Introduction
Adenoid cystic carcinoma (ACC) is a rare tumor which
represents the majority of malignant neoplasms of the lacrimal
gland, with a 5-year survival rate of <20%. It has a poor
prognosis for long-term disease-free survival (1-3).
ACC has a tendency to recur both locally and with distant
metastases despite radical treatment (4). Surgery with subsequent radiotherapy
is considered a standard treatment for ACC of the lacrimal gland,
but complete resection in most cases is not feasible (National
Comprehensive Cancer Network Head and Neck Cancers, version 3.2021)
(5). There is no consensus on the
recommended treatment in cases of metastatic disease, and patients
are usually treated with platinum-based chemotherapy; however, this
approach has recently been challenged by immunotherapy (6,7).
In the present case report, a rare clinical case of
ACC of the lacrimal gland with multiple oligometastatic events that
were successfully treated by radiosurgery over a 2,5-year period is
presented. To the best of our knowledge, this is the first time
such a case has been reported.
Case report
A 44-year-old female patient presented with facial
asymmetry and pain in the left orbit, in April 2019, at the
European Medical Center (Moscow, Russia). The patient was evaluated
by an ophthalmologist, and the examination showed exophthalmos and
lower eyelid retraction on the left side. The patient had no other
complaints, normal vision, and an Eastern Cooperative Oncology
Group (ECOG) score of 1. Brain magnetic resonance imaging (MRI) was
recommended.
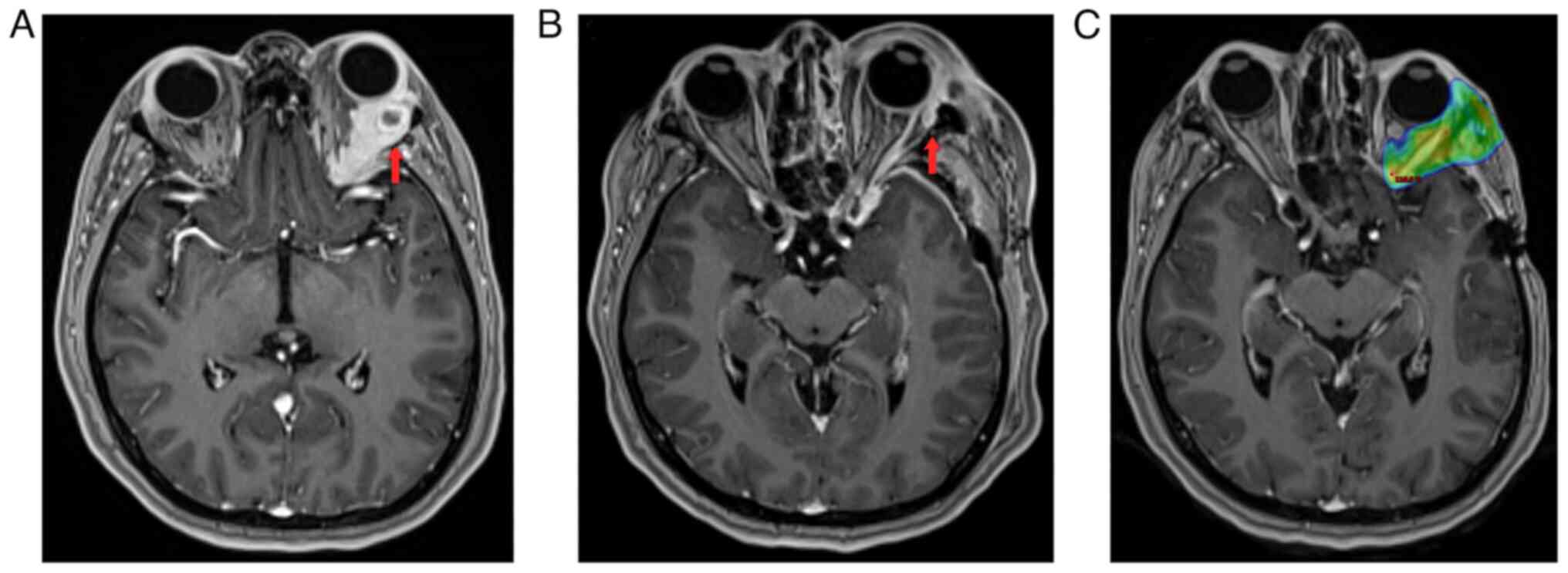
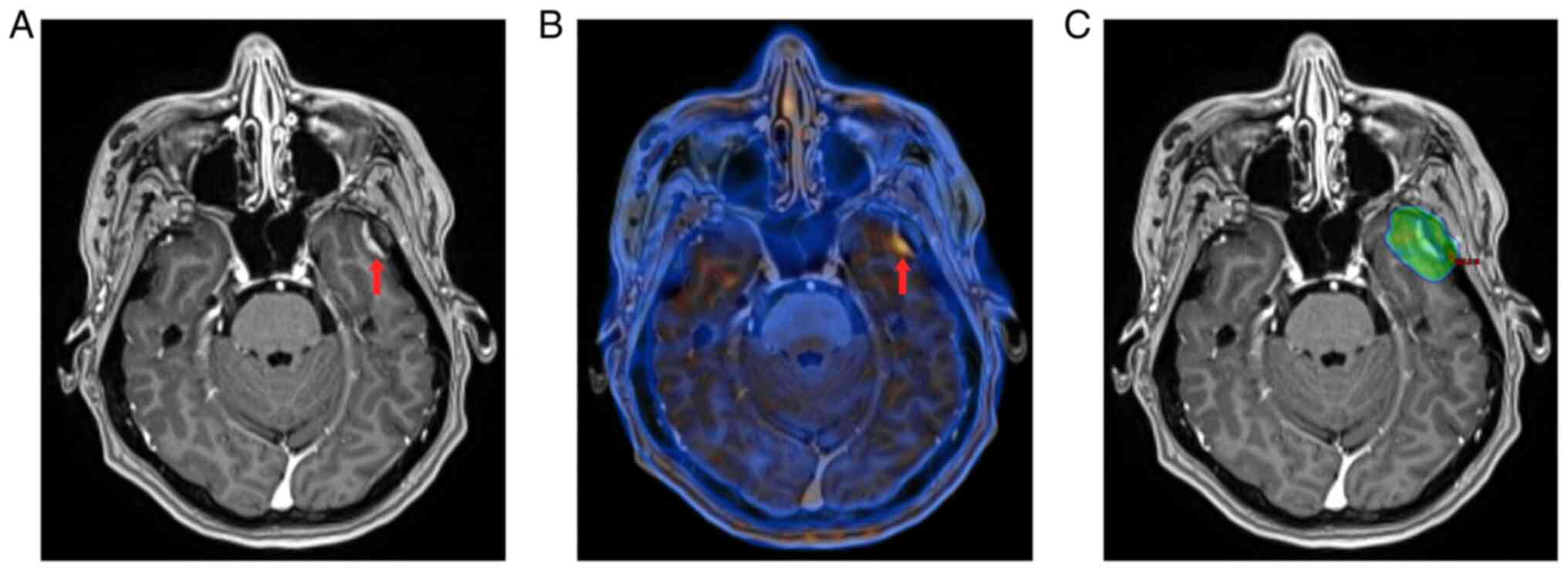
The initial brain MRI with intravenous (I/V)
contrast revealed a mass in the left orbit sized 4.0x2.1x3.5 cm
with sphenoid bone invasion (Fig.
1A). Upon suspicion of a malignant tumor, the patient underwent
microsurgical tumor excision (R2) in April 2019, during which the
eye was preserved. Pathology reports showed mix patterns of
cribriform and solid types of ACC with tumor cells expressing CK7,
CD117 with CK5/6 on some cells, S-100, and Ki-67 positive in 10-30%
of tumor cells; a final pathology stage was pT4bN0M0, R2, LV0 (no
lymphovascular invasion), Pn1 (perineural invasion). Molecular
genetic testing (Caris Life Sciences) provided no evidence of
microsatellite instability, low tumor mutational burden (six
mutations), negative PD-L1 status, and MYB, NOTCH,
and KRAS were not detected. Postoperative MRI images showed
a residual mass in the left orbit (Fig. 1B), and body positron emission
tomography-computed tomography (PET-CT) showed no evidence of
metastatic disease.
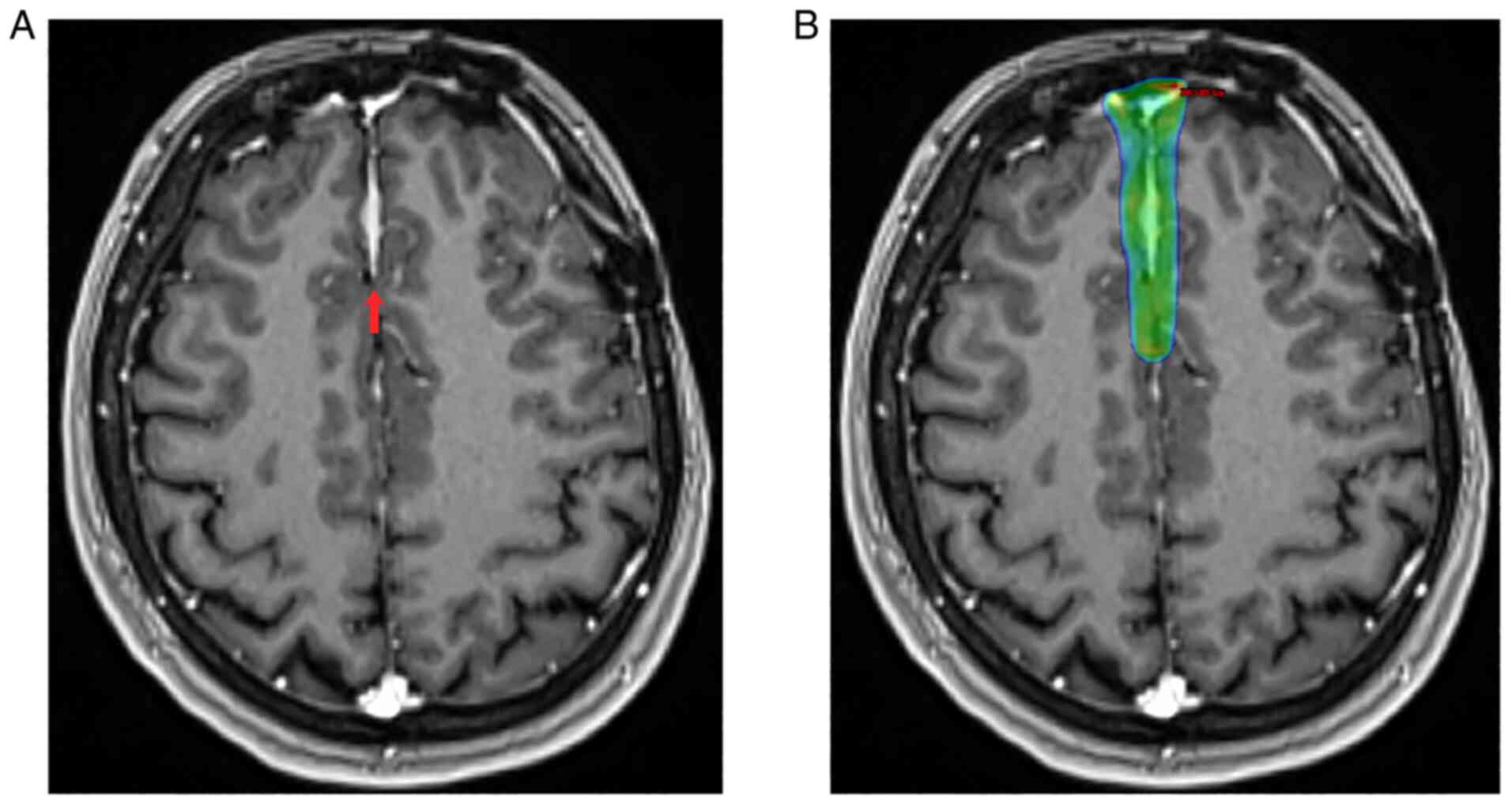
 | Figure 1(A) Brain MRI with I/V contrast before
surgery. The red arrow indicates a mass in the left orbit sized
4.0x2.1x3.5 cm with sphenoid bone invasion. (B) Brain MRI with I/V
contrast after surgery. The red arrow indicates a residual mass in
the left orbit. (C) Mapping of the treated lesion of the patient,
based on the pre-irradiation therapy brain CT scan fused with the
brain MRI. The patient was simulated in the supine position with
the arms down, using a customized thermoplastic facemask for
immobilization. PTV was defined as PTV_45 (the left orbit), 1.8 Gy
per fraction; PTV_54 (tumor bed), 1.8 Gy per fraction (total dose,
54 Gy); and PTV_64.8 (residual contrast-enhancing tumor on
post-surgical MRI), 1.8 Gy per fraction (total dose, 64.8). Organs
at risk were delineated using the EclipseTM treatment
planning system (version 15.6; Varian Medical Systems).
Heterogeneity correction was used for planning. The prescribed
radiation treatment was completed. MRI, magnetic resonance imaging;
I/V, intravenous; CT, computed tomography; PTV, planning target
volume. |
Two weeks after surgery, the patient received
adjuvant radiation therapy with image-guided radiation therapy
(IGRT) using a volumetric modulated arc therapy (VMAT) technique to
the left orbit, tumor bed, and subclinical extension with a boost
to the tumor bed (total dose, 64.8 Gy) (Fig. 1C). Follow-up MRI images
demonstrated complete radiological response and no evidence of
active disease.
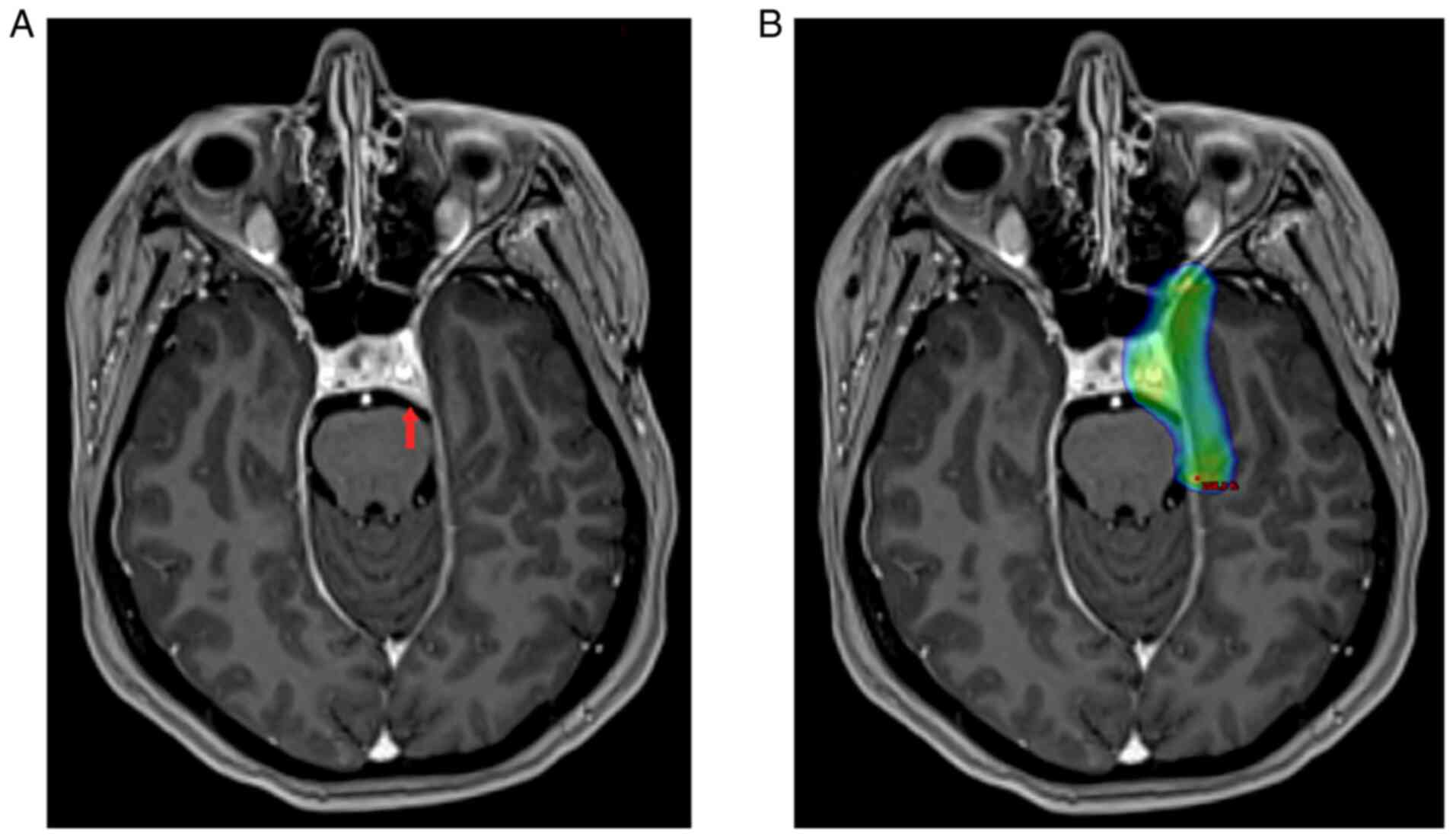
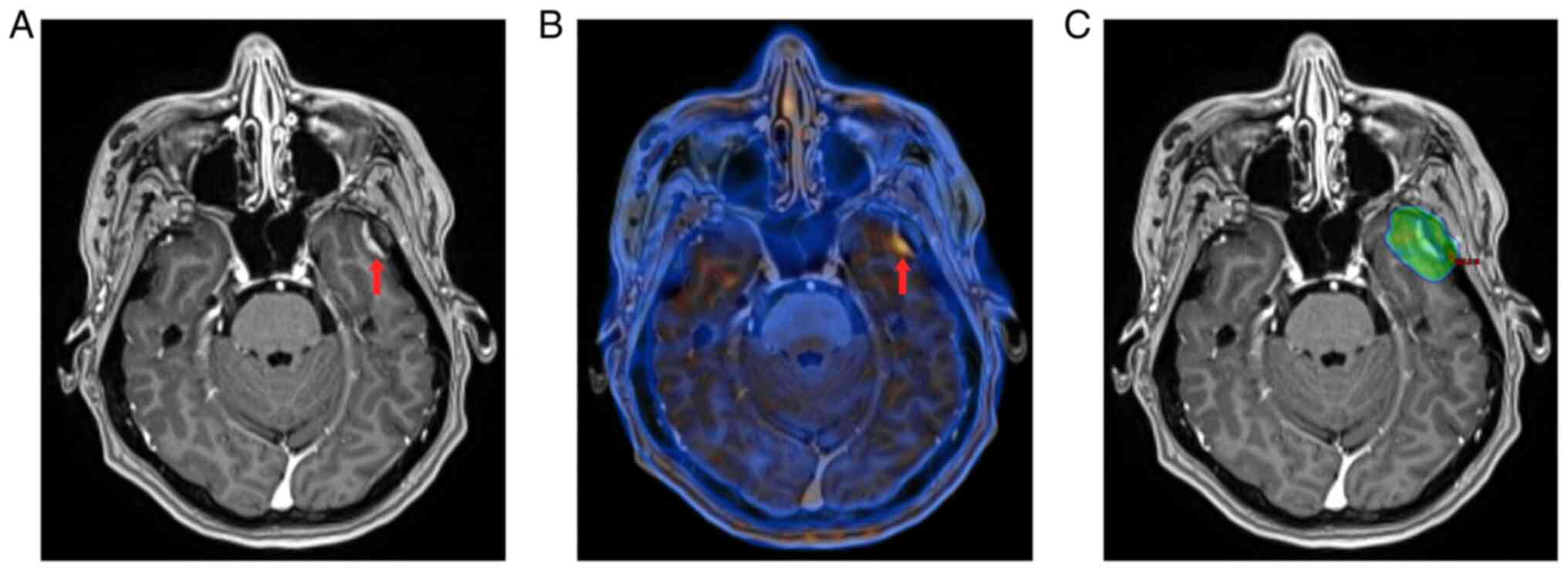
In December 2019, the MRI with I/V contrast revealed
a homogeneous contrast uptake near the left posterior cavernous
sinus (1.4x0.9 cm), outside of the radiation therapy fields
(Fig. 2A). The patient received
stereotactic fractionated radiation therapy (SFRT) to the left
posterior cavernous sinus with a total dose of 48 Gy (Fig. 2B). A follow-up MRI provided no
evidence of the disease.
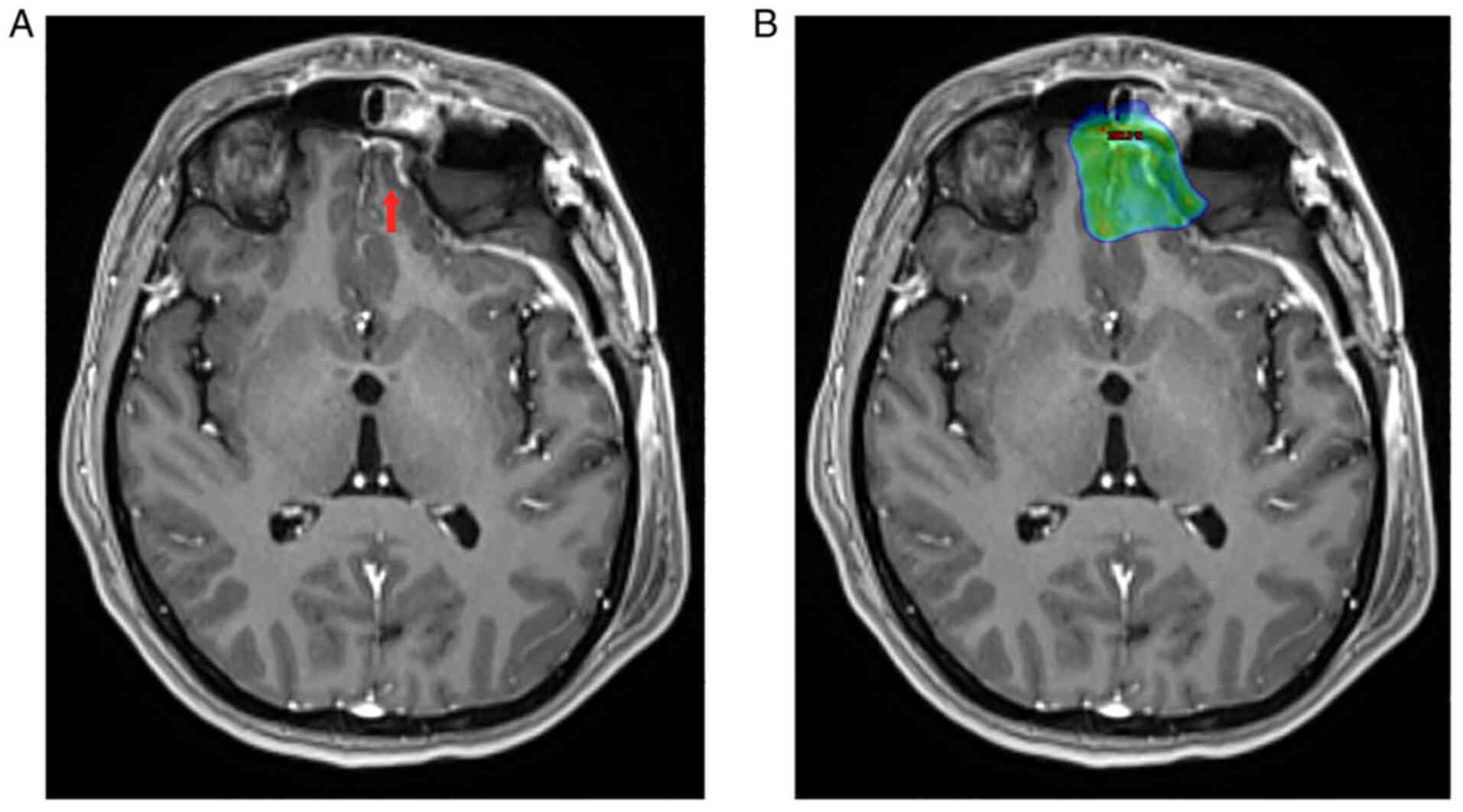
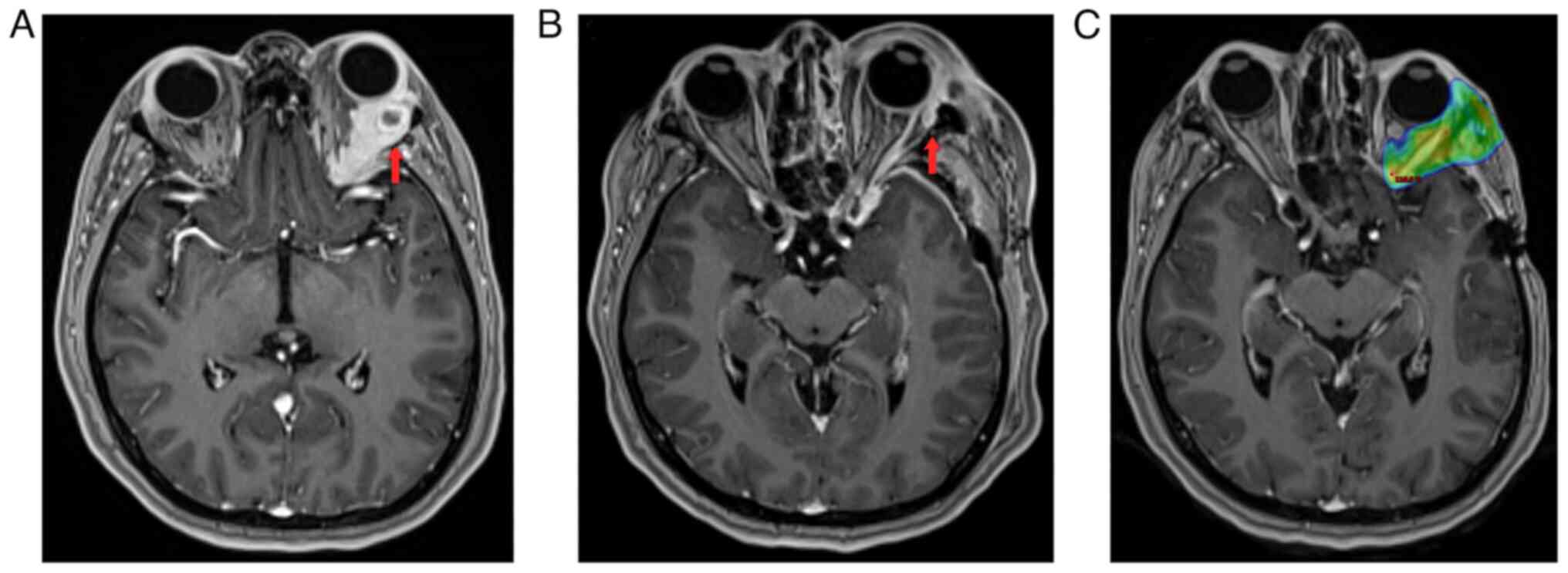
In April 2020, a brain MRI with I/V contrast showed
a new contrast-enhancing lesion on the surface of the left gyrus
rectus (Fig. 3A). A
multidisciplinary meeting recommended surgical excision to further
verify the histology of this lesion. On April 8 2020, the lesion
was removed and a pathology report confirmed metastasis of ACC.
Adjuvant radiation therapy to the postoperative area (a total dose,
33.0 Gy) was administered (Fig.
3B) with a complete radiological response.
In July 2020, an MRI scan revealed two meningeal
metastases in the temporal region along the postoperative tract
(Fig. 4A). In August 2020, the
patient underwent SFRT for the above mentioned lesions (a total
dose, 46.0 Gy), (Fig. 4B).
Follow-up MRI images showed complete radiological response.
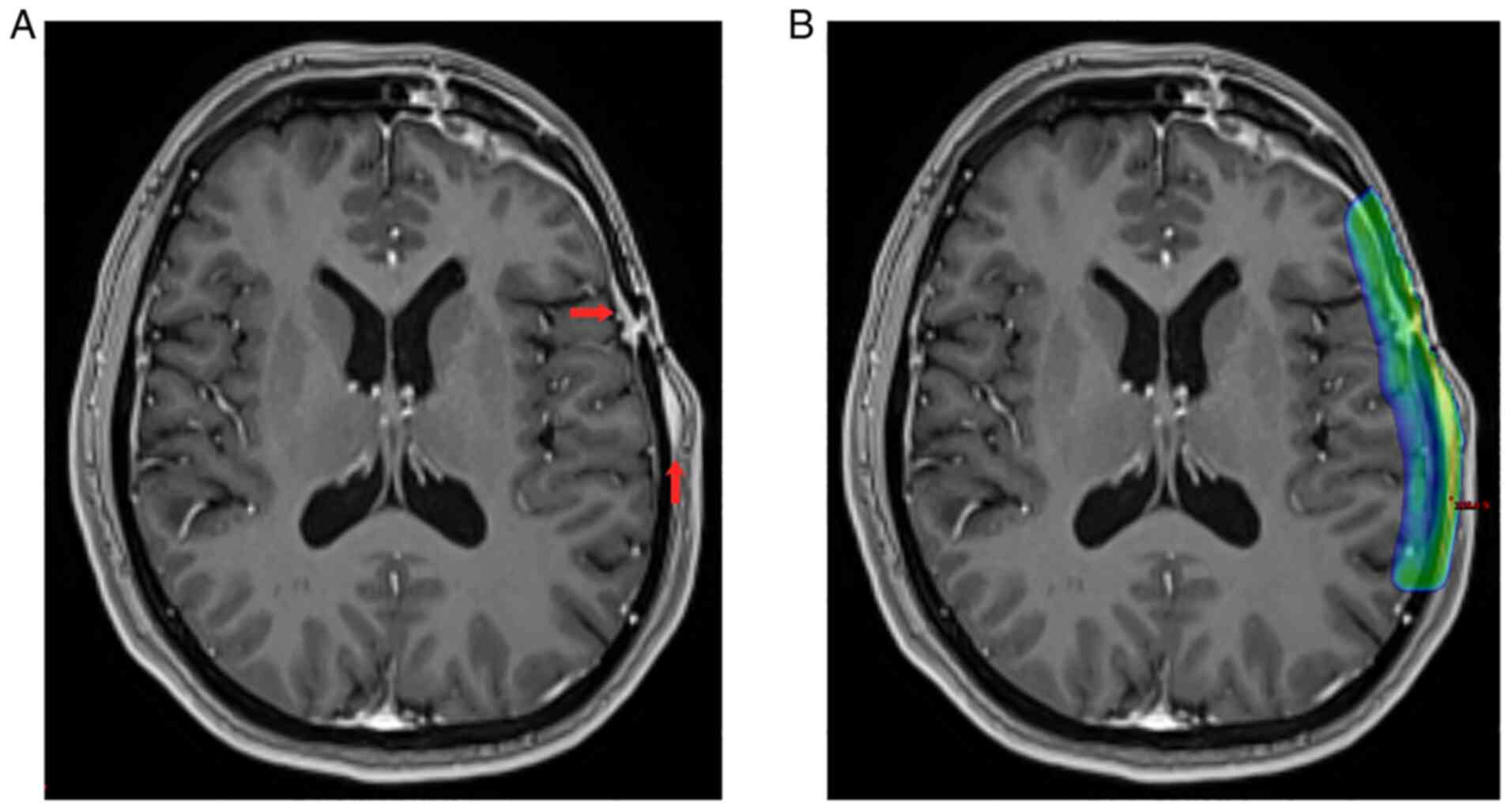 | Figure 4(A) Brain MRI with I/V contrast. The
red arrows indicate local thickening of the dura mater in the
region of postoperative burr holes in the temporal bone that
appears to be pachymeningeal recurrence, and similar solid
contrast-enhancing lesions in the soft tissue of the temporal
region that appears to be tumor progression. (B) Mapping of the
treated lesion of the patient, based on the pre-irradiation therapy
brain CT scan fused with the brain MRI. The patient was simulated
in the supine position with arms down, using a customized
thermoplastic facemask for immobilization. PTV was defined as two
lesions of local dura mater thickening in the region of
postoperative burr holes with subclinical extension, 3.5 Gy per
fraction (total dose, 28.0 Gy) with sequential boost, 3.0 Gy per
fraction (total dose, 46.0 Gy). Heterogeneity correction was used
for planning. The prescribed radiation treatment was completed.
MRI, magnetic resonance imaging; I/V, intravenous; CT, computed
tomography; PTV, planning target volume. |
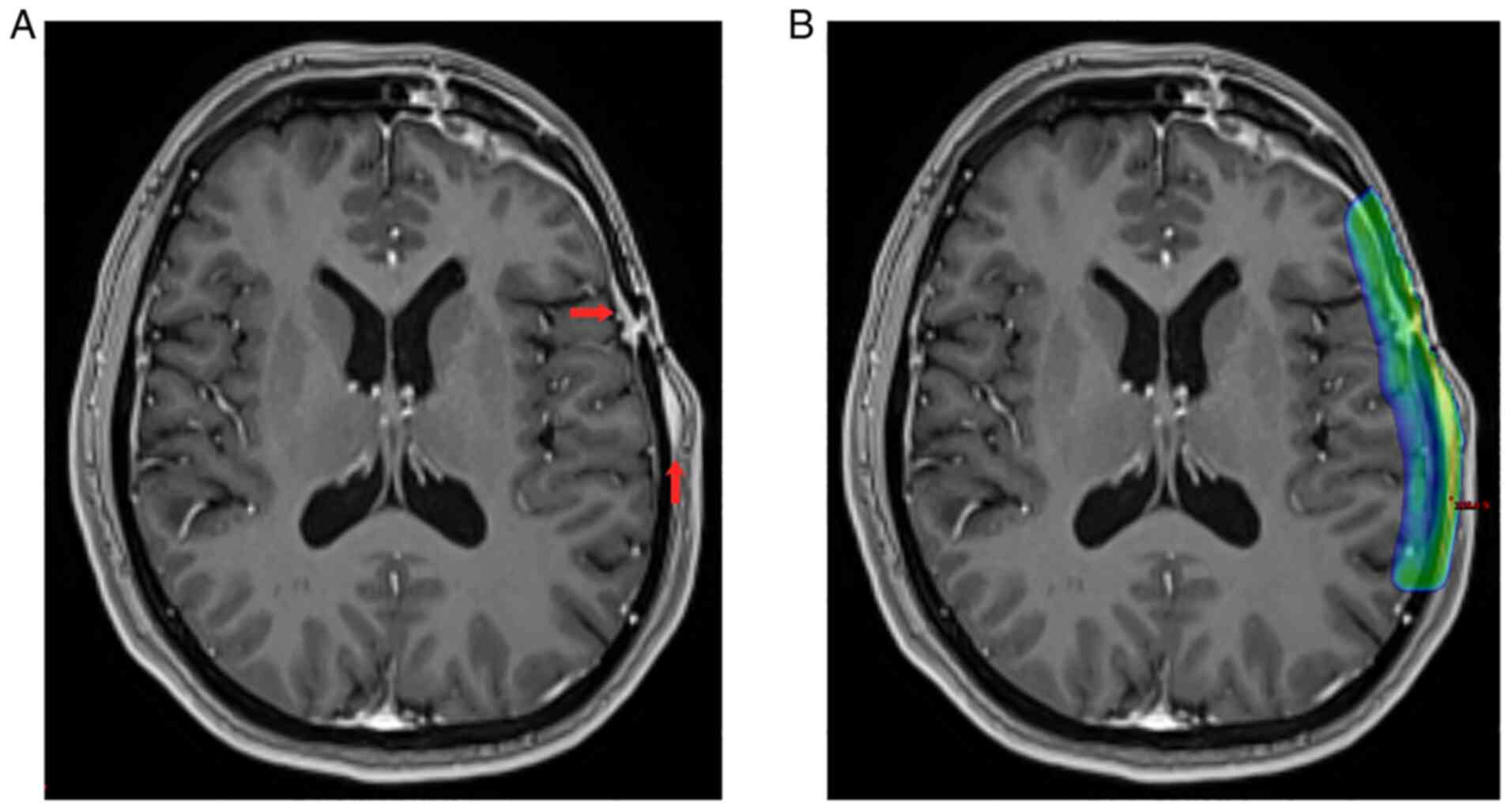
In January 2021, a brain MRI with I/V contrast
revealed a new contrast-enhancing lesion in the anterior part of
the falx cerebri (Fig. 5A). SFRT
was performed on this region (a total dose, 46.0 Gy) (Fig. 5B) in the same month. As of June
2021, the patient exhibited no evidence of residual disease.
In June 2021, an MRI with I/V contrast revealed a
new contrast-enhancing meningeal lesion of the left temporal lobe
(Fig. 6A). Head PET-CT
demonstrated solid dural metastasis in the region of the left
temporal lobe (SUVmax 2.95) (Fig.
6B). The planning target volume (PTV) of SFRT in the recurrence
area (a total dose, 46.0 Gy) in June-July 2021, is revealed in
Fig. 6C.
 | Figure 6(A) Brain MRI with I/V contrast. The
red arrow indicates a new contrast-enhancing pachymeningeal lesion
in the basal region of the left temporal lobe. (B) Head PET-CT. The
red arrow indicates solid dural metastasis in the left temporal
lobe (SUVmax 2.95). (C) Mapping of the treated lesion of the
patient, based on the pre-irradiation therapy brain CT scan fused
with the brain MRI. The patient was simulated in the supine
position with arms down, using a customized thermoplastic facemask
for immobilization. PTV was defined as a pachymeningeal lesion in
the basal region of the left temporal lobe with subclinical
extension, 3.5 Gy per fraction with sequential boost, 3.0 Gy per
fraction (total dose, 46.0 Gy). Heterogeneity correction was used
for planning. The prescribed radiation treatment was completed. CT,
computed tomography; I/V, intravenous; MRI, magnetic resonance
imaging; PET-CT, positron emission tomography-CT; PTV, planning
target volume. |
The final MRI and PET-CT scans from July 2021 showed
complete radiological response. The patient is currently living
with no evidence of disease and with a good quality of life.
Discussion
ACC of the lacrimal gland is a rare type of tumor
(8). Despite the lack of data on
large groups of patients, some authors recommend surgery followed
by radiation or proton therapy (9-11).
Others maintain that radical surgery should be incorporated into
the treatment and can improve control of the local disease, and
possibly, long-term survival (12,13).
Woo et al reviewed the published literature on management
strategies for lacrimal gland carcinomas from over the past 40
years and concluded that treatment strategies for ACC of the
lacrimal gland varied and local control did not necessarily prevent
future relapse. Improved radiation therapy techniques may offer
opportunities for the management of lacrimal gland carcinomas in
patients with unresectable disease (6). In the present case, radical surgery
was not possible due to bone invasion and due to the desire of the
patient, who, after receiving the histological report and a long
discussion with regard to the diagnosis and possible treatment
options, refused a radical surgical operation. In such cases,
radiotherapy remains the only viable treatment option.
Due to the impermeability of the blood-brain barrier
to numerous chemotherapeutic agents, there are no evidence-based
recommendations and there are no accepted standard chemotherapy
regimens for ACC. Additionally, the National Comprehensive Cancer
Network provides no recommendations regarding chemotherapy in this
context (http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf).
The effects of intra-arterial cytoreductive
chemotherapy with cisplatin + 5-FU or cisplatin, doxorubicin, and
cyclophosphamide (CAP) are currently being investigated, and
preliminary findings show poor results either as single agents or
as combination therapy (14,15).
Licitra et al described the cases of treatment with CAP, and
67% of patients achieved partial response or stable disease, but no
cases of complete response were reported (16). Previous research has revealed the
possibility of other treatment options, such as chemotherapy and
targeted therapy, based on genomic profiling (7,17).
In the present case, molecular genetic testing
(Caris Life Sciences) did not provide a sufficient basis for
alternative chemotherapy regimens.
Radiosurgery is a well-known and effective method
for the treatment of brain metastases. Results from a randomized,
controlled phase 3 trial presented at the American Society for
Radiation Oncology Annual Meeting in October 2020 suggested that
SRS should be the standard of care for patients with multiple brain
metastases (18). In addition, the
Radiation Therapy Oncology Group (RTOG) 9508 randomized trial
demonstrated that SRS improved survival in patients with single
brain metastases (19). Thus, SRS
was attempted as this was deemed as the only possible and safe
method for this patient.
In conclusion, a number of the rare defined disease
data on specific treatments and outcomes are not yet available.
Preliminary results confirmed that in the present case SRS achieved
excellent control of the six events of recurrence of the ACC
disease over 2,2 years, while other treatment options were not
possible. To date, the patient is still living with a good quality
of life, normal vision, no complications, and no evidence of
disease.
Unfortunately, this case was not presented to the
local Multidisciplinary Head and Neck Tumor Board (European Medical
Center, Moscow, Russia) before the first surgery. The surgery was
supposed to be diagnostic in order to obtain histological material.
The fact that the tumor was not radically removed and may have
affected the further course of the disease, is acknowledged.
Despite the efficiency, SRS has a number of
limitations such as limited availability, high price and
additionally, there is a paucity of professionals to commission,
utilize, and maintain safe and effective SRS practices in
developing countries. Furthermore, certain side effects such as
tiredness and swelling in the brain may occur in the first few
weeks after stereotactic radiosurgery. Swelling in the brain at or
near the treatment site can cause signs and symptoms such as
headaches, nausea and vomiting, which were not observed in the
present patient. Further clinical observation based on large groups
of patients is needed to evaluate this approach.
The present case is unique in our practice. Due to
the aggressive nature of the ACC and poor prognosis of this tumor
in the short/medium term the condition of the patient is
continually being monitored. The patient is also continuing to
undergo routine brain MRI with contrast every 3 months and PET-CT
every 6 months.
Acknowledgements
Not applicable.
Funding
Funding: The authors declare that no funds, grants, or other
support were received during the preparation of this
manuscript.
Availability of data and materials
Available from the corresponding author upon
reasonable request.
Authors' contributions
All authors (NS, EL, KT and IK) contributed to the
study conception and design. Material preparation, data collection
and analysis were performed by NS, KT and EL. The first draft of
the manuscript was written by KT and all authors commented on
previous versions of the manuscript. Images and description of MRI
results were prepared by IK. NS and KT confirm the authenticity of
all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Ethics approval for the study was obtained from the
Local Research Ethics Committee (European Medical Center, Moscow,
Russia) dated April 16, 2019. Informed consent was obtained from
the patient.
Patient consent for publication
Written consent for publication of this case report
including all images, was obtained from the patient.
Competing interests
The authors have no relevant financial or
non-financial interests to disclose.
References
|
1
|
Tse DT, Benedetto P, Dubovy S, Schiffman
JC and Feuer WJ: Clinical analysis of the effect of intraarterial
cytoreductive chemotherapy in the treatment of lacrimal gland
adenoid cystic carcinoma. Am J Ophthalmol. 141:44–53.
2006.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bernardini FP, Devoto MH and Croxatto JO:
Epithelial tumors of the lacrimal gland: An update. Curr Opin
Ophthalmol. 19:409–413. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
von Holstein SL, Fehr A, Persson M,
Therkildsen MH, Prause JU, Heegaard S and Stenman G: Adenoid cystic
carcinoma of the lacrimal gland: MYB gene activation, genomic
imbalances, and clinical characteristics. Ophthalmology.
120:2130–2138. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sanders JC, Mendenhall WM and Werning JW:
Adenoid cystic carcinoma of the lacrimal gland. Am J Otolaryngol.
37:144–147. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Han J, Kim YD, Woo KI and Sobti D:
Long-term outcomes of eye-sparing surgery for adenoid cystic
carcinoma of lacrimal gland. Ophthalmic Plast Reconstr Surg.
34:74–78. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Woo KI, Yeom A and Esmaeli B: Management
of lacrimal gland carcinoma: Lessons from the literature in the
past 40 years. Ophthalmic Plast Reconstr Surg. 32:1–10.
2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chae YK, Chung SY, Davis AA, Carneiro BA,
Chandra S, Kaplan J, Kalyan A and Giles FJ: Adenoid cystic
carcinoma: Current therapy and potential therapeutic advances based
on genomic profiling. Oncotarget. 6:37117–37134. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mallen-St Clair J, Arshi A, Tajudeen B,
Abemayor E and St John M: Epidemiology and treatment of lacrimal
gland tumors: A population-based cohort analysis. JAMA Otolaryngol
Head Neck Surg. 140:1110–1116. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lesueur P, Rapeaud E, Marzi LD, Goudjil F,
Levy C, Galatoire O, Jacomet PV, Dendale R and Calugaru V: Adenoid
cystic carcinoma of the lacrimal gland: High dose adjuvant proton
therapy to improve patients outcomes. Front Oncol.
10(135)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Polanowski PA, Księżniak-Baran DA,
Grządziel AB, Pietruszka A, Chmielik E, Pilecki B, Amrogowicz N,
Gajda K and Składowski K: Successful treatment of adenoid cystic
carcinoma with the application of a high-dose stereotactic body
radiotherapy boost. Case Rep Oncol. 14:371–377. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wang CC and Goodman M: Photon irradiation
of unresectable carcinomas of salivary glands. Int J Radiat Oncol
Biol Phys. 21:569–576. 1991.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mendenhall WM, Morris CG, Amdur RJ,
Werning JW, Hinerman RW and Villaret DB: Radiotherapy alone or
combined with surgery for adenoid cystic carcinoma of the head and
neck. Head Neck. 26:154–162. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Esmaeli B, Golio D, Kies M and DeMonte F:
Surgical management of locally advanced adenoid cystic carcinoma of
the lacrimal gland. Ophthalmic Plast Reconstr Surg. 22:366–370.
2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
De Haan LD, De Mulder PH, Vermorken JB,
Schornagel JH, Vermey A and Verweij J: Cisplatin-based chemotherapy
in advanced adenoid cystic carcinoma of the head and neck. Head
Neck. 14:273–277. 1992.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Papaspyrou G, Hoch S, Rinaldo A, Rodrigo
JP, Takes RP, van Herpen C, Werner JA and Ferlito A: Chemotherapy
and targeted therapy in adenoid cystic carcinoma of the head and
neck: A review. Head Neck. 33:905–911. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Licitra L, Cavina R, Grandi C, Palma SD,
Guzzo M, Demicheli R and Molinari R: Cisplatin, doxorubicin and
cyclophosphamide in advanced salivary gland carcinoma. A phase II
trial of 22 patients. Ann Oncol. 7:640–642. 1996.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Laurie SA, Ho AL, Fury MG, Sherman E and
Pfister DG: Systemic therapy in the management of metastatic or
locally recurrent adenoid cystic carcinoma of the salivary glands:
A systematic review. Lancet Oncol. 12:815–824. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Li J, Ludmire EB, Wang Y, et al:
Stereotactic radiosurgery versus whole-brain radiation therapy for
patients with 4-15 brain metastases: A phase III randomized
controlled trial. Lecture presented at the American Society for
Radiation Oncology (ASTRO) Annual Meeting, October 24-28, 2020.
|
|
19
|
Andrews DW, Scott CB, Sperduto PW,
Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J,
Bahary JP, et al: Whole brain radiation therapy with or without
stereotactic radiosurgery boost for patients with one to three
brain metastases: Phase III results of the RTOG 9508 randomised
trial. Lancet. 363:1665–1672. 2004.PubMed/NCBI View Article : Google Scholar
|