1. Introduction
Current treatment assessment
algorithms
Definitive chemoradiation (CRT) is a standard
treatment for locally-advanced human papillomavirus
(HPV)-associated oropharyngeal squamous cell carcinoma (OPSCC). The
response to treatment is assessed with both clinical and
radiographic information. In patients without evidence of primary
or nodal disease on clinical examination, surveillance imaging is
often performed with a 12-week FDG-PET/CT. Both lymph node size and
intensity of FDG uptake are used to assess the likelihood of
residual disease in the neck and guide the decision to either
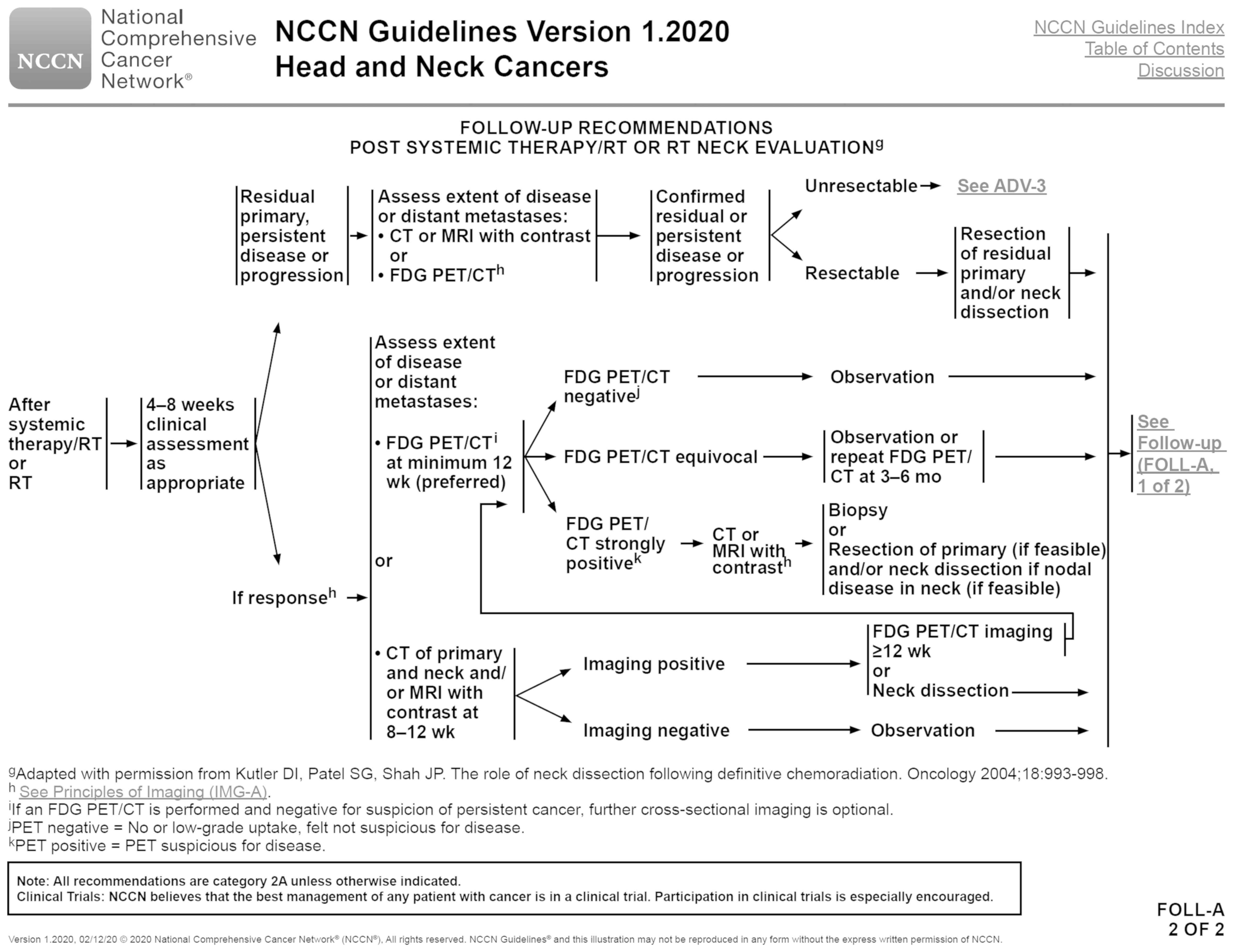
observe patients or proceed with neck dissection. Both NCCN and
UpToDate have published algorithms to assist clinicians with this
process (1,2). NCCN recommends observation for
negative scans, observation or repeat PET/CT at 3-6 months for
equivocal scans, and CT or MRI followed by neck dissection for
positive scans (Fig. 1). Negative
scans are defined by no or low-grade uptake and positive scans are
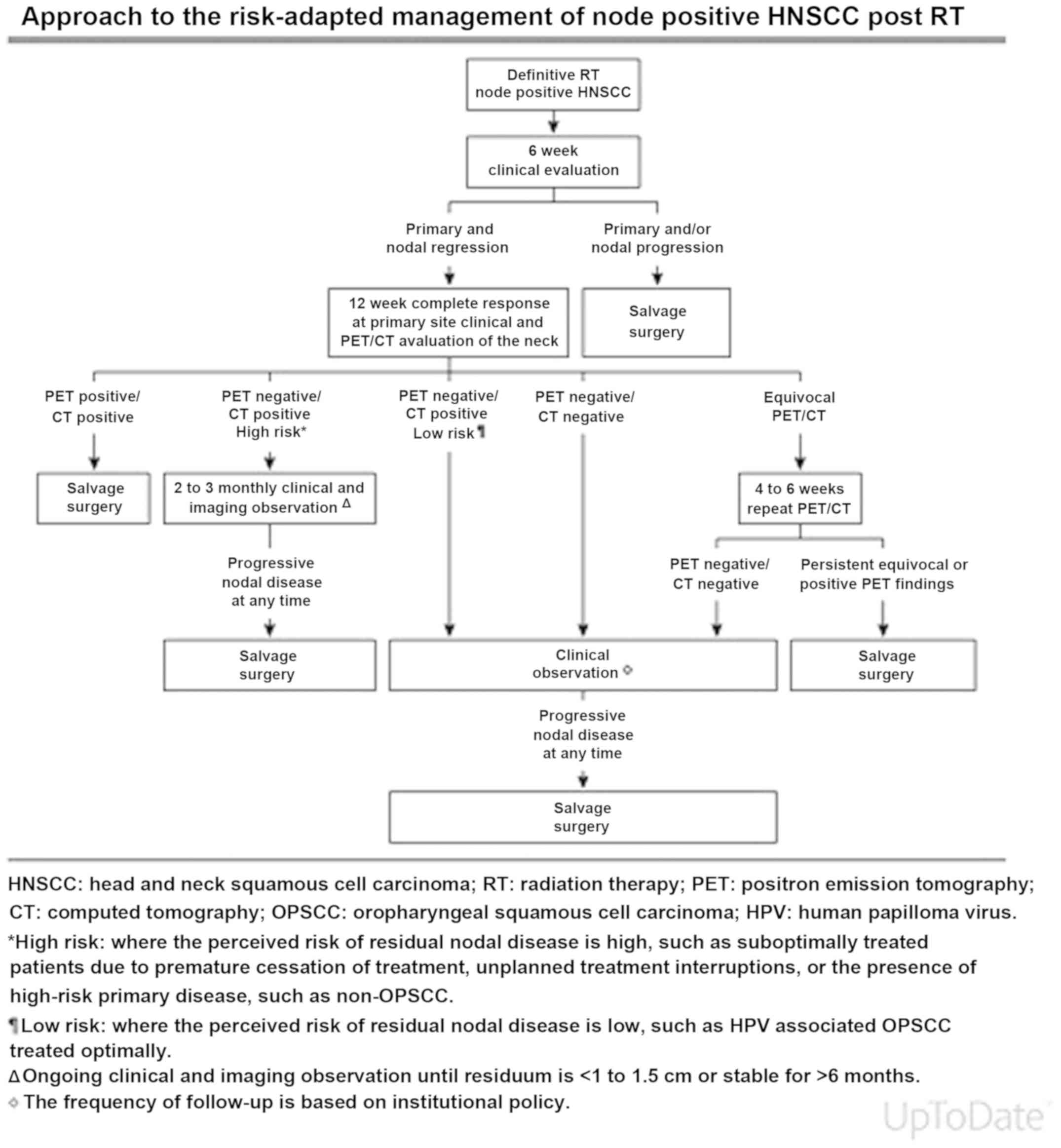
defined as suspicious for disease. According to UpToDate (Fig. 2), there are five different options
depending on imaging and clinical factors. It is recommended that
patients undergo salvage surgery for PET positive/CT positive scans
and clinical observation for PET negative/CT negative scans. If a
patient has a PET negative and CT positive result, 2-3 monthly
clinical and radiographic observation is recommended for high-risk
patients, while clinical observation is suggested for low-risk
individuals, including those with HPV-associated OPSCC. Finally, a
repeat PET/CT at 4-6 weeks is recommended for those with equivocal
findings.
Low positive predictive value of
12-week PET/CT
Although these surveillance strategies have been
shown to promote excellent oncologic control, replacing the policy
of planned neck dissections, they may not be broadly applicable to
all head and neck cancers (3-7).
In HPV-associated OPSCC, the reported positive predictive value
(PPV) of 12-week post-therapy PET/CT is low (8-11),
likely secondary to the lower pre-test probability of residual
nodal disease (12). In a
retrospective chart review of 233 patients with HPV-associated
OPSCC, Corpman et al found that post-treatment PET/CT had a
PPV of 13.4% and led to 60 additional imaging studies, 23
additional biopsies, and meaningful salvage therapy in only 3
patients (1.6%) (13). One of the
primary limitations of using PET/CT is the lack of a standardized
response criteria for HPV-associated disease. It has become
increasingly clear that this disease entity has unique radiographic
features, including a longer time to complete lymph node involution
(14). This finding has been
incorporated into the UpToDate algorithm, which recommends that CT
positive/PET negative scans be managed with clinical observation in
HPV-associated OPSCC. However, there is currently no effective
strategy to manage lymph nodes with residual FDG avidity. Current
algorithms guide decision-making by dividing responses into
positive and equivocal groups. However, this approach may not be
appropriate in HPV-associated disease. In a study of 79 patients
with HPV-associated OPSCC on a de-intensification trial, Wang et
al demonstrated a low PPV for PET/CT when responses were
categorized as equivocal/incomplete or incomplete (9 and 13%,
respectively) (9). The authors used
the Mehanna et al trial definitions for nodal response
(3), which defined an incomplete
response as ‘intense FDG uptake at 12 weeks after
chemoradiotherapy, with or without enlarged lymph nodes,’ and
equivocal response as ‘mild or no FDG uptake in enlarged nodes or
mild FDG uptake in normal-sized nodes.’
Limitations of Post-CRT fine-needle
aspiration
While FNA has central importance in the initial
workup of head and neck cancers, the utility of post-CRT FNA in
detecting persistent neck disease is limited. The accuracy of
post-CRT FNA in head and neck cancer has been questioned given the
difficulty in interpreting the viability of irradiated cancer
cells. In a series of 540 patients with cancers of the oral cavity,
oropharynx, hypopharynx, and larynx, van der Van der Putten et
al found that post-CRT FNA had a specificity of 42% in patients
with advanced disease; only 50% of patients with positive cytology
had viable disease on neck dissection pathology (15). On the other hand, in a pilot study
of 14 patients undergoing FNA before planned neck dissection for
persistent lymphadenopathy on imaging, Fleischman et al
found that the diagnostic accuracy of FNA was 88% at detecting
residual head and neck cancer (16). The authors suggested that FNA may be
a feasible ancillary diagnostic modality. In truth, the diagnostic
performance of post-CRT FNA has not been studied in HPV-associated
OPSCC, indicating that future research is needed before clinicians
can rely on this modality to reconcile concerning PET/CT
findings.
Aims of this article
Given these important shortcomings in post-CRT
treatment assessment in patients with HPV-associated OPSCC,
physicians are limited in appropriately selecting patients for
consolidative neck dissection, which results in over-treatment.
This consideration is especially important for patients with
HPV-associated disease, a population with a favorable prognosis.
Post-CRT neck dissection has important implications on long-term
quality of life as it is associated with a higher rate of
post-operative complications (17).
Therefore, a literature review was performed with the PubMed
Database to investigate potential strategies for improvement of
post-CRT treatment assessment of the neck in patients with
HPV-associated OPSCC.
2. Strategies to improve post-CRT neck
assessment
The existing literature highlights several potential
strategies to improve post-CRT neck assessment in patients with
HPV-associated OPSCC (Table I),
including continued surveillance with PET/CT, delayed timing of
restaging PET/CT, initial assessment with multimodality or
alternative imaging, and detection of circulating HPV DNA.
 | Table ISummary of the literature. |
Table I
Summary of the literature.
| Author, year | Level of
evidence | Year | Country | Number of
subjects | Recommendation for
post-CRT treatment assessment | Rationale | (Refs.) |
|---|
| Liu et al,
2019 | 4 | 2019 | Australia | 235 | Repeat PET/CT at 16
weeks for an incomplete response on 12 week imaging, excluding
those with clinical nodal progression or residual FDG avidity at
the primary or distant disease on initial post-therapy PET/CT. | 16-week PET/CT
reduced the rate of neck dissection from 17 to 2.6% without
impacting subsequent regional control. | (18) |
| Vainshtein et
al, 2014 | 4 | 2014 | USA | 101 | Delay initial
post-therapy PET/CT to 6 months after completion of CRT or reserve
PET/CT for patients with residual disease on CT at 3 months | 6-month PET/CT
demonstrated a false positive rate of only 2% and a false negative
rate of only 17%. | (8) |
| Pellini et al,
2014 | 4 | 2014 | Italy | 36 | 12-week neck
ultrasound with FDG-PET/CT could be an effective strategy to
identify patients with a complete response. A combination of
ultrasound, MRI, and FDG-PET/CT could useful in selecting patients
who require neck dissection. | A combination of
12-week neck ultrasound and FDG-PET/CT had the highest negative
predictive value (93.3%). A combination of US, MRI and FDG-PET/CT
had the highest specificity (100%), accuracy (93.8%) and positive
predictive value (100%). | (22) |
| Yu et al,
2017 | 4 | 2017 | USA | 41 | A single DWI-MRI
could be used to identify residual neck disease after definitive
CRT in patients with oropharyngeal cancer. | Compared to 14-week
PET/CT, 8-week DWI-MRI produced similar sensitivity and better
specificity. Moreover, the PPV was 50% with DWI-MRI and 25% with
PET/CT. | (23) |
| Lee et al,
2017 | 4 | 2017 | UK | 55 | Plasma HPV DNA can
potentially be used to predict response to CRT at both the primary
site and lymph nodes in patients with HPV-associated head and neck
cancers. | Post-treatment HPV
DNA levels in plasma correlated with clinical responses. | (29) |
Continued surveillance with
PET/CT
Numerous publications have promoted the notion of
exercising caution when interpreting 12-week PET/CT results,
adopting a high threshold for immediate neck dissection, and
observing patients with serial imaging (3,9,13). One
study was found that systematically evaluated a surveillance
strategy in patients with HPV-associated OPSCC (18). In a retrospective analysis of a
prospectively collected database, Liu et al assessed the
utility of a repeat PET/CT, instead of immediate neck dissection,
in patients with HPV-associated OPSCC who underwent RT or CRT, and
had an incomplete response on 12-week PET/CT (18). The authors enrolled 235 patients
with non-metastatic disease; 41 patients underwent 16-week imaging
for an incomplete response at 12-weeks, which included both
positive and equivocal responses. A positive response was defined
as focal FDG uptake greater than the liver and corresponding to a
structural abnormality, while an equivocal response was defined as
focal FDG uptake less than the liver, greater than adjacent tissue,
and corresponding to a structural abnormality. Patients were
excluded from undergoing 16-week imaging if they had residual FDG
avidity at the primary or distant site on 12-week PET/CT or if they
had evidence of clinical nodal progression (n=95). Re-evaluation at
a multidisciplinary tumor board was performed for patients with a
persistent incomplete response on 16-week imaging. In their
analysis, the authors found that 16-week PET/CT reduced the rate of
neck dissection from 17 to 2.6% without impacting subsequent
regional control; no regional failures occurred in patients who
underwent neck dissection following a 16-week PET/CT. Moreover, 29
(71%) patients converted to a complete response on 16-week imaging,
only one of which had nodal failure at 49 months post-therapy.
Compared to a PPV of 12% for 12-week PET/CT, the PPV of 16-week
imaging was 33%. Based on these findings, the authors suggested
that a 16-week repeat PET/CT could spare many patients from
unnecessary surgeries.
There are several important considerations
pertaining to this study. Regarding the inclusion criteria, the
authors grouped both positive and equivocal responses as
incomplete, which is appropriate given that both an equivocal and
positive response pose a clinical dilemma. PET/CT scans with
significant FDG avidity may still be false positives in
HPV-associated disease. In regard to the exclusion criteria,
patients did not undergo repeat PET/CT if they had evidence of
clinical nodal progression or had residual FDG avidity at the
primary or a distant site on 12-week PET/CT. These exclusion
criteria are also reasonable given the increased likelihood of
disease in these clinical scenarios. In a retrospective analysis of
146 patients with OPSCC and treated with CRT, Bird et al
found that all patients with residual FDG-uptake at both the
primary site and neck had pathologically confirmed persistent
disease (19), indicating that
these patients may not be appropriate for observation. Finally, it
is important to consider how the authors managed patients with
persistent FDG avidity on 16-week imaging. Eight patients had
stable FDG avidity on 16-week imaging; 4 individuals underwent neck
dissection, all of whom had residual disease, and 4 individuals
were observed and remained free of disease. Four patients had
reduced FDG avidity on 16-week imaging, none of whom had residual
disease. Based on these results, the authors recommended that
patients with persistent and unchanged FDG avidity on 16-week
PET/CT should undergo neck dissection. Given this small number of
patients, it is difficult to comment on the appropriate management
of patients with residual metabolic activity on repeat PET/CT.
Delayed timing of restaging
PET/CT
Delaying the time of restaging PET/CT scan was
proposed in a 2014 publication by Vainshtein et al, who
evaluated the performance of 12-week PET/CT in predicting local and
regional failure after CRT (8). The
authors retrospectively reviewed and re-classified post-therapy
scans in 101 patients with AJCC 7th edition stage III and IV
HPV-associated OPSCC, grouping responses into complete, near
complete, and less than complete. The PPV of 12-week PET/CT was
found to be 33% for detection of nodal disease. Given this low PPV,
the authors also assessed the diagnostic performance of
surveillance PET/CT scans in 67 patients who did not have any
clinical or radiographic suspicion of recurrent disease. The median
time from completion of CRT to first surveillance PET/CT was 7.3
months. All patients (12) with an
incomplete response on restaging PET/CT (near and less than
complete) achieved a complete response on surveillance PET/CT. The
authors reported that surveillance PET/CT had a NPV of 98% and PPV
of 83% for detection of regional recurrence. Based on the superior
operating characteristics of surveillance PET/CT, the authors
suggested that restaging PET/CT could be delayed to 6 months after
completion of CRT.
When considering a delay in restaging PET/CT, it is
necessary to consider the optimal timing since prolonging
assessment could impact patient anxiety, neck dissection
complication rates, type of neck dissection (selective versus
modified versus radical), regional control, and early detection of
distant metastases. In a 2010 retrospective analysis of 105
patients with HNSCC who underwent neck dissection after CRT, Goguen
et al compared the complication rates and survival outcomes
between patients undergoing neck dissection less than 12 weeks
versus greater than 12 weeks after CRT (20). The authors found that the two groups
did not differ in the rate of surgical complications or survival.
This type of analysis has not been performed for patients with
HPV-associated OPSCC. In regards to detection of distant
metastases, some studies indicate that they occur at later time
points in HPV-associated OPSCC (21). Therefore, the role of early PET/CT
for this purpose may not be significant.
Initial assessment with multimodality
or alternative imaging modalities
Several publications have highlighted the use of
ancillary imaging modalities to assist with treatment assessment,
either alone or in combination with PET/CT. In a retrospective
study from 2014, Pellini et al investigated the diagnostic
performance of a 12-week post-CRT neck ultrasound, MRI, and PET/CT
for detection of residual nodal disease (22). The authors prospectively enrolled 36
patients with OPSCC bulky nodal disease (>3 cm) who were treated
with definitive CRT. All patients in the study underwent planned
neck dissection 3 months after treatment; the pathology reports
were used to determine the operating characteristics of the three
imaging modalities. Individuals with less than a complete response
at the primary site were excluded. For response evaluation, lymph
nodes were considered metastatic on ultrasound if they had a ‘short
axis diameter >7 mm and/or round shape (reduction in the ratio
of maximal longitudinal to maximal axial diameter), unclear
boundary or irregular hilar and internal echoes.’ When comparing
each modality alone and in combination, the authors found that neck
ultrasound and PET/CT had the highest NPV (93.3%), while a
combination of neck ultrasound, MRI, and FDG-PET/CT had the highest
PPV (100%). The authors suggested that neck ultrasound with
FDG-PET/CT could be used to identify patients with a complete
response, while a combination of ultrasound, MRI, and FDG-PET/CT
could be useful in selecting patients who require neck dissection.
Of note, the authors did not include information on HPV or p16
status, limiting the applicability of these findings. Moreover, the
cost of obtaining three imaging modalities concurrently is an
important consideration; the authors argued that these health care
expenditures would be offset by a decreased number of unnecessary
surgical procedures. It is critical that further research is
performed to investigate the cost-effectiveness of this
strategy.
Yu et al compared the diagnostic performance
of diffusion-weighted magnetic resonance imaging (DWI-MRI) and
PET/CT for detection of persistent neck disease (23). DWI-MRI is a functional imaging
modality that allows for calculation of an apparent diffusion
coefficient (ADC), which reflects microscopic proton motion; a
lower value is associated with the presence of cancer. The
rationale for this modality is that it can detect persistent
disease earlier as diffusion signals are evident before changes in
tumor size. The authors retrospectively reviewed the records of 41
patients with HPV-associated OPSCC who were treated with definitive
CRT. DWI-MRI and PET/CT were performed at a median time of 8.6 and
14 weeks, respectively. The mean ADC and lymph node volume were
determined for each DWI-MRI; the maximum standardized uptake value
(SUV) was measured for each PET/CT. Using a receiver operating
characteristic (ROC) analysis, the authors calculated a threshold
of 1,500 for ADC and 2.5 for SUVmax. Using these thresholds and the
pathology results of either biopsy or neck dissection, the authors
found that DWI-MRI had a NPV and PPV of 100 and 50%, while PET/CT
had a NPV and PPV of 100 and 25%. Given the earlier and more
specific detection of residual nodal disease with DWI-MRI, the
authors proposed that this imaging modality could be used to
identify residual neck disease after definitive CRT.
This study was not the first to demonstrate the
utility of DWI-MRI in head and neck cancer, but was the only
publication that limited their analysis to HPV-associated OPSCC.
While the higher PPV, equivalent NPV, and earlier time of
acquisition support the use of DWI-MRI, it is important to consider
the fact that surveillance with PET/CT had shown to be noninferior
to planned neck dissection in regards to survival, which may
dissuade clinicians from abandoning PET/CT. Further, although the
PPV of DWI-MRI was shown to be higher than PET/CT, a value of 50%
may still be suboptimal. Another issue is the ability of DWI-MRI to
detect residual disease at the primary site. In a 2017 publication
with 46 patients with advanced OPSCC, Greuter et al reported
a PPV of 60.0% for DWI-MRI (24).
However, less than half of the cohort had HPV-associated disease.
Finally, Yu et al highlighted several important limitations
of their study, including a small sample size and retrospective
design, as well as limitations of DWI-MRI, such as a complex
technique and difficulty in evaluation of cystic nodes (23). Therefore, although DWI-MRI may offer
earlier and more specific detection of residual neck disease, which
could help limit unnecessary neck dissections, this modality also
has limitations.
Detection of circulating HPV DNA
The detection of plasma HPV DNA is an exciting new
development that may prove useful in detection of residual disease
(25-28).
Lee et al assessed the role of circulating HPV DNA in
detection of residual disease after CRT (29). The authors prospectively enrolled 88
patients with locally-advanced head and neck cancers and divided
them into test (55) and validation (33) cohorts. All participants
had HPV-associated disease, determined by p16 immunohistochemistry
(IHC) and E6 RT-PCR, and underwent 12-week PET/CT. Individuals with
residual FDG-avid nodes had a neck dissection and those with
residual uptake at the primary or distant site underwent biopsy.
The authors developed an amplicon-based next generation sequencing
(NGS) assay to detect circulating HPV DNA in serum. They collected
plasma samples at baseline as well as 6 and 12 weeks post-CRT. To
validate the detection assay, the authors compared pre-CRT HPV DNA
levels to both p16 IHC and E6 RT-PCR; they reported a sensitivity
and specificity of 90% and above. Moreover, the authors correlated
post-treatment HPV DNA levels to PET/CT and pathology reports. In
the test cohort, HPV DNA levels were below the threshold of
detection in all patients (23)
with a complete radiological response on 12-week PET/CT. The assay
was positive in the only patient with biopsy-proven persistent
disease. Further, HPV DNA was undetectable in 3 patients who
underwent biopsy at the primary and 1 patient who underwent neck
dissection for increased FDG uptake on 12-week PET/CT; the
pathology was negative in all 4 cases. In the validation cohort,
HPV DNA levels were below the threshold of detection in all 7
patients with a complete radiographic response. Moreover, the assay
was negative in 3 patients who underwent neck dissection for
increased FDG on 12-week PET/CT; no residual disease was found in
any of these patients. Based on these findings, the authors
suggested that plasma HPV DNA could be used to help guide treatment
decisions and avoid unnecessary surgeries, but commented that their
findings require validation in a larger cohort of patients with
longer follow-up. Indeed, the study had a small number of patients
with residual disease and/or recurrence. Moreover, it would be
helpful to compare the utility of this sequencing-based plasma
assay to other methods of HPV detection, such as those that involve
salivary collection or PCR technology.
3. Conclusions and prospects
This literature review highlights several strategies
that have been proposed to improve post-CRT neck assessment in
patients with HPV-associated OPSCC. A repeat PET/CT at 16-weeks for
patients with an incomplete response on 12-week imaging may help
reduce the number of neck dissections without comprising regional
control. Delaying the timing of the initial post-therapy PET/CT may
improve its PPV by allowing for radiation-induced inflammation to
resolve, but the appropriate timing is unknown and has important
clinical implications. DWI-MRI may offer an alternative to PET/CT,
but has its own limitations. Finally, detection of plasma HPV DNA
is an exciting development that may be able to effectively detect
residual disease, but it requires further validation in larger
cohorts. Given the current limitations of post-CRT assessment of
the neck in patients with HPV-associated OPSCC, further
investigation of these strategies will be highly beneficial for
this population.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
MW performed the literature review, wrote the
manuscript and edited the final version. MG, LM, TT, NS, DKa, DF
and DKr reviewed and edited the manuscript. ST reviewed the
published literature, wrote parts of the manuscript, and edited and
approved the final version. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Reproduced with permission from the NCCN
Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for
Head and Neck Cancers V.1.2020. © 2020 National Comprehensive
Cancer Network, Inc. All rights reserved. The NCCN Guidelines® and
illustrations herein may not be reproduced in any form for any
purpose without the express written permission of NCCN. To view the
most recent and complete version of the NCCN Guidelines, go online
to https://www.nccn.org. The NCCN
Guidelines are a work in progress that may be refined as often as
new significant data becomes available. NCCN makes no warranties of
any kind whatsoever regarding their content, use or application and
disclaims any responsibility for their application or use in any
way.
|
|
2
|
Porceddu SV and Weber RS: Management of
the neck following definitive radiotherapy with or without
chemoradiotherapy in head and neck squamous cell carcinoma. Post
TW, ed. UpToDate. Waltham, MA, 2018.
|
|
3
|
Mehanna H, Wong WL, McConkey CC, Rahman
JK, Robinson M, Hartley AG, Nutting C, Powell N, Al-Booz H,
Robinson M, et al: PET-CT surveillance versus neck dissection in
advanced head and neck cancer. N Engl J Med. 374:1444–1454.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Garden AS, Gunn GB, Hessel A, Beadle BM,
Ahmed S, El-Naggar AK, Fuller CD, Byers LA, Phan J, Frank SJ, et
al: Management of the lymph node-positive neck in the patient with
human papillomavirus-associated oropharyngeal cancer. Cancer.
120:3082–3088. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Goenka A, Morris LG, Rao SS, Wolden SL,
Wong RJ, Kraus DH, Ohri N, Setton J, Lok BH, Riaz N, et al:
Long-term regional control in the observed neck following
definitive chemoradiation for node-positive oropharyngeal squamous
cell cancer. Int J Cancer. 133:1214–1221. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Koshkareva Y, Branstetter BF, Gaughan JP
and Ferris RL: Predictive accuracy of first post-treatment PET/CT
in HPV-related oropharyngeal squamous cell carcinoma. Laryngoscope.
124:1843–1847. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chan JY, Sanguineti G, Richmon JD, Marur
S, Gourin CG, Koch W, Chung CH, Quon H, Bishop JA, Aygun N and
Agrawal N: Retrospective review of positron emission tomography
with contrast-enhanced computed tomography in the posttreatment
setting in human papillomavirus-associated oropharyngeal carcinoma.
Arch Otolaryngol Head Neck Surg. 138:1040–1046. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Vainshtein JM, Spector ME, Stenmark MH,
Bradford CR, Wolf GT, Worden FP, Chepeha DB, McHugh JB, Carey T,
Wong KK and Eisbruch A: Reliability of post-chemoradiotherapy
F-18-FDG PET/CT for prediction of locoregional failure in human
papillomavirus-associated oropharyngeal cancer. Oral Oncol.
50:234–239. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wang K, Wong TZ, Amdur RJ, Mendenhall WM,
Sheets NC, Green R, Thorp BD, Patel SN, Hackman TG, Zanation AM, et
al: Pitfalls of post-treatment PET after de-intensified
chemoradiotherapy for HPV-associated oropharynx cancer: Secondary
analysis of a phase 2 trial. Oral Oncol. 78:108–113.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Helsen N, Van den Wyngaert T, Carp L and
Stroobants S: FDG-PET/CT for treatment response assessment in head
and neck squamous cell carcinoma: A systematic review and
meta-analysis of diagnostic performance. Eur J Nucl Med Mol
Imaging. 45:1063–1071. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Taghipour M, Marcus C, Califano J, Fakhry
C and Subramaniam RM: The value of follow-up FDG-PET/CT in the
management and prognosis of patients with HPV-positive
oropharyngeal squamous cell carcinoma. J Med Imaging Radiat Oncol.
59:681–686. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Shonka DC Jr, Shoushtari AN, Thomas CY,
Moskaluk C, Read PW, Reibel JF, Levine PA and Jameson MJ:
Predicting residual neck disease in patients with oropharyngeal
squamous cell carcinoma treated with radiation therapy: Utility of
p16 status. Arch Otolaryngol Head Neck Surg. 135:1126–1132.
2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Corpman DW, Masroor F, Carpenter DM, Nayak
S, Gurushanthaiah D and Wang KH: Posttreatment surveillance PET/CT
for HPV-associated oropharyngeal cancer. Head Neck. 41:456–462.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Huang SH, O'Sullivan B, Xu W, Zhao H, Chen
DD, Ringash J, Hope A, Razak A, Gilbert R, Irish J, et al: Temporal
nodal regression and regional control after primary radiation
therapy for N2-N3 head-and-neck cancer stratified by HPV status.
Int J Radiat Oncol Biol Phys. 87:1078–1085. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Van der Putten L, Van den Broek GB, De
Bree R, van den Brekel MW, Balm AJ, Hoebers FJ, Doornaert P,
Leemans CR and Rasch CR: Effectiveness of salvage selective and
modified radical neck dissection for regional pathologic
lymphadenopathy after chemoradiation. Head Neck. 31:593–603.
2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fleischman GM, Thorp BD, Difurio M and
Hackman TG: Accuracy of ultrasonography-guided fine-needle
aspiration in detecting persistent nodal disease after
chemoradiotherapy. JAMA Otolaryngol Head Neck Surg. 142:377–382.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kao SS and Ooi EH: Survival outcomes
following salvage surgery for oropharyngeal squamous cell
carcinoma: Systematic review. J Laryngol Otol. 132:299–313.
2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Liu HY, Milne R, Lock G, Panizza BJ,
Bernard A, Foote M, McGrath M, Brown E, Gandhi M and Porceddu SV:
Utility of a repeat PET/CT scan in HPV-associated oropharyngeal
cancer following incomplete nodal response from
(chemo)radiotherapy. Oral Oncol. 88:153–159. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Bird T, Barrington S, Thavaraj S, Jeannon
JP, Lyons A, Oakley R, Simo R, Lei M and Guerrero Urbano T:
(18)F-FDG PET/CT to assess response and guide risk-stratified
follow-up after chemoradiotherapy for oropharyngeal squamous cell
carcinoma. Eur J Nucl Med Mol Imaging. 43:1239–1247.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Goguen LA, Chapuy CI, Li Y, Zhao SD and
Annino DJ: Neck dissection after chemoradiotherapy: Timing and
complications. Arch Otolaryngol Head Neck Surg. 136:1071–1077.
2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Subramaniam RM, Alluri KC, Tahari AK,
Aygun N and Quon H: PET/CT imaging and human papilloma
virus-positive oropharyngeal squamous cell cancer: Evolving
clinical imaging paradigm. J Nucl Med. 55:431–438. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Pellini R, Manciocco V, Turri-zanoni M,
Vidiri A, Sanguineti G, Marucci L, Sciuto R, Covello R, Sperduti I,
Kayal R, et al: Planned neck dissection after chemoradiotherapy in
advanced oropharyngeal squamous cell cancer: The role of US, MRI
and FDG-PET/TC scans to assess residual neck disease. J
Craniomaxillofac Surg. 42:1834–1839. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yu Y, Mabray M, Silveira W, Shen PY, Ryan
WR, Uzelac A and Yom SS: Earlier and more specific detection of
persistent neck disease with diffusion-weighted MRI versus
subsequent PET/CT after definitive chemoradiation for oropharyngeal
squamous cell carcinoma. Head Neck. 39:432–438. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Greuter MJ, Schouten CS, Castelijns JA, de
Graaf P, Comans EF, Hoekstra OS, de Bree R and Coupé VM:
Cost-effectiveness of response evaluation after chemoradiation in
patients with advanced oropharyngeal cancer using
18F-FDG-PET-CT and/or diffusion-weighted MRI. BMC
Cancer. 17(256)2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gupta GP, Kumar S, Marron D, Amdur RJ,
Hayes DN, Weiss J, Grilley-Olson J, Zanation A, Hackman T, Zevallos
JP, et al: Circulating tumor HPV16 DNA as a biomarker of tumor
genomics and disease control in HPV-associated oropharyngeal
squamous cell carcinoma. Int J Radiat Oncol Biol Phys.
100:1310–1311. 2018.
|
|
26
|
Ahn SM, Chan JY, Zhang Z, Wang H, Khan Z,
Bishop JA, Westra W, Koch WM and Califano JA: Saliva and plasma
quantitative polymerase chain reaction-based detection and
surveillance of human papillomavirus-related head and neck cancer.
JAMA Otolaryngol Head Neck Surg. 140:846–854. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dahlstrom KR, Li G, Hussey CS, Vo JT, Wei
Q, Zhao C and Sturgis EM: Circulating human papillomavirus DNA as a
marker for disease extent and recurrence among patients with
oropharyngeal cancer. Cancer. 121:3455–3464. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Jensen KK, Grønhøj C, Jensen DH and Von
buchwald C: Circulating human papillomavirus DNA as a surveillance
tool in head and neck squamous cell carcinoma: A systematic review
and meta-analysis. Clin Otolaryngol. 43:1242–1249. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lee JY, Garcia-Murillas I, Cutts RJ, De
Castro DG, Grove L, Hurley T, Wang F, Nutting C, Newbold K,
Harrington K, et al: Predicting response to radical
(chemo)radiotherapy with circulating HPV DNA in locally advanced
head and neck squamous carcinoma. Br J Cancer. 117:876–883.
2017.PubMed/NCBI View Article : Google Scholar
|