Introduction
Breast cancer (BC) is the most common cancer among
women worldwide, affecting 2.1 million women annually. An estimated
627,000 women succumbed to BC in 2018, accounting for ~15% of all
cancer deaths among women (1).
BC screening programs provide an important
opportunity for early BC detection and contribute to improved
survival and reduced BC-associated mortality (2-5).
Screening is the key element for early detection of BC, and it is
widely recommended by professional guidelines and supported by
organized screening programs in several countries around the globe.
There are several screening modalities, among which mammography
(MAM) is the most widely accepted (6). It has been repeatedly reported that
MAM screening is the most effective method for detecting
early-stage disease and decreasing mortality (7-10).
However, in certain areas and communities with limited access to
technology such as MAM, Clinical Breast Examination (CBE) plays a
critical role. CBE is the examination of a woman's breasts by a
healthcare professional who is experienced in identifying different
types of abnormalities and warning signs in the breast, and it is
particularly important in rural areas and developing countries
(11).
A minority group refers to a category of people who
experience a relative disadvantage as compared to members of a
dominant social group. It is typically based on differences in
observable characteristics or practices, such as ethnicity, race
and religion, among others (12,13).
Adherence to BC screening guidelines is frequently
lower in racial, ethnic and cultural minority populations and,
therefore, late diagnosis, worse prognosis and increased mortality
are commonly observed in these groups (14). This adherence is affected by
potential inequities or barriers to screening that these minorities
face; thus, it is crucial for physicians to have the necessary
information and skills to be able to reach these women, increasing
the commitment to screening and reducing BC mortality. Furthermore,
public health-related decisions and interventions must take into
account these disparities between racial, ethnic and cultural
groups to adopt the most efficient measures for dealing with this
issue (15,16).
A number of studies have recently been published on
this field about different minorities (12-16).
The aim of the present systematic review was to collect information
from different minority groups worldwide, assess adherence to BC
screening and evaluate barriers or limitations responsible for
non-adherence in order to pinpoint specific failures and their
causes. The findings may enable the development of effective
interventions aimed at the identified barriers to screening, with
the purpose of increasing screening among these women and,
subsequently, reducing mortality. Using a systematic review-based
study, the factors adversely affecting BC screening adherence were
critically examined, particularly among minorities, and the main
contingencies related to the adherence rates to BC screening were
investigated in ethnic, cultural and religious minorities in order
to assess the barriers of implementation of BC screening.
Materials and methods
Search methods
The primary search was conducted using the PubMed
and Web of Science databases. The key words and Boolean operators
used were as follows: ‘Breast cancer’ screening AND (adherence OR
uptake) AND (barriers OR inequities). In PubMed, a time filter for
the last 5 years was applied. In Web of Science, the search was
made by topic and a filter for the years 2015, 2016, 2017, 2018,
2019 and 2020 was applied. The last update of the search was
conducted on March 16th, 2020.
Duplicate citations were removed using Mendeley and
the remaining results were organized using a Microsoft Excel
document with records of the exclusion rationale.
The search focused on papers published in English
due to the impact on science literature; additionally, papers
published in Portuguese were also selected in order to include the
potential observations of Portuguese authors on this subject. The
search was initiated in 2015 due to the high number of publications
before that year without the modification of impact in BC
prevention in poor areas and minorities, and also due to the better
impact of articles published from 2015 onwards in terms of quality
of the information and also in terms of the number of women with
significant cultural and religious diversity enrolled in these
studies.
Eligibility criteria
Three independent reviewers evaluated all citations
for eligibility and any disagreements were resolved by
consensus.
Articles were considered when they fulfilled the
following inclusion criteria: i) Female patients; ii) BC screening
program implemented in the country; iii) minority groups; iv)
asymptomatic patients; v) study written in Portuguese or English;
and vi) study published from 2015 onwards.
The exclusion criteria were as follows: i) Age
<18 years; ii) emergency examination; iii) previous history of
BC or mastectomy; iv) family history of BC; v) target population
with congenital or chronic conditions; vi) no assessment of
barriers to screening; and vii) intervention-based programs.
Data extraction, synthesis and
analysis
Three review authors extracted all relevant
information from the included articles and organized it in a
Microsoft Excel document in a standardized form in order to
facilitate comparison between studies.
The following details were collected: Study ID
(authors, year of publication, country and main objective), design
(type of study, target population, selection process, inclusion and
exclusion criteria), characteristics of the population (number of
study participants, age range, data collection method), BC
screening details (type of screening recommended) and relevant
findings of the study (screening adherence rates, barriers
considered and outcomes of the study).
Critical appraisal
Three review authors independently appraised the
selected articles and any disagreements were resolved by
consensus.
For this purpose, the Critical Appraisal Skills
Program (CASP) checklist was used for qualitative studies and the
Strengthening The Reporting of Observational Studies in
Epidemiology (STROBE) checklist for cross-sectional studies.
Studies were classified according to their quality
assessment percentage as follows: ‘High quality’, >85%;
‘moderate to high’, 75-85%; ‘moderate’, 60-75%; ‘low to moderate’,
50-60%; and ‘low’, <50%.
Results
Study selection
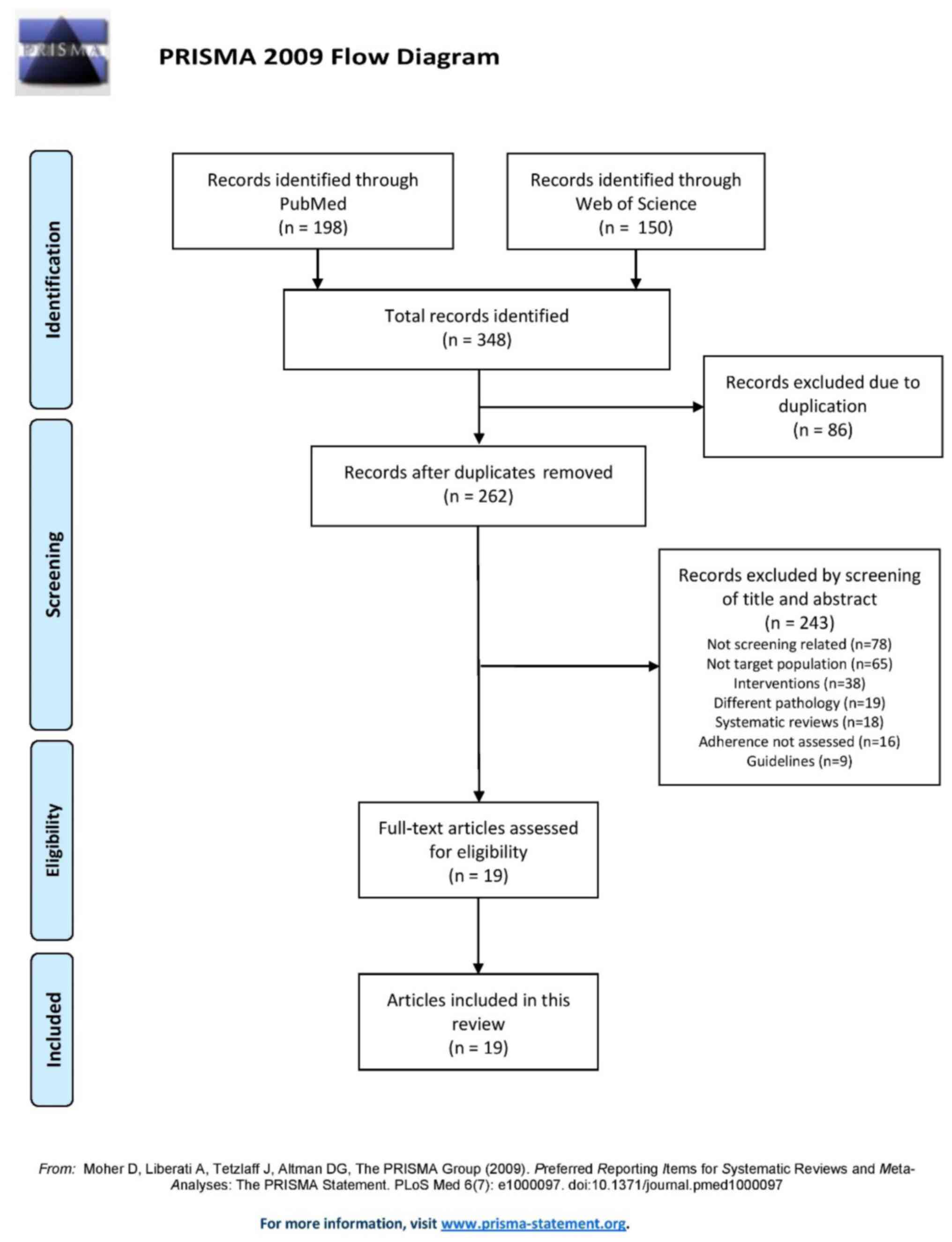
The study selection process is described in the
flowchart shown in Fig. 1. The
PubMed search yielded 198 results and the Web of Science search
yielded 150 results. Of those, 86 were duplicates, resulting in 262
records after duplicate removal.
Of the 262 studies, 243 were excluded: 78 were not
related to breast screening, 65 had a different target population,
38 were intervention-based studies, 19 were related to a different
pathology, 18 were systematic reviews, 16 did not assess adherence
and 9 were guidelines. Finally, 19 full-text articles in total were
deemed as eligible and were included in the present review.
Critical appraisal
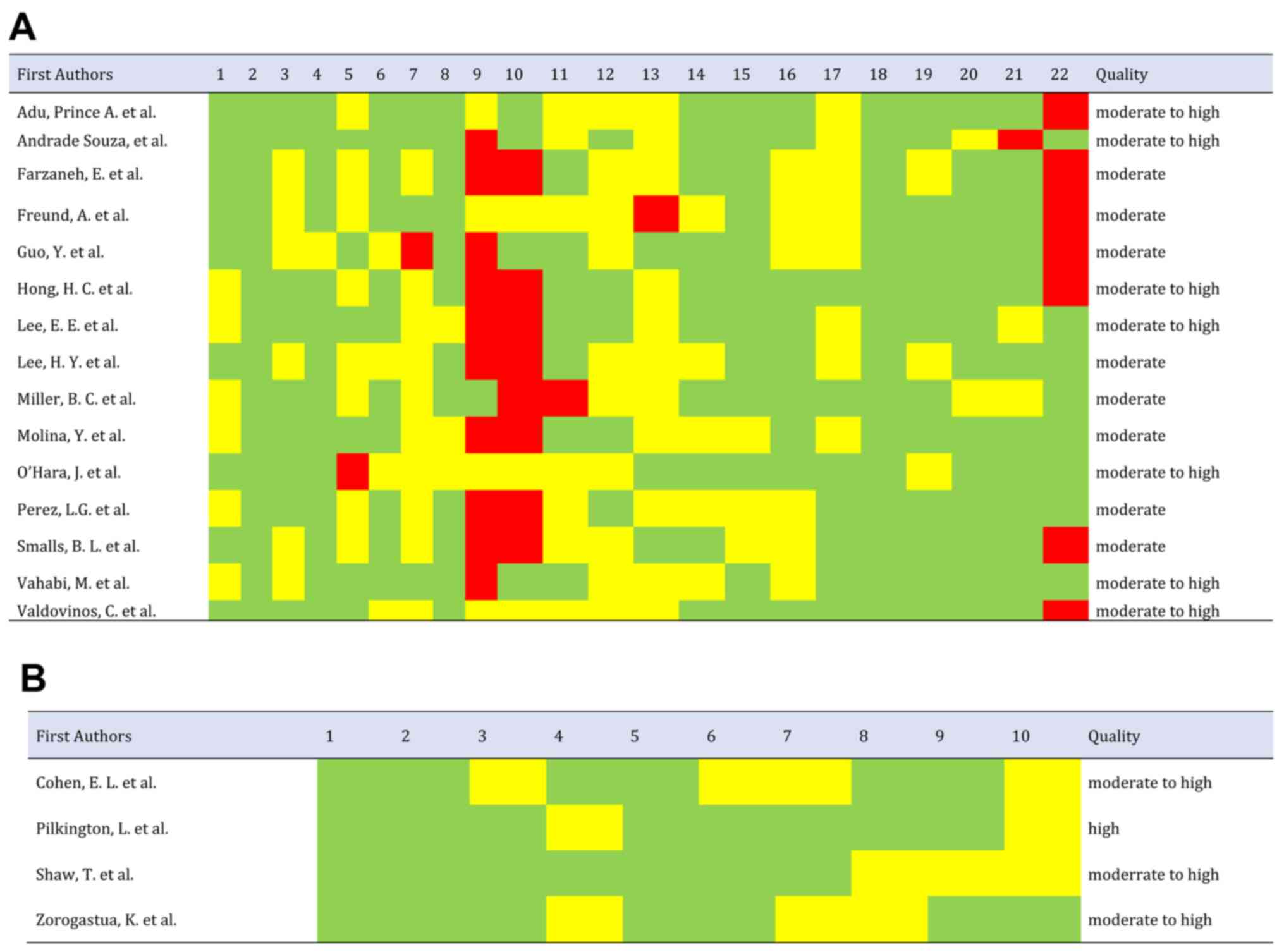
The quality parameters of the study based on STROBE
and CASP are comprehensively presented in Fig. 2A and B, respectively. Of the 19 studies
included, 5.3% were classified as high-quality, 52.6% as
moderate-to-high, 42.1% as moderate, and none of the articles
selected were rated as low-to-moderate or low-quality. Of the
cross-sectional studies, 66.7% failed to describe the efforts made
to address potential sources of bias; only Miller et al
(17) had included this parameter.
Furthermore, 53.3% of cross-sectional studies did not describe how
the study size was reached, while this was described in the studies
of Adu et al (18), De
Andrade Souza et al (19),
Guo et al (20) and Vahabi
et al (21). Finally, 46.7%
of cross-sectional studies did not specify the source of funding or
the role of the funders in the study. All the cross-sectional
studies explained the scientific background and rationale for the
investigation being reported in the introduction and summarized the
key results in the discussion with reference to study objectives.
All the qualitative studies had a high percentage on quality
assessment; they all clearly stated the aims of the research and
had an appropriate methodology.
Characterization of the studies
Of the 19 studies included in this review, 15 (79%)
were designed as cross-sectional and 4 (21%) as qualitative
(Table SI). The total number of
participants of the articles analysed in this systematic review was
250,733, mainly due to the article by Vahabi et al (21) that included data from 238,218 women.
The studies that included fewer participants (27 women) were the
ones with the qualitative design, which is justified by this method
limitation. The age range of the participants was similar in almost
all articles (minimum, 40-50 years and maximum, ~75 years) and
concordant with the screening programs recommended in each country.
The exceptions were the articles that, in parallel, evaluated the
screening for cervical cancer, for example Zorogastua et al
(22), which included younger
women. However, even these exceptions reported their results
separately, considering only women aged ≥40 years, for the BC
screening analysis. The target populations of the 19 articles
(Table SI) included in this
systematic review were the following: English-, Arabic- and
Italian-speaking women in Australia; immigrant women in Canada;
Hispanic Community in the USA; Arab and ultra-orthodox Jewish women
in Israel; immigrant women from Muslim majority and non-Muslim
majority countries; Latin American women; African American women;
African American and African-born Muslim women; Korean American
women; Chinese American women; Azeri, Malay, Amazonian, Appalachian
and Aboriginal women.
Results
In order to facilitate the interpretation of the
results, the data were divided by main themes as follows:
Adherence rate
In the 19 studies analysed, a rate of adherence to
MAM in the last 2 years was obtained, with percentages ranging from
10.1 to 80.2%, with a mean (x)=49.7% and a median (M)=52.5%. By
contrast, the rates of adherence to MAM at one point during the
womens' lifetimes varied between 29.9 and 90%, with x=63.5% and
M=71%. Regarding adherence to CBE in the last 2 years, the rates
ranged from 5.6 to 31.9%, with x=18.7% and M=18.6% (details are
available in Table SI) (17-20,23-30).
Sociodemographic factors
Sociodemographic determinants were extensively
mentioned in the articles analyzed. The most frequently mentioned
obstacles were economic factors, education and age.
Economic factors were associated with screening
uptake in 3 studies: Farzaneh et al (23) stated that high-income Azeri women
living in Iran had a higher chance of ever having a MAM [odds ratio
(OR)=8.7, 95% confidence interval (CI): 2.3-24.3]; Vahabi et
al (21) concluded that
immigrant Muslim women in Canada who resided in low-income
neighbourhoods had a lower chance of getting screened (OR=0.93, 95%
CI: 0.92-0.91); finally, De Andrade Souza et al (19) reported that receiving government aid
in the Amazonian community was associated with lower screening
adherence (OR=2.27, 95% CI: 1.14-4.52).
Educational status was also widely evaluated, with
conflicting results: Lee et al (31) stated that more years of education
were associated with a lower adherence to screening, both MAM and
CBE, in Korean Americans (OR=0.77 and 0.82, respectively); however,
De Andrade Souza et al (19)
concluded that Amazonian women who attended primary school (only)
were almost 2 times more likely to not seek screening compared with
women with a higher educational level (OR=1.98, 95% CI: 1.58-2.05);
Guo et al (20) also stated
that African American women had 11% more chance of getting screened
if they had a higher educational level (OR=1.11, P<0.05). This
item was also mentioned by Pilkington et al (24) in a qualitative study as an important
factor affecting screening behaviours among Aboriginal women.
Another important finding was the association
between older age and a higher chance of screening, reported in 3
of the analysed articles: Korean immigrant women (OR=1.08),
reported by Lee et al (31);
African American women (OR=1.08), reported by Guo et al
(20); and Korean American women
(OR=1.12), reported by Lee et al (25).
Personal factors
Personal factors were extensively described in most
of the articles. The most frequently mentioned obstacles to MAM and
CBE were fear, distrust of health professionals or the healthcare
system and knowledge of the procedures.
Fear was described in four articles. Arab women and
ultra-orthodox Jewish women in particular, revealed having more
fears regarding cancer-related losses (26), which was associated with more
up-to-date CBE screening (OR=1.51, 95% CI: 1.19-3.00). In focus
groups, African American and African-born Muslim women in NYC
(22) stated negative perceptions
and fear relating to BC screening as a barrier; Appalachian
Kentucky women (32) mentioned
specifically fear of detection, while Aboriginal women (24) reported fear of results.
Distrust of health professionals or healthcare
system was also extensively reported. Korean immigrant women
(31) reported distrust of health
professionals, which was related to a lower chance of having a CBE
(OR=0.71). African American women (20) reported not trusting the physicians
as a barrier to either MAM or CBE (OR=0.44). The results from
Korean American women (27) in
relation to MAM revealed that trusting the healthcare providers was
associated with a better chance of having a screening done
(OR=1.14, 95% CI: 1.01-1.29), while distrust in the healthcare
system was associated with a lower chance of being screened
(OR=0.84; 95% CI: 0.72-0.99). In the study of Zorogastua et
al (22), African American and
African-born Muslim women in NYC mentioned medical mistrust as a
barrier to screening in focus-based groups. In relation to
healthcare, these women also reported only seeking medical
attention when necessary and belief in alternative medicine as
barriers to screening.
Knowledge of the procedure was also among the
obstacles described. Korean immigrant women (31) declared better knowledge of the
procedure as a facilitator in both MAM and CBE (OR=105.47 and
28.77, respectively). In focus-based groups, African American and
African-born Muslim women in NYC (22) mentioned lack of
knowledge/misconception as a barrier to screening, and Aboriginal
women (24) also described lack of
knowledge as a barrier. A total of 35% of US-based Latin American
women (28) reported
knowledge-based reasons for not adhering to BC screening.
Pain, embarrassment or discomfort are barriers often
described in focus-based groups. Particularly, Appalachian Kentucky
women mention pain and embarrassment associated with MAM screening
(32) and Aboriginal women mention
discomfort of the MAM screening (24), alongside shame and other
factors.
Some populations also reported lack of time. African
American women (20) reported lack
of the time to visit doctors as a significant barrier to both MAM
and CBE (OR=0.46). African American and African-born Muslim women
in NYC also mentioned lack of time as a barrier (22).
High self-efficacy is significantly described in two
articles. Assessing Azeri women living in Ardabil, northwest Iran
(23), showed that high
self-efficacy was associated with a higher change of having a
regular MAM (OR=2.56, 95% CI: 1.41-4.6). Similar results were
observed in Korean immigrant women (25), with self-efficacy serving as a
facilitator to MAM screening [adjusted OR (AOR)=3.07, 95% CI:
1.48-6.38]. Modesty was described by Chinese American women
(17) as being related to a lower
chance of having a MAM (OR=4.78, 95% CI: 2.11-10.85). In addition,
African American and African-born Muslim women in NYC mention
modesty in focus-based groups as a barrier to screening (22). English-, Arabic- and
Italian-speaking women living or working in Australia extensively
described emotional barriers (OR=0.72, 95% CI: 0.54-0.94) (33), whereas19% of US-based Latin American
women indicated psychological reasons for not adhering to BC
screening (28).
The spousal role was found to be significant in
first-generation of Korean American women married to Korean
American men (25). Health beliefs
and spousal support, particularly focused on importance of breast
cancer prevention, were significantly associated with a higher
chance of screening (AOR=2.25, 95% CI: 1.40-3.63). The wife's
perception of support received is also important for positive
screening behaviours (AOR=1.99, 95% CI: 1.14-3.48).
Perception of a higher risk of cancer is described
as a motivator for screening among Arab and ultra-orthodox Jewish
women (26), for both CBE and MAM
(AOR=1.93, 95% CI: 1.23-3.04 and AOR=3.22, 95% CI: 1.53-6.61,
respectively). Great confidence in screening efficacy is linked to
regular MAM and regular CBE uptake (OR=4.2, 95% CI: 1.9-9.3; and
OR=1.25, 95% CI: 1.2-1.3, respectively) in Azeri women living in
Ardabil, northwest Iran (23).
Perceiving greater advantages of CBE appears to favour CBE
screening in Arab and ultra-orthodox Jewish women (AOR=1.82, 95%
CI: 1.45-2.29) (26). Perceived
lack of need (OR=0.27, 95% CI: 0.13-0.58) and perceived lack of
access (OR=0.36, 95% CI: 0.16-0.82) appear to be significant
barriers in non-adherent Chinese American women (17). A total of 14% of US-based Latin
American women indicated no reason and 31% economic-based reasons
for non-adherence (28).
Ethnic, cultural and religious
factors
Factors associated with the participants culture and
religion were mentioned in a few articles, most of which had a
qualitative design. Shaw et al (29) revealed, through focus groups, that
spiritual and religious beliefs (for example, Aurat, fatalism and
black magic) play an important role in BC screening among Malay
women in Singapore. Furthermore, the confidence in traditional
medicine and the distrust in western practices among those women,
as well as the role of family and community ties and shared
beliefs, were also among the factors mentioned. In the qualitative
study conducted by Zorogastua et al (22), focus groups with African Muslim
women in the USA revealed 4 themes related to this topic: ‘Role of
religion’, ‘role of men’, ‘role of community’ and ‘stigma and
shame’.
In the last qualitative study, Pilkington et
al (24), through
semi-structured interviews, focus group discussions and yarning
circles, stated that perceived support was important to BC
screening adherence among Aboriginal women in West Australia.
Finally, Freund et al (26)
reported that, having higher religious belief scores was associated
with a lower MA uptake among Arab and ultra-orthodox Jewish women
in Israel (OR=0.62, 95% CI: 0.39-0.82).
External factors
Regarding factors external to the participants'
characteristics or cultural context, a few statistically
significant barriers were identified. The first, mentioned in at
least 6 of the articles analysed, is access to healthcare: Vahabi
et al (21) (Muslim women in
Canada) and Guo et al (20)
(African American women) assessed that not having a primary care
physician reduced the odds of screening adherence (OR=0.20 and
0.71, respectively); Hong et al (27) stated that Korean American women with
regular doctors or healthcare centres were nearly 30 times more
likely to get screened (OR=29.91; 95% CI: 3.75-238.13); similarly,
Lee et al (25) concluded
that Korean American women were more adherent to screening if they
had regular access to healthcare (OR=2.44, 95% CI: 1.34-4.64); a
self-perceived lack of access to healthcare among Chinese American
women was associated with reduced chances of screening uptake
(OR=0.36, 95% CI: 0.16-0.82) in the study by Miller et al
(17); finally, having had a
medical consultation in the past year was associated with a lower
chance of non-adherence in Amazonian women (OR=0.16, 95% CI:
0.05-0.46) in the study by De Andrade Souza et al (19). Second, 4 articles analysed the
impact of having a positive reinforcement for screening: O'Hara
et al (33) stated that
receiving a screening invitation increased the odds of adherence
among English-, Arabic- and Italian-speaking women in Australia
(OR=3.46); having a physician's recommendation among Arab and
ultra-orthodox Jewish women (26)
was linked to an increased screening uptake (OR=1.82, 95% CI:
1.45-2.29); De Andrade Souza et al (19) stated that having been visited by a
healthcare agent lowered the odds of non-adherence to screening for
Amazonian women (OR=0.43, 95% CI: 0.22-0.85); the qualitative study
by Pilkington et al (24),
after conducting semi-structured interviews, focus group
discussions and yarning circles, suggested that a mobile van would
increase the screening adherence in the Aboriginal women community.
Third, the sex of the physician or healthcare provider was also
linked to screening adherence: Vahabi et al (21) assessed that having a male doctor
reduced the odds of Muslim immigrant women in Ontario seeking
screening (OR=0.88, 95% CI: 0.88-0.89), and Guo et al
(20) associated having a female
healthcare provider with an increased chance of adherence (OR=3.23)
among African American women. Finally, the qualitative study by
Cohen et al (32) stated,
through semi-structured interviews, that impersonal and
unprofessional MAM experiences adversely affected the screening
behaviours of Appalachian Kentucky women.
Discussion
According to the American Cancer Society (34), MAM rates are expected to increase to
90% among American women in the next few years. In our studies,
values have ranged from 43-75% at least once to 10.1-71.3% in the
last 2 years and 26-80.2% in the last year. According to the Cancer
Care Ontario (35), the goal was to
reach a 70% of MAM rate. The rates reported herein from the
minorities in Canada were 56.1 and 51% in the last 2 years, which
is considerably lower compared with the national target. The Breast
Screen Singapore (36) reported
that the programme aims to achieve a target of 70%. In the present
study, the adherence rate to MAM in the last 2 years was 44.4%,
which is lower compared with the set target. The Breast Screen
Australia data from 2014-2015(37)
show an adherence rate of 53.7%. In our cross-sectional study, a
MAM adherence of 69% was obtained, which is considered
satisfactory. According to the Israel Cancer Association, the
compliance to MAM among Arab women was 49% in 2001, whereas it is
currently similar to that of Jewish women at ~70% (38). The results of the present study were
quite contradictory, with Jewish ultra-Orthodox women having a
screening rate of 50.6% and Arab women 72.7%. In Brazil, the
findings revealed low national MAM coverage, with 32% in the 50-59
years age group and 25% in the 60-69 years age group (39). Although no more recent data were
included, the present study also demonstrated a low MAM coverage,
with a rate of 44.4% in the last 2 years.
Similar to the present findings, previous studies
reported an association between high income and higher BC screening
rates (40,41). Furthermore, our analysis is
concordant with the literature that also shows an association
between lower educational level and inadequate BC screening.
However, Lee et al (31)
reported that more years of education were associated with lower
adherence to BC screening in Korean American women. This may be
attributed to the fact that women with a higher level of education
may be more concerned of radiation exposure during MAM, which may
also act as a barrier (42,43).
Older age has been associated with a higher chance
of screening uptake among Korean immigrant (31), African American (20), and Korean American women (25). Surprisingly, no additional
evidence was found in the literature to support this hypothesis.
This is an important topic for future researches to consider in
order to be able to intervene.
The results of the present study suggest that fear
may act as both a motivator (when relating to cancer-related loss)
and as a barrier (when related to fear of the screening process or
diagnosis). The literature is contradictory, so a critical review
was performed to find a consensus for anxiety, worry and fear as BC
screening predictors (44). It was
suggested that fear has diverse effects on screening behaviour,
with a specific association of lower adherence with higher fear
(45). Similar to our review, it
was hypothesized that the fear of cancer may favour screening. Fear
of negative outcomes appeared to occupy a middle ground in terms of
impact on screening behaviour. Furthermore, a systematic review of
qualitative studies found that a common barrier to BC screening was
fear of a positive screening result and of pain associated with the
procedure (45).
Distrust of healthcare professionals or system,
according to our findings, was correlated with lower adherence in
four studies, which mention three immigrant minorities in the USA:
Korean, African American and African-born Muslim women. According
to the literature, distrust of the healthcare system is known as a
significant predictor of the last CBE and MAM (46). In a review about this topic, none of
the studies analyzed reported a positive association between
distrust and care (47).
In our findings, lack of knowledge or misconception
about the procedure was an obstacle described by Korean immigrant,
African American, African-born Muslim, Aboriginal and US-based
Latin American women. Similarly, Chinese American women described
perceived lack of need as a barrier. In the review of qualitative
studies mentioned earlier, lack of knowledge about the screening
procedure was one of the most important barriers (45).
Pain and embarrassment were also important barriers
according to our findings, mentioned by Appalachian Kentucky and
Aboriginal women in focus-based groups. In the review of
qualitative studies, fear of pain was a common factor (45). Most women also mentioned
embarrassment as a barrier, particularly when the healthcare
professional was male. By contrast, another study concluded that
the majority of women described MAM as painful, but relatively few
indicated that the pain may deter them from future screening
(48).
Highly religious women, as well as those who believe
in black magic and other curative methods, were less likely to seek
screening. These women often placed more trust in alternative
medicine rather than in western practices (29,49).
Another conviction that diminished adherence was
faith in destiny. These findings are controversial in the
literature, with some articles reporting that religious women are
more likely to undergo screening (50,51).
Therefore, it would be of value assessing each
religion separately in order to be able to correctly address this
issue in clinical practice.
As regards the role of family, men and cultural
factors, the effects on BC screening uptake are also distinct.
Family is important for encouraging women to undergo screening
(52), while the cultural context
can often function as a barrier to screening, due to the stigma
associated with cancer diagnosis in some cultures (53). The role of men is quite pronounced
and restraining in some cultures, with disapproval and forbidding
of screening, particularly if the physician is male (54). In conclusion, it is important to
study these issues among different contexts, preferably with
qualitative methods, in order to improve clinical approach to
non-adherent women.
The articles that explored access to healthcare were
unanimous in the conclusion that women with higher self-perceived
access, primary care physicians and regular medical consultations
are more likely to seek BC screening (55). This statement is concordant with the
literature. Having a regular primary care provider is known to
promote screening and the potential explanation is that these
professionals help with reminding and managing patients' clinical
examinations (56-59).
The articles that evaluated the impact of bringing
healthcare providers closer to women that need screening, for
example with screening invitations, have all concluded that this
type of dynamics improved the adherence to screening. These
findings are similar to those found in the literature (60). The remarkable role of some religious
institutions that provide means and education to women attending
church, should also be mentioned (61).
The sex of the physician was also found to play an
important role, with a higher adherence among patients who have a
female doctor. The literature suggests that this may be associated
with the differences in the beliefs of male and female primary care
providers regarding screening (30).
There were certain appreciable limitations to the
present study. First, the sample may not be representative of all
minorities. Second, the used methods, selection process, data
collection, screening and age range differed among the studies. The
adherence rate was also measured at different intervals. Finally, a
number of the studies included were conducted in the USA, where
screening may require payment, which may not be comparable to other
health services.
Evidence was found that BC screening adherence among
women that belong to minority groups depends on several factors,
such as sociodemographic (high income, educational level and age);
personal (fear, distrust of health professionals or healthcare
system, lack of knowledge and pain or discomfort); ethical,
cultural and religious (religious beliefs, role of men, family and
community) and external (access to healthcare, sex of the physician
and efforts to bring healthcare facilities closer to women). For
lowering the level of distrust and discomfort, it may be useful to
assign a female physician in certain cases, considering that women
may feel more comfortable with healthcare professionals of the same
sex (62,63). The lack of knowledge may be
addressed by distributing flyers and organizing informative
sessions on BC screening. This may also help to reduce womens' fear
of screening, cancer detection and its consequences. It may also be
valuable to establish a mobile screening program (e.g., in the form
of a van), in order to deal with distrust in the healthcare system
and other potential logistic barriers. The pain associated with MAM
is inevitable to a certain extent, but training technicians to be
aware and support women through the procedure may help minimize
discomfort. It would be beneficial to consider the different
backgrounds of the women that seek screening. Including husbands
and partners in clinical consultations, with the patient's consent,
may be a method for increasing adherence. Finally, taking into
consideration that having a regular primary care provider promote
screening adherence, health policies related to BC prevention
should aim to prioritize primary healthcare.
Supplementary Material
Supplementary Data
Acknowledgements
Not applicable.
Funding
The present study was developed under the scope of project
NORTE-01-0145-FEDER- 000013, supported by the Northern Portugal
Regional Operational Programme (NORTE 2020) under the Portugal
Partnership Agreement, through the European Regional Development
Fund (FEDER), and by National funds, through the Foundation for
Science and Technology (FCT)-project UIDB/50026/2020 and
UIDP/50026/2020.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Author's contributions
CSF, JR and SM are accountable for the integrity of
this work, in particular its design, literature search, data
collection and interpretation, quality assessment and manuscript
preparation. FR contributed to the systematic review assessment and
interpretation. ALF contributed to the conception and design and
critical revision of the manuscript for important intellectual
content. All the authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization: WHO|Breast
cancer. https://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/.
Accessed March 22, 2020.
|
|
2
|
Morrell S, Taylor R, Roder D and Dobson A:
Mammography screening and breast cancer mortality in Australia: An
aggregate cohort study. J Med Screen. 19:26–34. 2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nelson HD, Fu R, Cantor A, Pappas M,
Daeges M and Humphrey L: Effectiveness of breast cancer screening:
Systematic review and meta-analysis to update the 2009 U.S.
Preventive services task force recommendation. Ann Intern Med.
164:244–255. 2016.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Roder D, Houssami N, Farshid G, Gill G,
Luke C, Downey P, Beckmann K, Iosifidis P, Grieve L and Williamson
L: Population screening and intensity of screening are associated
with reduced breast cancer mortality: Evidence of efficacy of
mammography screening in Australia. Breast Cancer Res Treat.
108:409–416. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Morrell S, Taylor R, Roder D, Robson B,
Gregory M and Craig K: Mammography service screening and breast
cancer mortality in New Zealand: A National Cohort Study 1999-2011.
Br J Cancer. 116:828–839. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Niell BL, Freer PE, Weinfurtner RJ, Arleo
EK and Drukteinis JS: Screening for breast cancer. Radiol Clin
North Am. 55:1145–1162. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Coleman C: Early detection and screening
for breast cancer. Semin Oncol Nurs. 33:141–155. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Moss SM, Nyström L, Jonsson H, Paci E,
Lynge E, Njor S and Broeders M: Euroscreen Working Group. The
impact of mammographic screening on breast cancer mortality in
Europe: A review of trend studies. J Med Screen. 19 (Suppl
1):S26–S32. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Van Schoor G, Moss SM, Otten JD, Donders
R, Paap E, den Heeten GJ, Holland R, Broeders MJ and Verbeek AL:
Increasingly strong reduction in breast cancer mortality due to
screening. Br J Cancer. 104:910–914. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Puliti D and Zappa M: Breast cancer
screening: Are we seeing the benefit? BMC Med.
10(106)2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Veitch D, Goossens R, Owen H, Veitch J,
Molenbroek J and Bochner M: Evaluation of conventional training in
Clinical Breast Examination (CBE). Work. 62:647–656.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Greenwald ZR, Fregnani JH, Longatto-Filho
A, Watanabe A, Mattos JSC, Vazquez FL and Franco EL: The
performance of mobile screening units in a breast cancer screening
program in Brazil. Cancer Causes Control. 29:233–241.
2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lopes LV, Miguel F, Freitas H, Tavares A,
Pangui S, Castro C, Lacerda GF, Longatto-Filho A, Weiderpass E and
Santos LL: Stage at presentation of breast cancer in Luanda,
Angola-a retrospective study. BMC Health Serv Res.
15(471)2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Talley CH, Yang L and Williams KP: Breast
cancer screening paved with good intentions: Application of the
information-motivation-behavioral skills model to racial/ethnic
minority women. J Immigr Minor Health. 19:1362–1371.
2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Mauad EC, Nicolau SM, Moreira LF, Haikel
RL, Longatto-Filho A and Baracat EC: Adherence to cervical and
breast cancer programs is crucial to improving screening
performance. Rural Remote Health. 9(1241)2009.PubMed/NCBI
|
|
16
|
Mauad EC, Silvay TB, Haikel RL, Bauab S
and Longatto-Filhoy A: Is community intervention in breast cancer
screening in Brazil feasible? J Med Screen. 18(51)2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Miller BC, Sarma EA, Sun Y, Messina CR and
Moyer A: Psychosocial predictors of mammography history among
Chinese American women without a recent mammogram. Ethn Health.
25:862–873. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Adu PA, Ukah UV and Palmer SD: Association
between recency of immigration and mammography uptake: Results from
a Canadian National Survey. J Immigr Minor Heal. 19:228–235.
2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
De Andrade Souza CI, Araújo DS, Teles DA,
Carvalho SG, Cavalcante KW, Rabelo WL, Alves CN and Fonseca AJ:
Factors related to non-adherence to mammography in a city of the
Brazilian Amazonian area: A population-based study. Rev Assoc Med
Bras (1992). 63:35–42. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Guo Y, Cheng TC and Lee HY: Factors
associated with adherence to preventive breast cancer screenings
among middle-aged African American women. Soc Work Public Health.
34:646–656. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Vahabi M, Lofters A, Kim E, Wong JP,
Ellison L, Graves E and Glazier RH: Breast cancer screening
utilization among women from Muslim majority countries in Ontario,
Canada. Prev Med. 105:176–183. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zorogastua K, Sriphanlop P, Reich A, Aly
S, Cisse A and Jandorf L: Breast and cervical cancer screening
among US and non US born African American Muslim Women in New York
City. AIMS PUBLIC Health. 4:78–93. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Farzaneh E, Heydari H, Shekarchi AA and
Kamran A: Breast and cervical cancer-screening uptake among females
in Ardabil, northwest Iran: A community-based study. Onco Targets
Ther. 10:985–992. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Pilkington L, Haigh MM, Durey A,
Katzenellenbogen JM and Thompson SC: Perspectives of Aboriginal
women on participation in mammographic screening: A step towards
improving services. BMC Public Health. 17(697)2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Lee EE, Nandy K, Szalacha L, Park H, Oh
KM, Lee J and Menon U: Korean American women and mammogram uptake.
J Immigr Minor Heal. 18:179–186. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Freund A, Cohen M and Azaiza F: Factors
associated with routine screening for the early detection of breast
cancer in cultural-ethnic and faith-based communities. Ethn Health.
24:527–543. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hong HC, Ferrans CE, Park C, Lee H, Quinn
L and Collins EG: Effects of Perceived Discrimination and Trust on
Breast Cancer Screening among Korean American Women. Womens Health
Issues. 28:188–196. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Molina Y, Plascak JJ, Patrick DL, Bishop
S, Coronado GD and Beresford SAA: Neighborhood predictors of
mammography barriers among US-based latinas. J Racial Ethn Heal
Disparities. 4:233–242. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Shaw T, Ishak D, Lie D, Menon S, Courtney
E, Li ST and Ngeow J: The influence of Malay cultural beliefs on
breast cancer screening and genetic testing: A focus group study.
Psychooncology. 27:2855–2861. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wildes KA, Nápoles-Springer A,
Pérez-Stable E, Talavera G and Rios E: Physician gender differences
in general and cancer-specific prevention attitudes and practices.
J Cancer Educ. 24:85–93. 2009.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Lee HY, Lee MH, Jang YJ and Lee DK: Breast
cancer screening disparity among Korean American immigrant women in
midwest. Asian Pac J Cancer Prev. 18:2663–2667. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Cohen EL, Wilson BR, Vanderpool RC and
Collins T: Identifying sociocultural barriers to mammography
adherence among Appalachian Kentucky Women. Health Commun.
31:72–82. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
O'Hara J, McPhee C, Dodson S, Cooper A,
Wildey C, Hawkins M, Fulton A, Pridmore V, Cuevas V, Scanlon M, et
al: Barriers to breast cancer screening among diverse cultural
groups in Melbourne, Australia. Int J Environ Res Public Health.
15(1677)2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Ma J, Jemal A, Fedewa SA, Islami F,
Lichtenfeld JL, Wender RC, Cullen KJ and Brawley OW: The American
Cancer Society 2035 challenge goal on cancer mortality reduction.
CA Cancer J Clin. 69:351–362. 2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Brouwers MC, De Vito C, Bahirathan L,
Carol A, Carroll JC, Cotterchio M, Dobbins M, Lent B, Levitt C,
Lewis N, et al: What implementation interventions increase cancer
screening rates? a systematic review. Implement Sci.
6(111)2011.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Yeoh KG, Chew L and Wang SC: Cancer
screening in Singapore, with particular reference to breast,
cervical and colorectal cancer screening. J Med Screen. 13 (Suppl
1):S14–S19. 2006.PubMed/NCBI
|
|
37
|
Australian Institute of Health and
Welfare: Breast Screen Australia Monitoring Report 2006-2007 and
2007-2008. Canberra, 2010. AIHW, Canberra, Cancer series no. 55.
Cat. no. CAN 51, 2010.
|
|
38
|
Israel Cancer Association. The Israel
Cancer Association-Colorectal Cancer. http://en.cancer.org.il/template_e/default.aspx?PageId=7747.
Accessed March 25, 2020.
|
|
39
|
Azevedo e Silva G, Bustamante-Teixeira MT,
Aquino EML, Tomazelli JG and dos-Santos-Silva I: Acesso à detecção
precoce do câncer de mama no sistema Único de saúde: Uma análise a
partir dos dados do sistema de informações em saúde. Cad Saude
Publica. 30:1537–1550. 2014.PubMed/NCBI View Article : Google Scholar : (In
Portuguese).
|
|
40
|
Moser K, Patnick J and Beral V:
Inequalities in reported use of breast and cervical screening in
Great Britain: Analysis of cross sectional survey data. BMJ.
338(b2025)2009.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Nuche-Berenguer B and Sakellariou D:
Socioeconomic determinants of cancer screening utilisation in Latin
America: A systematic review. PLoS One. 14(e0225667)2019.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Davis TC, Arnold C, Berkel HJ, Nandy I,
Jackson RH and Glass J: Knowledge and attitude on screening
mammography among low-literate, low- income women. Cancer.
78:1912–1920. 1996.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Davis TC, Williams MV, Marin E, Parker RM
and Glass J: Health Literacy and Cancer Communication. CA Cancer J
Clin. 52:134–149. 2002.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Consedine NS, Magai C, Krivoshekova YS,
Ryzewicz L and Neugut AI: Fear, anxiety, worry, and breast cancer
screening behavior: A critical review. Cancer Epidemiol Biomarkers
Prev. 13:501–510. 2004.PubMed/NCBI
|
|
45
|
Azami-Aghdash S, Ghojazadeh M, Sheyklo SG,
Daemi A, Kolahdouzan K, Mohseni M and Moosavi A: Breast cancer
screening barriers from the womans perspective: A meta-synthesis.
Asian Pacific J Cancer Prev. 16:3463–3471. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Katapodi MC, Pierce PF and Facione NC:
Distrust, predisposition to use health services and breast cancer
screening: Results from a multicultural community-based survey. Int
J Nurs Stud. 47:975–983. 2010.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Mouslim MC, Johnson RM and Dean LT:
Healthcare system distrust and the breast cancer continuum of care.
Breast Cancer Res Treat. 180:33–44. 2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Keemers-Gels ME, Groenendijk RP, van den
Heuvel JH, Boetes C, Peer PG and Wobbes TH: Pain experienced by
women attending breast cancer screening. Breast Cancer Res Treat.
60:235–240. 2000.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Elewonibi B and BeLue R: The influence of
socio-cultural factors on breast cancer screening behaviors in
Lagos, Nigeria. Ethn Heal. 24:544–559. 2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
O'Reilly D, Kinnear H, Rosato M, Mairs A
and Hall C: Uptake of breast screening is influenced by current
religion and religion of upbringing. J Relig Health. 52:1168–1176.
2013.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Fox SA, Pitkin K, Paul C, Carson S and
Duan N: Breast cancer screening adherence: Does church attendance
matter? Health Educ Behav. 25:742–758. 1998.PubMed/NCBI View Article : Google Scholar
|
|
52
|
McEwan J, Underwood C and Corbex M:
Injustice! that is the cause: A qualitative study of the social,
economic, and structural determinants of late diagnosis and
treatment of breast cancer in Egypt. Cancer Nurs. 37:468–475.
2014.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Lee SY: Cultural factors associated with
breast and cervical cancer screening in Korean American Women in
the US: An integrative literature review. Asian Nurs Res (Korean
Soc Nurs Sci). 9:81–90. 2015.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Kawar LN: Barriers to breast cancer
screening participation among Jordanian and Palestinian American
women. Eur J Oncol Nurs. 17:88–94. 2013.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Glazier RH, Klein-Geltink J, Kopp A and
Sibley LM: Capitation and enhanced fee-for-service models for
primary care reform: A population-based evaluation. CMAJ.
180:E72–E81. 2009.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Todd L, Harvey E and Hoffman-Goetz L:
Predicting breast and colon cancer screening among
English-as-a-second- language older Chinese immigrant women to
Canada. J Cancer Educ. 26:161–169. 2011.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Alexandraki I and Mooradian AD: Barriers
related to mammography use for breast cancer screening among
minority women. J Natl Med Assoc. 102:206–218. 2010.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Gierisch JM, O'Neill SC, Rimer BK, DeFrank
JT, Bowling JM and Skinner CS: Factors associated with
annual-interval mammography for women in their 40s. Cancer
Epidemiol. 33:72–78. 2009.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Baron RC, Melillo S, Rimer BK, Coates RJ,
Kerner J, Habarta N, Chattopadhyay S, Sabatino SA, Elder R and
Leeks KJ: Task Force on Community Preventive Services. Intervention
to increase recommendation and delivery of screening for breast,
cervical, and colorectal cancers by healthcare providers. A
systematic review of provider reminders. Am J Prev Med. 38:110–117.
2010.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Lurie N, Margolis KL, McGovern PG, Mink PJ
and Slater JS: Why do patients of female physicians have higher
rates of breast and cervical cancer screening? J Gen Intern Med.
12:34–43. 1997.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Perez LG, Elder JP, Haughton J, Martinez
ME and Arredondo EM: Socio-demographic moderators of associations
between psychological factors and Latinas' breast cancer screening
behaviors. J Immigrant and Minority Health. 20:823–830.
2018.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Smalls BL, Aroh A, McQuerry K, Adegboyega
A, Schoenberg N and Hatcher J: Social support and breast cancer
screening in rural Appalachia. Psychooncology. 27:2281–2288.
2018.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Valdovinos C, Penedo FJ, Isasi CR, Jung M,
Kaplan RC, Giacinto RE, Gonzalez P, Malcarne VL, Perreira K,
Salgado H, et al: Cancer Causes Control 27:27-37, 2016.
|