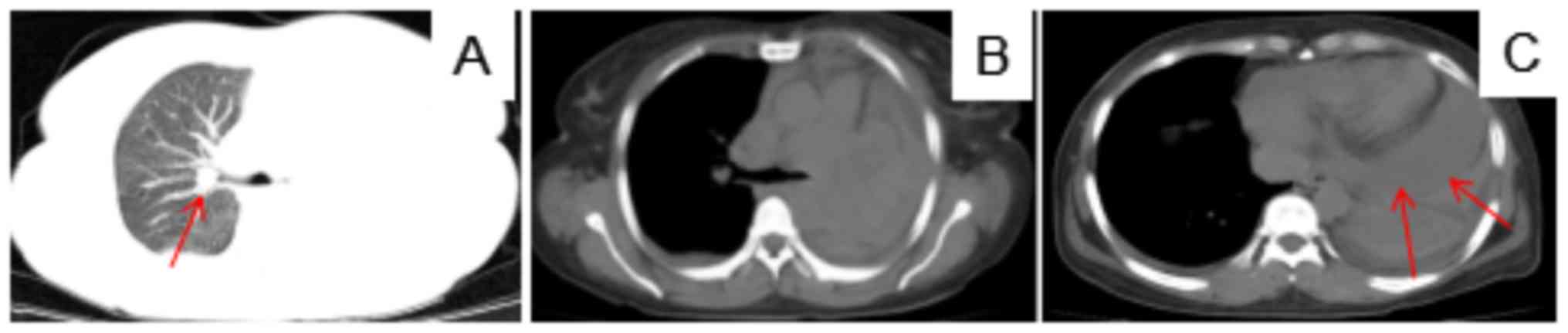
damages. A computed tomography (CT) scan of the chest showed a
space-occupying lesion, bilateral pleural effusion and
hydropericardium in the left lung (Fig.
2). Ultrasound-guided pericardial puncture and exfoliative
cytological examination were performed. Malignant cells were
identified, resembling a poorly differentiated carcinoma. Lung
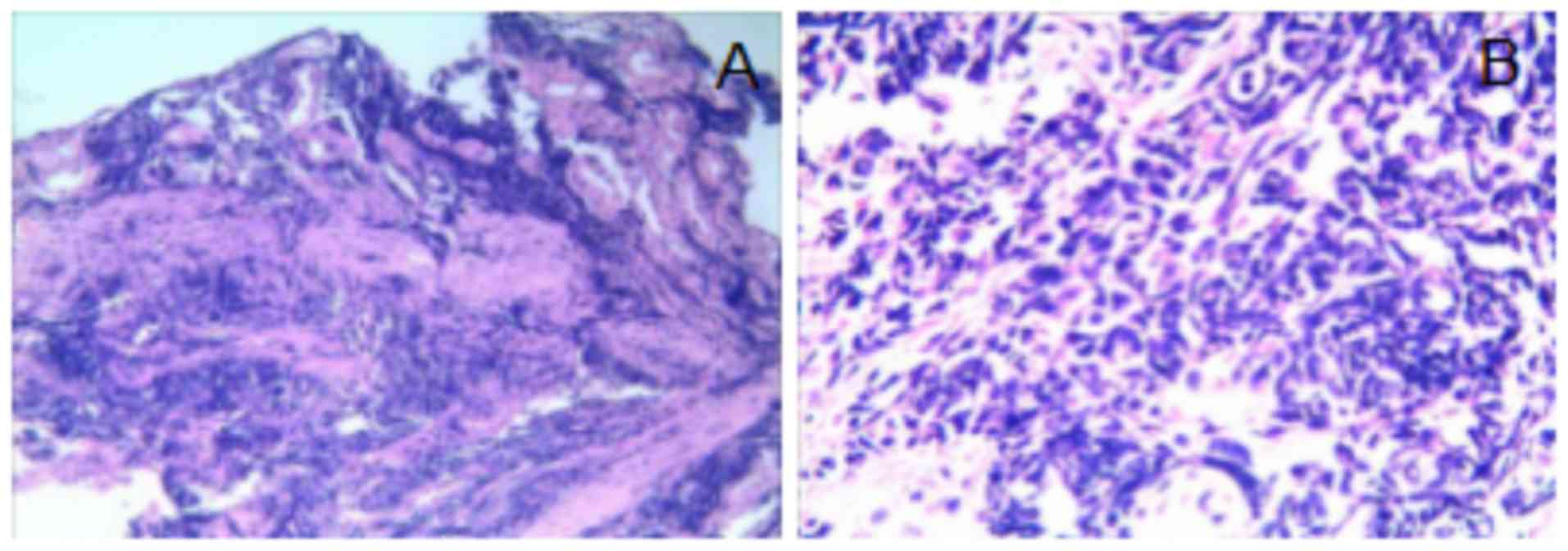
biopsy under ultrasonographic guidance was also performed and the
results of the pathological examination revealed small-cell lung
cancer (Fig. 3). The results of the
laboratory examinations were as follows: Lactate dehydrogenase 915
U/l (reference value: 313–618 U/l), erythrocyte sedimentation rate
(ESR) 34 mm/h (reference value: 0–20 mm/h), creatine kinase (CK)
846 U/l (reference value: 40–200 U/l), CK MB isoenzyme, 31 U/l
(reference value: 0–25 U/l) and blood calcium 2.0 mmol/l (reference
value: 2.11–2.52 mmol/l). Taking into consideration the patient's
history, symptoms, signs and the results of the physical and
laboratory examinations, the patient was diagnosed with small-cell
lung cancer with bilateral pleural and pericardial effusion and DM
(TxNxM1 stage IV). Glucocorticoids (80 mg) were administered to
treat DM for 5 days, and treatment with etoposide 100 mg d1-5+
cisplatin 30 mg d1-4 (EP regimen) was initiated on March 2, 2018.
After one course of chemotherapy, there were no obvious
gastrointestinal adverse reactions or bone marrow suppression. The
patient then received the second cycle of chemotherapy. However, on
March 19, 2018, the patient became unconscious while hospitalized
and her family members requested treatment discontinuation. The
patient was discharged from the hospital and succumbed to
respiratory failure on March 22, 2018.
Discussion
DM is an autoimmune disease characterized by
inflammatory changes involving the muscle and skin, manifesting as
proximal muscle weakness and characteristic skin rashes. The
clinical manifestations of DM do not differ between patients with
and those without concurrent malignancies (1). The incidence of DM is ~1/100,000
(3) and it may occur at any age,
although its incidence is high among adults aged >45 years. DM
in children is not associated with malignancies (1). The diagnosis of DM is mainly based on
the diagnostic criteria proposed by Bohan and Peter in 1975
(3): i) Asymmetrical progressive
muscle weakness in the lower and upper limbs, with or without
dysphagia or dyspnea; ii) myositis confirmed by muscle biopsy; iii)
increased serum creatine kinase levels; iv) abnormal EMG
manifesting as primary muscle injury; v) characteristic skin
lesions. Our patient was diagnosed with DM based of the
abovementioned criteria (i and iii-v). Among all adult DM patients,
10–25% develop DM as a paraneoplastic syndrome, which may be
associated with various malignancies. The studies of De Souza and
Shinjo (4) demonstrated that cancer
prevalence may be as high as 8.6% among newly diagnosed DM
patients, and the incidence of malignancies is the highest within
the first year after the diagnosis of DM. DM-associated
malignancies include breast, ovarian, lung and gastrointestinal
cancers (5). The most common is
adenocarcinoma, accounting for ~70% of all tumors in DM and
polymyositis (PM) patients (5).
Combined with the diagnostic criteria confirming DM and the
histopathological results of the lung biopsy, our patient was
diagnosed with small-cell lung cancer with bilateral pleural and
pericardial effusion and DM (TxNxM1 stage IV).
Paraneoplastic syndromes, which are caused by
tumor-secreted substances, abnormal immune responses, or other
unknown causes, can affect most systems and organs, including the
endocrine, nervous, digestive and hematopoietic systems, joints,
kidneys and skin, with corresponding clinical manifestations. These
manifestations are not related to the invasion and metastasis of
primary tumors, and usually result from tumor-produced functional
polypeptides, hormones and cytokines, or by the immune
cross-reaction between tumors and normal host tissues (6). Paraneoplastic syndromes are a group of
non-metastatic systemic diseases associated with malignancies and
they occur in 7–15% of cancer patients, affecting multiple organs
of the entire body (7). In the
majority of the cases, paraneoplastic syndromes are the first or
most prominent manifestation of the underlying malignancy, and they
may present prior to the diagnosis of the tumor with a mean
interval of 2–12 months (8).
Paraneoplastic syndromes are associated with a
variety of malignancies, the most common of which is lung cancer
(9). Approximately 10% of lung
cancer patients develop paraneoplastic syndromes, and different
histological types of lung cancer are associated with different
paraneoplastic syndromes (9).
Humoral hypercalcemia of malignancy in squamous cell carcinoma and
syndrome of inappropriate antidiuretic hormone secretion in
small-cell lung cancer are the two most common types. The most
common type of DM-related lung cancer is small-cell lung cancer
(29%), followed by squamous cell carcinoma (21%) and adenocarcinoma
(8%) (5). The severity of the
symptoms is not related to the size of the primary tumor and, in
the majority of the cases, paraneoplastic syndromes are present
before cancer diagnosis (7). The
patient in the present case was diagnosed with small-cell lung
cancer. Sparsa et al (10)
studied 40 patients with DM and PM and found that the following
clinical characteristics may be associated with malignancies:
Systemic symptoms, no Raynaud's phenomenon, rapid onset of
myositis, elevated ESR and CK levels. The systemic symptoms were
obvious, the ESR and CK levels were both higher than normal and
there was no Raynaud's phenomenon in our patient, consistently with
the abovementioned criteria. Therefore, the patient was considered
likely to have an underlying malignancy. Basset-Seguin et al
(11) reported that the 3-year
survival rate of DM patients was 57%, while the 2-year survival
rate of DM patients with cancer was 25%. For most paraneoplastic
syndromes, the best treatment is to treat the underlying
malignancy. Glucocorticoids are the main drugs used in the
treatment of DM, but other immunomodulatory treatments for
paraneoplastic DM are also needed (12). The muscular symptoms can be improved
with treatment targeting the tumor, but the skin involvement, which
is often difficult to treat, may persist (13). Good treatment outcomes may be
achieved by using corticosteroids and a variety of non-steroid
drugs, including methotrexate, antimalarial drugs, mycophenolate,
azathioprine and cyclosporine. Immunoglobulins, rituximab and tumor
necrosis factor-α inhibitors are beneficial for patients with drug
resistance (13,14). For patients diagnosed with DM,
additional evaluation is recommended, including whole-blood cell
count, metabolic function examination, urine and hematological
examination, chest and abdominal CT scan, among others. For female
patients, additional examinations should include breast
examination, pelvic CT scan and gynecological examination (5). The patient was misdiagnosed with only
DM, since only skin manifestations were present at the early stages
of the disease. No chest or abdominal CT examination was performed
to rule out other systemic diseases. The patient only received
treatment targeting DM at the local hospital; she developed chest
congestion and palpitations when transferred to our hospital, which
were considered to be the result of pericardial effusion. At that
time, the patient had terminal cancer with distant metastasis. She
succumbed to the disease within 1 month after being diagnosed with
small-cell lung cancer.
The clinical characteristics of DM concurrently with
lung cancer may be non-specific and easy to overlook. The patient
presented only with skin manifestations at the early stages. As a
result, lung cancer was discovered at a late stage. The treatment
efficacy and prognosis are very poor. At present, the main
challenge in treating cancer-associated PM or DM is timely
identification of the underlying malignancies. Extensive
examination should be performed in DM and PM patients to eliminate
the possibility of malignancy, particularly for patients aged
>40 years. This case stresses the fact that early diagnosis and
timely treatment are crucial for patient prognosis, and the
diagnosis of DM should always be considered as an early warning
sign of malignancy.
Acknowledgements
Not applicable.
Funding
The present study was supported by funding from the
National Natural Sciences Foundation of China (grant no. 81702450),
the Natural Science Research major Project of Education Office of
Anhui Province (grant no. KJ2016SD40) and Support Program for
Outstanding Young Talents in Colleges and Universities of Anhui
Province (grant no. gxyq2018038).
Availability of data and materials
Not applicable.
Authors' contributions
FS provided the case, formulated the therapeutic
regimen and revised the manuscript. ZW and RW aided in patient
management. YL collected the imaging data. TZ collected clinical
data and wrote the manuscript. QW and SQ performed the analyses
with constructive discussions. All the authors have read and
approved the final version of this manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Informed consent for publication was obtained from
the family member of the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Silva JA, Mesquita Kde C, Igreja AC, Lucas
IC, Freitas AF, Oliveira SM, Costa IM and Campbell IT:
Paraneoplastic cutaneous manifestations: Concepts and updates. An
Bras Dermatol. 88:9–22. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sterz G: Polymyositis. Berliner Klinische
Wochenschrift. 53:4891916.
|
|
3
|
Zhang X, Wang Y, Ma G, Zhang L, Jing H and
Du J: Dermatomyositis as a symptom of primary lung cancer: A case
report and review of the literature. Oncol Lett. 11:3413–3416.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Souza FH and Shinjo SK: Newly diagnosed
dermatomyositis in the elderly as predictor of malignancy. Rev Bras
Reumatol. 52:713–721. 2012.(In English, Portuguese).
|
|
5
|
Zahr ZA and Baer AN: Malignancy in
myositis. Curr Rheumatol Rep. 13:208–215. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miret M, Horváth-Puhó E, Déruaz-Luyet A,
Sørensen HT and Ehrenstein V: Potential paraneoplastic syndromes
and selected autoimmune conditions in patients with non-small cell
lung cancer and small cell lung cancer: A population-based cohort
study. PLoS One. 12:e01815642017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Porto L, Miranda M, Gomes A, André R and
Rodrigues B: Paraneoplastic neurological syndrome as an initial
indicator of small cell carcinoma of the lung. BMJ Case Rep.
2013:bcr20120084322013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Santacroce L: Paraneoplastic syndromes.
Drugs & Diseases. 2017, https://emedicine.medscape.com/article/280744-overviewUpdated
December 06 2018.
|
|
9
|
Kanaji N, Watanabe N, Kita N, Bandoh S,
Tadokoro A, Ishii T, Dobashi H and Matsunaga T: Paraneoplastic
syndromes associated with lung cancer. World J Clin Oncol.
5:197–223. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sparsa A, Liozon E, Herrmann F, Ly K,
Lebrun V, Soria P, Loustaud-Ratti V, Bouyssou-Gauthier ML,
Boulinguez S, Bédane C, et al: Routine vs extensive malignancy
search for adult dermatomyositis and polymyositis: A study of 40
patients. Arch Dermatol. 138:885–890. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Basset-Seguin N, Roujeau JC, Gherardi R,
Guillaume JC, Revuz J and Touraine R: Prognostic factors and
predictive signs of malignancy in adult dermatomyositis. A study of
32 cases. Arch Dermatol. 126:633–637. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pelosof LC and Gerber DE: Paraneoplastic
syndromes: An approach to diagnosis and treatment. Mayo Clin Proc.
85:838–854. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Iorizzo LJ III and Jorizzo JL: The
treatment and prognosis of dermatomyositis: An updated review. J Am
Acad Dermatol. 59:99–112. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kovacs SO and Kovacs SC: Dermatomyositis.
J Am Acad Dermatol. 39:899–920. 1998. View Article : Google Scholar : PubMed/NCBI
|