Introduction
Cerebrovascular accidents (CVAs) constitute a major
cause of morbidity and mortality worldwide. There are >700,000
cases of CVAs in the United States annually (1). The thalamus, which is involved in
numerous brain functions, including memory, emotions, the
processing of sensory inputs and sensorimotor functions, can be
involved in CVAs, either alone, or with infarcts in other brain
structures (2,3). Thalamic pain syndrome is an adverse
occurrence following of a CVA that is concentrated neuropathic pain
triggered by temperature fluctuations. Patients frequently
experience hyperalgesia and allodynia. Following a CVA, the onset
of a patient's symptoms is frequently delayed. A patient with a
thalamic CVA may not experience substantial discomfort for months
or years following the stroke. The thalamic pain syndrome is a form
of central post-stroke pain in all situations (1).
As reported in the study by Cambier (4), Dejerine and Roussy first described the
classic thalamic syndrome in 1906. Following their description, a
number of modifications and other clinical manifestations related
to the thalamus were included. In this manner, ocular movement
abnormalities, which are uncommonly associated with thalamic
strokes, were already associated with the impairment of vertical
gaze with or without affecting the sixth cranial nerve (5). The abducens nerve (sixth cranial nerve)
innervates the ipsilateral lateral rectus muscle and is thus
involved in the abduction or lateral movement of the eye. Abduction
palsy causes double vision and horizontal binocularity, and worsens
when looking to the same side of the lesion (6). Pseudo-abducens palsy is a neurological
limitation of abduction when the abducens nerve is intact. This
rare condition may be observed when spontaneous eye movements
exhibit an impaired lateral gaze, although the vestibulo-ocular
reflex (VOR) exhibits complete abduction (7).
Isolated pseudo-abducens palsy secondary to thalamic
stroke was rarely reported in the literature. Only two case reports
of the individuals with infarction of the thalamus presenting with
isolated sixth cranial nerve palsy have been described to date, at
least to the best of our knowledge (8,9). The
present study describes the case of a middle-aged male patient who
presented with 1-day progressive diplopia and occipital headache
who had abducens palsy on the left side as a result of a right
thalamic infarction.
Case report
A 38-year-old right-handed male presenting with
diplopia was admitted to University Hospital of Santa Maria (Santa
Maria, Brazil). The individual reported that this clinical
manifestation began within 1 day and progressively worsened. He
also complained of a new-onset mild occipital headache on the right
side unrelated to eye movements or photo- and phonophobia. He was a
construction worker, and there was no history of neurological
diseases in his family. The patient had a history of smoking for
years and 1 year of hypertension, for which the patient was not
compliant with the medications.
The subject was fully conscious, and oriented to
time and place. The neurological examination revealed left abducens
palsy with intact bilateral vertical and right horizontal to
voluntary movements. In addition, the diplopia was more prominent
when the patient looked toward the left side. Monocular horizontal
ductions exhibited the same abduction limitation as when viewing
with both eyes. The oculocephalic reflex was normal. Palpebral
oculogyric reflex was normal. Myosis, ptosis, nystagmus and skew
deviation were not present. Muscle strength was normal, graded as
five [Medical Research Council Muscle Power Scale (10)] all over the four extremities. Deep
tendon reflexes were normal. A sensory examination yielded normal
results and the rest of the cranial nerves were intact. There were
no cerebellar signs. The remaining physical examination was
normal.
Laboratory tests, including a complete blood count,
platelet count, prothrombin time, partial thromboplastin time,
serum lipids and inflammatory test results were within normal
limits; an investigation for hypercoagulable disorders yielded
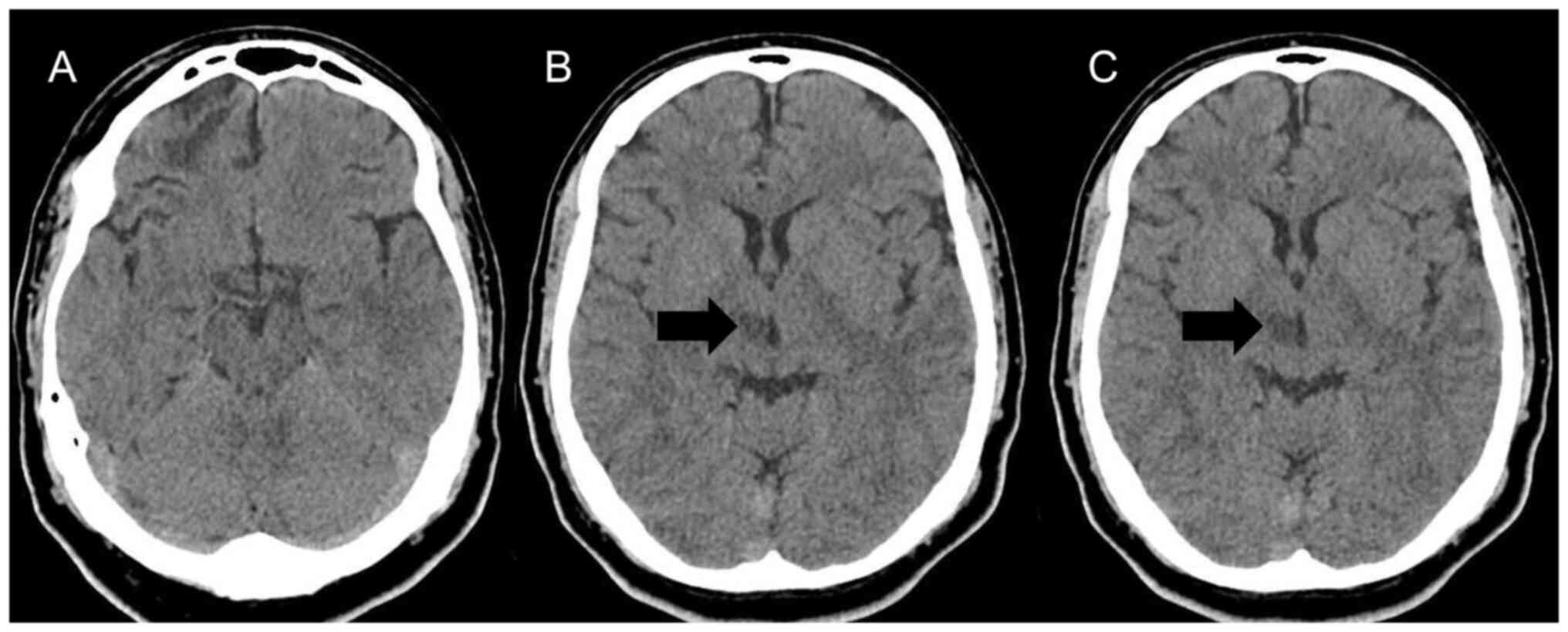
negative results. A cranial computed tomography (CT) scan revealed
a right thalamic infarction (Fig.
1). A brain magnetic resonance imaging (MRI) demonstrated a
lesion of 1.2x1 cm in size (data not shown; image not available),
limited to the thalamus, which was hyperintense on T2-weighted and
fluid-attenuated inversion recovery, consistent with acute ischemic
infarct without affecting the subthalamic or midbrain area.
Cerebrospinal fluid analysis and culture yielded normal
findings.
Upon a stroke etiology investigation, cardiac
monitoring throughout his admission was normal. A transthoracic
echocardiography revealed mild left ventricle hypertrophy with a
normal ejection fraction (56%), left segmental contraction and
valves. A CT angiography of the head and neck yielded normal
findings. The patient was managed in the stroke unit of the
hospital and on day 5 of admission, the patient fully recovered his
eye movements and was discharged.
Discussion
The thalamus is a diencephalic grey matter structure
whose circuits represent a gateway for input and output, in which
nuclei integrate sensory, motor and behavioral signals of the
cerebral cortex with other pathways (4). This complex structure is supplied by
four arteries, three derived from the vertebrobasilar system
(paramedian thalamic-subthalamic, thalamogeniculate and posterior
choroidal arteries) and one derived from the posterior
communicating artery (polar artery) (3). Therefore, thalamic lesions can present
as a number of syndromes depending on the compromised vascular
territory.
Infarctions of the thalamus correspond to ~3% of all
ischemic stroke cases (3). Notably,
thalamic strokes constitute 20-33% of post-stroke centralized pain
cases (1). Moreover, when the stroke
is specifically analyzed in the diencephalon, abnormalities in
vertical or horizontal eye movements following ischemia in this
region are only observed in 5% individuals. In this manner, ocular
abnormalities are rarely reported in thalamic strokes (5).
In 1959, Fisher (11)
were the first to characterize the term ‘sixth nerve pseudopalsy’,
which was described as a paralysis of the voluntary ocular
abduction that could be overcome by ice water caloric stimulation.
Following that study, numerous reports with pure thalamic lesions
have demonstrated oculomotor defects associated with thalamic
infarctions. These ocular manifestations include the ocular tilt
reaction, skew deviation, supranuclear third cranial nerve palsy
and upward gaze palsy (5,8). Furthermore, experimental studies with
provoked lesions in the thalamus of models support the hypothesis
that the thalamus may be involved in oculomotor control (12).
To date, at least to the best of our knowledge, only
a few cases of patients with thalamic infarctions who developed
isolated pseudo-abducens palsy have been reported in the
literature. In the present study, after performing a thorough
review of the literature published in the English language, two
cases were identified and these were compared with the present case
(Table I) (8,9). A
literature search was performed in Embase, Google Scholar, Lilacs,
Medline, Scielo and ScienceDirect, using a set of terms that
included the thalamus, thalamic stroke, stroke, and abducens
palsy.
 | Table ICase reports of individuals who
developed isolated pseudo-abducens palsy secondary to a thalamic
stroke. |
Table I
Case reports of individuals who
developed isolated pseudo-abducens palsy secondary to a thalamic
stroke.
| | Study |
|---|
| Parameter | Wiest et al
(9) | Ghasemi et al
(8) | Present study |
|---|
| Age, years/sex | 57/M | 31/M | 38/M |
| Initial clinical
symptoms | Coma, pneumonia | 12 h of horizontal
diplopia associated with unsteady and contralateral occipital
headache | 24 h of horizontal
diplopia with contralateral occipital headache |
| Comorbidities,
medications in use, and risk factors for cerebrovascular
diseases | None | Smoking | Smoking,
hypertension |
| Key findings in the
neurological examination | Bilateral abducens
palsy | Right abducens
palsy | Left abducens
palsy |
| Neuroimaging
requested | MRI | MRI | CT scan, MRI |
| Lesion site | Bilateral
thalamus | Left thalamus | Right thalamus |
| MRA and CTA | NR | Normal | Normal |
| Stroke etiology | NR | Embolic stroke of
undetermined source | Lacunar infarct
probably secondary to hypertension |
| Time since clinical
presentation and recovery (days) | NR | Three | Five |
In the cases presented in Table I, the majority of patients exhibited
some notable characteristics. First, their presentation included
horizontal diplopia and contralateral headache. Headaches are
common in individuals with stroke, and are more common when the
infarction is in the thalamus (13).
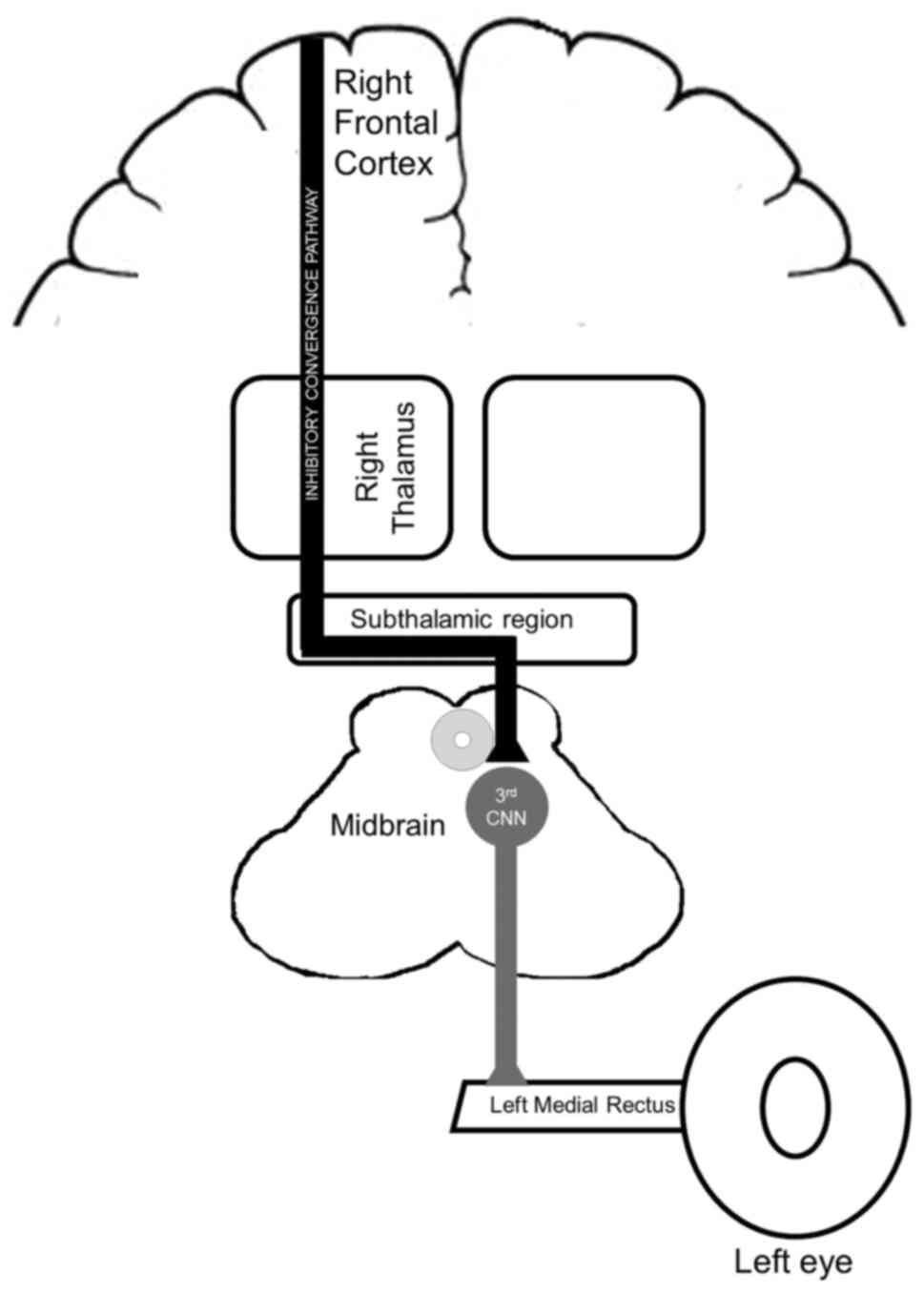
Secondly, the ocular finding contralateral to the stroke supports
the hypothesis presented in the study by Wiest et al
(9), who proposed that the
oculomotor features could occur secondary to an interruption of the
inhibitory convergence pathway that goes through the paramedian
thalamus and probably decussates in the subthalamic region
(Fig. 2) (8,9). Another
key finding was the good prognosis of this acute thalamic
presentation from the time from admission to full recovery only
required a few days.
The paramedian thalamic-subthalamic artery is the
second most common vascular territory of the thalamus to be
affected by stroke, which is associated with pure motor
abnormalities along with third cranial nerve involvement and
vertical gaze abnormalities (3). In
this manner, the nuclei in this vascular territory are probably
connected with the frontal and supplementary eye field in the motor
cortex (12). Thus, as previously
demonstrated, individuals with an isolated stroke of the thalamus
who present with oculomotor deficits probably have lesions in the
intralaminar and dorsomedial nuclei (8,12).
Vasculopathy and non-vasculopathy risk factors exist
for abducens nerve palsy in adults. Diabetes and other medical
disorders are among the top prevalent vasculopathy risk factors in
elderly adults. However, non-vasculopathy reasons, which can affect
both adults and children, may include a variety of elements such as
trauma, inflammation, or compression (5).
The onset of pseudo-abducens palsy is markedly
influenced by lesions in the vicinity of the midbrain-diencephalic
junction. Both convergence-retraction nystagmus and pseudo-abducens
palsy are most likely signs of aberrant vergence activation. The
thalamus may be the passageway for inhibitory descending processes
that terminate in the subthalamic area (14). It is noteworthy that horizontal
diplopia resulting from an isolated abducens (sixth) nerve palsy
can also manifest as the first sign of multiple sclerosis; thus,
this should also be kept as a differential diagnosis (15). Numerous conditions can present
similarly to the thalamic pain syndrome including chronic pain
syndrome, idiopathic peripheral neuropathy, multiple sclerosis,
brain space-occupying lesions and lateral medullary infarction.
However, thorough history and physical examination are essential to
deem these diagnoses less likely (1,2).
In conclusion, the present study describes the case
of a middle-aged male patient with unilateral pseudo-abducens palsy
and contralateral headache as manifestations of acute thalamic
stroke. The present case report suggests that thalamic infarctions
should be listed as a probable cause of pseudo-abducens palsy.
Moreover, patients presenting with acute thalamic syndrome probably
have a good prognosis. The case study highlights the need for an
in-depth understanding of the complex neural pathways within the
thalamus, as well as the various clinical outcomes that can occur
following a thalamus infarction. Further investigations are
necessary in order to better understand the underlying mechanisms
and to optimize treatment approaches for patients presenting with
similar complications associated with thalamic strokes.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JPR was a main contributor to the conception of the
study, as well as to the literature search for related studies.
HTA, AR and ALFC were involved in the literature review, in the
writing of the manuscript, and in the analysis and interpretation
of the patient's data. JPR and ALFC confirm the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent for
participation
The present study was performed in accordance with
the ethical standards of the Declaration of Helsinki, 1964.
Informed consent was obtained from the patient for inclusion in the
study. Ethics approval was waived by the local committee as no
personal data were used.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dydyk AM and Munakomi S: Thalamic pain
syndrome. In: StatPearls. StatPearls Publishing, Treasure Island
(FL), 2023.
|
|
2
|
Chen XY, Wang Q, Wang X and Wong KS:
Clinical features of thalamic stroke. Curr Treat Options Neurol.
19(5)2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Schmahmann JD: Vascular syndromes of the
thalamus. Stroke. 34:2264–2278. 2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cambier J: Dejerine-Roussy syndrome. Rev
Neurol (Paris). 138:979–988. 1982.PubMed/NCBI(In French).
|
|
5
|
Pullicino P, Lincoff N and Truax BT:
Abnormal vergence with upper brainstem infarcts: Pseudoabducens
palsy. Neurology. 55:352–358. 2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Thomas C and Dawood S: Cranial nerve VI
palsy (Abducens nerve). Dis Mon. 67(101133)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Reid MS, DePoe SA, Darner RL, Reid JP and
Slagle WS: Clinical presentation of pseudo-abducens palsy. Optom
Vis Sci. 92:S76–S80. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ghasemi M, Riaz N, Bjornsdottir A and
Paydarfar D: Isolated pseudoabducens palsy in acute thalamic
stroke. Clin Imaging. 43:28–31. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wiest G, Mallek R and Baumgartner C:
Selective loss of vergence control secondary to bilateral
paramedian thalamic infarction. Neurology. 54:1997–1999.
2000.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Vanhoutte EK, Faber CG, Van Nes SI, Jacobs
BC, van Doorn PA, van Koningsveld R, Cornblath DR, van der Kooi AJ,
Cats EA, van den Berg LH, et al: Modifying the medical research
council grading system through Rasch analyses. Brain.
135:1639–1649. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fisher CM: The pathologic and clinical
aspects of thalamic hemorrhage. Trans Am Neurol Assoc. 84:56–59.
1959.PubMed/NCBI
|
|
12
|
Leichnetz GR: The prefrontal
cortico-oculomotor trajectories in the monkey. J Neurol Sci.
49:387–396. 1981.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Vestergaard K, Andersen G, Nielsen MI and
Jensen TS: Headache in stroke. Stroke. 24:1621–1624.
1993.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Graham C, Gurnani B and Mohseni M:
Abducens Nerve Palsy. In: StatPearls. StatPearls Publishing,
Treasure Island (FL), 2023.
|
|
15
|
Sundaram AN and Gelkopf MJ: Abducens Nerve
Palsy as a presenting symptom of multiple Sclerosis. Turk J
Ophthalmol. 52:291–294. 2022.PubMed/NCBI View Article : Google Scholar
|