Introduction
Cervical cancer is a worldwide public health issue
with 570,000 new cases and 311,000 deaths estimated to have
occurred in 2018(1). Squamous cell
carcinoma is the main histological type, ranging between 75-85%,
while 15-25% are adenocarcinomas (2,3). The
incidence of cervical adenocarcinoma has increased proportionally
in the last decade (2,3).
Standard treatment for locally advanced cervical
cancer is concurrent chemoradiotherapy. Surgery, either radical or
extrafascial hysterectomy performed after radiation therapy
provides no benefit, notably in squamous cell carcinoma cases
(4). Existing evidence regarding
cervical adenocarcinoma is based on studies evaluating
adenocarcinoma in conjunction with squamous cell carcinoma,
representing a small proportion of cases (5,6).
Several studies have indicated that cervical
adenocarcinoma may be a particular group of cancers that have a
worse prognosis and a 20% decrease in overall survival (7,8), which
may be explained by the infiltrative growth pattern of cervical
adenocarcinoma, bulky and barrel-shaped, and the higher proportion
of distant metastasis (9). Thus, to
improve local control, a strategy considered by several cancer
centers is to perform hysterectomy after radiotherapy in selected
cases and eliminate possible central residual cancer cells
(10), but there is a lack of
consensus on hysterectomy benefits.
The purpose of the present study was to evaluate
long-term outcomes achieved with the use of extrafascial
hysterectomy after radiation therapy for locally advanced cervical
adenocarcinoma.
Materials and methods
Study design
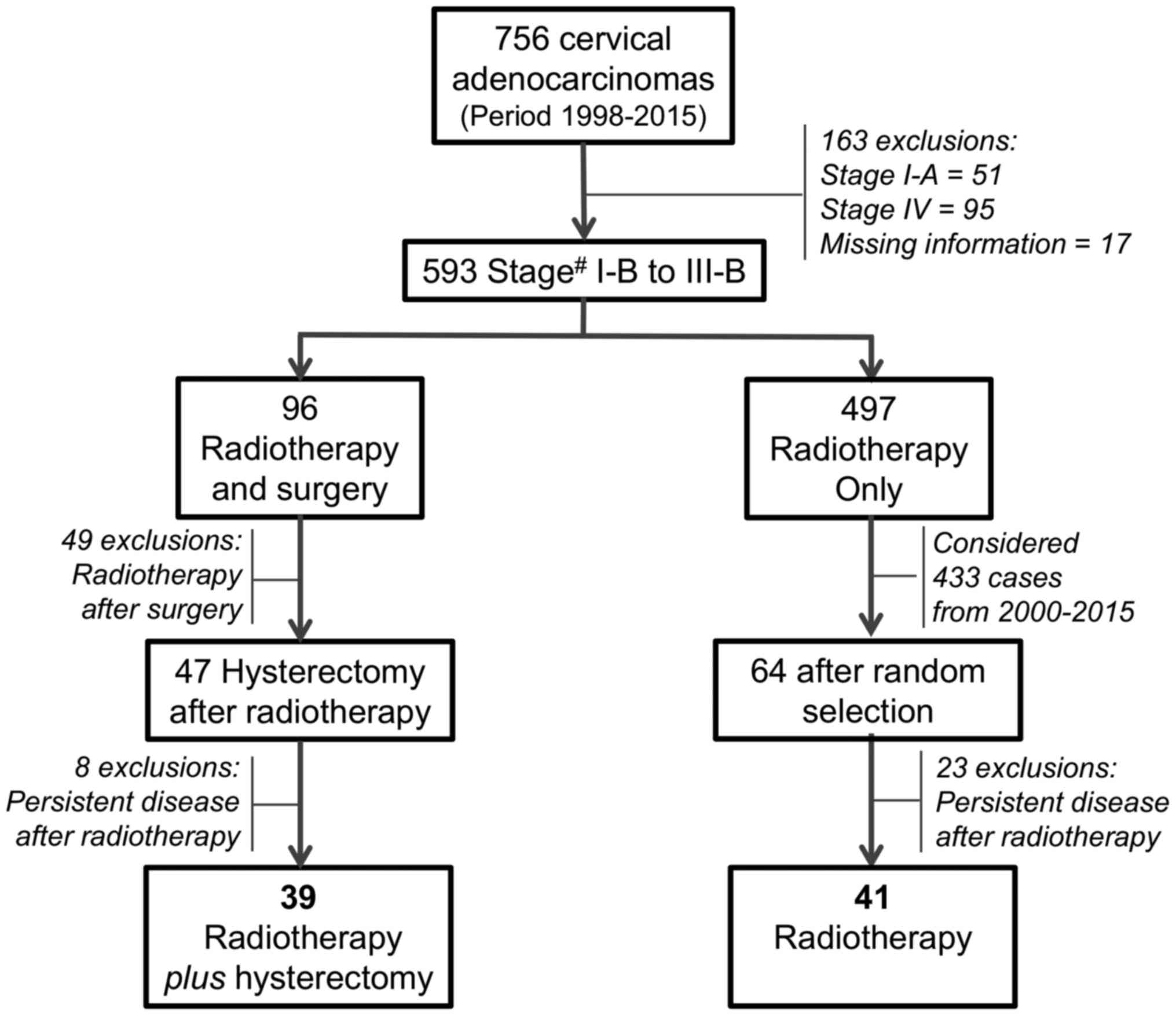
This retrospective study selected cases from 756
cervical adenocarcinoma patients (Fig.
1) managed at the Women's Hospital of the University of
Campinas (UNICAMP), in Campinas (SP), Brazil from 1988 to 2015.
Subject selection
The inclusion criteria considered for the selection
of patients were cancer stage IB to IIIB according to FIGO-2014
system (11), complete medical
records with all information related available, radiotherapy as the
first approach followed by hysterectomy performed within 100 days
after completion of actinic therapy, and exhibited complete
clinical response in the clinical or image evaluation after 30 to
40 days of radiotherapy ending. UNICAMP is a teaching and research
institution and a referral center for the Brazilian public health
system, and in the considered period, 3,810 females with cervical
cancer were assisted. According to the case selection criteria were
excluded 51 cervical adenocarcinomas cases at stage IA, 95 at stage
IV, and 17 with missing information in the medical records. 497
women managed only with radiotherapy were considered to build a
comparison group. Of the remaining 96 cases, 49 additional cases
were excluded because the surgery was performed before radiotherapy
and 8 additional cases were excluded because they had persistent
disease after radiotherapy and the hysterectomy was considered as
salvage surgery. Finally, all 39 remaining cases had confirmation
of complete clinical response following radiotherapy (no disease at
physical examination and for image evaluation if available), and
the post-radiation hysterectomy was considered as consolidation
therapy.
Control group
For reference, a comparison group was established by
searching for institutional digital medical records among the 497
cases treated only with radiotherapy. Initially, 433 cervical
adenocarcinomas from the period 2000-2015 were considered and 64
cases were selected for detailed review at random. After all 64
medical records have been reviewed, 23 cases exhibited a persistent
disease after completion of the radiotherapy and were excluded,
resulting in 41 females with a complete clinical response after
primary radiotherapy or chemoradiotherapy without surgery and with
adequate follow-up were identified (Fig. 1).
Case management
Diagnosis of the cervical cancer stage is generally
completed after clinical examination by gynecological oncologist
surgeons and according to the FIGO staging system. Doubtful cases
are reviewed together with radiotherapists and by clinical
examination with sedation. FIGO system updates from 1988-2015 are:
(1994) Stage IA divided into IA1 and IA2 (microinvasive cervical
cancer), and Stage IB division into IB1 (tumor <4 cm) and IB2
(tumor ≥4 cm); (2009) Stage IIA divided into IIA1 (tumor <4 cm)
and IIA2 (tumor ≥4 cm); (2014) staging system maintained (11,12).
For this study, the stages were grouped into 2 categories (stages
IB-IIA vs. IIB-IIIB) according to FIGO-2014 staging system
(11). Definition of management
follows a multidisciplinary approach, and the decision for a
hysterectomy after radiotherapy is optional and influenced by the
preference of the gynecological oncologist. Radiation therapy for
cervical cancer in our center follows an institutional protocol,
associating external-beam radiation therapy with uterovaginal
high-dose-rate (HDR) brachytherapy. Typically, 20 daily fractions
of 1.8-2.0 Gray are applied, followed by 4 weekly sessions of HDR
brachytherapy of 7 Gray each. In advanced disease, an additional
boost dose of 14.4 Gray is prescribed over the compromised
parametrial region, to ultimately achieve a total radiation dose of
85 Gray at point A. Our institution started to offer radiotherapy
with weekly cisplatin concurrent chemotherapy in 2003, and we
expected to find this strategy to be more frequently applied in the
cases managed following that year.
Follow-up
Following the completion of radiotherapy, patients
returned within 30-45 days for clinical response and toxicity
evaluation. In the case of cervical adenocarcinoma, return visits
could be scheduled earlier at intervals of 14-21 days to assess the
indication of hysterectomy. Hysterectomy was finally indicated
after clinical evaluation by gynecological oncologists who operated
at the same oncology center. Typically, an extrafascial Piver type
I (Querleu A) hysterectomy was performed by laparotomy. After
treatment completion, the follow-up evaluation was performed by
gynecological oncologists and consisted of periodical clinic
evaluation in appointments every 3 months in the first year and
every 6 months until completing the fifth year, with cytology
collection from the vaginal cuff every 6 months.
Statistical analysis
Treatment period, age group, staging according to
the International Federation of Gynecology and Obstetrics (FIGO)
2014(11), type of radiotherapy,
radiation dose and duration of treatment were compared in groups
with and without hysterectomy after radiotherapy. For the series of
cases of interest, the time interval between completion of
radiation therapy and hysterectomy, surgical duration,
postoperative complications, presence of histopathological residual
disease and relation to the occurrence of pelvic relapses or
distant metastases were evaluated. For this analysis, χ2
or Fisher's exact tests were performed for frequencies. Student's
t-test was used for unpaired samples for comparison of means.
Analysis of overall survival and disease-free survival was
performed by Kaplan-Meier method and log-rank tests by treatment
group and based on the presence of residual disease in the
hysterectomy specimen. A follow-up of 150 months was considered at
most. The significance level adopted for the statistical tests was
5%, and StatsDirect (version 3.0, 2018) statistical package was
used for statistical analysis.
This study followed recommendations of the National
Health Council of Brazil and was previously approved by the Ethics
Committee of UNICAMP (approval no. 1.207.539; August 31, 2015).
Results
Group comparison
The series of cases of interest had 67% of
hysterectomies performed until the year 2002 (vs. 22%,
P<0.0001), and 49% of the group without surgery performed
concurrent chemoradiotherapy (vs. 15%, P=0.001), a difference due
to the criterion used for the selection of the comparison group
that considered cases from 2,000. Groups were matched by age, tumor
stage, total radiation dose, duration of treatment and a follow-up
>70 months for both groups (Table
I).
 | Table IComparison between cervical
adenocarcinoma cases that received or did not receive hysterectomy
after radiotherapy. |
Table I
Comparison between cervical
adenocarcinoma cases that received or did not receive hysterectomy
after radiotherapy.
| | Hysterectomy after
radiotherapy | |
|---|
| Characteristic | Yes (n=39) n (%) | No (n=41) n (%) | P-valuea |
|---|
| Period | | | |
|
1988-2002 | 26(67) | 9(22) | |
|
2003-2015 | 13(33) | 32(78) | <0.001 |
| Age group
(years) | | | |
|
<40 | 11(28) | 6(15) | |
|
40-59 | 22(57) | 28(68) | |
|
≥60 | 6(15) | 7(17) | 0.330 |
| Stagec | | | |
|
IB to
IIA | 9(23) | 5(12) | |
|
IIB to
IIIB | 30(77) | 36(88) | 0.200 |
| Radiation
therapy | | | |
|
Total dose
(Gray) | | | |
|
Mean ±
SD | 83.1±13 | 86.6±5 | 0.108b |
|
Median | 87.4 | 87.4 | |
| Duration (days) | | | |
|
Mean ±
SD | 88.2±45 | 78.9±25 | 0.124b |
|
Concurrent
chemoradiotherapy | 6(15) | 20(49) | 0.001 |
| Follow-up period
(months) | | | |
|
Mean ±
SD | 72±44 | 78±38 | 0.279b |
Post-radiotherapy hysterectomy
Post-radiotherapy hysterectomy was performed after
54 days on average (range: 13-97 days, median=49 days), following
the completion of radiation therapy. The mean surgical duration was
159 min (90-300 min). The most relevant perioperative complications
occurred in nine patients, including blood transfusion (most
common), cardiac arrhythmia, ureteral injury, vascular injury and
abdominal wall dehiscence. Late complications in the hysterectomy
group occurred in three cases and included vesicovaginal fistula,
bowel obstruction and subclavian vein thrombosis, all in patients
without active disease. An additional two cases of fistulas and one
case of deep venous thrombosis were observed in females with active
disease. In the control group, six cases of genital fistulas were
recorded during follow-up, all in patients associated with local
active disease. Histopathological residual disease was detected in
56% (22/39) of uterine specimens, 12 cases with up to 10 mm in size
(10 cases with ≥11 mm), and 11 cases with radiotherapy-surgery
interval time up to 49 days (11 cases with interval ≥50 days).
Recurrence and survival
No significant differences in recurrence rates
(pelvic and/or metastases) were observed in the follow-up. Nine
cases (23%) from the hysterectomy group and 10 cases (24%) from the
control group had recurrences. In the hysterectomy group, the
detection of residual disease in hysterectomy specimens was
associated with a higher recurrence rate (8 cases, 31%), including
distant metastases (vs. 6%, P=0.028, Table II). Six of the eight cases with
recurrence of the residual disease was ≥11 mm in size, and four of
them had radiotherapy end-surgery intervals up to 49 days. There
was a similar distribution of radiotherapy end-surgery interval
time according to detection or not of residual disease for all 39
cases managed with hysterectomy.
 | Table IICervical adenocarcinoma recurrences in
the follow-up period of women that received or did not receive
hysterectomy in addition to pelvic radiotherapy, with the presence
of residual disease in the uterus. |
Table II
Cervical adenocarcinoma recurrences in
the follow-up period of women that received or did not receive
hysterectomy in addition to pelvic radiotherapy, with the presence
of residual disease in the uterus.
| | Pelvic
recurrence | Any recurrence |
|---|
| Variable | Yes n (%) | No n (%) | P-valuea | Yes n (%) | No n (%) | P-valuea |
|---|
| Hysterectomy after
radiotherapy | | | | | | |
|
Yes
(n=39) | 5(13) | 34(87) | | 9(23) | 30(74) | |
|
No
(n=41) | 4(10) | 37(90) | 0.468 | 10(24) | 31(76) | 0.890 |
| Residual disease | | | | | | |
|
Yes
(n=22) | 4(18) | 18(82) | | 8(31) | 14(69) | |
|
No
(n=17) | 1(6) | 16(94) | 0.262 | 1(6) | 16(94) | 0.028 |
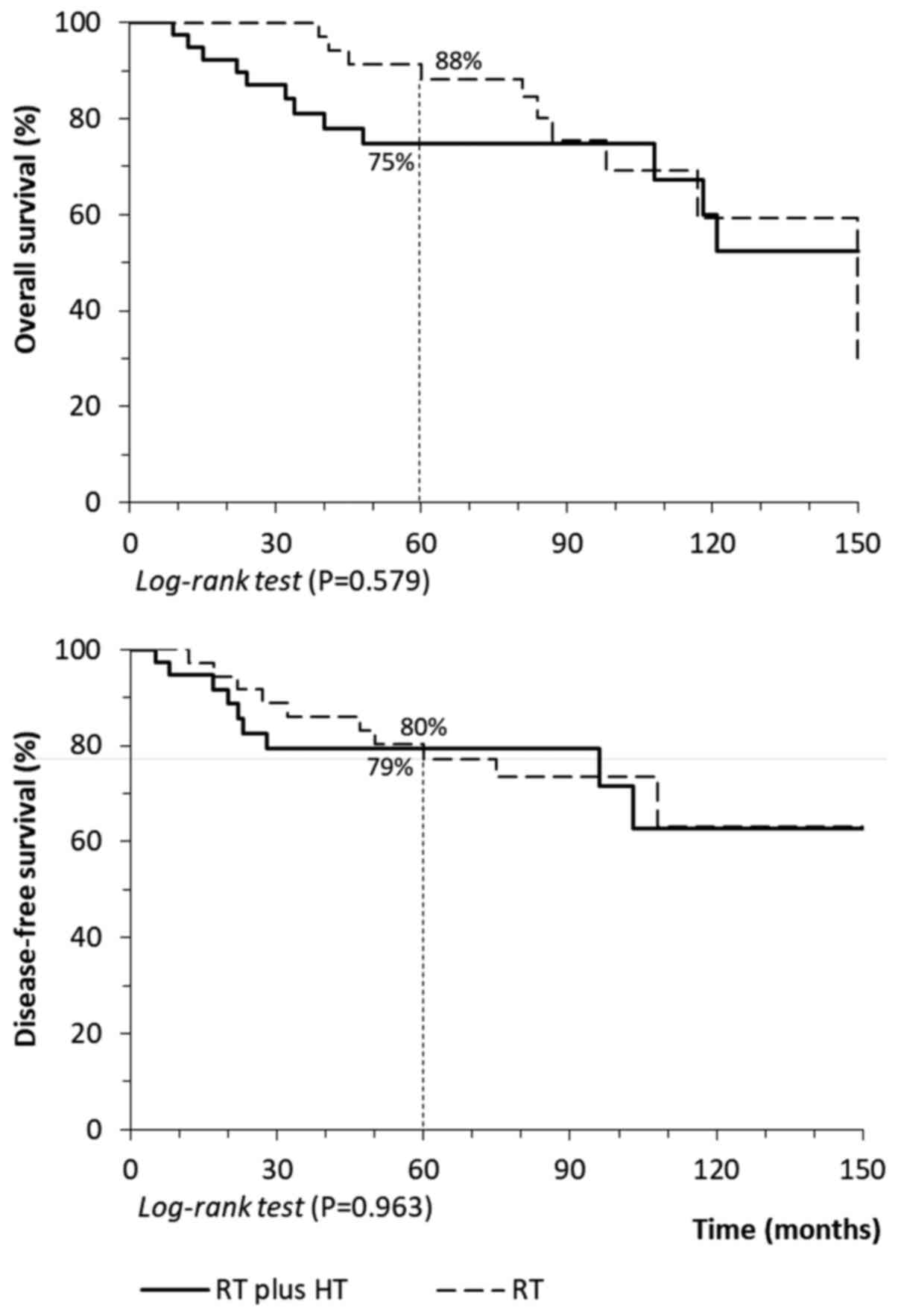
In Fig. 2, the
overall survival and disease-free survival rates showed no
difference between groups. After five years, the overall survival
rate was 75% for the group undergoing hysterectomy and 88% for the
control group (P=0.579), and the disease-free survival rate was
79-80% for both groups (Fig.
2).
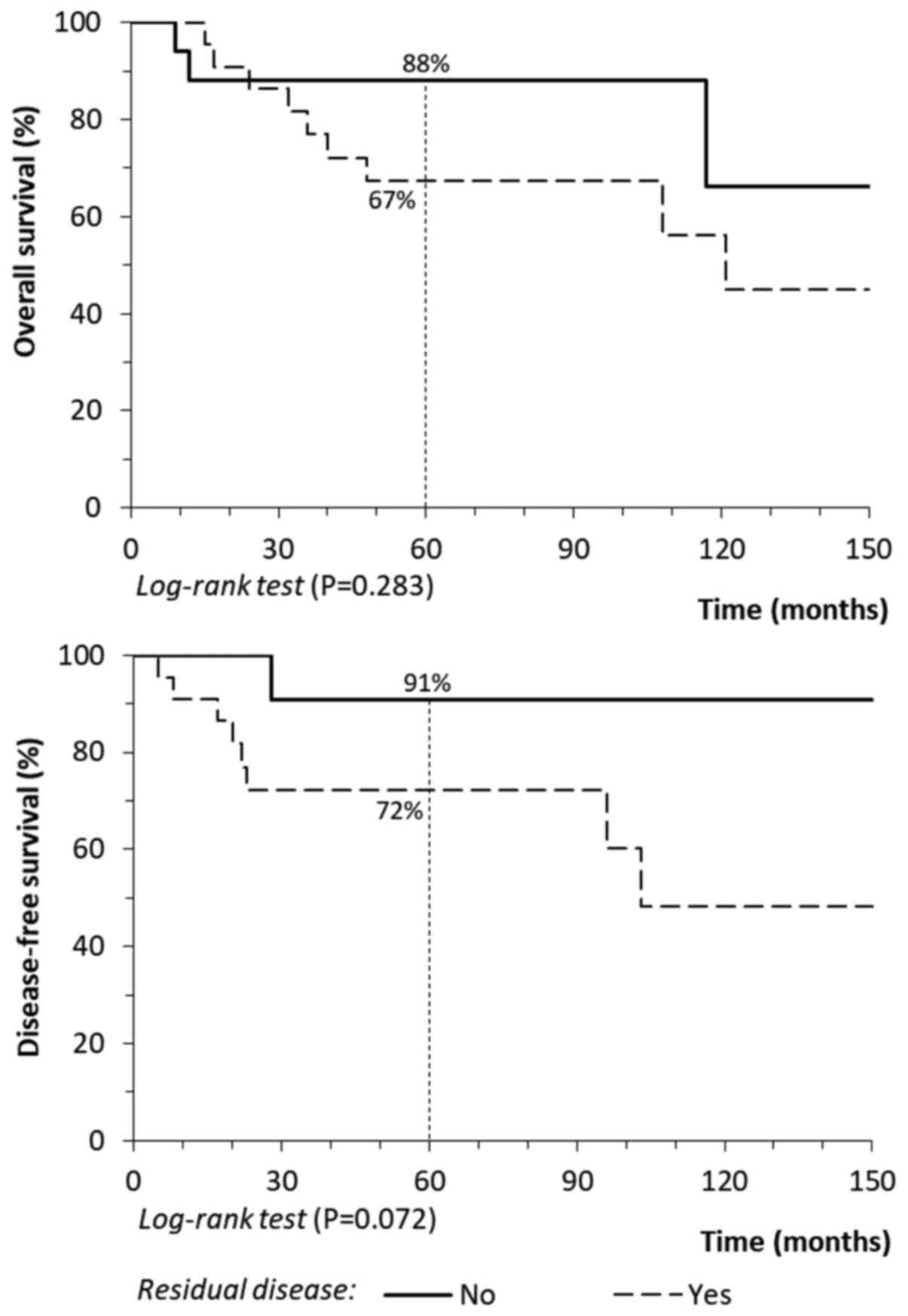
During follow-up care, there was no improvement in
long-term outcomes, even among cases with residual disease that was
detected and removed during the hysterectomy. By contrast, that
overall survival (P=0.283) and disease-free survival rates
(P=0.072) decreased by ~20%, although it was not statistically
significant (Fig. 3).
Discussion
In females with cervical adenocarcinoma,
post-radiotherapy hysterectomy did not change the rates of disease
recurrence (23-24%), disease-free survival rate (79-80% at 5 years)
and 5-year overall survival rate (75 vs. 88%), in comparison to
exclusive radiation therapy (with more proportion of
chemoradiation). Among the 39 cases managed by radiotherapy plus
hysterectomy, uterine residual disease was detected in 56% of cases
and the removal of this residual tumor also had no impact on
outcomes during follow-up. The presence of residual disease was
associated with more frequent disease recurrence (31 vs. 6%,
P=0.028) and a decrease to 20% in disease-free survival rate (91
vs. 72%) and 5-year overall survival rate (88 vs. 67%). Females
submitted to a hysterectomy after radiotherapy (with a low
proportion of chemoradiation), and detection of residual disease in
histopathology indicated a group with a worse prognosis which was
not controlled by surgery.
There is a perception that radiation therapy may be
less effective in bulky tumors, ultimately persisting central
residual foci of tumor that favor disease recurrence and a poorer
prognosis. Cervical adenocarcinoma generally correlates with a
barrel-shaped tumor, favoring this type of behavior. In practice,
evidence suggested that cervical adenocarcinoma may be more
resistant to radiotherapy, justifying a report describing that
persistent residual disease occurs after radiotherapy in 50% of
cases, which was confirmed in our study (56%, 22/39 cases). The
fact that residual disease is frequently present after radiation,
supports the hypothesis that adjuvant surgical resection may
improve local disease control, disease-free survival, and overall
survival rates (13,14). Nevertheless, it is worth mentioning
that none of the studies, this one included, showed any benefit
arising from the removal of residual disease at hysterectomy in
terms of disease-free survival and overall survival, although this
study had a greater proportion of patients in the comparison group
(without hysterectomy) receiving chemotherapy. Chemosensitized
radiotherapy used in more recent years may have compensated any
positive effect of post-radiotherapy surgery performed before 2003
and the year when the chemoradiation started in our
institution.
The use of concurrent chemoradiotherapy in locally
advanced cervical carcinomas has shown an improved response to
treatment and could justify the lower number of surgical
indications, as observed in this study with fewer cases operated
since 2003 (15,16). Although this study did not resolve
the effect of chemoradiation on the therapeutic outcome, this study
may have directed the perception that any gain with hysterectomy
following radiotherapy using older protocols may have been
compensated due to the higher rate of chemoradiation that has been
recently applied.
Surgical complications related to procedures
following radiotherapy may be higher than expected (15). In the studied cases, hysterectomy
procedures after radiotherapy probably had a longer duration than
expected (2 h and 30 min). However, higher surgical difficulty is
encountered in irradiated fields due to local fibrosis and
inflammation. In this study, complications included one ureteral
and one vascular injury, and increased intraoperative bleeding
requiring transfusion in four cases. Late complications, mainly
related to radiotherapies, such as proctitis, cystitis or fistulas,
occurred in rates expected for the pattern of cases studied and
were similar in both groups.
Few studies have reported outcomes of hysterectomies
after radiotherapy in specific cases of females with cervical
adenocarcinoma, and most have described salvage situations, with
evident persistent residual disease after completion of actinic
treatment. The study with the largest number of post-radiotherapy
hysterectomies for cervical adenocarcinoma (34 cases) was published
in 2016 by Yang et al (15),
with only 18 cases exhibiting complete clinical response after
chemoradiation. The study concluded that hysterectomy improved
survival but counted patients who submitted to salvage surgery.
Our data showed that residual disease in
hysterectomy specimens was considered a prognostic factor for
disease recurrence in females with adenocarcinoma primarily managed
with radiotherapy. Nonetheless, the actual impact of surgical
excision remains unclear, since it did not significantly change
overall survival and disease-free survival rates when compared with
more recent cases with a higher proportion of chemoradiation. Among
the nine patients presenting disease recurrence observed in the
hysterectomy group, eight patients had residual disease in the
surgical specimen and four patients had only distant metastases
during follow-up.
This study has limitations related to the number of
cases, despite being one of the largest case studies of cervical
adenocarcinoma undergoing post-radiotherapy hysterectomy to date.
Furthermore, it is a retrospective study and the comparison group
may not reflect reality since cases treated in distinct periods
were considered with different proportions of chemoradiation.
Additional studies need to be performed to assess
the actual impact to remove clinically undetectable residual
cervical adenocarcinoma post-radiotherapy, and how much concurrent
chemoradiotherapy improves control without need for any
surgery.
In conclusion, post-radiotherapy hysterectomy in
females with locally advanced cervical adenocarcinoma managed by
radiation with complete clinical response is a feasible procedure
that has an acceptable level of complications. However, it did not
confer relevant benefits in terms of disease recurrence,
disease-free survival, and overall survival in comparison to
radiotherapy or chemoradiotherapy alone and should not be routinely
indicated.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ECAS conceived and designed the current study,
acquired and revised the data, and drafted the manuscript. DZS
contributed to the acquisition of data, data revision, and drafted
the manuscript. JCCT acquired and revised the data, and drafted the
manuscript. DBV developed the methodology, revised, analyzed and
interpreted the data, and drafted the manuscript. JFB developed the
methodology, and analyzed and interpreted the data. JCT conceived
and designed the current study, acquired, analyzed and interpreted
the data, drafted the manuscript, and supervised the study. All
authors were involved in revising critically the manuscript and
providing final approval of the version to be published.
Ethics approval and consent to
participate
The present study was developed in compliance with
Resolution 466/12 of the Brazilian National Health Council and
Declaration of Helsinki and was previously approved by the Research
Ethics Committee of the University of Campinas (approval no.
1.207.539, August 31, 2015).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Castellsagué X, Díaz M, de Sanjosé S,
Muñoz N, Herrero R, Franceschi S, Peeling RW, Ashley R, Smith JS,
Snijders PJ, et al: Worldwide human papillomavirus etiology of
cervical adenocarcinoma and its cofactors: Implications for
screening and prevention. J Natl Cancer Inst. 98:303–315.
2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Teixeira JC, Maestri CA, Machado HDC,
Zeferino LC and Carvalho NS: Cervical cancer registered in two
developed regions from Brazil: Upper limit of reachable results
from opportunistic screening. Rev Bras Ginecol Obstet. 40:347–353.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Keys HM, Bundy BN, Stehman FB, Okagaki T,
Gallup DG, Burnett AF, Rotman MZ and Fowler WC Jr: Gynecologic
Oncology Group. Radiation therapy with and without extrafascial
hysterectomy for bulky stage IB cervical carcinoma: A randomized
trial of the gynecologic oncology group. Gynecol Oncol. 89:343–353.
2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhou J, Wu SG, Sun JY, Li FY, Lin HX, Chen
QH and He ZY: Comparison of clinical outcomes of squamous cell
carcinoma, adenocarcinoma, and adenosquamous carcinoma of the
uterine cervix after definitive radiotherapy: A population-based
analysis. J Cancer Res Clin Oncol. 143:115–122. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lèguevaque P, Motton S, Delannes M,
Querleu D, Soulé-Tholy M, Tap G and Houvenaeghel G: Completion
surgery or not after concurrent chemoradiotherapy for locally
advanced cervical cancer? Eur J Obstet Gynecol Reprod Biol.
155:188–192. 2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kaidar-Person O, Yosefia S and
Abdah-Bortnyak R: Response of adenocarcinoma of the uterine cervix
to chemoradiotherapy. Oncol Lett. 9:2791–2794. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gadducci A, Guerrieri ME and Cosio S:
Adenocarcinoma of the uterine cervix: Pathologic features,
treatment options, clinical outcome and prognostic variables. Crit
Rev Oncol Hematol. 135:103–114. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jonska-Gmyrek J, Gmyrek L,
Zolciak-Siwinska A, Kowalska M and Kotowicz B: Adenocarcinoma
histology is a poor prognostic factor in locally advanced cervical
cancer. Curr Med Res Opin. 35:595–601. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Huang YT, Wang CC, Tsai CS, Lai CH, Chang
TC, Chou HH, Hsueh S, Chen CK, Lee SP and Hong JH: Long-term
outcome and prognostic factors for adenocarcinoma/adenosquamous
carcinoma of cervix after definitive radiotherapy. Int J Radiat
Oncol Biol Phys. 80:429–436. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
FIGO Committee on Gynecologic Oncology.
FIGO staging for carcinoma of the vulva, cervix, and corpus uteri.
Int J Gynaecol Obstet. 125:97–98. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Odicino F, Pecorelli S, Zigliani L and
Creasman WT: History of the FIGO cancer staging system. Int J
Gynaecol Obstet. 101:205–210. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Mazeron R, Gouy S, Chargari C, Rivin Del
Campo E, Dumas I, Mervoyer A, Genestie C, Bentivegna E, Balleyguier
C, Pautier P, et al: Post radiation hysterectomy in locally
advanced cervical cancer: Outcomes and dosimetric impact. Radiother
Oncol. 120:460–466. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hequet D, Marchand E, Place V, Fourchotte
V, De La Rochefordière A, Dridi S, Coutant C, Lecuru F, Bats AS,
Koskas M, et al: Evaluation and impact of residual disease in
locally advanced cervical cancer after concurrent chemoradiation
therapy: Results of a multicenter study. Eur J Surg Oncol.
39:1428–1434. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yang J, Shen K, Wang J, Yang J and Cao D:
Extrafascial hysterectomy after concurrent chemoradiotherapy in
locally advanced cervical adenocarcinoma. J Gynecol Oncol.
27(e40)2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Shi D, Liang Z, Zhang C, Zhang H and Liu
X: The effect of surgery on the survival status of patients with
locally advanced cervical cancer after
radiotherapy/chemoradiotherapy: A meta-analysis. BMC Cancer.
18(308)2018.PubMed/NCBI View Article : Google Scholar
|