Introduction
Metastatic tumors in the oral region are extremely
rare, constituting <1% of all malignancies (1,2).
They primarily affect individuals aged 50-70 years-old, with no
significant sex disparity. The mandible and gingiva are the
predominant sites for jawbone and soft tissue metastases,
respectively; however, the frequency varies depending on the
primary lesion (3-8).
In men, oral metastases commonly arise from lung, kidney, liver and
prostate cancers, whereas in women, breast, genital and kidney
cancers are frequently associated with oral metastases (6). The metastasis of colorectal cancer to
the oral cavity is relatively uncommon (only 1-2% of all cases)
(5-10).
The significance of perioperative oral function
management (POM) in preventing and mitigating post-operative
complications, including surgical site infections and pneumonia,
and improving the overall quality of life of the cancer patient, is
increasingly evident (11-16).
POM interventions have demonstrated positive outcomes, including
reduced hospital stays, decreased medical costs, and improved
patient survival rates, consequently gaining recognition as an
indispensable procedure during the perioperative period (11-18).
However, limited literature exists regarding the effectiveness of
POM in managing oral metastases, particularly in the context of
colorectal cancers.
The present case report presents a rare case of
metastases to the maxillary gingiva originating from a stage IIIB
tumor-node-metastatic (TNM) colorectal carcinoma. The patient's
condition improved with the POM, resulting in a significant
enhancement in the quality of life. In contrast to expectations,
the patient defied prognostic predictions and survived for over a
year before succumbing to multiple organ failure (MOF). These
findings underscore the urgent need for timely administration of
POM to improve the quality of life and survival rates of surgical
patients with a history of cancer and oral symptoms.
Case report
A 58-year-old man complaining of an uncomfortable
swelling on the left side of the upper jaw and decreased oral
intake was referred to the Department of Oral and Maxillofacial
Functional Rehabilitation in March 2018 for a POM consultation. The
patient had a surgical history of segmental bowel resection due to
TNM stage IIIB colorectal cancer, with elevated serum
carcinoembryonic antigen (CEA; recorded value, 5.9 ng/ml; reference
value, 0.0-4.0 ng/ml) and serum hepatitis B surface antibody
(HBsAb; recorded value, 104.04 mIU/ml; reference value, 0.00-9.99
mIU/ml) levels, and normal liver function test values. In January
2015, the patient had a history of melena and occasional
hematochezia. TNM stage IIIB colorectal adenocarcinoma was
diagnosed following a thorough clinical evaluation, and the patient
was surgically treated using the Hartmann procedure (13) under general anesthesia in March
2015. Thereafter, the patient was followed up ~1 year without
evidence of recurrence or metastatic disease. After March 2016, the
patient was lost to follow-up for two years. However, the patient
returned in March 2018 with complaints of abdominal pain and oral
symptoms. Additionally, the patient had a history of a remnant root
following extraction of the left maxillary second premolar; the
family history was unremarkable.
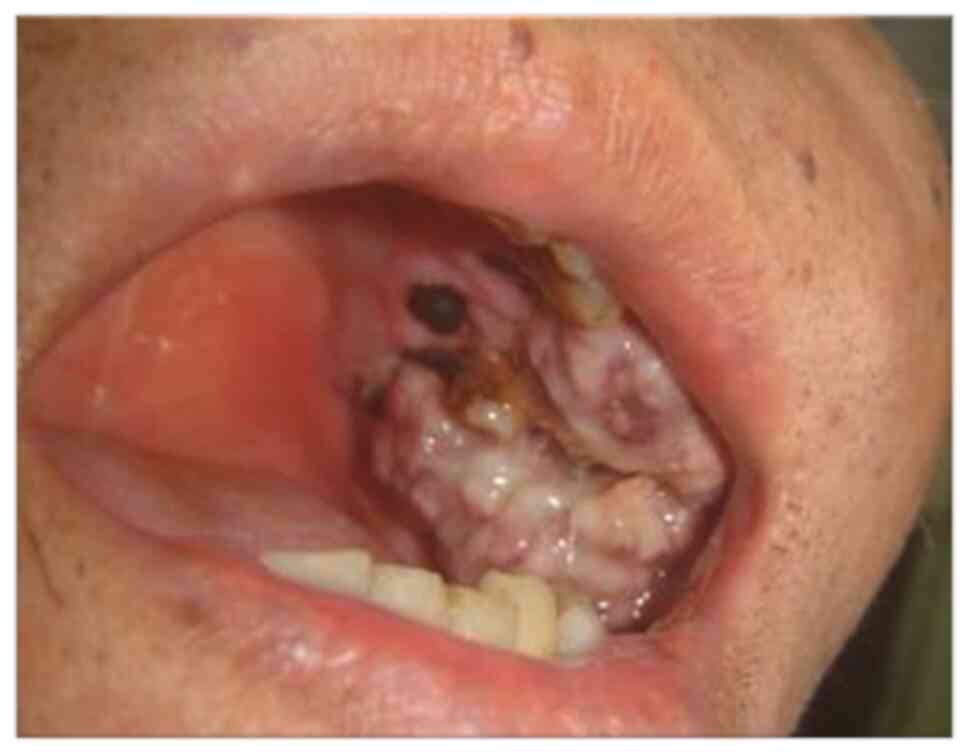
Upon examination, the patient was cachectic and sick
looking with mild pallor, a tinge of jaundice, and cervical
lymphadenopathy on the left side. Extraoral examination indicated
facial asymmetry and swelling of the left cheek. Intraoral
investigations revealed a large, ulcerative, moderately-tender,
irregular mass (size, 22x20x18 mm) with focal areas of necrosis
extending distally from the left maxillary first premolar (Fig. 1).
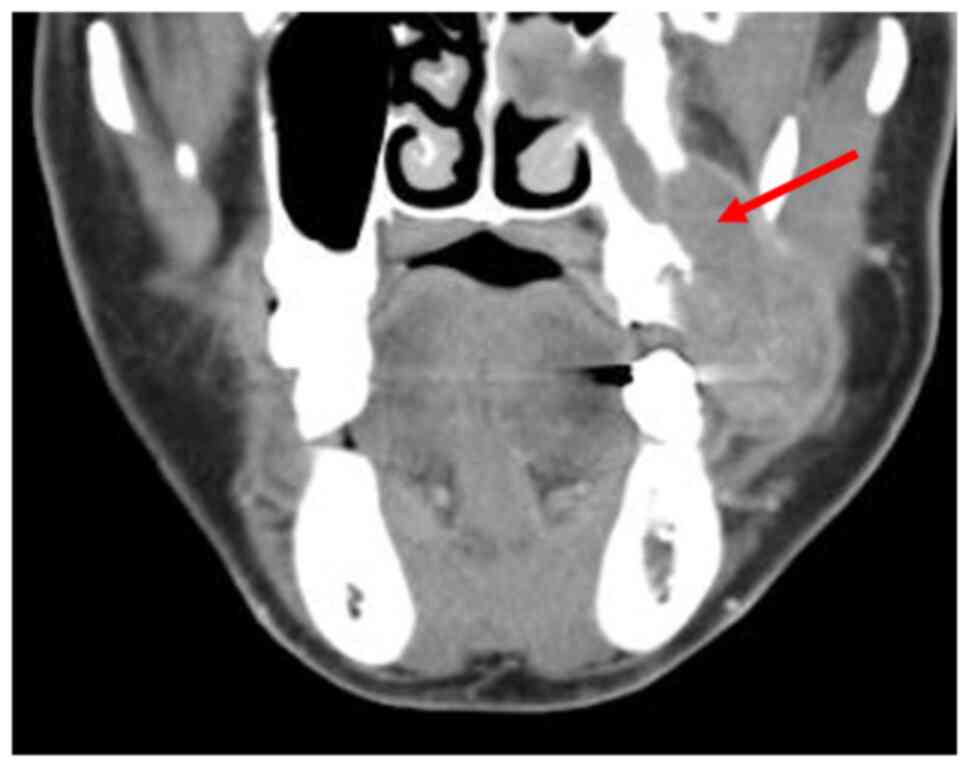
The patient underwent radiological, hematologic and
histological examinations, with a differential diagnosis of a
gingival tumor invading the maxillary sinus. Orthopantomography and
computed tomography (CT) were performed in the radiology
department. The orthopantomograms showed horizontal bone resorption
in the jaw, particularly in the left maxillary molar root region
and around the second premolar (Fig.
2). CT scan of the oral cavity showed a large, poorly
demarcated soft tissue mass extending into the left maxillary
sinus, with generalized bone resorption around the left second
premolar and the base of the maxillary sinus (Fig. 3). CT scans of the chest and abdomen
showed relatively distinct nodules in the lung and tumor recurrence
in the residual bowel. Liver metastases were also detected. The
hematology and blood biochemistry test results are shown in
Table I. The levels of the tumor
markers CEA and carbohydrate antigen 19-9 (CA19-9), also known as
Sialyl-LewisA, were exponentially elevated; other blood parameters
were essentially unremarkable.
 | Table IHematology and blood biochemistry
findings. |
Table I
Hematology and blood biochemistry
findings.
| Test parameter | Obtained value | Reference range | Unit |
|---|
| Initial hospital
visit | | | |
|
WBC | 10,900 | 4,000~9,000 | Μl |
|
s-Glu | 117 | 70~110 | mg/dl |
|
HBsAb | 104.04 | 0.00~9.99 | mIU/ml |
|
CEA | 5.9 | 0.0~5.0 | Ng/ml |
|
CA19-9 | <2.0 | 0.0~37.0 | U/ml |
| Emergency visit | | | |
|
WBC | 10,200 | 4,000-9,000 | Μl |
|
AST
(GOT) | 46 | 13~37 | IU/l |
|
ALT
(GPT) | 30 | 8~45 | IU/l |
|
LDH | 1,212 | 122~228 | IU/l |
|
ALP | 1,749 | 118~335 | IU/l |
|
γ-GT | 870 | 8~33 | IU/l |
|
ALB | 3.3 | 4.1~5.2 | g/dl |
|
BUN | 14.6 | 7.8~18.9 | mg/dl |
|
CREA | 0.77 | 0.45~0.82 | mg/dl |
|
s-Glu | 92 | 70~110 | mg/dl |
|
HBsAb | 29.79 | 0.00~9.99 | mIU/ml |
|
CEA | 10,945.4 | 0.0~5.0 | Ng/ml |
|
CA19-9 | <2.0 | 0.0~37.0 | U/ml |
|
5-S-CD | 2.7 | 1.5~8.0 | |
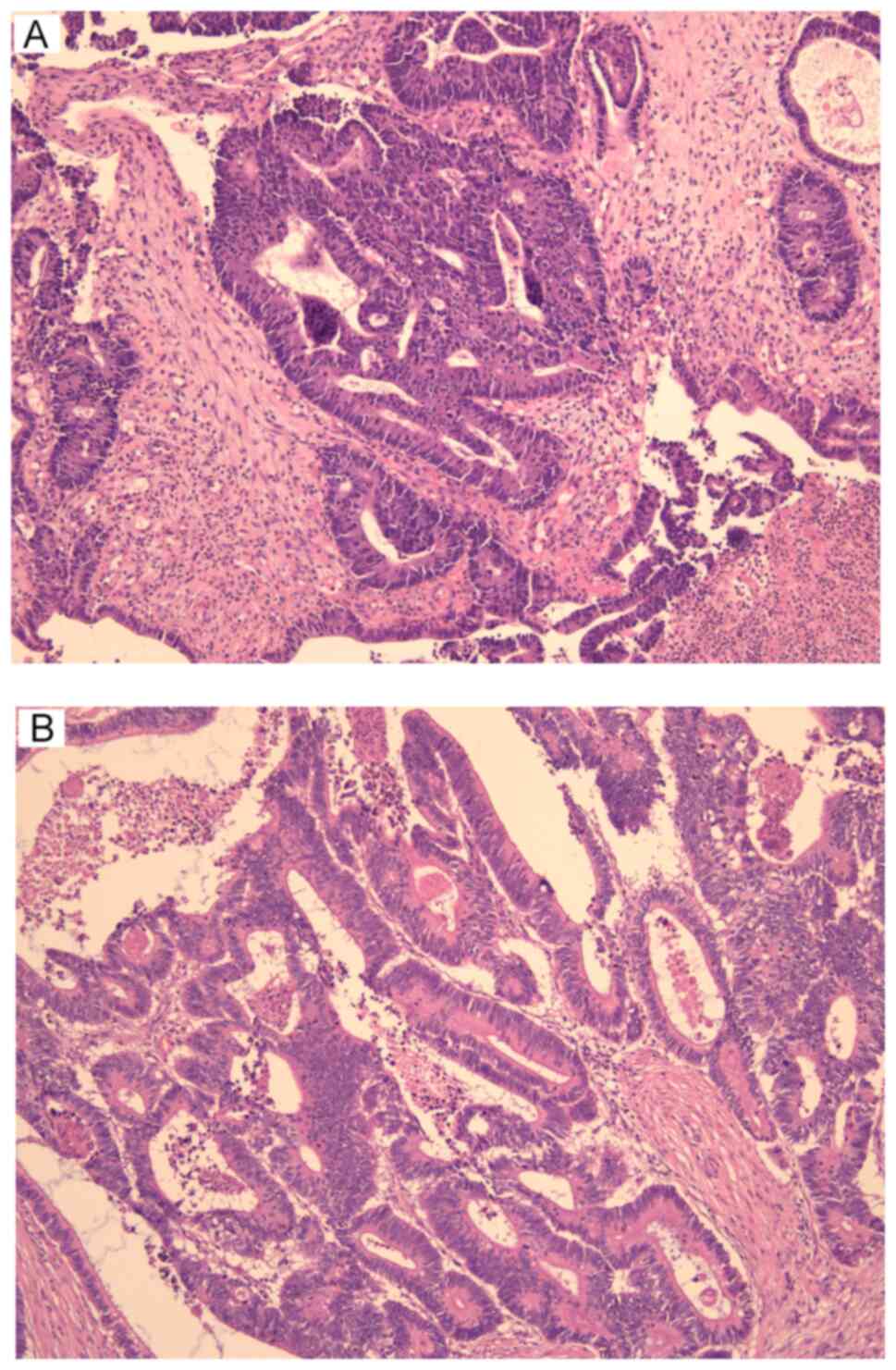
Fresh surgical biopsy specimens from the jaw tumor
underwent histopathological analysis in the university hospital
pathology department, conducted by at least 2 pathologists. This
involved the utilization of hematoxylin and eosin (H&E)
staining and immunohistochemistry (IHC). For H&E staining, the
process commenced by sectioning the specimen into 4-µm thick
segments following fixation with 96% ethanol. Subsequently, these
sections were immersed in a 10% formalin solution for 24 h.
Hematoxylin staining was initiated for 30 sec, followed by a 5-min
water rinse and a 15-sec eosin Y counterstaining. Dehydration using
96 and 99.8% ethanol, along with xylene fixation and cover slipping
with a mounting medium, followed suit. Diagnostic images were
captured via a Nikon Eclipse Ci microscope equipped with a Nikon
DS-Fi3 camera with a 4X objective (Nikon Corporation).
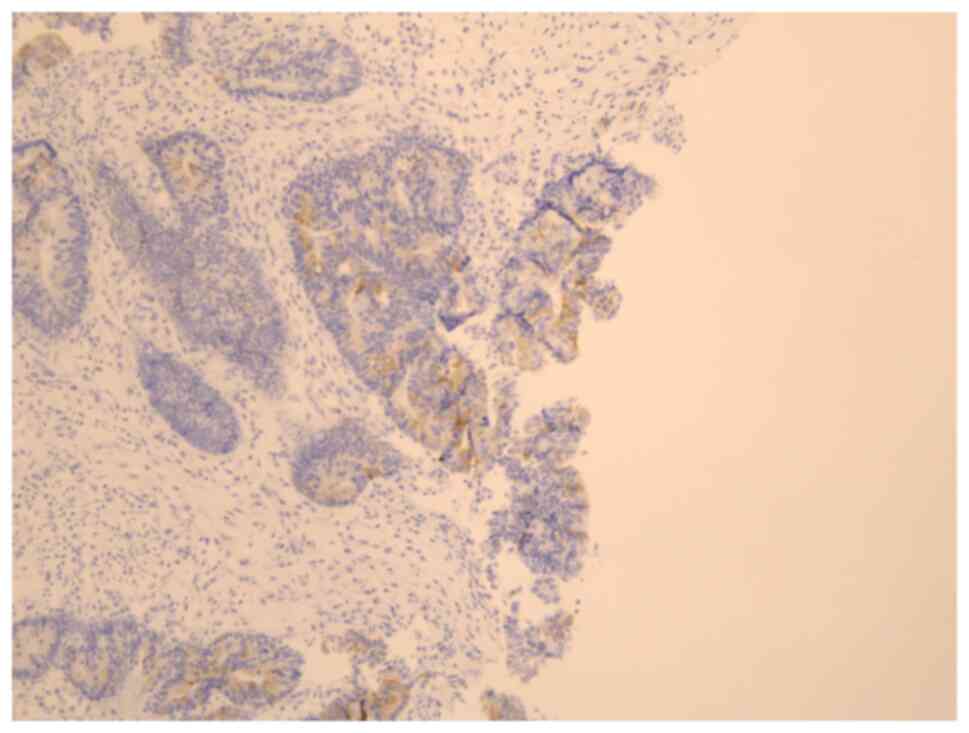
For IHC, the streptavidin-peroxidase technique was
employed on 4-µm thick specimen sections. Following rinsing with
phosphate-buffered saline (PBS) and a 10-min pepsase activity for
antigen retrieval, sections were incubated in methanol alongside 3%
hydrogen peroxide to deactivate endogenous peroxidases.
Subsequently, blocking with PBS 0.5% Tween-20 (PBS-T;
MilliporeSigma), containing 3% bovine serum albumin
(MilliporeSigma), occurred for 1 h at room temperature. Incubation
at 4˚C overnight with primary antibodies including cytokeratin
(CK)7 and CK20 was performed. As an example, the primary antibody
for CK7, rabbit anti-CK7 (1:1,600; cat. no. ab199718; Abcam), was
utilized. Following three PBS washes, a secondary antibody, goat
anti-rabbit IgG H&L (HRP) (1:500; cat. no. ab97051; Abcam), was
introduced, along with fresh Diaminobenzidine as the substrate.
Negative controls employed PBS instead of the primary antibody.
Philips IntelliSite Pathology Solution (Philips) was employed for
image acquisition.
H&E staining analysis unveiled atypical cell
growth within tubular structures coupled with necrotic tissue,
indicating a moderately-differentiated adenocarcinoma (Fig. 4). Furthermore, IHC demonstrated
CK20 positivity and CK7 negativity in the atypical glandular ducts,
implying metastasis from the colorectal carcinoma (Fig. 5).
Based on the results of the POM examination, the
oral lesion was diagnosed as metastatic colorectal adenocarcinoma
of the maxillary gingiva. In addition, metastases were observed in
the lung and liver. After thorough consultations among the surgeons
and considering several factors, including the patient's general
condition and the late stage of the disease, the patient was
treated with adjuvant chemotherapy and radiotherapy with removal of
the remaining root tooth, rather than aggressive surgical treatment
of the tumor in the oral cavity. Chemotherapy was initiated using a
combination of XELOX: capecitabine (Xeloda®; Chugai Pharmaceutical
Co., Ltd.) plus oxaliplatin (Yakult Honsha Co., Ltd.), and
bevacizumab (BV). A total of seven doses of XELOX (170 mg) plus BV
(450 mg) were followed by 21 doses of cetuximab; cetuximab
administration started with a single dose of 620 mg, which was
reduced to 390 mg once daily. The oral cavity and primary tumor
were treated by radiation therapy (8 Gy each). The patient's oral
intake improved after the extraction of the residual tooth and the
comprehensive implementation of POM, which included customized
hygiene, chemoprophylaxis, collaborative efforts from an
interdisciplinary medical team, pain management, and patient
education. Subsequently, an improvement in the patient's quality of
life was observed for >12 months before his clinical condition
deteriorated due to multiple organ metastases. The patient
succumbed to MOF in March 2019.
Discussion
Metastases in the oral cavity are rare, and studies
on the efficacy of POM for managing such cases are limited.
Patients with metastatic tumors in the oral cavity can present with
various symptoms, such as swelling, pain, nerve paralysis and
dental issues (tooth mobility or displacement). Gingival metastases
may be asymptomatic or manifest as painless granulomatous masses
(7,8). Therefore, it is crucial to
differentiate metastatic oral tumors from other dental conditions
accurately.
Colorectal carcinomas account for ~18% of all
malignancies, with sigmoid carcinoma constituting ~30% of these
cases (8). Orofacial metastatic
tumors can potentially originate from various organs, such as the
lungs and kidneys; nonetheless, the rare occurrence of oral
metastases stemming from colorectal cancer can pose complex
challenges in both diagnosis and treatment (7-10).
A precise diagnosis of metastatic tumors in the oral cavity is
vital for identifying the primary tumor and any metastases to other
organs (9,11-20).
Furthermore, distinguishing between primary and metastatic tumors
in the oral cavity is crucial for selecting the appropriate
treatment approach.
The diagnostic criteria for metastatic tumors
include the presence of a primary tumor or the absence of other
tumor lesions (Tables II and
III) (21-32).
Additionally, histopathological similarities to the primary tumor
and the clinical metastatic status are considered during the
diagnosis (32). In the present
case report, histopathological examination revealed a
moderately-differentiated adenocarcinoma. Immunostaining with CK20
and CK7 aided in establishing its correlation with the primary site
(19,33-35).
The positive CK20 and negative CK7 results were consistent with the
findings of metastatic colorectal carcinoma (32). The elevated serum levels of CEA and
CA19-9 and the CT images confirmed cancer infiltration in the liver
and lungs.
 | Table IIShowing some reported cases of
colorectal cancer metastasis in the maxillary gingiva. |
Table II
Showing some reported cases of
colorectal cancer metastasis in the maxillary gingiva.
| Case | Authors | Publication
year | Age | Sex | Prognosis | Other metastasis
sites |
|---|
| 1 | Cama et al
(24) | 2002 | 57 | Female | <1 year | Not indicated |
| 2 | Kataoka et
al (23) | 2003 | 37 | Female | 3.6 years | Lung, brain |
| 3 | Koizumi et
al (21) | 2004 | 69 | Male | 3.7 years | Lung, liver |
| 4 | Kitamura et
al (22) | 2007 | 64 | Male | 1 Year | None |
| 5 | Baranović et
al (25) | 2015 | 78 | Male | <1 year | Liver |
| 6 | Dalirsani et
al (26) | 2020 | 69 | Female | <1 year | Not indicated |
| 7 | Nair et al
(27) | 2021 | 50 | Male | <1 year | Lung, liver,
adrenal and vertebral |
| 8 | Prasad et al
(28) | 2021 | 51 | Male | <1 year | Not indicated |
| 9 | Neumann et
al (29) | 2021 | 59 | Male | 26 other cases were
listed, reported over 30 years (mostly with poor prognosis) | Peritoneum |
| 10 | Todorova et
al (30) | 2021 | 73 | Male | Not indicated | Locoregional
lymphatic nodes |
| 11 | Present case | 2023 | 58 | Male | >1 Year | Lung, liver,
bone |
 | Table IIIShows suggested diagnostic criteria
for oral metastatic tumors. |
Table III
Shows suggested diagnostic criteria
for oral metastatic tumors.
| Item number | Criterion | (Refs.) |
|---|
| 1 | Clinical and
histological evidence of a primary tumor | (31) |
| 2 | The histological
similarity between the primary tumor and the metastases | |
| 3 | No previous tumor
in the metastatic area | |
| 4 | No direct invasion
from the primary tumor or other metastases | |
| 1 | Histopathological
similarity to the primary tumor | (32) |
| 2 | Sufficient clinical
and histological suspicion of metastatic disease | |
| 3 | A tumor suspected
to be metastatic must not resemble a primary tumor arising in the
oral cavity | |
The metastasis of sigmoid carcinoma to the liver and
lungs is considered to occur via the portal vein system and to
other sites (such as the oropharyngeal region) via the inferior
vena cava and pulmonary veins (36,37).
The mandible commonly serves as the primary site for metastatic
tumors due to its high vascularity, while the rich capillary
network in the gingiva facilitates the infiltration of tumor cells
(8,20,38).
In the present case report, chronic gingival irritation resulting
from a retained root fragment in the left upper second premolar may
have contributed to the dissemination of cancer cells through the
bloodstream.
Consistent with the findings in this case,
metastatic tumors in the oral and maxillofacial regions are
frequently encountered as multiple metastases and exhibit a high
fatality rate (22,23). A comprehensive evaluation of the
primary tumor and the presence or absence of metastases is crucial
in determining an effective treatment plan. POM during the
perioperative period is widely recognized as a critical procedure
in the surgical management of patients with cancer, offering
notable advantages (11-16).
Kurasawa et al (39)
investigated the impact of POM on pneumonia and the mortality of
patients with cancer and reported its effectiveness in decreasing
the incidence of pneumonia across various cancer types, including
musculoskeletal, lung, brain, head and neck, thyroid gland,
pancreatic, stomach, and esophageal cancers. In addition, POM was
beneficial for patients with compromised immune systems and
respiratory dysfunction. Factors such as preoperative conditions,
nutritional status, oral hygiene, and the relationship between the
operative field and airway were identified as crucial determinants
of the effectiveness of POM. Importantly, POM was associated with
decreased mortality rates, particularly in lung and pancreatic
cancer, which was attributed to enhanced oral hygiene and
swallowing function. Additionally, a case report by Nashi et
al (40) underscored the
significance of standardized techniques and guidelines for oral
management to prevent complications, especially in patients with
cardiac conditions, which served as a reminder for healthcare
practitioners to prioritize appropriate POM protocols. In another
study, Suzuki et al (41)
reported that preoperative periodontal treatment improved oral
health before and after cardiac valve surgery; the intervention
group also experienced fewer postoperative fever days. Although the
present case report had certain limitations, the results suggested
that preoperative treatment may help mitigate the risk of
postoperative infections, thus emphasizing the necessity for
perioperative oral health interventions and education. Conversely,
a retrospective review on POM conducted at a cancer treatment
hospital demonstrated positive outcomes, such as reduced
complications and improved patient experiences; however, the
authors observed challenges associated with POM due to the absence
of standardized practices and limited collaboration between medical
and dental professionals (42).
The present case report highlighted the importance of education and
early intervention in oral management to optimize cancer treatment
outcomes.
In the present case report, the proactive
implementation of POM significantly enhanced the patient's quality
of life via comprehensive assessment and palliative care, despite
the advanced stage of the disease. This interdisciplinary approach
prolonged survival by over a year before the eventual demise of the
patient. Metastatic tumors in the oral cavity were promptly
identified through POM, although surgery was deemed not feasible
due to liver and lung involvement. Prompt consideration of clinical
findings, differentiation of oral symptoms from tumor lesions, and
emphasis on oral care in systemic disease through effective
collaboration between medical and oral/dental professionals are
crucial for the perioperative oral management of patients with
malignant tumors.
In conclusion, the present case report highlighted
the rarity of metastases, especially colon carcinoma metastasis, to
the maxilla. An accurate diagnosis, differentiation from dental
conditions, and POM are indispensable for the effective treatment
of patients in this condition. POM offers significant advantages in
preventing pneumonia, reducing mortality, and improving oral
health. Standardized practices and interdisciplinary collaboration
are imperative for optimizing the outcomes. Further research on POM
can enhance the management of oral metastases and improve the
well-being of the patient.
Acknowledgements
The authors would like to thank the staff of the
Department of Oral and Maxillofacial Functional Rehabilitation for
their clinical support.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MM and EHN contributed to the drafting of the
manuscript. MM, EHN and NK performed the literature search. MM,
EHN, NK, IK, SJ, MN,KT, SY and NH collected the data and assisted
in drafting the case report section. MM, EHN, SY and NH critically
revised the manuscript. All authors confirm the authenticity of all
the raw data. All authors have read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for the publication of the
patient's clinical information and images was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shimono H, Hirai H, Oikawa Y, Mochizuki Y,
Kuroshima T, Tomioka H, Kayamori K, Ikeda T and Harada H:
Metastatic tumors in the oral region: A retrospective chart review
of clinical characteristics and prognosis. Oral Surg Oral Med Oral
Pathol Oral Radiol. 132:648–652. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
de Almeida Lança ML, Carvalho YR, Almeida
JD and Kaminagakura E: Hidden colon adenocarcinoma diagnosed from
mouth metastasis: Case report and literature review. World J Surg
Oncol. 21(88)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ho DP, Wilkinson PE, Vogel RI,
Gopalakrishnan R and Argyris PP: Metastatic tumors to the oral soft
tissues and jawbones: A retrospective analysis of 40 cases and
review of the literature. Head Neck Pathol. 16:802–813.
2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Watanabe M, Tada M, Satomi T, Chikazu D,
Mizumoto M and Sakurai H: Metastatic rectal adenocarcinoma in the
mandibular gingiva: A case report. World J Surg Oncol.
14(199)2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hirshberg A and Buchner A: Metastatic
tumors to the oral region. An overview. Eur J Cancer B Oral Oncol.
31B:355–360. 1995.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hirshberg A, Shnaiderman-Shapiro A, Kaplan
I and Berger R: Metastatic tumors to the oral cavity-pathogenesis
and analysis of 673 cases. Oral Oncol. 44:743–752. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Meyer I and Shklar G: Malignant tumors
metastatic to mouth and jaws. Oral Surg Oral Med Oral Pathol.
20:350–362. 1965.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cash CD, Royer RQ and Dahlin DC:
Metastatic tumors of the jaws. Oral Surg Oral Med Oral Pathol.
14:897–905. 1961.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hadhri A, Abidi R, Ben Rejeb M, Yahyaoui S
and Nasr C: Metastasis of colon adenocarcinoma to the mandible: A
case report. Tunis Med. 98:518–521. 2020.PubMed/NCBI
|
|
10
|
Hirshberg A, Berger R, Allon I and Kaplan
I: Metastatic tumors to the jaws and mouth. Head Neck Pathol.
8:463–474. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ishimaru M, Matsui H, Ono S, Hagiwara Y,
Morita K and Yasunaga H: Preoperative oral care and effect on
postoperative complications after major cancer surgery. Br J Surg.
105:1688–1696. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Shin JH, Kunisawa S, Fushimi K and Imanaka
Y: Effects of preoperative oral management by dentists on
postoperative outcomes following esophagectomy: Multilevel
propensity score matching and weighting analyses using the Japanese
inpatient database. Medicine (Baltimore). 98(e15376)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Akutsu Y, Matsubara H, Shuto K, Shiratori
T, Uesato M, Miyazawa Y, Hoshino I, Murakami K, Usui A, Kano M and
Miyauchi H: Pre-operative dental brushing can reduce the risk of
postoperative pneumonia in esophageal cancer patients. Surgery.
147:497–502. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shigeishi H, Ohta K, Fujimoto S, Nakagawa
T, Mizuta K, Ono S, Shimasue H, Ninomiya Y, Higashikawa K, Tada M,
et al: Preoperative oral health care reduces postoperative
inoammation and complications in oral cancer patients. Exp Ther
Med. 12:1922–1928. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Nobuhara H, Yanamoto S, Funahara M,
Matsugu Y, Hayashida S, Soutome S, Kawakita A, Ikeda S, Itamoto T
and Umeda M: Effect of perioperative oral management on the
prevention of surgical site infection after colorectal cancer
surgery: A multicenter retrospective analysis of 698 patients via
analysis of covariance using propensity score. Medicine
(Baltimore). 97(e12545)2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kurasawa Y, Maruoka Y, Sekiya H, Negishi
A, Mukohyama H, Shigematsu S, Sugizaki J, Karakida K, Ohashi M,
Ueno M and Michiwaki Y: Pneumonia prevention effects of
perioperative oral management in approximately 25,000 patients
following cancer surgery. Clin Exp Dent Res. 6:165–173.
2020.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Iwata E, Hasegawa T, Yamada SI, Kawashita
Y, Yoshimatsu M, Mizutani T, Nakahara H, Mori K, Shibuya Y, Kurita
H and Komori T: Effects of perioperative oral care on prevention of
postoperative pneumonia after lung resection: Multicenter
retrospective study with propensity score matching analysis.
Surgery. 165:1003–1007. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nishi H, Takahashi S, Ohta K, Takamoto M,
Shigeishi H, Go S, Obayashi T, Yoshioka Y, Konishi M, Shimizu Y, et
al: Effects of perioperative oral care on postoperative
inflammation following heart valve surgery. Oral Dis. 27:1542–1550.
2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Khosraviani K, Campbell WJ, Parks TG and
Irwin ST: Hartmann procedure revisited. Eur J Surg. 166:878–881.
2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hirshberg A, Leibovich P and Buchner A:
Metastases to the oral mucosa: Analysis of 157 cases. J Oral Pathol
Med. 22:385–390. 1993.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Koizumi K, Hayashido Y, Yoshioka Y, Hara J
and Okamoto T: A case of carcinoma of the sigmoid colon
metastatizing to the maxillary gingiva. Jpn J Oral Maxillofac Surg.
50:396–399. 2004.
|
|
22
|
Kitamura N, Ishida K, Deguchi H, Tsuyoshi
H, Okamoto T and Hosoda M: A case of transverse colon
adenocarcinoma metastatic to the maxilla and cervical lymph nodes.
Jpn J Oral Maxillofac Surg. 53:504–508. 2007.
|
|
23
|
Kataoka S, Shibata M, Doi R, Onda M, Sudoh
M and Ryoke K: A clinical study of 17 cases of malignant tumors
metastatic to the mouth and jaws. Jpn J Oral Maxillofac Surg.
49:566–569. 2003.
|
|
24
|
Cama E, Agostino S, Ricci R and Scarano E:
A rare case of metastases to the maxillary sinus from sigmoid colon
adenocarcinoma. ORL J Otorhinolaryngol Relat Spec. 64:364–367.
2002.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Baranović M, Vidaković B, Sauerborn D,
Perić B, Uljanić I and Mahovne I: Colorectal adenocarcinoma
metastasizing to the oral mucosa of the upper jaw. Srp Arh Celok
Lek. 143:314–316. 2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Dalirsani Z, Mohtasham N and Samiee N:
Metastasis of colon adenocarcinoma to maxillary gingiva and palate.
Iran J Otorhinolaryngol. 32:327–331. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Nair LM, Mathews A, Aparna MP and Sajeed
A: Maxillary gingival metastasis from adenocarcinoma colon. Case
Rep. 11:122–124. 2021.
|
|
28
|
Prasad A, Alrifai T, Vijaya Rangan S and
Garcia J: Rare case of metastatic adenocarcinoma to the maxillary
sinus. BMJ Case Rep. 14(e244485)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Neumann ED, León Vintró X, Vega García C
and Quer Agustí M: Oral cavity colon adenocarcinoma metastases: A
case report with surgical approach and review of more than 30 years
literature. Oral Maxillofac Surg. 25:99–101. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Todorova RS, Tanevaa I, Toshevaa E,
Jivkova E, Ionkova A, Bojinov P and Bogdanov V: Atypical pattern of
rectal cancer metastasis into mouth cavity. J Clin Rev Case Rep.
6:711–713. 2021.
|
|
31
|
Zegarelli DJ, Tsukada Y, Pickren JW and
Greene GW: Metastatic tumor to the tongue. Report of twelve cases.
Oral Surg Oral Med Oral Pathol. 35:202–211. 1973.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Clausen F and Poulsen H: Metastatic
carcinoma of the jaws. Acta Pathol Microbiol Scand. 57:361–374.
1963.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Rubin BP, Skarin AT, Pisick E, Rizk M and
Salgia R: Use of cytokeratins 7 and 20 in determining the origin of
metastatic carcinoma of unknown primary, with special emphasis on
lung cancer. Eur J Cancer Prev. 10:77–82. 2001.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Chu P, Wu E and Weiss LM: Cytokeratin 7
and cytokeratin 20 expression in epithelial neoplasms: A survey of
435 cases. Mod Pathol. 13:962–972. 2000.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Tot T: Adenocarcinomas metastatic to the
liver the value of cytokeratins 20 and 7 in the search for unknown
primary tumors. Cancer. 85:171–177. 1999.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Naylor GD, Auclair PL, Rathbun WA and Hall
EH: Metastatic adenocarcinoma of the colon presenting as
periradicular periodontal disease: A case report. Oral Surg Oral
Med Oral Pathol. 67:162–166. 1989.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Banerjee SC: Metastasis to the mandible.
Oral Surg Oral Med Oral Pathol. 23:71–77. 1967.PubMed/NCBI View Article : Google Scholar
|
|
38
|
van der Waal RI, Buter J and van der Waal
I: Oral metastases: Report of 24 cases. Br J Oral Maxillofac Surg.
41:3–6. 2003.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kurasawa Y, Iida A, Narimatsu K, Sekiya H,
Maruoka Y and Michiwaki Y: Effects of perioperative oral management
in patients with cancer. J Clin Med. 11(6576)2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Nashi M, Yamamoto S, Maeda K, Taniike N
and Takenobu T: A case of infective endocarditis due to oral
streptococci after perioperative oral function management. Cureus.
13(e20446)2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Suzuki H, Matsuo K, Okamoto M, Nakata H,
Sakamoto H and Fujita M: Preoperative periodontal treatment and its
effects on postoperative infection in cardiac valve surgery. Clin
Exp Dent Res. 5:485–490. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
42
|
Watanabe M, Ioku Y, Motohashi T, Hamada S,
Hase K, Ikebe S, Nishiguchi Y, Shoju Y and Sugitatsu M: Clinical
study of perioperative oral management at Osaka Red Cross Hospital.
J Osaka Dent Univ. 56:183–191. 2022.PubMed/NCBI View Article : Google Scholar
|