1. Introduction
Spinal tuberculosis (ST) or Pott's disease is the
infection of the tissues of the spine, particularly the vertebrae
and the intervertebral discs, caused by Mycobacterium
tuberculosis (MT) (1). ST
typically originates when MT-infected droplets are inhaled,
primarily affecting the lungs, then entering the bloodstream and
spreading to other sites of the body. including the spine (2). Therefore, ST is often the consequence
of hematogenous dissemination into the dense vascular system of the
spongy bone of the vertebral bodies (3).
The incidence of tuberculosis has exhibited an
increasing trend over the past decade, reaching eight million new
cases per year (4). ST remains a
worldwide health concern, accounting for 3 to 4% of tuberculosis
cases and 15% of extra pulmonary localizations, and constitutes
>50% of all musculoskeletal tuberculosis cases (5). ST may lead to the development of severe
spinal and neurological sequelae. In fact, the occurrence of this
pathology is often misleading and it is characterized by insidious
clinical manifestations, which can lead to a delayed diagnosis and
severe complications, such as spinal deformity, paraplegia or
tetraplegia (6).
The therapeutic management of ST is based on a
multidisciplinary approach, including medical treatment
(anti-tuberculosis chemotherapy), on-demand surgery and a specific
rehabilitation program (7).
Rehabilitation is often a multidisciplinary approach, aimed at
restoring and enhancing an individual's physical, mental and social
well-being following illness or disability. It involves
personalized assessment, goal setting, and a combination of
medical, therapeutic and educational interventions provided by a
various team of healthcare professionals (physiatrists,
physiotherapists and occupational therapists). The main goal of
rehabilitation is to improve the quality of life (QoL) and
functional abilities of patients (8). Thus, rehabilitation management
constitutes a crucial part of the treatment of patients with ST,
alongside medical therapy. The implementation of the rehabilitation
program is based on a narrow clinical evaluation, seeking the
assessment of spinal and neurological complications. Although
rehabilitation plays a crucial role in the management of ST, it has
not yet received adequate research attention. Thus, analyzing the
literature in this field could be of paramount importance.
Therefore, the present review aimed to outline the rehabilitation
options associated with clinical features, potential complications
and the advancement of the disease.
2. Rehabilitation of ST neurological
complications
A well-defined rehabilitation program should be
tailored according to the location of the lesion, the severity of
the neurological deficit and the actual functional status. Patients
with ST with neurological disorders secondary to spinal cord
compression are commonly assessed using the American Spinal Injury
Association (ASIA) Impairment Scale (AIS), which provides a
standardized method used to determine the level and the severity of
the neurological impairment (9). The
AIS grading criteria are as follows: Grade A, complete spinal cord
injury (SCI) with a complete loss of sensory and motor function in
the sacral segments S4 ± S5; grade B, incomplete injury with
sensory preservation and a complete loss of motor function below
the neurological level, extending to the sacral segments S4 ± S5;
grade C, incomplete injury with motor function preserved below the
neurological level, but most key muscles below this level have a
muscle grade <3; grade D, incomplete injury with motor function
preserved below the neurological level, and most key muscles below
this level have a muscle grade ≥3; grade E, normal sensory and
motor function (no impairment).
Therefore, patients ST with neurological deficit due
to spinal cord compression should be managed with the basics of the
SCI program (10) which requires the
following: Preventive measures of bed confinement complications
(adaptive support, pressure ulcer prevention mattress, alternate
positions and early progressive verticalization), general
peripheral articular mobilization (passive, helped-active or
active), core and upper limb strengthening exercises, breathing
exercises, encountered spastic muscle posturing and stretching, and
the assessment of any vesico-sphincter disorders in order to avoid
damage to the upper urinary tract and to preserve renal function.
In fact, some cases may require intermittent catheterization
training to maintain appropriate bladder emptying. In the latter
situation, a physiatrist educates and supports the patient or their
caregiver in performing clean intermittent catheterization. The
physiatrist emphasizes various precautions, including adequate hand
hygiene to reduce the risk of urinary tract infections, ensuring
comfortable positioning, and gently inserting the lubricated
catheter to prevent urethral irritation or injury. Initially, the
physiatrist conducts the procedure with detailed explanations, and
the patient then carries it out under the doctor's supervision.
Regular follow-up appointments are necessary to assess the
patient's proficiency and provide ongoing assistance to ensure the
continued success of the procedure.
For example, in the case of ST with L1 spinal cord
compression and an AIS grade A, the prognosis is expected to be
severe, resulting in paraplegia with a complete loss of motor and
sensory capabilities below the L1 neurological level. The patient
will be exposed to frequent complications, such as deep vein
thrombosis and thromboembolic events, pressure sores and decubitus
ulcers. Additionally, they may experience disuse-induced muscle
atrophy, urinary tract infections, urinary retention, bladder
dysfunction and constipation. The rehabilitation management is
primordial in this case, consisting of passive mobilizations of the
lower limbs and the prescription of compression socks to improve
lower limbs circulation, specific mattress, alternating positions,
and early progressive verticalization for ulcer prevention, and
intermittent urinary catheterization is vital to prevent urinary
infections and upper urinary tract complications. This management
will be tailored according to clinical improvement.
The rehabilitation program may be challenging in the
case of ST, involving the cervical spinal level. In the case of
complete tetraplegia, particularly when cervical stages above C6
are involved and the case is categorized as AIS grade A, bed
confinement complication preventive measures are of paramount
importance. Special attention should be paid to alternating
positions, correct patient positioning, breathing exercises and
chest physiotherapy, as well as urinary catheterization. In fact,
the risk of ulcers, respiratory complications, joints stiffness and
deformities, and urinary complications is higher in tetraplegic
patients. Thus, the paralysis of upper and lower limbs implicates
the constant need for external assistance to perform these
measures. Furthermore, these patients are characterized by
dysautonomia complications, including cardiovascular issues,
impaired temperature regulation and autonomic dysreflexia. Thus,
regular monitoring by a healthcare professional is crucial to
tailor treatment.
Despite the ST level, in patients with AIS grade D
or E, the rehabilitation program will focus mainly on flexibility
and strengthening exercises, proprioception techniques, balance and
gait tasks, and cardiorespiratory reconditioning.
3. Rehabilitation of pain associated with
ST
Pain is the main complaint of patients with ST. Of
note, 90 to 100% of patients complain of back pain (11). The immobilization of the affected
spinal segment with adequate equipment (a corset in the case of
lumbar or dorsal involvement and a cervical collar in the case of
cervical spine involvement) and in some cases, strict bed rest, are
primordial measures used to decrease the intensity of pain
(12). In fact, bracing offers the
advantage of combining several targeted objectives which are
restricting movement, relieving pressure, promoting the healing and
relieving the weight on the involved spinal region. Furthermore,
bracing is of paramount importance following eventual surgery,
providing post-operative support. However, attention should be paid
to the occurrence of decubitus complications potentially worsening
the prognosis. Thus, early and progressive physiotherapy could be
helpful to prevent such complications (13).
In addition to painkillers, physical means,
particularly transcutaneous electrical nerve stimulation (TENS),
are paramount, mainly in the management of neuropathic pain by
activating the gait control at the spinal level, therefore
modulating painful pathways. For nociceptive pain, TENS with other
heat physical means, such as ultrasounds and infrared light may
attenuate patients' pain by acting on superficial and subcutaneous
anatomical structures and reducing local pain mediators. However,
before employing TENS, it is imperative to observe several
precautions to guarantee its safe and effective application. A
physiatrist should rule out any medical conditions, such as a
pacemaker, heart condition, epilepsy, skin diseases or sensory
impairment that contraindicate the application of TENS. In
addition, the presence of a physiotherapist is obligatory during
the TENS session to ensure vigilant monitoring for skin
sensitivity, irritation, burns, or allergic reactions. Therefore,
adhering to precautions diligently and promptly addressing any
side-effects is indispensable for ensuring the safe and effective
utilization of TENS therapy in pain management. Additionally, joint
mobilizations and musculo-tendinous stretching are useful for
relieving musculo-skeletal pain (12,13).
4. Rehabilitation of ST musculoskeletal,
postural, balance and gait complications
Musculoskeletal complications, essentially joint
stiffness, apart from upper and lower limb and spinal muscular
weakness should be managed in order to prevent the increased risk
of possible bone destruction and deformity, and to promote
functional outcomes. The rehabilitation program may involve the
following: A range of motion exercises to all joints of the upper
and lower limbs to maintain or improve joint mobility, and prevent
muscular contractures and hypotrophy (12). Additionally, the strengthening of
core and upper and lower limb muscles through isometric and
resistive exercises using manual resistance initially, and weight
cuffs at a later stage, allows for overcoming muscular
weakness.
Furthermore patients with ST are at a high risk of
developing postural abnormalities, particularly spinal kyphosis
(14). Thus, the education of
patients on proper body mechanics and posture, alongside specific
rehabilitation techniques are paramount for minimizing the risk of
spinal deformities, particularly kyphosis and adjusting postural
issues (15). These techniques may
comprise active the axial self-stretching of the spine, thoracic
expansion work, repositioning and the active stretching of the
anterior pectoralis and lower limbs muscles, and the strengthening
of the spinal extensor muscles with isometric, concentric and
eccentric dynamic exercises. The strengthening program should be
progressive, beginning with isometric contractions (where the
muscle contracts but does not change length, and there is no
movement at the joint; the force generated by the muscle is equal
to the applied resistance), and subsequently progressing to
concentric contractions (where the muscle contracts while
shortening, and the force generated is greater than the applied
resistance), and ultimately to eccentric contractions (where the
muscle contracts while lengthening, and the force generated is less
than the applied resistance). These exercises should be performed
under the supervision of a physical therapist to ensure these are
commenced with appropriate weight, gradually increasing intensity,
and monitoring muscle fatigue to prevent muscle soreness and
damage. Patients may receive instructions and ergonomic advices to
promote and maintain an appropriate posture during daily
activities.
Neurological and musculoskeletal impairments may
lead to balance and proprioception disorders, particularly in the
elderly and those with morbidities who are at a high risk of falls
and loss of autonomy. Exercise-based rehabilitation aiming at the
improvement of sensory perception and proprioception in affected
limbs enables patients to regain stability, enhance coordination,
restore normal walking patterns and improve mobility. This, in
turn, helps reduce the risk of falls and injuries, particularly in
elderly patients. Exercises focus on walking ability and
proprioception, according to the neurological damage and the degree
of recovery. They may involve assisted walking with the aid of a
physical therapist and mobility aids, such as a walker or parallel
bars, functional electrical stimulation to stimulate leg muscles
and promote walking patterns, and seated leg extensions targeting
the quadricep muscles and improve knee stability (16). In order for patients to maintain
their autonomy, further assistive equipment, such as crutches,
walking frames and wheelchairs may be helpful.
Additionally, patients are prescribed postural
reprogramming, involving exercises to correct seated and standing
postures, the stretching of tight muscles, biofeedback training
utilizing devices or mirrors for visual feedback on posture
alignment, and breathing exercises aimed at promoting relaxation
and proper spine alignment. Patients are re-trained to perform
progressive resistance training with hand resistance, resistance
bands and free weights, and functional training focusing on daily
living activities (16). Daily
activities and QoL may be promoted by physical therapy,
occupational therapy, ergonomic advices and the patient's
environmental adaptation.
5. ST cardiorespiratory rehabilitation
Patients with ST commonly have limited activity
during the acute phase of the disease with frequent
cardiorespiratory deconditioning. In this stage, patients should
commence cardiorespiratory rehabilitation, even in bed confinement,
through breathing exercises, which include pursed lip breathing and
thoracic expansion exercises in order to improve respiratory
function. Furthermore, respiratory muscle training techniques,
including the use of incentive spirometers or respiratory muscle
trainers are useful for strengthening breathing muscles and
enhancing respiratory endurance. Flexibility exercises incorporated
in stretching routines targeting joint stiffness and muscle
tightness may enhance overall functional capacity (17).
Furthermore, cardiorespiratory rehabilitation will
involve working on walking ability, cardiovascular endurance and
reconditioning with a progressive schedule. Exercises programs may
begin with progressive walking with the aid of a physical therapist
and mobility aids such as a walker or parallel bars. Aerobic
exercises may involve arm ergometry, such as arm bike or hand cycle
training (combined effects on cardiovascular fitness and upper body
strength), treadmill, staircase climbing, stationary bicycle and
aquatic therapy (aerobic exercises in water). At an advanced stage,
fast walking, jogging and running with interval training
(alternating between periods of high intensity exercise and rest or
lower intensity exercise) may be used according to the capacities
of the patient (12).
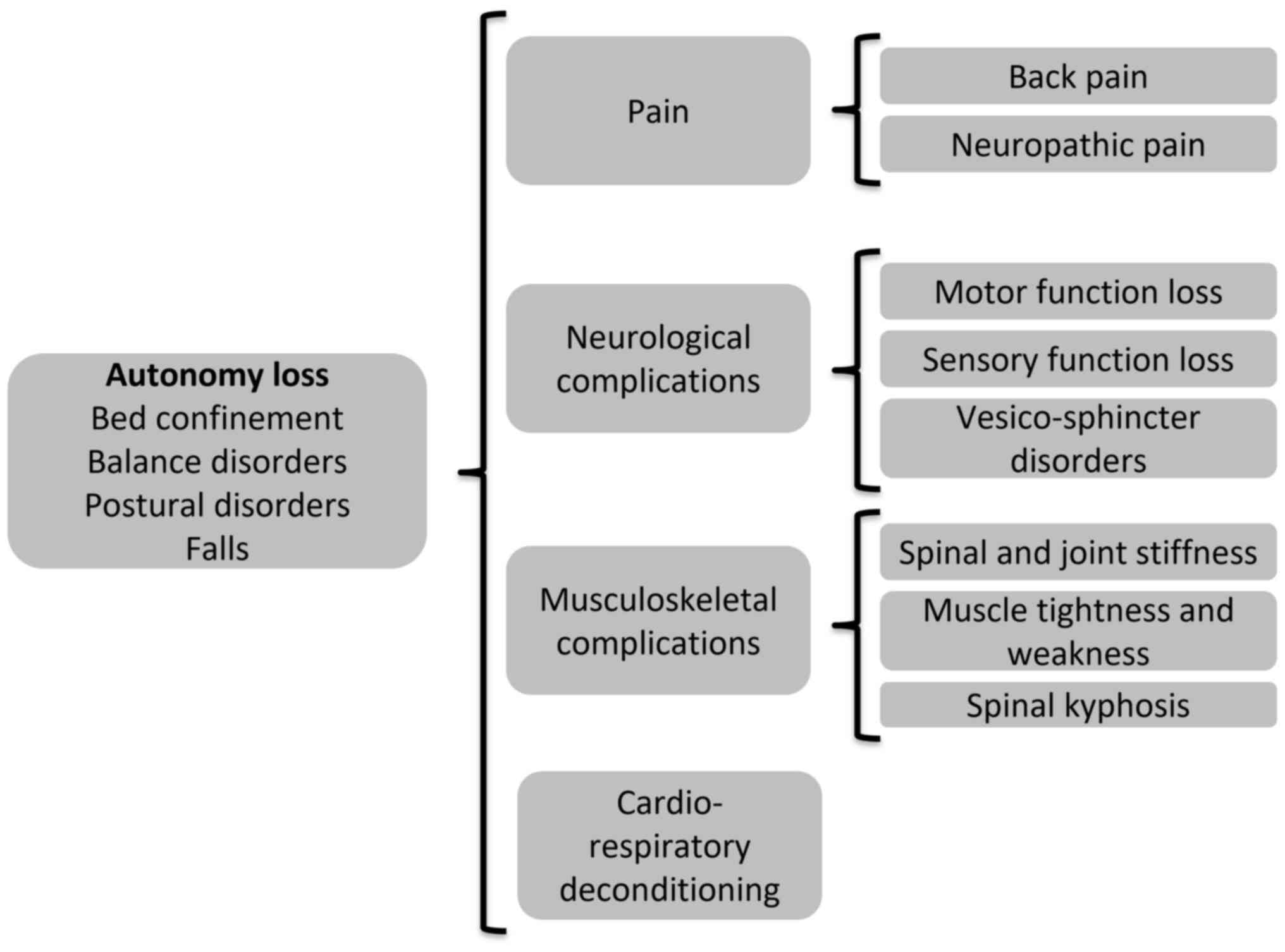
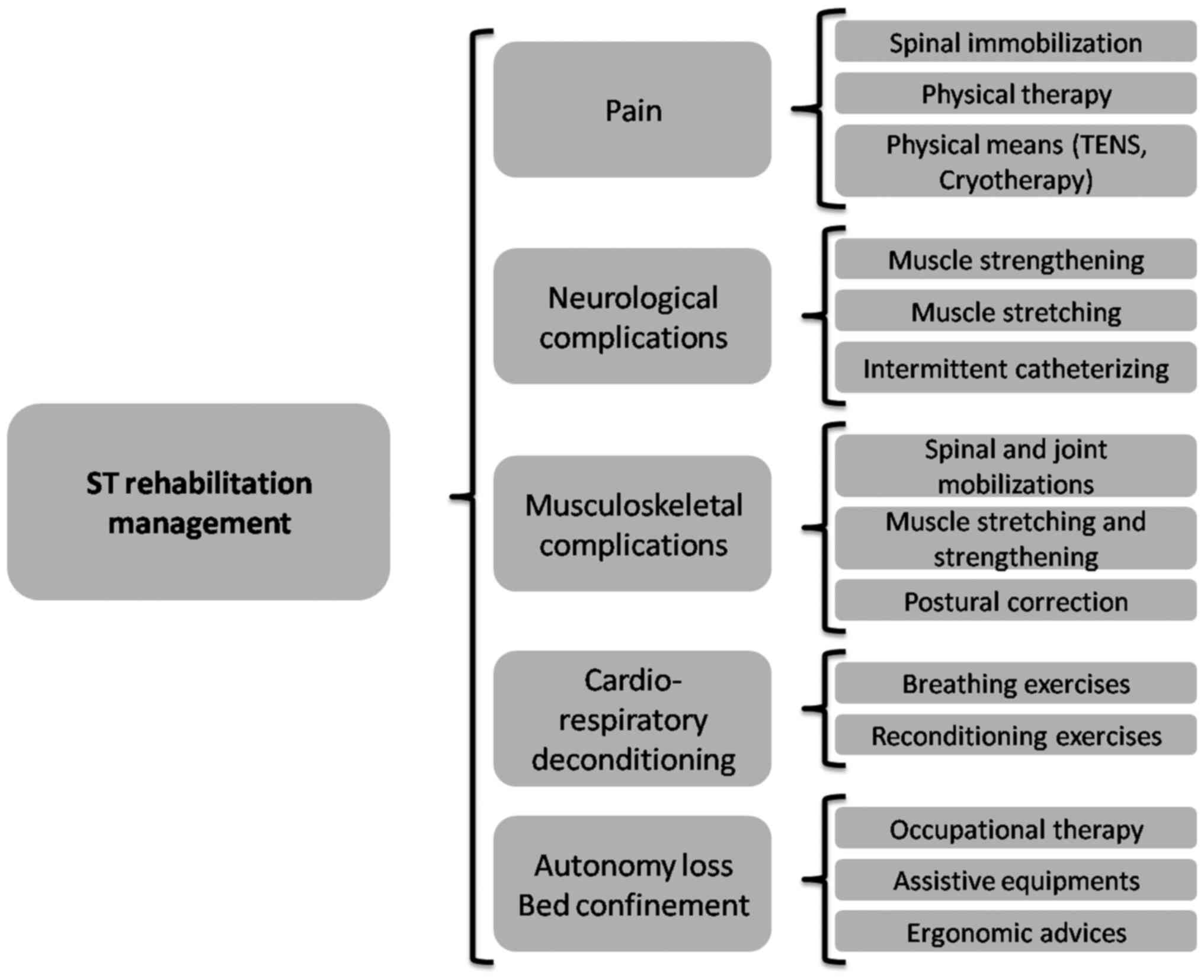
In summary, the combination of several symptoms and
complications of ST may result in the loss of autonomy and bed
confinement, accompanied by several related complications (Fig. 1). The rehabilitation management of
patients with ST offers multiple options, targeting the main
disabling symptoms and clinical abnormalities (Fig. 2).
6. Conclusion and future perspectives
Rehabilitation plays a crucial role in the
management of patients with ST, addressing a spectrum of
complications, including neurological, pain, musculoskeletal,
postural, balance, gait and cardio-respiratory issues. Hence, it
aims at primarily minimizing disability, regaining autonomy and
improving the QoL of patients. Rehabilitation programs should be
tailored according to the impairments of patients, such as muscle
weakness, spine and joint stiffness, postural disorders, and
cardio-respiratory deconditioning. Despite the plethora of
rehabilitation techniques with notable efficacy in the management
of ST, there remains a lack of well-codified programs tailored to
its stages and complications. Further research is imperative,
particularly to analyze optimal bracing duration and
verticalization delay. Robotics and artificial intelligence hold
promise for significantly enhancing the efficacy of rehabilitation
in this domain.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
JD, ZBSF and AJ were involved in the conception and
design of the study. JD, AK and AA were involved in the literature
search for related studies. JD, AC and AJ were involved in the
analysis and interpretation of the data in the identified
literature. All authors were involved in the drafting and
preparation of the manuscript, and all authors have read and
approved the final version of the manuscript. Data authentication
is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing
interests.
References
|
1
|
Garg D and Goyal V: Spinal tuberculosis
treatment: An enduring bone of contention. Ann Indian Acad Neurol.
23:441–448. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Dunn RN and Ben Husien M: Spinal
tuberculosis: Review of current management. Bone Joint J.
100-B:425–431. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rahim Khan S, Ahmad A, Saqib M and
Iftikhar M: Cervical Pott's disease presenting as quadriplegia in a
young patient: A case report. Cureus. 15(e46949)2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Heyde CE, Lübbert C, Wendt S, Rodloff A,
Völker A and von der Höh NH: Spinal tuberculosis. Z Orthop Unfall.
160:74–83. 2022.PubMed/NCBI View Article : Google Scholar : (In English,
German).
|
|
5
|
Leowattana W, Leowattana P and Leowattana
T: Tuberculosis of the spine. World J Orthop. 14:275–293.
2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Goyal R and Parakh A: Post-tuberculosis
sequelae in children. Indian J Pediatr: Nov 20, 2023 (Epub ahead of
print).
|
|
7
|
Jasiewicz B and Helenius I: Tumors and
infections of the growing spine. J Child Orthop. 17:556–572.
2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Negrini S, Meyer T, Arienti C, Kiekens C,
Pollock A, Selb M and Stucki G: 3rd Cochrane Rehabilitation
Methodology Meeting participants. The 3rd Cochrane rehabilitation
methodology meeting: ‘Rehabilitation definition for scientific
research purposes’. Eur J Phys Rehabil Med. 56:658–660.
2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kirshblum S, Snider B, Rupp R and Read MS:
International Standards Committee of ASIA and ISCoS. Updates of the
international standards for neurologic classification of spinal
cord injury: 2015 and 2019. Phys Med Rehabil Clin N Am. 31:319–330.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zaoui A, Kanoun S, Boughamoura H, Ben
Maitigue M, Bouaziz MA, Khachnaoui F and Rejeb N: Patients with
complicated Pott's disease: Management in a rehabilitation
department and functional prognosis. Ann Phys Rehabil Med.
55:190–200. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Na S, Lyu Z and Zhang S: Diagnosis and
treatment of skipped multifocal spinal tuberculosis lesions. Orthop
Surg. 15:1454–1467. 2023.PubMed/NCBI View
Article : Google Scholar
|
|
12
|
Mandhane KS, Phansopkar P and Chitale NV:
Physiotherapy rehabilitation of a conservatively managed patient
with Pott's disease: A case report. Cureus.
15(e33815)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ahuja K, Gupta T, Ifthekar S, Mittal S,
Yadav G and Kandwal P: Variability in management practices and
surgical decision making in spinal tuberculosis: An expert
survey-based study. Asian Spine J. 16:9–19. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Boussaid S, M'rabet M, Rekik S, Jammali S,
Rahmouni S, Zouaoui K, Sahli H and Elleuch M: Spinal tuberculosis:
Features and early predictive factors of poor outcomes. Mediterr J
Rheumatol. 34:220–228. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bettany-Saltikov J, Turnbull D, Ng SY and
Webb R: Management of spinal deformities and evidence of treatment
effectiveness. Open Orthop J. 11:1521–1547. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Defi IR, Hamam NR, Biben V and Al Barqi
NC: Improving functional outcomes and quality of life in an elderly
woman with sarcopenia and spinal tuberculosis: A case report. Front
Rehabil Sci. 4(1076010)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Basso-Vanelli RP, Di Lorenzo VA, Labadessa
IG, Regueiro EM, Jamami M, Gomes EL and Costa D: Effects of
inspiratory muscle training and calisthenics-and-breathing
exercises in COPD with and without respiratory muscle weakness.
Respir Care. 61:50–60. 2016.PubMed/NCBI View Article : Google Scholar
|