Introduction
All orbital tissues, including extra-ocular muscles,
can be affected by the varicella-zoster virus (VZV) (1). However, <10% of all patients with
VZV infections present with herpes zoster ophthalmicus. Notably,
there is a great variability as regards orbital involvement,
affecting 20-70% of individuals with herpes zoster ophthalmicus
(2). Usually, ophthalmic
complications of herpes zoster opthalmicus occur between 5 and 14
days following cutaneous lesions (3).
The present study reports the case of a middle-aged
male patient presenting with orbital myositis due to herpes zoster
ophthalmicus prior to the appearance of vesicular lesions. To the
authors' knowledge, there are only four cases reported in the
literature of herpes zoster ophthalmicus with orbital myositis
prior to the appearance of vesicular lesions (4-7).
Case report
A 56-year-old male patient with a prior medical
history of hyperlipidemia, and who was not on pharmacotherapy,
arrived at the Emergency Department of Cooper University Hospital,
Camden, NJ, USA with an acute intractable right-sided headache. His
headache began 3 days prior to his presentation and was described
as primarily right-sided with radiation to the neck, along with
associated fevers, blurred vision and photophobia. He stated he was
cleaning out an old farm devoid of animals during the onset of the
headache. Of note, the patient had no prior history of headaches,
and his only medication has been testosterone cypionate by
intramuscular route once every 4 weeks over the past 6 months. He
had no previous surgical history and no pertinent family history of
neuropsychiatric disorders.
In the emergency department, an examination of his
vital signs revealed a temperature of 98.5 F, a blood pressure of
141/67 mmHg, a heart rate of 88 beats per minute and an oxygen
saturation of 96% in room air. A cardiopulmonary examination did
not reveal any notable findings. A head examination revealed
normocephalic and atraumatic findings, with normal bilateral
external ear canals. His neurological examination yielded normal
results. His sensory and motor examination revealed no focal
deficits and his coordination was normal. There was no evidence of
skin changes. In consideration of a differential inclusive of
intracranial hemorrhage vs. meningitis vs. venous thrombosis
secondary to anabolic abuse, a thorough workup was performed,
including a cranial computed tomography (CT) scan, cranial
CT-venogram and a lumbar puncture.
The cranial CT and CT venogram scans did not reveal
any notable findings. The lumbar puncture demonstrated a protein
level of 38 mg/dl, glucose level of 65 mg/dl and an acellular fluid
analysis. However, polymerase chain reaction of the cerebrospinal
fluid (CSF) revealed a positive result for VZV. The patient was
thus commenced on intravenous treatment with acyclovir at 10 mg/kg
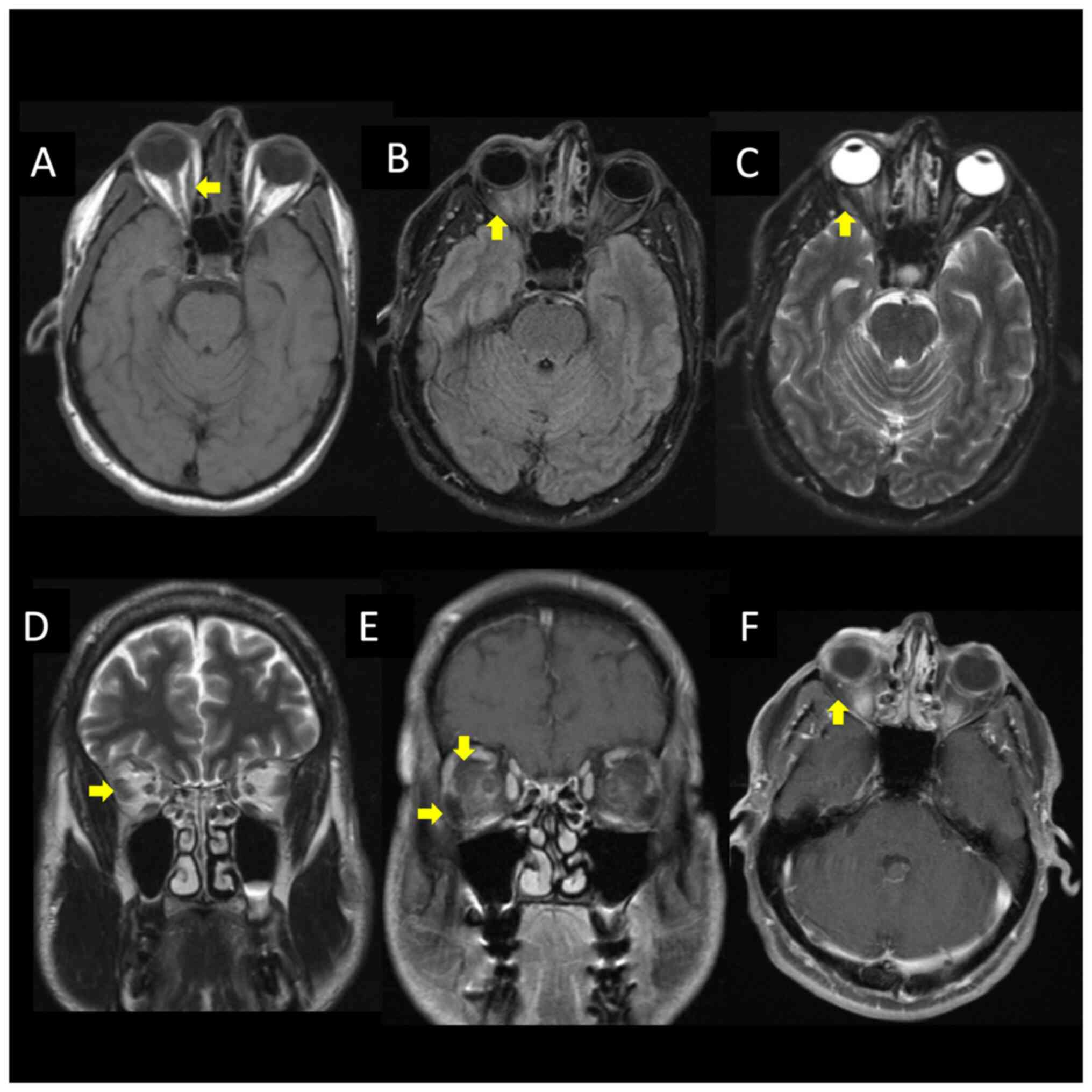
every 8 h, and a follow-up brain magnetic resonance imaging was
performed, revealing bilateral intraorbital intraconal enhancement
consistent with herpes zoster ophthalmicus with myositis (Fig. 1). An infectious disease consult was
pursued, and a course of intravenous acyclovir was continued
throughout his hospitalization period. The results of the complete
assessment of all the laboratory tests performed are presented in
Table I.
 | Table ILaboratory tests performed for the
patent in the present study. |
Table I
Laboratory tests performed for the
patent in the present study.
| Laboratory tests | Results |
|---|
| Complete blood cell
count | White blood cells
(5.41; 10x3/µl), red blood cells (5.7 10x6/µl), hemoglobin (16.9
g/dl), hematocrit (49.50%), mean corpuscular volume (86.8 fl), mean
corpuscular hemoglobin (29.6 pg), mean corpuscular hemoglobin
concentration (34.1 g/dl), red cell distribution width (12.80%),
platelet count (212; 10x3/µl), basophils (0.40%), eosinophils
(1.50%), granulocytes (53.50%), lymphocytes (29.20%) and monocytes
(14.8%) |
| Basic metabolic
panel | Glucose (83 mg/dl),
blood urea nitrogen (12 mg/dl), creatinine (1.32 mg/dl), sodium
(141 mmol/l), potassium (5.1 mmol/l), chloride (105 mmol/l),
CO2 (24 mmol/l), calcium (9.2 mg/dl), eGFR [63
ml/min/(1.73_m2)] |
| HIV antibody | Non-reactive |
| HIV p24 antigen | Non-reactive |
| COVID-19 PCR | Negative |
| Influenza A | Negative |
| Influenza B | Negative |
| Lyme antibody | Negative |
| Cerebrospinal fluid
analysis | Appearance (clear and
colorless), protein (38 mg/dl), corrected nucleated cells (2/µl),
red blood cells (<1/µl), glucose (65 mg/dl), cryptococcal
antigen (negative) |
| Cerebrospinal fluid
polymerase chain reaction | Escherichia
coli (negative), Neisseria meningitidis (negative),
Haemophilus influenzae (negative), Listeria
monocytogenes (negative), Group B streptococcus
(negative), Streptococcus pneumoniae (negative),
Cryptococcus neoformans (negative),
Cytomegalovirus (negative), Herpes simplex virus 1
and 2 (negative), Enterovirus (negative), varicella zoster
virus (positive) |
| Cerebrospinal fluid
cultures | Acid-fast bacteria
(no growth), cerebrospinal fluid fungal (no growth), cerebrospinal
fluid (no growth) |
During his admission, the symptoms of the patient
evolved into a shock-like pain over the scalp associated with pain
in ocular movements. His clinical course was further complicated by
a follicular reaction on the palpebral conjunctiva, which was
determined to be a viral follicular conjunctivitis likely secondary
to the VZV. On the 2nd day of admission, he developed new vesicular
lesions found on the right-side cranial nerve V1 dermatome
(Fig. 2). On the 4th day of
admission, he began to experience relief from his headache and
ocular disturbances. By the 6th day of admission, he had
experienced the complete resolution of his symptoms, and his
physical examination revealed the resolution of the dermatologic
manifestations of the VZV. The culture of his CSF remained
negative. The patient was stable for outpatient follow-up with
ophthalmology and was discharged on an oral valacyclovir (1 g, 2
tablets every 6 h) course for 7 days.
Discussion
Orbital myositis is characterized by worsening pain
with eye movements. Other common features in individuals with
orbital myositis are proptosis, swollen eyelids and hyperemic
conjunctiva. Common causes of orbital myositis are thyroid disease,
syphilis and auto-immune diseases, which were not observed in the
patient described herein. His ocular pain related to eye movements
significantly improved after treatment with acyclovir was
commenced, and he fully recovered within 1 week of therapy.
The patient was treated with acyclovir intravenously
when he was hospitalized and his treatment regiment was then
changed to oral valacyclovir for a period of 7 days. As clinical
signs and symptoms associated with VZV, the CNS infection improved
and the patient was able to take oral medications; therapy was thus
completed with oral treatment. Acyclovir and valacyclovir are both
effective against VZV CNS infections. Notably, acyclovir, compared
to valacyclovir, has some drawbacks, including dosing at multiple
times per day, poor oral bioavailability and inadequate CNS
penetration/levels, which render oral acyclovir a suboptimal option
for such cases (8).
A previous study by Marsh and Cooper (9), using a large cohort, assessed 1,356
patients with herpes zoster ophthalmicus. That study found that
extraocular muscle involvement was associated with the appearance
of skin lesions and that the severity of the rash was related to
recurrence and postherpetic neuralgia. However, that study did not
describe neuroimaging analyses (9).
In addition, to date, to the best of our knowledge, there are no
radiological and histopathological studies available associating
orbital myositis with herpes zoster ophthalmicus.
In 1948, Parkinson (10) described a case of herpes zoster
ophthalmicus followed by ptosis on the same side. He reported that
idiopathic cases of myositis should be reserved only after the
availability of negative serological and immunological results for
herpes zoster (10). Of note, 10
years later, Lewis (11) reported a
syndrome known as ‘ophthalmic zoster sine herpete’, characterized
by orbital pain, extraocular palsy and periorbital skin swelling
without skin rashes.
In the case in the present study, the patient
developed a significant headache with concern from vascular
etiology. Following initial neuroimaging, the CSF was analyzed, and
the VZV infection was noticed. A possible explanation for the
headache could be related to prodromal symptoms or myositis
affecting the extraocular muscles. Ophthalmic complications
following herpes zoster ophthalmicus may result from inflammatory
changes, nerve damage, or secondary tissue scarring.
The authors searched six databases to locate studies
describing the appearance of myositis prior to skin manifestations
in individuals with herpes zoster ophthalmicus published from 1991
to January, 2024 in electronic form. The Excerpta Medica (Embase),
Google Scholar, Latin American and Caribbean Health Sciences
Literature (Lilacs), Medline, Scientific Electronic Library Online
(SciELO), and ScienceDirect databases were searched. Publications
in the English language were included in the search (Table II).
 | Table IICases reported in the literature of
orbital myositis preceding skin symptoms in patients with varicella
zoster infection. |
Table II
Cases reported in the literature of
orbital myositis preceding skin symptoms in patients with varicella
zoster infection.
| Author(s), year of
publication | Age (years)/sex | Comorbidities | Timea (days) | Neurologic
manifestations | Management and
outcomes | Comments | (Refs.) |
|---|
| Volpe and Shore,
1991 | 45/M | Colitis | 3 | Proptosis | Initially, oral
prednisone for idiopathic orbital inflammation was prescribed.
After the skin lesion appeared, oral acyclovir and prednisone for
three days were prescribed. After three days, the symptoms
returned, and he received seven days of the same therapy. A
complete imaging resolution was observed within seven weeks. | First report. Only a
cranial CT scan was performed. | (4) |
| Kawasaki and Borruat,
2003 | 47/F | NA | 4 | Proptosis and pain
worsen with ocular movements | IV and topical
acyclovir, and. prednisone | First report with.
brain MRI | (5) |
| Tseng, 2008 | 54/M | Liver cirrhosis | 7 | Proptosis and pain
worsen with ocular movements | 7 Days of IV
acyclovir. treatment and discharged. After 7 days, he returned with
the same symptoms, and he received 7 days of valacyclovir. A
complete imaging resolution was observed within 3 months. PHN was
observed at the follow-up | Visual evoked
potential was normal. Hutchinson's sign. | (6) |
| Bak et al,
2018 | 59/F | Healthy | 8 | Proptosis | IV dexamethasone 10
mg once a day for 2 days and oral famciclovir 750 mg once a day for
10 days were administered. Oral prednisolone 10 mg once a day for
10 days was prescribed. | Dacryoadenitis. | (7) |
| Rissardo et
al | 56/M | Hyperlipidemia | 5 | Pain worsening with
ocular movements | IV acyclovir 10 mg/kg
every 8 h for 6 days, followed by oral valacyclovir course for 7
days. | | Present study |
To the authors' knowledge, Volpe and Shore (4) described the first case of orbital
myositis appearing before skin manifestations in individuals with
herpes zoster ophthalmicus. They reported the enlargement of
extraocular muscles with tendon sparing on a cranial computed
tomography scan, which appeared one day before the appearance of
the skin rashes.
Oh et al (12)
reported a patient presenting with eyelid swelling and headache;
that study is not included in Table
II. They described it as rare, as they considered only
vesicular rashes as a skin manifestation (12). Nevertheless, that case illustrates a
common presentation of individuals with herpes zoster with skin
lesions appearing prior to orbital myositis (8). In addition, Park and Lee (13), Chiang et al (14), Bae and An (15) and Pereira et al (16) and the first patient reported by Bak
et al (7) developed
periorbital erythematous edema at presentation; these studies are
not included in Table II.
The general rule is that the optimal time for
initiating antiviral medication is within 72 h following the onset
of the vesicular rash. However, the role of systemic steroid
therapy in acute orbital syndromes caused by herpes zoster
ophthalmicus needs to be further investigated. In the case
described herein, this class of medication was not prescribed.
However, corticosteroids can attenuate the pain, and may also
influence the course of the viral infection by inflammatory
pathways.
A possible differential diagnosis for the case in
the present study is testosterone-induced myositis. The patient had
used testosterone for the past 6 months due to low testosterone
levels and symptoms of sexual dysfunction, mood disorder and
generalized weakness. Notably, testosterone-induced orbital
myositis is uncommonly observed in humans, although it is a common
finding in rat models (17).
However, myositis secondary to testosterone was considered unlikely
in the patient in the present study, as the patient had used
testosterone for a long period of tims and had VZV found in the
CSF.
In conclusion, patients with orbital pain who have a
significant headache should be further investigated. Herpes zoster
virus serology needs to be investigated before a final diagnosis of
idiopathic orbital myositis is made. The case described in the
present study favors management with oral antivirals following a
course of at least 5 days with intravenous medications.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors (JPR, ALFC and PP) contributed to the
diagnosis and treatment of the patient, and to the conception of
the study. JPR was a major contributor to the writing of the
manuscript. JPR and PP confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study followed international and
national regulations and was performed in agreement with the
Declaration of Helsinki, and ethical principles. The patient signed
an informed consent form.
Patient consent for publication
The patient provided written informed consent for
the publication of any data and/or accompanying images. Patients
have a right to anonymity and privacy, and authors have a legal and
ethical responsibility to respect this right.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gurwood AS, Savochka J and Sirgany BJ:
Herpes zoster ophthalmicus. Optometry. 73:295–302. 2002.PubMed/NCBI
|
|
2
|
McCrary ML, Severson J and Tyring SK:
Varicella zoster virus. J Am Acad Dermatol. 41:1–14.
1999.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Vardy SJ and Rose GE: Orbital disease in
herpes zoster ophthalmicus. Eye (Lond). 8:577–579. 1994.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Volpe NJ and Shore JW: Orbital myositis
associated with herpes zoster. Arch Ophthalmol. 109:471–472.
1991.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kawasaki A and Borruat FX: An unusual
presentation of herpes zoster ophthalmicus: Orbital myositis
preceding vesicular eruption. Am J Ophthalmol. 136:574–575.
2003.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tseng YH: Acute orbital myositis heralding
herpes zoster ophthalmicus: Report of a case. Acta Neurol Taiwan.
17:47–49. 2008.PubMed/NCBI
|
|
7
|
Bak E, Kim N, Khwarg SI and Choung HK:
Case series: Herpes zoster ophthalmicus with acute orbital
inflammation. Optom Vis Sci. 95:405–410. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cunha BA and Baron J: The pharmacokinetic
basis of oral valacyclovir treatment of herpes simplex virus (HSV)
or varicella zoster virus (VZV) meningitis, meningoencephalitis or
encephalitis in adults. J Chemother. 29:122–125. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Marsh RJ and Cooper M: Ophthalmic herpes
zoster. Eye (Lond). 7:350–370. 1993.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Parkinson T: Rarer manifestations of
herpes zoster; a report on three cases. BMJ. 1:8–10.
1948.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lewis GW: Zoster sine herpete. BMJ.
2:418–421. 1958.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Oh HY, Cho SW and Kim SH: Herpes zoster
ophthalmicus presenting as acute orbital myositis preceding a skin
rash: A case report. J Korean Soc Radiol. 66:213–216. 2012.
|
|
13
|
Park JH and Lee JE: An Unusual case of
orbital inflammation preceding herpes zoster ophthalmicus. J Korean
Ophthalmol Soc. 58:1099–1105. 2017.
|
|
14
|
Chiang E, Bajric J and Harris GJ: Herpes
zoster ophthalmicus with orbital findings preceding skin rash.
Ophthalmic Plast Reconstr Surg. 34:e113–e115. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bae DW and An JY: Herpes zoster
ophthalmicus presenting as acute orbital inflammation preceding the
vesicular rash. J Neurosonology Neuroimaging. 12:91–94. 2020.
|
|
16
|
Pereira A, Zhang A, Maralani PJ and
Sundaram AN: Acute orbital myositis preceding vesicular rash
eruption in herpes zoster ophthalmicus. Can J Ophthalmol.
55:e107–e109. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bai X, Zhang X and Zhou Q: Effect of
testosterone on TRPV1 expression in a model of orofacial myositis
pain in the rat. J Mol Neurosci. 64:93–101. 2018.PubMed/NCBI View Article : Google Scholar
|