Introduction
Ameloblastic fibro-odontoma (AFO) is an infrequent,
gradually progressing, expansile epithelial odontogenic neoplasm
(1). The aforementioned lesion
exhibits histological characteristics and biological features
similar to those of an ameloblastic fibroma (AF). However, in AFO,
one or more cellular foci of inductive epithelium persist during
the differentiation process, leading to the production of both
enamel and dentin (2). According to
the 2017 publication of the World Health Organization (WHO)
classification, AFO should now be classified as an odontoma rather
than an odontogenic tumor (3). It
typically manifests in younger individuals and displays no
significant tendency toward either sex. It has been observed to
occur with an equal frequency in both the maxilla and mandible, and
its commonly observed site of occurrence is in the region posterior
of the premolars and molars (4).
AFO, which frequently affects young children, is often challenging
to diagnose prior to surgical intervention due to the lack of
pre-surgical pathological information (1). This is typically resolved by relying on
observations obtained from a presurgical biopsy performed under
local anesthesia. Consequently, clinical diagnosis assumes an
exceedingly prominent role in the preemptive delineation of
surgical procedures, particularly as regards the determination of
the feasibility of conserving teeth situated in close proximity to
the lesion (5).
The present study describes the clinical case of an
18-year-old individual with AFO, with a lesion involving the
posterior mandible that was managed through enucleation.
Case report
An 18-year-old adolescent male was referred to the
Department of Oral and Maxillofacial Surgery, Teerthankar Mahaveer
Dental College and Research Institute, Moradabad in March, 2020
with a primary concern of swelling on the right side of his face.
The patient's medical history indicated the existence of an
indistinct, non-painful and slowly developing bulge over a span of
1 year. Moreover, a discernible slight asymmetry of the face was
noted and linked to the engagement of the posterior area of the
mandibular bone. The medical records of the patients did not reveal
any significant findings, and the dental history did not indicate
any evidence of local injury or infectious activity at the site of
the lesion. Upon an extraoral examination, it was determined that
the enlargement exhibited an osseous morphology, characterized by a
rigid consistency, with the integumentary covering displaying
typical characteristics. No paralysis was identified in the
affected area, although the displacement of the inferior alveolar
nerve was detected. During an intraoral examination, an
asymptomatic protuberance was observed on the posterior aspect of
the right mandible. The mucosal layer exhibited unremarkable
pigmentation, which was consistent with the overlying skin. The
swelling spanned from the second to third molar region and
displayed buccal and lingual cortical expansion.
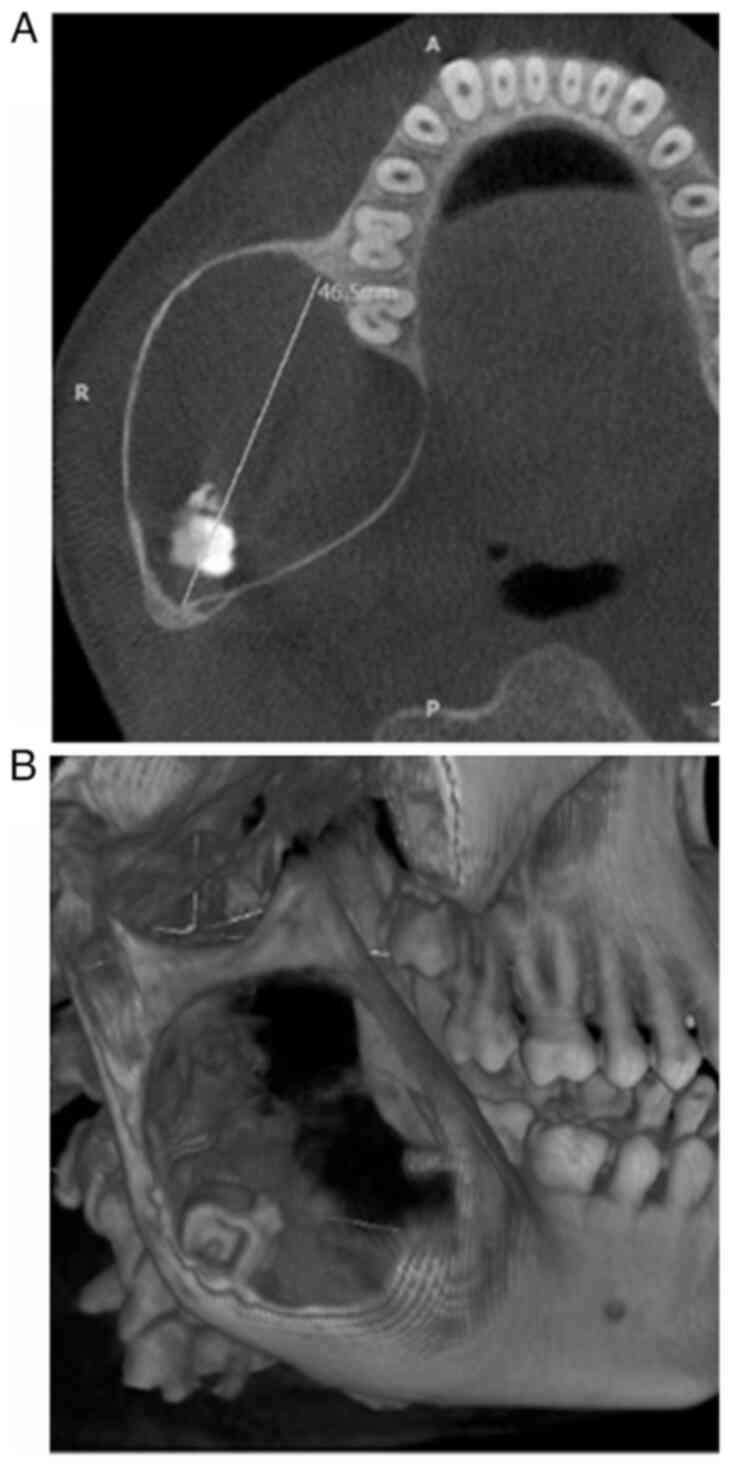
Cone-beam computed tomography was used to identify a
predominantly hypodense area of unilocular nature. This area
involved the right body, angle and ramus of the mandible, with a
thin corticated margin. The area extended anteriorly from the lower
right first molar region to the posterior border of the ramus. The
dimensions of this area were 46.5 mm anteroposteriorly, 38.3 mm
mediolaterally, and 53.8 mm superioinferiorly, as illustrated in
Fig. 1A. An apically displaced third
molar in the right mandibular region near the angle of the mandible
was observed, in association with calcification flecks (Fig. 1B). The presence of a bony crypt
related to the third molar was not observed. However, both the
lingual and buccal cortical plates appeared to be attenuated and
displayed an obvious expansion without any discernible disruption
of continuity.
Based on a comprehensive clinical and radiographic
assessment, a tentative diagnosis of odontoameloblastoma,
calcifying cystic odontogenic tumor, complex or compound odontoma,
ameloblastic fibroma (AF), or ameloblastic fibro-dentinoma (AFD)
was made. Following a scrupulous pre-surgical evaluation, the
procedure was performed under general anesthesia, with an intraoral
approach selected for the enucleation of the lesion along with the
third molar. The extraction of the right second mandibular molar
was performed due to root resorption. The curettage of the bony
walls was subsequently performed, as illustrated in Fig. 2. Bone smoothing was accomplished, and
the excision site was securely sutured with 3-0 vicryl sutures.
Intermaxillary fixation was performed to immobilize the mandible
and prevent any pathological fracture of the mandibular body.
The tissue obtained from the lesion underwent a
histopathological examination. Tissue was sent to pathology
laboratory JMF's ACPM Dental College Dhule in 10% formaldehyde
fixative solution and stored at 4˚C in the laboratory prior to the
processing of tissue. Paraffin-embedded 5-µm-thick sections were
stained with hematoxylin and eosin stain (Merck KGaA) at room
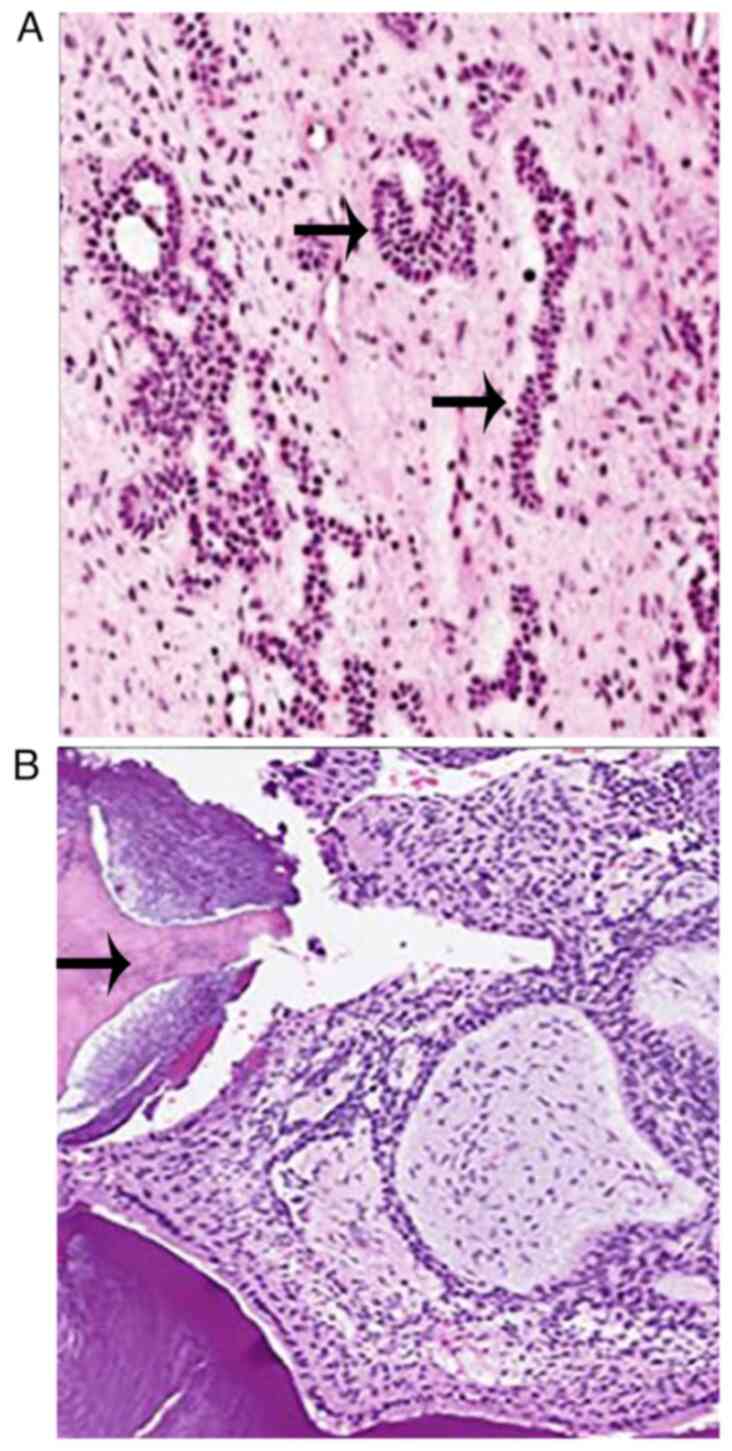
temperature following Bancroft's protocol (6). The microscopic examination of the
stained section under a binocular research microscope (Labomed
LX500) revealed islands, cords and strands of ameloblast-like cells
in a loose, immature connective tissue similar to dental papillae.
Calcified flecks were also observed in the stroma near the
aforementioned islands, with stromal calcifications indicating the
possibility of dentinoid or enameloid material (Fig. 3).
The final diagnosis of the tumor was AFO. The soft
tissue healing process was uneventful, with no evidence of
recurrence during the 2-year follow-up period (Fig. 4).
Discussion
AFO is a pathological condition that can be
categorized as a slowly developing benign, mixed odontogenic
neoplasm (1). This type of tumor is
predominantly observed in the jaw bones, with a low incidence rate
of 1-3% (4). The available
literature substantiates that AFO predominantly targets juveniles,
who have a mean age of 9.4±3.5 years, and evinces a predilection
towards males, indicating a male-to-female ratio of 2.3:1(7). Furthermore, it is notable that the
condition primarily affects the mandible, which differs from the
conclusions presented in the 2005 WHO classification (8). The assertion made by the latter posited
the absence of sex predilection in the distribution of the lesion,
which was equally distributed across the mandible and maxilla,
particularly in the molar region (7). Notably, several instances of the lesion
were associated with an unerupted tooth or with the corresponding
tooth displaced in the apical direction. This observation suggests
that the origin of the lesion is tissues of dental follicle,
primarily dental lamina (9).
According to the 2022 WHO classification of
odontogenic tumors, a revision from the 2017 WHO classification,
AFO has been designated as a precursor of complex odontoma
(7). However, Soluk-Tekkesinand
Vered (10) analyzed a series of
cases of AFO and odontomas, and concluded that AFOs affect
individuals between the ages of 3 and 16 years, and possess a size
>2 cm. Bycontrast, odontomas tend to affect older individuals,
whose age ranges ~27 years, and whose size is <2 cm. Hence, it
is imperative to consider AFO with measurements >2 cm as a true
neoplasm rather than a hamartomatous odontoma (10). The radiographic features of the AFO
describe a distinct and identifiable radiolucency that was
well-circumscribed and round-to-ovoid in shape. This radiolucency
is surrounded by a thin sclerotic margin that contains various
amounts of radiopaque material with an irregular size and form.
Notably, the ratio of radiopaque to radiolucent areas may differ
from one lesion to another, indicating the uniqueness of each case
(2). The present case was documented
in an 18-year-old male who presented with an enlargement >5 cm
in the posterior section of the mandible with flecks of
calcification, indicative of AFO.
A histopathological examination can provide an
accurate diagnosis for cases involving odontoameloblastoma, complex
odontomas, calcifying epithelial odontogenic tumor (CEOT), AF and
AFD due to their similar clinical and radiological features
(1).
Odontoameloblastoma is a combination of complex
odontoma and ameloblastoma with an invasive nature, as observed in
classical ameloblastoma. Radiographically,
odontoameloblastomasrepresent a unilocular radiolucency associated
with impacted molars and radiopaque substances. They may exhibit
theperforation of cortical plates, which is not a feature of AFO.
Histologically, odontoameloblastomas exhibita mature stroma with
epithelial islands of ameloblastic cells and calcification
(11).
There is a current and ongoing debate regarding the
consideration of AF, AFO, AFD and odontomas as distinct entities or
varying stages in the developmental process of odontomas (10). According to the 2017 WHO
classification, certain lesions that exhibit a histopathological
similarity to an AFO are likely indicative of the development of
odontomas (3). Furthermore, it is
plausible that the histopathological appearance of an AFO may be
indistinguishable from that of developing odontomas. In such
instances, the evaluation of concurrent clinical and radiological
features may be a valuable tool for establishing diagnostic
differentiation.
Histopathologically, it is imperative to note that a
CEOT is typified by the noticeable presence of epithelial cells,
homogenous eosinophilic amyloid-like material and calcification.
Epithelial cells are organized, forming nests and sheets that are
polygonal in shape and structure. In addition, the cells have a
clear to eosinophilic cytoplasm and vesicular nuclei with prominent
nucleoli (12). However, it is
noteworthy that the aforementioned features were absent in the case
described herein.
Microscopically, AF comprises various strands and
small islands of the odontogenic epithelium. However, unlike the
enamel organ-like structures that are commonly observedin AFO, AF
does not possess such structures. Moreover, the fibrous elements in
AF may range from cellular to mature collagenous tissue. Despite
this fact, it is noteworthy that the primitive dental papilla-like
appearance isnot obvious in AF (13). Furthermore, the ectomesenchymal
component of AFO bears a striking resemblance to the dental
papilla.
AFO shares some similarities with AFD; however, AFO
contains both enamel and dentinal materials, whereas AFD solely
comprises dentinal materials. Consequently, it can be noted that
upon radiological observation, the characteristics of AFO entail a
greater presence of opaque and denser elements within the lesion as
opposed to AFD. The observable difference in radiology between AFD
and AFO is distinctly evident by the multilocular nature of AFD
lesions, which sets them apart from the unilocular lesions of AFO
(14).
In terms of radiology and histology, unlike AFO,
odontomas encompass a profound calcified component comprised of
enamel, dentin, cementum and connective tissue pulp. The
aforementioned components are observed in the advanced stages of
compound odontoma, where oral maturation attains a state of
completeness (10).
In the case described in the present study, the AFO
exhibited a considerable size exceeding 5 cm and was well
encapsulated with minimal inclination without localized invasion.
Consequently, the recommended course of treatment involved
conservative surgical intervention, entailing enucleation, in
conjunction with the extraction of a non-erupted tooth. However, it
is worth noting that documented cases exist in which the involved
teeth have been preserved (15,16).
Despite the limited propensity of the lesion for recurrence, there
have been instances where conservative treatment aimed at
preserving the associated teeth has yielded reports of recurrence
(15). Consequently, to eliminate
the possibility of recurrence, the unerupted third molar was
extracted in conjunction with AFO enucleation.
In conclusion, the clinical and radiographic
features of AFO are heterogeneous, and its diagnosis can be
determined solely by a histological examination. Although
infrequent, it is important to consider the possibility of its
presence in the differential diagnosis of intraoral radiolucencies
that comprise radiopaque material, particularly when managing
pediatric patients. Irrespective of its classification, considering
its benign behavior, minimal invasiveness and a low recurrence
rate, the preferred method of treatment is a conservative approach,
which typically involves enucleating the lesion and extracting the
associated tooth to prevent future recurrences. The case described
in the study had a positive post-operative course with no signs of
recurrence. Owing to the potential for malignant transformation,
the implementation of long-term monitoring and observation are it
is strongly advised.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MG supervised the study, and was involved in the
conception and design of the study, as well as in the acquisition
of the patient's data and in performing treatment. AQ was involved
in the acquisition and analysis of the patient's data and in
performing treatment, as well as in the critical writing of the
manuscript. MD was involved in the conception and design of the
study, provided advice on the patient's treatment, and was also
involved in the critical writing of the manuscript. SRC and SP were
involved in the laboratory processing of the patient's tissues, in
the histopathological examination, in the review of the literature
and in the critical revision of the manuscript. MS was involved in
the histopathological analysis in the formatting of the figures and
in reviewing the manuscript. MG, AQ and MD confirm the authenticity
of all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for his participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cossiez M and Pin DD: A rare case of
maxillary ameloblastic fibro-odontoma and a review of the
literature. J Oral Med Oral Surg. 26:17–22. 2020.
|
|
2
|
Bharat D, Vahanwala J, Dabir A and
Jobanputra P: Ameloblastic fibro-odontoma in the mandible-clinical,
radiological and surgical aspect. Adv Oral Maxillofac Surg.
2(100066)2021.
|
|
3
|
Wright JM and Vered M: Update from the 4th
edition of the world health organization classification of head and
neck tumours: Odontogenic and maxillofacial bone tumors. Head Neck
Pathol. 11:68–77. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Saeed DM, Setty S, Markiewicz MR and Cabay
RJ: Ameloblastic fibro-odontoma associated with paresthesia of the
chin and lower lip in a 12-year-old girl. SAGE Open Med Case Rep.
7(2050313X19870642)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Omar N, Ullah A, Ghleilib I, Patel N and
Abdelsayed RA: A locally aggressive ameloblastic fibro-odontoma: A
case report and literature review. Cureus.
13(e20366)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Suvarna KS, Layton C and Bancroft JD:
Bancroft's theory and practice of histological techniques. 8th
Edition. Elsevier Health Sciences, Amsterdam, pp126-169, 2018.
|
|
7
|
Soluk-Tekkesin M and Wright JM: The world
health organization classification of odontogenic lesions: A
summary of the changes of the 2022 (5th) edition. Turk Patoloji
Derg. 38:168–184. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Barnes L, Eveson JW, Reichart P and
Sidransky D (eds): World Health Organization classification of
tumours: Pathology and genetics, head and neck tumours. IARC Press,
Lyon, 2005.
|
|
9
|
Thulasirman SK, Thuasidoss G, Prabhu NK
and Raja VB: A rare case of ameloblastic fibro-odontoma of mandible
with literature review. Ann Maxillofac Surg. 8:324–326.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Soluk-Tekkesin M and Vered M: Ameloblastic
fibro-odontoma: At the crossroad between ‘Developing Odontoma’ and
‘True Odontogenic Tumour’. Head Neck Pathol. 15:1202–1211.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sanjai K, Pandey B, Shivalingaiah D and
Kumar HM: Odontoameloblastoma: A report of a rare case. J Oral
MaxillofacPathol. 22:254–259. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kaushal S, Mathur SR, Vijay M and Rustagi
A: Calcifying epithelial odontogenic tumor (Pindborg tumor) without
calcification: A rare entity. J Oral Maxillofac Pathol. 16:110–112.
2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nasir A, Khare A, Ali I and Khan MI:
Ameloblastic fibroma: A case report. J Oral Maxillofac Pathol.
27:S60–S63. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sabu AM, Gandhi S, Singh I, Solanki M and
Sakharia AR: Ameloblastic fibrodentinoma: A rarity in odontogenic
tumors. J Maxillofac Oral Surg. 17:444–448. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Guerra RC, Carvalho PH, Thieringer FM,
Pereira RS and Hochuli-Vieira E: Recurrence of ameloblastic
fibro-odontoma in a child: A case report. Craniomaxillofacial
Trauma & Reconstruction Open. 5:1–4. 2020.
|
|
16
|
Reis SR, de Freitas CE and do Espírito
Santo AR: Management of ameloblastic fibro-odontoma in a 6-year-old
girl preserving the associated impacted permanent tooth. J Oral
Sci. 49:331–335. 2007.PubMed/NCBI View Article : Google Scholar
|