Introduction
The incidence of the hypercoagulable state in occult
or overt malignancy patients has been observed since the first
observation in 1865 by Trousseau. Patients with cancer are at a
higher risk of developing venous thromboembolism (VTE), as
confirmed in numerous studies. The reason for developing VTE is due
to pathology multifactorials, such as the toxic effect on vascular
endothelium, and upregulation of platelet and monocyte activity
(1,2).
Thus far, the mechanisms according to which cancer cells contribute
to the hypercoagulable state are complex and not completely
understood. In the hypercoagulable state, tumor cells are packaged
by a polymerid of hemaleucin and platelets so that they escape from
immunological surveillance (3,4). This
state directly facilitates the production of thrombin and numerous
signal conduction mechanisms are activated to enhance the
production of new tumor vessels and to promote metastasis.
As the use of anticoagulants may be associated with
an unacceptably high risk of bleeding complications, investigations
have focused on discovering a marker to identify patients at the
highest risk for VTE and poor prognosis who would benefit from
careful prophylaxis (5).
Coagulation-related markers, including thrombin-antithrombin,
fibrinogen (FIB), D-dimer, tissue factor (TF), platelet count,
activated partial thromboplastin time (APTT) and prothrombin time
(PT), have been assayed by investigators to evaluate the state of
the haemostatic and procoagulant systems. Alteration of these
parameters in malignancy patients have been found in certain
studies, and specific alterations have been assumed to be
associated with malignancy-induced hypercoagulable state (6,7).
Several researchers have reported that chemotherapy
is able to induce alterations in markers of coagulation in breast
cancer patients (8). However, few
have regarded the change of haemostasis markers in specific
regimens commonly used in breast cancer patients. The
cyclophosphamide, epirubicin and fluorouracil (CEF) regimen as an
adjuvant therapy for breast cancer has widespread implementation in
China. The toxic effects, such as granulocytopenia, nausea and
vomiting, have been widely investigated and have already satisfied
the therapeutic effect. Recently, certain studies and clinical
activities have begun to focus on the measurement of coagulation
markers and anticoagulant treatment (9,10). The
proper control of the hypercoagulabale state may be a novel
breakthrough for an improved therapeutic effect and lower risk. The
present study aimed to investigate the effect of the
chemotherapy-induced change in haemostasis biomarkers of the CEF
regimen and to assess the risk of deep vein thrombosis and other
short- and long-term complications. According to the results and
previous studies, the addition of anticoagulant treatment will be
discussed to improve the therapeutic effect for chemotherapy.
Patients and methods
Patients
A total of 80 female patients [median age, 50 years
(range, 34–72 years)] commencing chemotherapy for breast cancer in
the Department of Oncology Surgery, First Affiliated Hospital of
Xi'an Jiaotong University (Shaanxi, China) and 80 female controls
[median age, 52 years (range, 32–76 years)] with no history of
cancer were recruited who met the following criteria: Female,
Karnofsky performance score >80, no history of hematopoietic
system disease, and laboratory examination confirmed normal heart,
liver and kidney function. Exclusion criteria were heart failure as
defined by the New York Heart Association (11), hemodynamic instability, hepatic
dysfunction or renal dysfunction. The study was approved by the
Ethics Committee of The First Affiliated Hospital of Xi'an Jiaotong
University. All the patients received CEF regimen chemotherapy.
Patients with operable breast cancer received cyclophosphamide at
600 mg/m2, epirubicin at 80 mg/m2 and
fluorouracil at 500 mg/m2 every 21 days for four
cycles.
Of all the patients, 18 patients exhibited state I
breast cancer, 22 had state IIa, 35 had state IIb and five
exhibited state IIIa (Table I).
Infiltrating ductal carcinoma was observed in 61 patients,
infiltrating lobular carcinoma in 16 patients, colloid carcinoma in
two patients and erebriform carcinoma in one patient (Table II).
 | Table I.Carcinoma states in breast cancer
patients receiving chemotherapy. |
Table I.
Carcinoma states in breast cancer
patients receiving chemotherapy.
| Carcinoma states | No. of patients |
|---|
| State |
|
| I | 18 |
| IIa | 22 |
| IIb | 35 |
| IIIa | 5 |
 | Table II.Pathological type in breast cancer
patients receiving chemotherapy. |
Table II.
Pathological type in breast cancer
patients receiving chemotherapy.
| Pathological
type | No. of patients |
|---|
| Infiltrating ductal
carcinoma | 61 |
| Infiltrating lobular
carcinoma | 16 |
| Colloid
carcinoma | 2 |
| Erebriform
carcinoma | 1 |
Blood sampling and methods
Markers of haemostasis, such as FIB, D-dimer, PT and
APTT, were measured before chemotherapy and the state of
haemostatic and procoagulant systems following commencement of
chemotherapy in all the patients were evaluated at 24 h on days 4,
7 and 21. Venous blood punctuation sampling was performed at the
antecubital fossa. Within 2 h after being collected into tubes, all
the specimens containing anticoagulants were separated as heparin.
Serum samples were allowed to clot at room temperature. All the
samples were centrifuged for 20 min at 41°C and 2,500 × g and the
plasma or serum was removed from the cells. Serum and plasma
samples were subsequently divided into 0.3 ml aliquots.
All the patients were pathologically diagnosed with
breast cancer and were administered in The First Affiliated
Hospital of Xi'an Jiaotong University. In total, 62 received
modified radical mastectomy or breast-conserving surgery on the
basis of the tumor size, position, preoperational biopsy results
and imaging examination. Colony-stimulating factor and other
supportive treatments were administered to ensure the tolerance of
patients in the whole treatment. When any presymptom of a fatal
event was identified during chemotherapy, the treatment was stopped
immediately. A prospective cohort study was undertaken based on the
above condition. All the patients provided written informed
consent. The study was approved by the Conduct of Human Ethics
Committee of Xi'an Jiaotong University.
Statistical analysis
Data on PT, APTT, FIB and D-dimer were assayed by
standard laboratory methods with a Sysmex CA-7000 (Sysmex
Corporation, Kobe, Japan) automated blood coagulation analyzer with
the appropriate reagents and standards. Laboratory analyses were
performed in a blinded fashion. APTT and PT data were reported as
mean (confidence interval) and D-dimer and FIB data were recorded
and reported by geometric means (confidence interval). The analysis
of the values in patients prior and subsequent to chemotherapy was
performed by repeated measure analysis of variance; the analysis of
values between patients and controls was conducted by one-way
analysis of variance. P<0.05 was considered to indicate a
statistically significant difference.
Results
Changes in the haemostasis markers
during systemic chemotherapy
In total, 71 of the 80 patients completed the
therapy. Six patients did not complete the treatment due to
myelosuppression, including thrombocytopenia and penineutroa. A
total of three patients withdrew due to non-hematological toxic
responses, such as strong dizziness, nausea, vomiting and declined
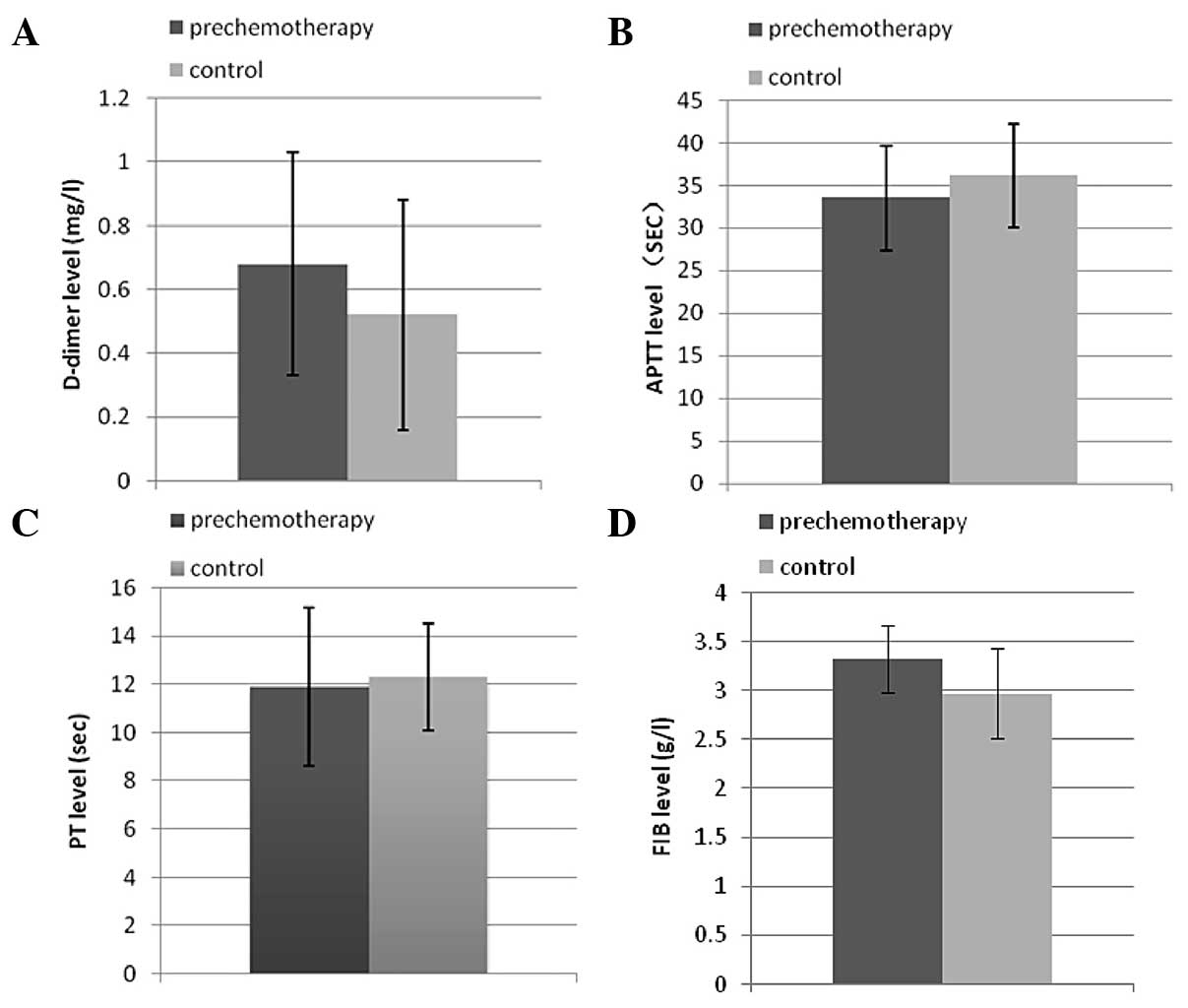
appetite. The value of D-dimer was significantly different between
prechemotherapy and control patients (P<0.05), while APTT, PT
and FIB were not altered in breast cancer patients compared to the
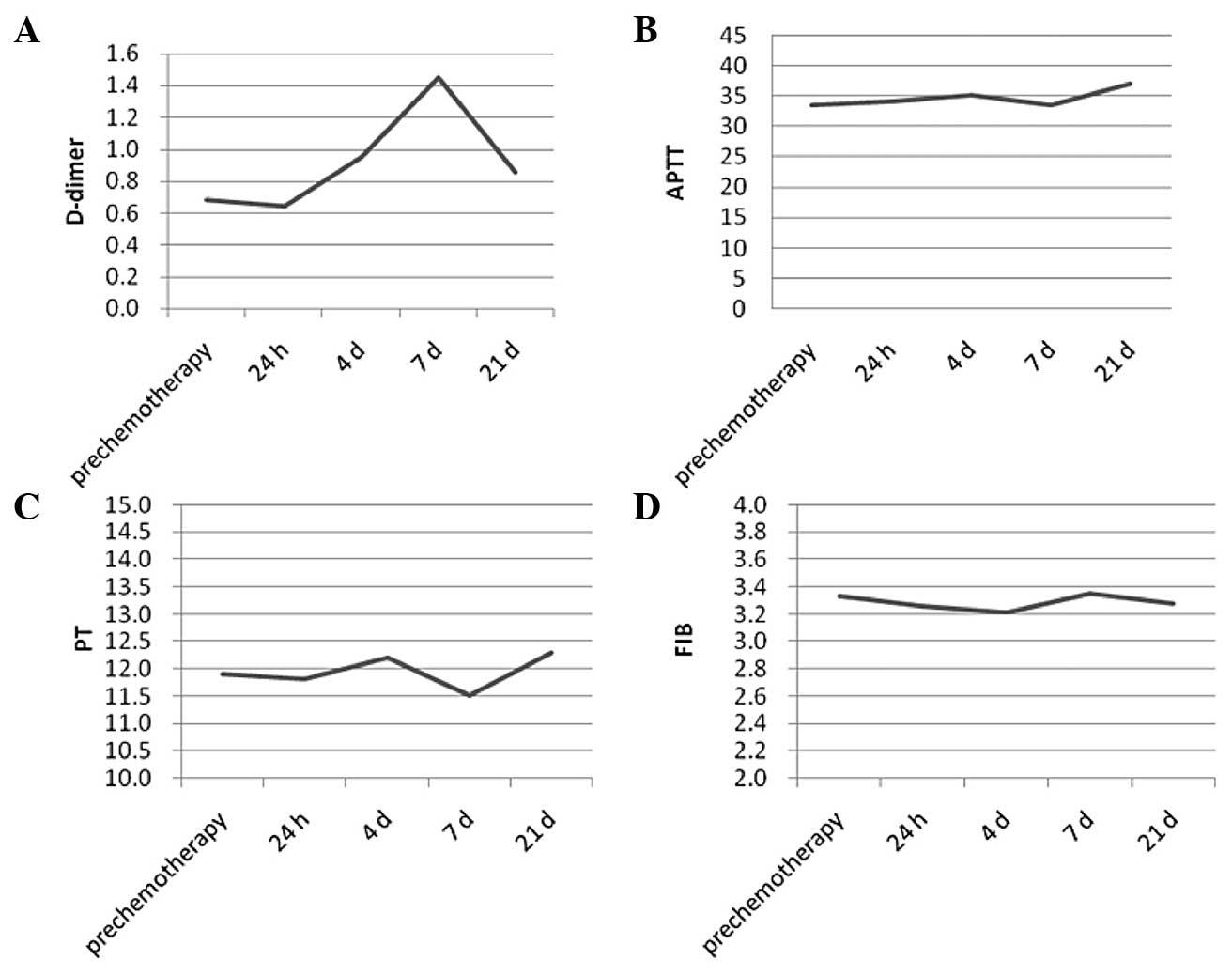
controls prior to chemotherapy (P>0.05) (Fig. 1). The value of coagulation parameters
in response to chemotherapy demonstrated a different trend; PT was
not significantly different among days 1, 4, 7 and 21
(repeated-measures analysis). FIB showed a similar trend to PT.
APTT on day 1 was prolonged but was not significantly different in
comparison to before the chemotherapy. APTT showed an increase
within 4 days after the commencement of chemotherapy and returned
to the level of prechemotherapy on day 7, but it remained under
normal limits and maintained at this level until day 21 (P>0.05)
(Fig. 2).
The plasma D-dimer level was above the reference
value (1.0 mg/l) in 20 out of the 71 patients with breast cancer
prior to chemotherapy (28.2%). There was a significant difference
between the prechemotherapy group and controls (P<0.05).
Although statistical significance was found in the analysis, 53 out
of the 71 values were postoperative, and were not able to exclude
the effect of surgery. At 24 h, no significant difference was
identified when comparing to the D-dimer level prior to
chemotherapy and in patients commencing chemotherapy. A marked
increase was observed within 4 days after the commencement of
chemotherapy and this was more pronounced on day 7 (P<0.001).
Although the increase in D-dimer was maintained until day 21, the
geometric means on day 21 was declining in comparison to those on
days 4 and 7 (Table II).
Discussion
Malignancy is closely associated with the
hypercoagulable state. Idiopathic or scandium VTE occurs with the
prevalence of ~10% in malignancy patients as a paraneoplastic
phenomenon (6). Necroscopy shows that
50% of patients with malignancy have thrombogenesis in their body
circulation (7). Certain researchers
have found that the risk of developing cancer one year after
thrombogenesis is 4.4 times that of those without thrombogenesis
(12). Tumor itself induces the
hypercoagulability state, and the net haemostatic disorder is a
characteristic of patients with solid tumors (13).
The aggravation of the hypercoagulability state by
chemotherapy has been observed in numerous studies. Several results
suggest that the pathogenesis of thrombotic complications may be an
important event of the coagulation-fibrinolysis system disorder
during chemotherapy (14). The change
in the haemostatic and procoagulant systems is reflected by certain
TFs and laboratory test values, such as APTT, PT, D-dimer, FIB,
cancer procoagulant and plasma vascular endothelial growth factor,
and the thromboplastin activation test. A previous study showed a
significantly prolonged APTT in low-grade malignant non-Hodgkin's
lymphoma (15). APTT, PT, D-dimer and
FIB are four widely used measurements that evaluate the coagulation
system in China. Therefore, these four measurements were used to
observe and analyze the results in the present study.
In numerous studies, D-dimer was observed to be more
sensitive and significant in breast cancer and other malignant
diseases than other measurements, and it is associated with the
complication and prognosis of cancer (16,17,18).
D-dimer is a degradation product of fibrin and reflects the fibrin
concentration. The development of deep venous thrombosis has been
proved to be associated with D-dimer. Increased D-dimer levels have
been reported to show the potential presence of silent VTE prior to
treatment in ovarian cancer (19).
Furthermore, in the majority of relapse or resistance to
chemotherapy cases, a further increase of plasma concentration of
D-dimer is commonly observed.
The elevated plasma D-dimer values at presentation
are associated with a poor overall survival rate, event-free
survival and underlying cancer (20).
A high preoperative plasma D-dimer level is a marker of advanced
tumor stage and short survival rate following curative resection in
patients with colorectal cancer (21), as the recovery of the haemostatic
balance with effective chemotherapy is associated with the
prognosis for patients with gynecological malignancies (22). According to these studies, the
importance of D-dimer levels is particularly emphasized in the
present study.
For the evaluative role in the curative effect of
chemotherapy, the change of D-dimer levels during chemotherapy has
been focused on by numerous investigators. Studies have shown that
elevated D-dimer plasma levels in patients with lung cancer are
associated with a decreased survival rate and a poor response to
treatment (16). The result of this
study suggests that an imbalance of the coagulation-fibrinolysis
system may be a contributing factor in the pathogenesis of
thrombotic complications during chemotherapy. D-dimer was also used
as a prognosis marker in breast cancer patients (23). Certain results have indicated the
presence of a hypercoagulability state in females with operable
hormone receptor-negative breast cancer. A significantly high
D-dimer level in patients contributed to a poor prognosis, which
may be an encouraging marker for the prognosis of operable hormone
receptor-negative breast cancer females (24).
The chemotherapy-provoked hypercoagulability state
in breast cancer is demonstrated by D-dimer levels in the study of
Rella et al (9).
Cyclophosphamide, methotrexate and fluoreuracil provokes a trend
towards hypercoagulability, which should be considered when
chemotherapy is employed in advanced cancer patients with a high
risk for thrombosis, or in patients with other risk factors. The
present study provided additional clinical data for the field.
The present study showed that
coagulation-fibrinolysis manifested a hypercoagulability state
through D-dimer and APTT during the CEF regiment chemotherapy. The
change of D-dimer was more significant compared to APTT and varied
during the chemotherapy treatment. D-dimer levels were elevated on
day 4 and reached a peak on day 7. The levels reduced on day 21 but
remained higher than that in the prechemotherapy and controls.
According to the results and other previous studies, day 7 may be
of the highest risk for thrombosis. The significant elevation of
D-dimer in patients during chemotherapy may have a poorer
prognosis.
Certain studies hypothesized that the D-dimer value
could be used in predicting the outcome of cancer. Data showed that
the preoperative D-dimer plasma level may not be a predictor of
clinical outcome in advanced ovarian cancer patients, while other
studies suggested standardizing assays (25,26).
However, the positive views were dominating and supported in the
present study.
In the present study, the hypothesis was that the
proper control of the hypercoagulability state can reduce the risk
and improve the prognosis of breast cancer patients receiving
chemotherapy. The most sensitive measurement for this could be
D-dimer. Certain treatments have been administrated to the
hypercoagulability state. There have been studies regarding
treatment of the chemotherapy-induced hypercoagulability state
(27,28). Improving the prevention and treatment
of VTE in cancer patients is required. The American Society of
Clinical Oncology and the National Comprehensive Cancer Network has
published the guidelines that encourage improving the appropriate
use of low molecular weight heparin (LMWH) and other agents to
enhance the clinical outcomes in medical cancer patients at risk
for VTE and its complications (27).
Another study has certified the safety of long-term anticoagulation
with LMWH and is effective in reducing the recurrence of VTE in
cancer. The role of thromboprophylaxis in ambulatory cancer
patients receiving chemotherapy is an area of new insight (28). LMWH was confirmed to be a more
effective and safer commonly-used anticoagulant agent (28). However, no prospective clinical
studies have addressed the alternation of D-dimer during
anticoagulant administration chemotherapy. Forthcoming studies
should focus on this topic. Although the clinical trials are
limited, the beneficial effect of anticoagulant treatment on the
survival rate of cancer patients is positively confirmed. Regarding
the safety consideration of the anticoagulant therapy, more
clinical trials on the suitable dose and the duration of treatment
are required in this area. However, for an improved response to
treatment and prognosis, the use of anticoagulant therapy is
recommended in the present study.
In conclusion, during the CEF regiment chemotherapy,
the change of D-dimer was more significant than APTT and was not at
the same level during the chemotherapy. D-dimer levels were
elevated on day 4 and reached a peak on day 7. According to the
results and other previous studies, day 7 may be of the highest
risk for thrombosis. A hypothesis was introduced that the proper
control of the hypercoagulability state can reduce the risk and
improve the prognosis of breast cancer patients receiving
chemotherapy. The most sensitive measurement for this could be
D-dimer. For an improved response to treatment and prognosis, the
use of anticoagulant therapy is recommended. Regarding the safety
consideration of the anticoagulant therapy, more clinical trials on
the suitable dose and the duration of treatment are required in
this area.
References
|
1
|
Zecchina G, Ghio P, Bosio S, Cravino M,
Camaschella C and Scagliotti GV: Reactive thrombocytosis might
contribute to chemotherapy-related thrombophilia in patients with
lung cancer. Clin Lung Cancer. 8:264–267. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Albertsson P, Lennernas B and Norrby K:
Low-dose continuous 5-fluorouracil infusion stimulates
VEGF-A-mediated angiogenesis. Acta Oncol. 48:418–425. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Milanini-Mongiat J, Pouyssegur J and Pages
G: Identification of two Sp1 phosphorylation sites for p42/p44
mitogen-activated protein kinases: their implication in vascular
endothelial growth factor gene transcription. J Biol Chem.
277:20631–20639. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Karpatkin S: Does hypercoagulability
awaken dormant tumor cells in the host? J Thromb Haemost.
2:2103–2106. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sood SL: Cancer-associated thrombosis.
Curr Opin Hematol. 16:378–385. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rak J, Yu JL, Luyendyk J and Mackman N:
Oncogenes, trousseau syndrome, and cancer-related changes in the
coagulome of mice and humans. Cancer Res. 66:10643–10646. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sutherland DE, Weitz IC and Liebman HA:
Thromboembolic complications of cancer: epidemiology, pathogenesis,
diagnosis, and treatment. Am J Hematol. 72:43–52. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Oberhoff C, Winkler UH, Hoffmann O and
Schindler AE: Adjuvant CMF-chemotherapy and haemostasis. Effect of
‘classical’ and ‘modified’ adjuvant CMF-chemotherapy on blood
coagulation fibrinolysis in patients with breast cancer. Eur J
Gynaecol Oncol. 21:147–152. 2000.PubMed/NCBI
|
|
9
|
Rella C, Coviello M, Giotta F, et al: A
prothrombotic state in breast cancer patients treated with adjuvant
chemotherapy. Breast Cancer Res Treat. 40:151–159. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nomura H, Wada H, Mizuno T, et al:
Elevated fibrin-related markers in patients with malignant diseases
suspected of having thrombotic disorders. Clin Appl Thromb Hemost.
16:266–272. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
American Heart Association, . Classes of
heart failure. http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heat-Failure_UCM_306328_Article.jspSeptember
6–2011
|
|
12
|
Baron JA, Gridley G, Weiderpass E, Nyren O
and Linet M: Venous thromboembolism and cancer. Lancet.
351:1077–1080. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Garcia-Avello A, Galindo-Alvarez J,
Martinez-Molina E, Cesar-Perez J and Navarro JL: Coagulative system
activation and fibrinolytic system inhibition activities arise from
tumoral draining vein in colon carcinoma. Thromb Res. 104:421–425.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gabazza EC, Taguchi O, Yamakami T, et al:
Alteration of coagulation and fibrinolysis systems after multidrug
anticancer therapy for lung cancer. Eur J Cancer. 30A:1276–1281.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Siemens HJ, Gerke P, Steinhoff J,
Roth-Isigkeit A, Wagner K and Bruckner S: A prolonged APTT in a
patient with a low grade malignant NHL - a case report.
Haematologica. 87:ELT082002.PubMed/NCBI
|
|
16
|
Tamizifar B, Oghab P and Esfahani MA: The
prediction role of D-dimer in recurrence of venous thromboembolism
1-year after anticoagulation discontinuing following idiopathic
deep vein thrombosis. J Res Med Sci. 19:586–591. 2014.PubMed/NCBI
|
|
17
|
Arpaia G, Carpenedo M, Verga M, et al:
D-dimer before chemotherapy might predict venous thromboembolism.
Blood Coagul Fibrinolysis. 20:170–175. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gadducci A, Marrai R, Baicchi U, et al:
Preoperative D-dimer plasma assay is not a predictor of clinical
outcome for patients with advanced ovarian cancer. Gynecol Oncol.
66:85–88. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Satoh T, Oki A, Uno K, et al: High
incidence of silent venous thromboembolism before treatment in
ovarian cancer. Br J Cancer. 97:1053–1057. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lippi G, Franchini M, Biasiutti C,
Dellagiacoma G, Salvagno GL and Guidi GC: Increased D-dimer value
and occult cancer in the absence of detectable thrombosis.
Haematologica. 92:e53–e55. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Oya M, Akiyama Y, Yanagida T, Akao S and
Ishikawa H: Plasma D-dimer level in patients with colorectal
cancer: its role as a tumor marker. Surg Today. 28:373–378. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sawaguchi K, Yabushita H, Higuchi K, et
al: Effect of remission induction chemotherapy on blood
coagulability in patients with gynecological malignancies. Nippon
Gan Chiryo Gakkai Shi. 24:798–808. 1989.(In Japanese). PubMed/NCBI
|
|
23
|
Yigit E, Gonullu G, Yucel I, Turgut M,
Erdem D and Cakar B: Relation between hemostatic parameters and
prognostic/predictive factors in breast cancer. Eur J Intern Med.
19:602–607. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Batschauer AP, Figueiredo CP, Bueno EC, et
al: D-dimer as a possible prognostic marker of operable hormone
receptor-negative breast cancer. Ann Oncol. 21:1267–1272. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lyman GH: Thromboprophylaxis with
low-molecular-weight heparin in medical patients with cancer.
Cancer. 115:5637–5650. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Di Nisio M, Klerk CP, Meijers JC and
Büller HR: The prognostic value of the D-dimer test in cancer
patients treated with and without low-molecular-weight heparin. J
Thromb Haemost. 3:1531–1533. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sousou T and Khorana AA: New insights into
cancer-associated thrombosis. Arterioscler Thromb Vasc Biol.
29:316–320. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gerotziafas GT, Papageorgiou C, Hatmi M,
Samama MM and Elalamy I: Clinical studies with anticoagulants to
improve survival in cancer patients. Pathophysiol Haemost Thromb.
36:204–211. 2008. View Article : Google Scholar : PubMed/NCBI
|