Introduction
The treatment of cirrhotic patients with refractory
ascites is a clinical challenge for hepatologists. Refractory
ascites is defined as ascites that cannot be resolved using
standard doses of diuretics, namely spironolactone, loop and
thiazide diuretics, among others (1).
Patients with advanced cirrhosis have a decreased estimated
glomerular filtration rate (eGFR) due to diminished circulating
volume (2). This is partially due to
increased reabsorption in the proximal convoluted tubule, resulting
in a poor current in the distal convoluted tubule. Consequently,
the effect of vasopressin on the collecting duct is blunted,
resulting in sodium and water retention (2). Additionally, hypoalbuminemia due to
cirrhosis induces intravascular dehydration through decreased
colloid osmotic pressure. This depleted circulation volume may
decrease the effect of standard diuretics (2).
Tolvaptan, a novel aquaporin modulator, was made
available in Japan in 2013 for the treatment of patients with
refractory ascites due to cirrhosis (3). Tolvaptan enhances renal function by
inhibiting water reabsorption in the collecting duct, namely by
preventing the binding of vasopressin to V2 receptors and thus
suppressing the expression of aquaporin-2 (3). This therapeutic mechanism has the
potential to improve cirrhosis-induced ascites, and may decrease
the need for paracentesis, cell-free and concentrated ascites
reinfusion therapy, and trans-jugular intrahepatic portosystemic
shunt placement. A phase III trial of tolvaptan in Japan observed a
marked reduction in fluid retention in patients with refractory
ascites due to cirrhosis (4).
Additionally, tolvaptan may improve refractory ascites even in
patients with hypoalbuminemia (5).
However, despite the therapeutic potential of tolvaptan, few
reports are available on its clinical use, particularly regarding
long-term outcomes. Thus, the present study aimed to clarify the
short-term efficacy and review the long-term clinical outcomes of
tolvaptan in patients with refractory ascites due to cirrhosis.
Patients and methods
Study design
From June 2013 to April 2017, 89 patients with
refractory ascites due to cirrhosis were treated with tolvaptan at
Saiseikai Utsunomiya Hospital (Utsunomiya, Japan). The patient
medical records were retrospectively reviewed and data were
collected regarding the following parameters: Age, gender, weight,
body mass index, smoking habits, etiology of cirrhosis, Child-Pugh
classification (6), Model for
End-Stage Liver Disease (MELD) score (7), the presence of comorbidities, varices,
viable hepatocellular carcinoma (HCC) and/or pleural effusion,
history of hepatic encephalopathy, previous doses of standard
diuretics, laboratory findings and long-term follow-up data. The
presence of varices, HCC and pleural effusion was determined by
esophagogastroduodenoscopy, computed tomography/ultrasound and
chest X-ray. All patients were hospitalized for the control of
refractory ascites that had not been controlled by standard
diuretics (furosemide ≥20 mg/day and/or spironolactone ≥25 mg/day).
The starting dose of tolvaptan was 7.5 mg daily for all patients.
During hospitalization, sodium (Na) chloride intake was limited to
6 g/day while fluid intake was not limited. At present, there is no
formal criteria to define a ‘responder’ to diuretic treatment in
patients with refractory ascites due to cirrhosis. Therefore, a
“responder” was defined in the present study by ≥2 kg weight
reduction within seven days of starting tolvaptan. The follow-up
time was defined as the period between starting tolvaptan and the
last clinic visit or date of mortality. To obtain homogeneous data,
24 of the 89 patients were excluded for the following reasons:
Failure to measure weight (n=11), half-dose (3.75 mg) tolvaptan
intake (n=6), ascites drained by paracentesis within seven days of
starting tolvaptan (n=4) and warfarin use (n=3). The remaining 65
patients were analyzed as the final cohort. The study was approved
by the Institutional Review Board of Saiseikai Utsunomiya Hospital
(Utsunomiya, Japan) prior to data collection.
Statistical analysis
Cut-off values were determined using a receiver
operating characteristic curve to convert continuous data into
categorical data. To identify predictive factors associated with
response to tolvaptan, univariate and multivariate logistic
regression analyses were performed. For multivariate analysis,
factors were selected by the stepwise forward selection method. To
assess long-term follow-up data, risk factors associated with
survival were analyzed with the Cox proportional hazards model. The
Kaplan-Meier method with a log-rank test was used to compare the
survival curves of tolvaptan responders and non-responders, and
Child-Pugh scores prior to and at six months of tolvaptan therapy
were compared using a Wilcoxon rank sum test. Statistical analysis
was performed using StatFlex 6.0 software (Artech Co., Ltd., Osaka,
Japan) and differences were considered significant when
P<0.05.
Results
Baseline characteristics and
short-term outcomes
The mean age of the patients was 71.5±9.1 years, and
62% (40/65) exhibited hepatitis C virus (HCV) etiology, while 57%
(37/65) were classified as class C of the Child-Pugh classification
(Table I). All 40 patients with HCV
etiology exhibited a positive HCV-RNA tests. All patients received
furosemide (≥20 mg/day) and/or spironolactone (≥25 mg/day) prior to
starting tolvaptan therapy. After one week of tolvaptan treatment,
the mean weight reduction was 3.4±2.9 kg, with a 69% (45/65)
response rate to tolvaptan (Table I).
No adverse events occurred during the hospital stay.
 | Table I.Baseline characteristics and patient
outcomes. |
Table I.
Baseline characteristics and patient
outcomes.
| Variable | Total, n=65 |
|---|
| Age, years, mean ±
SD | 71.5±9.1 |
| Gender, male, n
(%) | 41 (63) |
| Weight, kg, mean ±
SD | 62.4±15.4 |
| Body mass index, mean
± SD | 24.5±4.6 |
| Current Smoker, n
(%) | 9 (14%) |
| Etiology, n (%) |
|
| HCV | 40 (62) |
|
Alcohol | 12 (18) |
| AIH | 4 (6) |
| PBC | 3 (5) |
| NASH | 1 (1) |
|
Unknown | 5 (8) |
| Child-Pugh
classification, class |
|
| B | 28 (43) |
| C | 37 (57) |
| MELD score, mean ±
SD | 12.4±4.8 |
| Comorbidities, n
(%) |
|
| Diabetes
mellitus | 24 (37) |
|
Hypertensiona | 10 (15) |
| Heart
failure | 3 (5) |
| Liver related
complications, n (%) |
|
|
Varices | 49 (75) |
| Viable
hepatocellular carcinoma | 28 (43) |
| History
hepatic encephalopathy | 23 (35) |
| Current
pleural effusion | 6 (9) |
| Diuretics, n (%);
mg/day, mean ± SD |
|
|
Furosemide | 54 (83);
43.5±20.8 |
|
Spironolactone | 54 (83);
48.6±27.9 |
|
Azosemide | 12 (18);
46.7±14.2 |
| Biochemistry |
|
| Platelet,
×10,000/µl) | 12.4±8.5 |
| Albumin,
g/dl | 2.3±0.5 |
| Total
bilirubin, mg/dl | 2.0±1.9 |
| Serum Na,
mEq/l | 137.0±4.7 |
| Serum K,
mEq/l | 3.9±0.5 |
| eGFR,
ml/min | 55.1±25.6 |
|
PT-INR | 1.3±0.3 |
| Weight reduction over
initial seven days, kg, mean ± SD | 3.4±2.9 |
| Tolvaptan responder,
n (%) | 45 (69) |
| Length of first
hospital stay, days, median (IQR) | 14 (9–24) |
| Follow-up period,
days, median (IQR) | 175 (56–406) |
Factors associated with tolvaptan
responders
Factors associated with response to tolvaptan were
analyzed (Table II). On univariate
analysis, maintaining serum Na ≥140 mEq/l and eGFR ≥55 ml/min were
significantly associated with response to tolvaptan (P<0.05). On
multivariate analysis, HCV etiology, maintaining serum Na ≥140
mEq/l and eGFR ≥55 ml/min were significantly associated with
response (P<0.05).
 | Table II.Factors associated with tolvaptan
response assessed by logistic regression analysis. |
Table II.
Factors associated with tolvaptan
response assessed by logistic regression analysis.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factor | OR | 95% CI | P-value | OR | 95% CI | P-value |
|---|
| Age, ≥75 years | 2.041 | 0.665–6.266 | 0.212 | – | – | – |
| Male gender | 0.886 | 0.295–2.661 | 0.830 | – | – | – |
| Hepatitis C virus
infection | 2.706 | 0.915–7.998 | 0.071 | 4.998 | 1.214–20.576 | 0.025 |
| Viable hepatocellular
carcinoma | 0.893 | 0.309–2.580 | 0.834 | – | – | – |
| Platelet,
≥90,000/µl | 1.647 | 0.568–4.771 | 0.357 | – | – | – |
| Serum albumin, ≥2.3
mg/dl | 0.583 | 0.200–1.699 | 0.323 | – | – | – |
| Total bilirubin,
≥1.7 mg/dl | 2.231 | 0.727–6.846 | 0.160 | – | – | – |
| Serum Na, ≥140
mEq/l | 5.420 | 1.391–21.106 | 0.014 | 8.291 | 1.641–41.870 | 0.010 |
| eGFR, ≥55
ml/min | 3.826 | 1.105–13.245 | 0.034 | 6.890 | 1.442–32.921 | 0.015 |
| PT-INR, ≥1.4 | 2.206 | 0.629–7.735 | 0.216 | – | – | – |
| History of
encephalopathy | 1.416 | 0.457–4.387 | 0.545 | – | – | – |
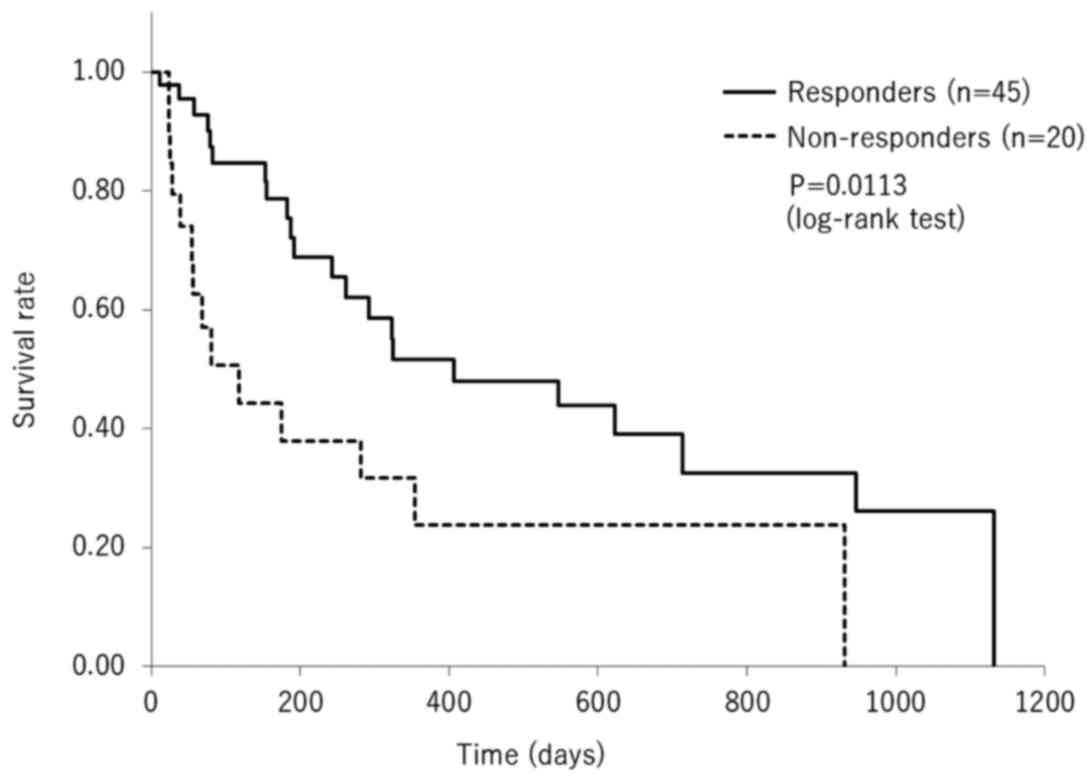
Long-term outcomes
The long-term outcomes of tolvaptan therapy were
evaluated. The median follow-up period was 175 days (interquartile
range 56–406). During the follow-up period, a total of 36 patients
succumbed, due to hepatic failure (n=20), hepatocellular carcinoma
(n=13), gastrointestinal bleeding (n=2) and heart failure (n=1).
Risk factors associated with survival were analyzed using the Cox
proportional hazards model. On univariate analysis, tolvaptan
responsiveness was a predictor of long-term survival (P=0.012),
while viable HCC was a predictor of short-term survival (P=0.044;
Table III). On multivariate
analysis, responsiveness to tolvaptan remained a predictor of
long-term survival (P=0.002), while hyperbilirubinemia was a
predictor of short-term survival (P=0.028; Table III). Kaplan-Meier analysis of
survival with a log-rank test indicated a significantly longer
overall survival time of responders compared with non-responders
(P=0.011; Fig. 1).
 | Table III.Risk factors associated with survival
analyzed by the Cox proportional hazards model. |
Table III.
Risk factors associated with survival
analyzed by the Cox proportional hazards model.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factor | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Responder to
tolvaptan | 0.418 | 0.210–0.830 | 0.012 | 0.269 | 0.113–0.638 | 0.002 |
| Age, ≥75 years | 1.410 | 0.709–2.804 | 0.326 | – | – | – |
| Male gender | 1.253 | 0.632–2.484 | 0.517 | 1.609 | 0.726–3.565 | 0.241 |
| Hepatitis C virus
infection | 1.953 | 0.883–4.323 | 0.098 | 2.170 | 0.906–5.198 | 0.082 |
| Viable
hepatocellular carcinoma | 2.008 | 1.016–3.969 | 0.044 | 1.336 | 0.581–3.072 | 0.495 |
| Platelet,
≥90,000/µl | 0.789 | 0.399–1.559 | 0.495 | – | – | – |
| Serum albumin, ≥2.3
mg/dl | 0.976 | 0.501–1.900 | 0.944 | – | – | – |
| Total bilirubin,
≥1.7 mg/dl | 1.425 | 0.718–2.825 | 0.310 | 2.447 | 1.098–5.455 | 0.028 |
| Serum Na, ≥140
mEq/l | 0.648 | 0.326–1.289 | 0.216 | – | – | – |
| Estimated GFR, ≥55
ml/min | 0.613 | 0.302–1.244 | 0.175 | – | – | – |
| PT-INR, ≥1.4 | 1.210 | 0.563–2.602 | 0.624 | – | – | – |
| History of
encephalopathy | 1.212 | 0.605–2.430 | 0.586 | – | – | – |
After six months of tolvaptan therapy, 19 patients
had succumbed and 15 were lost to follow-up. The remaining 31
patients were followed for more than six months. Child-Pugh scores
of the patients were assessed prior to and six months after
starting tolvaptan therapy to evaluate hepatic function. For the 31
patients followed for six months and longer, the Child-Pugh scores
were significantly decreased at six months (8.5±2.1) compared with
those prior to starting tolvaptan (9.7±1.2; P<0.001).
Discussion
The present retrospective cohort study demonstrated
that tolvaptan was an effective treatment for cirrhotic patients
with refractory ascites. Notably, HCV etiology and maintaining
serum Na ≥140 mEq/l and renal function ≥55 ml/min were
significantly associated with response to tolvaptan on multivariate
analysis. Additionally, response to tolvaptan was associated with
improved long-term outcomes in cirrhotic patients with refractory
ascites.
The short-term effects of tolvaptan in patients with
refractory ascites due to cirrhosis have been reported (8–13). As the
starting doses in previous studies were 3.75 mg with dose
escalation up to 7.5 mg within one week, tolvaptan doses in these
studies were heterogeneous. The dose of tolvaptan was consistent at
7.5 mg per day in the current study. In prior studies with a
starting dose of tolvaptan of 3.75 mg daily, weight reduction
within one week ranged from 1.5–3.8 kg (8–11,13). The mean weight reduction at one week
was 3.4±2.9 kg in the present study. Thus, the lower dose of
tolvaptan used in prior studies (3.75 mg) may be as effective as a
higher dose (7.5 mg). However, the optimal starting dose of
tolvaptan is yet to be determined in future studies.
In the current study, HCV-related cirrhosis was a
positive predictor for response to tolvaptan, as reported by Ohki
et al previously (11), though
the reason for this association remains unclear. A possible
explanation may be that alcohol-related cirrhosis was the etiology
for ~half of the patients with non-HCV-related cirrhosis in the
current study. Patients with alcohol-related cirrhosis may not be
as strictly followed compared with HCV-infected individuals, and
may have a delay in treatment with tolvaptan. Additionally,
patients with alcohol-related cirrhosis possibly have greater
intravascular dehydration than patients with HCV-related cirrhosis,
which may affect their response.
In the present study, patients with normal renal
function exhibited an adequate response to tolvaptan. It was also
identified that serum Na (>140 mEq/l) was a positive predictor
of response to tolvaptan. Umemura et al reported that serum
Na <139 mEq/l was significantly associated with mortality in
patients with cirrhosis (14).
Additionally, hyponatremia has been documented to be an independent
predictor for poor prognosis in patients with cirrhosis (7), and is observed in ~half of cirrhotic
individuals (15). Recent studies
have also reported that low serum creatinine is a predictor of
response to tolvaptan in the short-term in univariate analyses
(8,9).
Deterioration of renal function in patients with cirrhosis directly
influences their prognosis (7). In
contrast to standard diuretics, which cause hyponatremia and
glomerular damage with continuous and high dose administration, no
hyponatremia or glomerular damage has been observed with tolvaptan
treatment (8). Additionally, unlike
standard diuretics, tolvaptan is not affected by serum albumin
level (5). Tolvaptan may also resolve
hyponatremia, potentially resulting in improved survival (1,7). Although
administration of albumin may be a viable treatment option in
patients with refractory ascites, albumin is a high-cost medical
biological product. Therefore, the use of tolvaptan may be
appropriate in the early stages of cirrhosis prior to high-dose
administration of standard diuretics.
There are few reports of the long-term outcomes of
tolvaptan therapy in cirrhotic patients with refractory ascites.
Response to tolvaptan was associated with improved survival in the
current study. Previous studies have reported similar results from
univariate analyses (8,9). As aforementioned, renal function and
serum Na level may be considered as major indicators of tolvaptan
responsiveness, particularly as these are established prognostic
factors in patients with cirrhosis (7). To exclude confounding factors, the
present study used multivariate analysis and identified response to
tolvaptan as a positive predictor for survival. A recent Japanese
study reported similar results based on multivariate analysis
(13). It is probable that patients
who exhibit alleviated ascites are in less advanced disease stages,
and therefore have better prognosis. Regardless, a preserved serum
sodium and high eGFR, which may indicate preserved
cardiocirculatory function, may be potential predictors of
tolvaptan responsiveness. Furthermore, total serum bilirubin level
is an established negative prognostic marker in patients with
cirrhosis and is included in the MELD score (16).
Tolvaptan has been used for the treatment of
patients with heart failure worldwide (17). The Japanese health insurance system
began reimbursement for tolvaptan therapy in cirrhotic patients
with refractory ascites in 2013, as the first country globally
(3). Prior to the reimbursement of
tolvaptan therapy in Japan, dose escalation of spironolactone, loop
and thiazide diuretics had been the first-choice strategy for the
medical management of patients with refractory ascites, despite its
associations with glomerular damage and hyponatremia (3). Although abdominal paracentesis with
drainage, cell-free and concentrated ascites reinfusion therapy and
trans-jugular intrahepatic portosystemic shunt placement are
occasionally used, results suggest that these procedures do not
improve overall prognosis (18–20).
Tolvaptan may delay the need for invasive procedures and
readmission for patients with refractory ascites.
The present study had some limitations. Firstly, it
was a single center, retrospective study. Secondly, patients
treated without tolvaptan were not included as a control group.
Thirdly, the study defined a ‘responder’ by ≥2 kg weight reduction.
As body weight reduction may be caused various factors including
gastroenteritis, other parameters such as abdominal circumference
should have been measured. A future prospective study with a large
number of patients and longer follow-up is necessary to confirm the
current preliminary results.
In conclusion, tolvaptan was effective for the
treatment of patients with refractory ascites due to cirrhosis.
Tolvaptan was more effective in patients with HCV etiology, a
maintained serum Na ≥140 mEq/l and renal function (eGFR) ≥55
ml/min. Additionally, response to tolvaptan was a positive
independent predictor of survival, while hyperbilirubinemia was a
negative predictor of survival. Therefore, tolvaptan therapy may
improve the long-term outcomes of patients with cirrhosis through
its potential therapeutic effect on refractory ascites.
Glossary
Abbreviations
Abbreviations:
|
eGFR
|
estimated glomerular filtration
rate
|
|
HCC
|
hepatocellular carcinoma
|
|
HCV
|
hepatitis C virus
|
|
MELD
|
Model for End-Stage Liver Disease
|
References
|
1
|
Dahl E, Gluud LL, Kimer N and Krag A:
Meta-analysis: The safety and efficacy of vaptans (tolvaptan,
satavaptan and lixivaptan) in cirrhosis with ascites or
hyponatraemia. Aliment Pharmacol Ther. 36:619–626. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kawaratani H, Fukui H and Yoshiji H:
Treatment for cirrhotic ascites. Hepatol Res. Jul 1–2016.(Epub
ahead of print).
|
|
3
|
Kurosaki M and Izumi N: Tolvaptan for the
Treatment of Refractory Ascites. Intern Med. 55:2909–2910. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sakaida I, Kawazoe S, Kajimura K, Saito T,
Okuse C, Takaguchi K, Okada M and Okita K; ASCITES-DOUBLEBLIND
Study Group, : Tolvaptan for improvement of hepatic edema: A phase
3, multicenter, randomized, double-blind, placebo-controlled trial.
Hepatol Res. 44:73–82. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sakaida I, Nakajima K, Okita K, Hori M,
Izumi T, Sakurai M, Shibasaki Y, Tachikawa S, Tsubouchi H, Oka H,
et al: Can serum albumin level affect the pharmacological action of
tolvaptan in patients with liver cirrhosis? A post hoc analysis of
previous clinical trials in Japan. J Gastroenterol. 50:1047–1053.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Londoño MC, Cárdenas A, Guevara M, Quintó
L, de Las Heras D, Navasa M, Rimola A, Garcia-Valdecasas JC, Arroyo
V and Ginès P: MELD score and serum sodium in the prediction of
survival of patients with cirrhosis awaiting liver transplantation.
Gut. 56:1283–1290. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Iwamoto T, Maeda M, Hisanaga T, Saeki I,
Fujisawa K, Matsumoto T, Hidaka I, Ishikawa T, Takami T and Sakaida
I: Predictors of the Effect of Tolvaptan on the Prognosis of
Cirrhosis. Intern Med. 55:2911–2916. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kogiso T, Yamamoto K, Kobayashi M,
Ikarashi Y, Kodama K, Taniai M, Torii N, Hashimoto E and Tokushige
K: Response to tolvaptan and its effect on prognosis in cirrhotic
patients with ascites. Hepatol Res. 47:835–844. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Akiyama S, Ikeda K, Sezaki H, Fukushima T,
Sorin Y, Kawamura Y, Saitoh S, Hosaka T, Akuta N and Kobayashi M:
Therapeutic effects of short- and intermediate-term tolvaptan
administration for refractory ascites in patients with advanced
liver cirrhosis. Hepatol Res. 45:1062–1070. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ohki T, Sato K, Yamada T, Yamagami M, Ito
D, Kawanishi K, Kojima K, Seki M, Toda N and Tagawa K: Efficacy of
tolvaptan in patients with refractory ascites in a clinical
setting. World J Hepatol. 7:1685–1693. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Komiyama Y, Kurosaki M, Nakanishi H,
Takahashi Y, Itakura J, Yasui Y, Tamaki N, Takada H, Higuchi M,
Gotou T, et al: Prediction of diuretic response to tolvaptan by a
simple, readily available spot urine Na/K ratio. PLoS One.
12:e01746492017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamada T, Ohki T, Hayata Y, Karasawa Y,
Kawamura S, Ito D, Kojima K, Seki M, Toda N and Tagawa K: Potential
Effectiveness of Tolvaptan to Improve Ascites Unresponsive to
Standard Diuretics and Overall Survival in Patients with
Decompensated Liver Cirrhosis. Clin Drug Investig. 36:829–835.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Umemura T, Shibata S, Sekiguchi T,
Kitabatake H, Nozawa Y, Okuhara S, Kimura T, Morita S, Komatsu M,
Matsumoto A and Tanaka E: Serum sodium concentration is associated
with increased risk of mortality in patients with compensated liver
cirrhosis. Hepatol Res. 45:739–744. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Angeli P, Wong F, Watson H and Ginès P:
CAPPS Investigators: Hyponatremia in cirrhosis: Results of a
patient population survey. Hepatology. 44:1535–1542. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kamath PS, Wiesner RH, Malinchoc M,
Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER and Kim
WR: A model to predict survival in patients with end-stage liver
disease. Hepatology. 33:464–470. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Imamura T, Kinugawa K, Shiga T, Kato N,
Muraoka H, Minatsuki S, Inaba T, Maki H, Hatano M, Yao A, et al:
Novel criteria of urine osmolality effectively predict response to
tolvaptan in decompensated heart failure patients-association
between non-responders and chronic kidney disease. Circ J.
77:397–404. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tan HK, James PD, Sniderman KW and Wong F:
Long-term clinical outcome of patients with cirrhosis and
refractory ascites treated with transjugular intrahepatic
portosystemic shunt insertion. J Gastroenterol Hepatol. 30:389–395.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsusaki K, Ohta K, Yoshizawa A and Gyoda
Y; Japanese CART Study Group, : Novel cell-free and concentrated
ascites reinfusion therapy (KM-CART) for refractory ascites
associated with cancerous peritonitis: Its effect and future
perspectives. Int J Clin Oncol. 16:395–400. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kario K: Key Points of the Japanese
Society of Hypertension Guidelines for the Management of
Hypertension in 2014. Pulse Basel. 3:35–47. 2015. View Article : Google Scholar : PubMed/NCBI
|