Introduction
Mature cystic teratoma is a common neoplasm
accounting for 10–20% of all ovarian tumors, and most of ovarian
mature cystic teratomas occur in women of reproductive age
(1). Although mature cystic teratoma
is benign, malignant transformation occurs in ~1–2% of all cases,
often in postmenopausal women with large tumors (2). The lack of characteristic symptoms and
specific imaging findings may lead to preoperative misdiagnosis.
Although preoperative diagnosis of mature cystic teratoma of the
ovary is usually achieved with the use of sonography, computed
tomography (CT) and magnetic resonance imaging (MRI), due to the
detection of teeth, bones and cartilage (3), malignant transformation of mature
cystic teratoma is usually detected incidentally postoperatively
based on detailed pathological examination (4). The optimal treatment for malignant
transformation of mature cystic teratoma is uncertain due to the
rarity of the disease (5).
The most common malignant tumor in mature cystic
teratomas is squamous cell carcinoma, whereas papillary thyroid
carcinoma arising from mature cystic teratoma is extremely rare
(6), with only 11 such cases
documented in the English literature to date (5,7–16). In the majority of the cases,
malignant transformation is diagnosed on postoperative pathological
examination. Only 5 cases of papillary thyroid carcinoma arising
from mature cystic teratoma have been reported in younger patients
who wished to preserve their fertility (5,7–10), and the optimal clinical management
strategy is not always clear due to our limited experience with
such cases.
We herein report a rare case of live birth following
two laparoscopic surgeries for papillary thyroid carcinoma arising
from mature ovarian cystic teratoma. The patient was of
reproductive age and the effects of surgical options on fertility
were fully discussed when considering treatment.
Case report
A 30-year-old female patient, gravida 1 para 1, who
had her first transvaginal delivery 1 month earlier, was referred
to the Department of Obstetrics and Gynecology (Hashimoto Municipal
Hospital, Wakayama, Japan) in April 2011 for a routine
gynecological examination. Transvaginal ultrasound examination
revealed bilateral cystic ovarian tumors, sized 2.7 cm on the right
and 3.2 cm on the left side, which contained high-echogenicity
regions. The tumor size grew to 4.2 cm on the right and 6.1 cm on
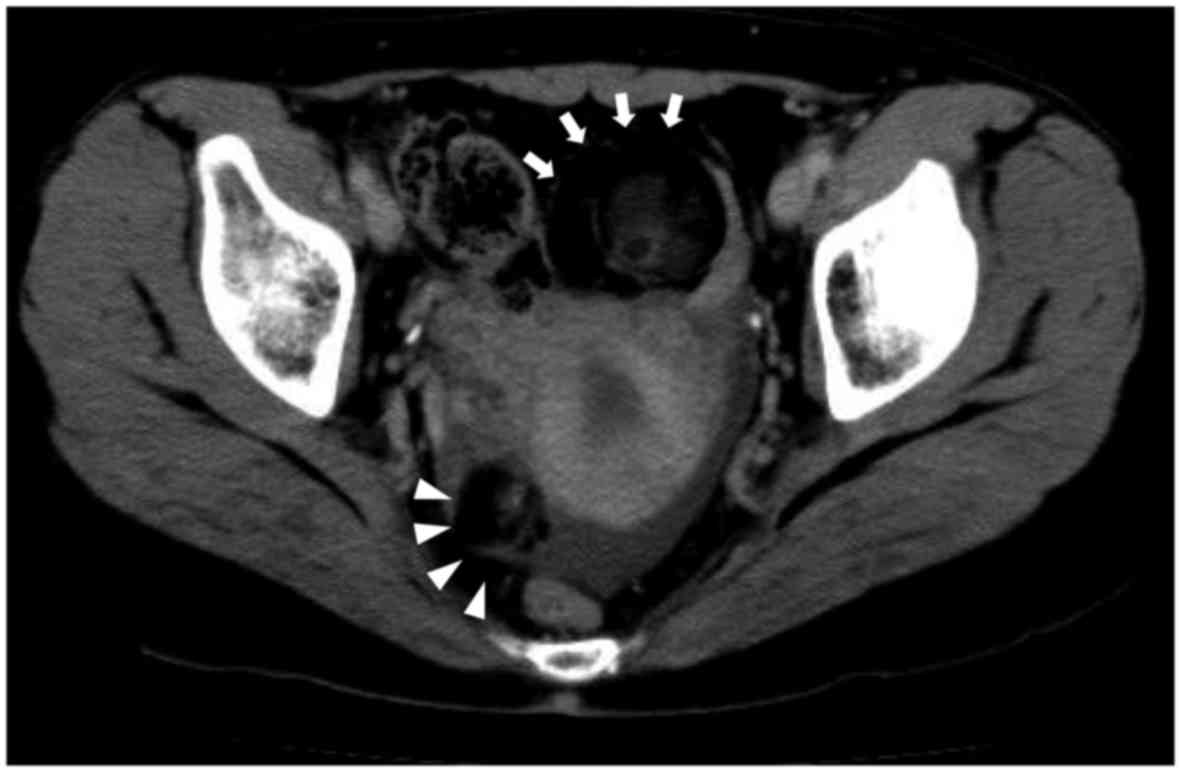
the left side over the next 3 months. A CT scan revealed bilateral
ovarian tumors with a partial solid component and calcification,
without pelvic lymph node enlargement (Fig. 1). MRI could not be performed, as the
patient had a cardiac pacemaker. Based on the imaging findings, the
suspected diagnosis was bilateral ovarian teratoma. The results of
the laboratory tests revealed normal levels of carbohydrate antigen
(CA) 125 and carcinoembryonic antigen, and an elevated CA19-9 level
to 70.0 U/ml (normal level ~37.0 U/ml). The serum biochemical
examination and coagulation profile were within normal limits. The
serum level of thyroid-stimulating hormone was also within normal
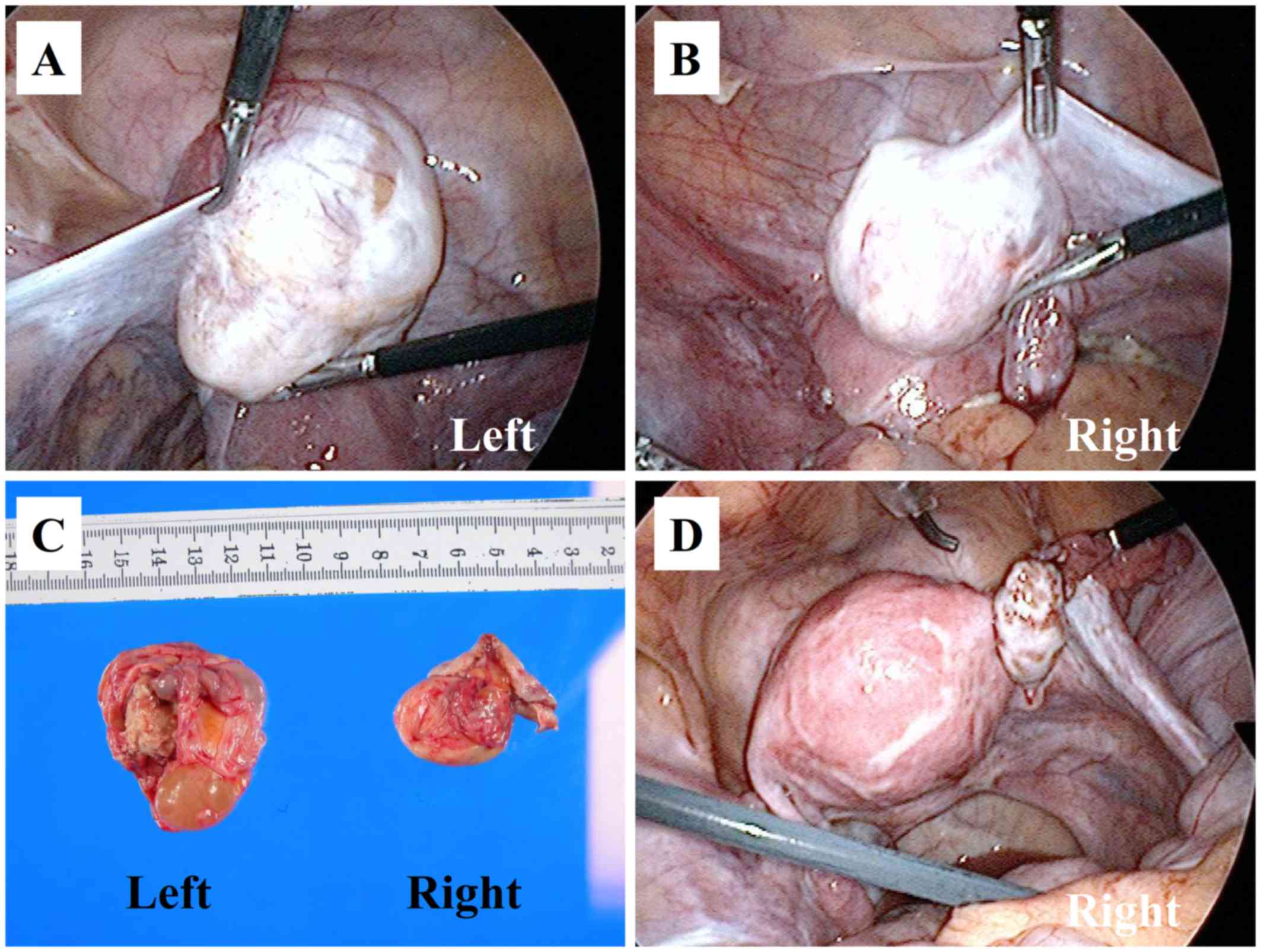
limits. Laparoscopic bilateral cystectomy was performed. An
intraoperative examination revealed bilateral ovarian cystic
tumors, which were mobile and had a smooth surface, both of which
were enucleated; there were no adhesions or invasion of other
organs (Fig. 2A and B). The tumors
were placed in a plastic bag and ruptured, and the contents of the
bag were aspirated and removed through the umbilical trocar site.
No free fluid was detected in the peritoneal cavity. No frozen
sections were prepared for pathological examination.
Macroscopically, the bilateral cystic ovarian tumors
exhibited the typical structure of dermoid cysts containing hair
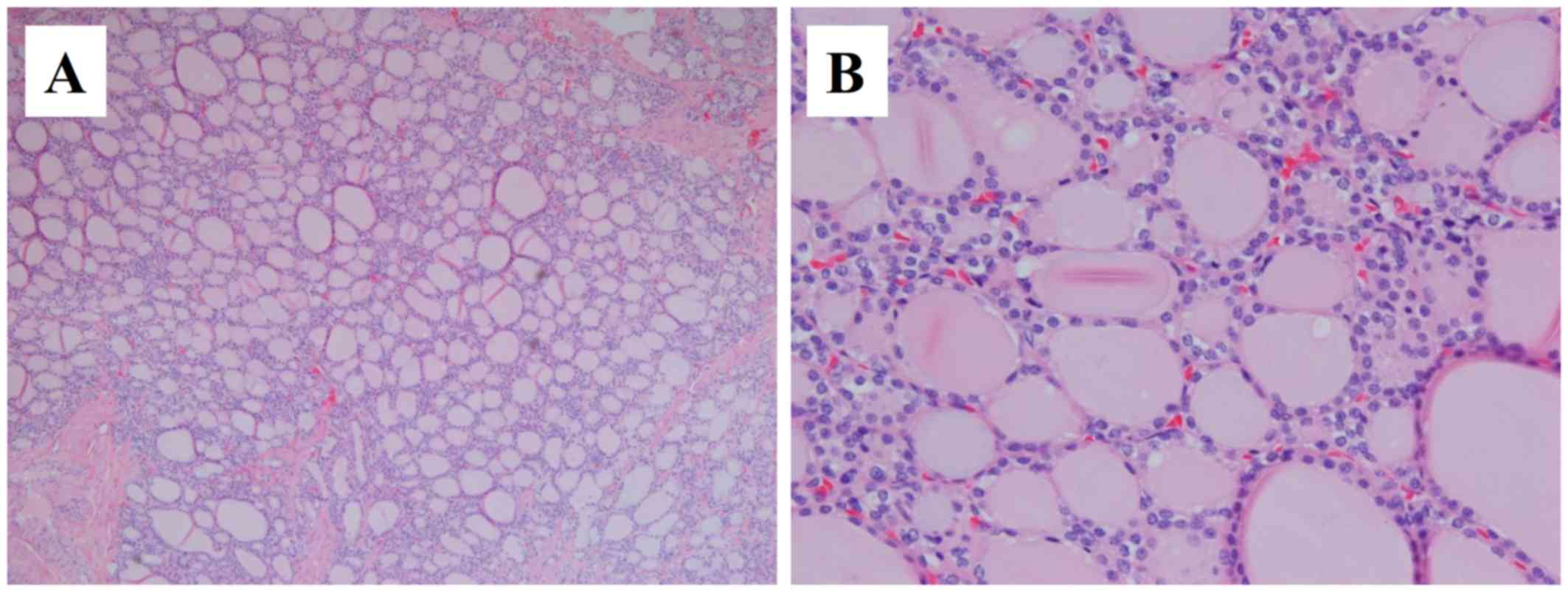
and fat (Fig. 2C). Microscopically,
the left tumor was a mature cystic teratoma containing hair
follicles, adipose, bone, cartilaginous and brain tissue, whereas
the right tumor was a mature cystic teratoma with a thyroid gland
component displaying papillary structure (Fig. 3). The tumor cells had oval or round
overlapping nuclei with a ground glass appearance.
Immunohistochemical examination revealed positive staining of the
tumor cells for cytokeratin (CK) 19, and Hector Battifora
mesothelial epitope-1 (HBME-1). The diagnosis of papillary thyroid
carcinoma arising from ovarian mature cystic teratoma was confirmed
based on the pathological findings.
In order to exclude distant metastasis, positron
emission tomography (PET)-CT was performed. PET-CT revealed normal
thyroid, lung, liver, pancreas, spleen, kidneys and retroperitoneal
space. No enlarged lymph nodes were identified in the
intra-abdominal and retroperitoneal space. The surgical options
were fully discussed with the patient, in order to decide whether
to perform right unilateral salpingo-oophorectomy or complete
surgery for ovarian cancer (total abdominal hysterectomy, bilateral
salpingo-oophorectomy, omentectomy, pelvic lymphadenectomy and
para-aortic lymphadenectomy), and she opted for unilateral
salpingo-oophorectomy to preserve her fertility. One month after
the first laparoscopic surgery, laparoscopic right unilateral
salpingo-oophorectomy was performed. No free fluid was detected in
the peritoneal cavity, and the peritoneal lavage cytology was
negative. The right ovary was normal in size, without adhesions or
obvious invasion of other organ (Fig.
2D). On histopathological examination, the right ovary was free
from cancer infiltration. Adjuvant chemotherapy was not
administered and the patient gave birth following natural
conception without any problems 2 years following surgery. There
was no evidence of local recurrence or systemic disease in
September 2017.
Discussion
The majority of mature cystic teratomas are composed
of well-differentiated derivatives of the three germ layers, namely
the ectoderm, the mesoderm and the endoderm, while ectodermal
elements usually predominate, and it has been reported that ~15% of
the tumors contain thyroid tissue (6). The complications of mature cystic
teratoma include torsion (16%), malignant degeneration (2%),
rupture (1–2%) and infection (1%) (17), whereas uncomplicated teratomas are
found incidentally on routine gynecological examination in
asymptomatic patients. The main concern with treating mature cystic
teratoma is the possibility of malignant transformation, which can
only be correctly diagnosed postoperatively based on detailed
pathological examination. Particularly in women of reproductive
age, malignant transformation of mature cystic teratoma is even
more uncommon. The survival outcome of patients with malignant
transformation of mature cystic teratoma depends on the stage at
diagnosis.
Papillary thyroid cancer arising from mature cystic
teratoma is a rare occurrence, with an estimated incidence of
0.1–0.3% (18), with 11 cases in
total reported in the literature to date (5,7–16), among which only 5 were patients of
reproductive age (5,7–10)
according to a search of the English literature on PubMed and
MEDLINE. In patients of reproductive age, including the case in the
present study (5,7–10), the
mean age and tumor size were 29.2 years (range, 19–39 years) and
8.62 cm (range, 4.2–15 cm), respectively. In two cases the patients
were asymptomatic and the tumors were discovered incidentally
(5,10). To the best of our knowledge, the
tumor in the present case was the smallest among all reported
asymptomatic cases of reproductive age, indicating that the size of
the tumor and the presence of symptoms are not indicative of the
diagnosis.
The most appropriate clinical management strategy
for papillary thyroid carcinoma arising from mature cystic teratoma
is not always clear, as our experience with such cases is limited.
Laparoscopic surgery is usually selected when the gynecologist
suspects mature cystic teratoma, as it is a minimally invasive
surgery, and it may also be possible to treat patients wishing to
preserve their fertility by fertility-sparing surgery including
unilateral salpingo-oophorectomy or cystectomy without adjuvant
chemotherapy. According to previous reports on the condition,
abdominal cystectomy was performed in 2 cases (7,8),
laparoscopic salpingo-oophorectomy in 1 case (5), laparoscopic salpingo-oophorectomy
followed by total abdominal hysterectomy with contralateral
salpingo-oophorectomy in 1 case (9),
and abdominal cystectomy followed by abdominal adnexectomy in 1
case (10). The long-term prognosis
of papillary thyroid carcinoma arising from mature cystic teratoma
is unclear, with a limited number of reports on follow-up time
(6–33 months). The prognosis appears to be favorable, as no
metastasis or recurrence have been reported. In the present case,
laparoscopic bilateral cystectomy was first performed, followed by
unilateral salpingo-oophorectomy. The options were fully discussed
with the patient and their family and written informed consent was
obtained. The patient was advised that she would be able to become
pregnant following treatment, provided there was no evidence of
disease for 6 years. To improve the treatment of papillary thyroid
carcinoma arising from mature cystic teratoma in the future,
further data regarding its natural history, diagnosis and treatment
outcome are needed.
In summary, we herein present a rare case of
papillary thyroid carcinoma arising from a mature cystic ovarian
teratoma, in which two laparoscopic surgeries was performed and the
patient was able to successfully carry a pregnancy to term after
treatment. Gynecologists should be aware of the possibility of such
rare cases, and the available surgical interventions should be
fully discussed with patients who wish to preserve their fertility.
Laparoscopic fertility-sparing surgery may be a viable treatment
option when encountering such rare cases.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets obtained and/or analyzed during the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
NI and YD diagnosed, investigated and managed the
patient. NI wrote the initial draft of the report. NI, YD and YH
acquired the data in the surgical field. TN, TY and NO acquired the
data in the diagnostic imaging and pathological examination. KI and
KF supervised the study and critically reviewed the manuscript. All
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Written informed consent for surgery was obtained
from the patient.
Patient consent for publication
Written informed consent for publication of the case
details and associated images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lai PF, Hsieh SC, Chien JC, Fang CL, Chan
WP and Yu C: Malignant transformation of an ovarian mature cystic
teratoma: Computed tomography findings. Arch Gynecol Obstet.
271:355–357. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wen KC, Hu WM, Twu NF, Chen P and Wang PH:
Poor prognosis of intraoperative rupture of mature cystic teratoma
with malignant transformation. Taiwan J Obstet Gynecol. 45:253–256.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kido A, Togashi K, Konishi I, Kataoka ML,
Koyama T, Ueda H, Fujii S and Konishi J: Dermoid cysts of the ovary
with malignant transformation: MR appearance. AJR Am J Roentgenol.
172:445–449. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mori Y, Nishii H, Takabe K, Shinozaki H,
Matsumoto N, Suzuki K, Tanabe H, Watanabe A, Ochiai K and Tanaka T:
Preoperative diagnosis of malignant transformation arising from
mature cystic teratoma of the ovary. Gynecol Oncol. 90:338–341.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lataifeh I, Abdel-Hadi M, Morcos B,
Sughayer M and Barahmeh S: Papillary thyroid carcinoma arising from
mature cystic teratoma of the ovary. J Obstet Gynaecol. 30:884–886.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Peterson WF: Malignant degeneration of
benign cystic teratomas of the overy; a collective review of the
literature. Obstet Gynecol Surv. 12:793–830. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dane C, Ekmez M, Karaca A, Ak A and Dane
B: Follicular variant of papillary thyroid carcinoma arising from a
dermoid cyst: A rare malignancy in young women and review of the
literature. Taiwan J Obstet Gynecol. 51:421–425. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Soto Moreno A, Venegas EM, Rodriguez JR,
Sánchez F, Robles MJ, Martinez MA, Gonzalez D, Navarro E and
Astorga R: Thyroid carcinoma on an ovarian teratoma: A case report
and review of the literature. Gynecol Endocrinol. 16:207–211. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee JM, Kim JW, Song JY, Lee JK, Lee NW,
Kim SH and Lee KW: Adenocarcinoma arising in mature cystic
teratoma: A case report. J Gynecol Oncol. 19:199–201. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cymbaluk-Ploska A, Chudecka-Głaz A, Chosia
M, Ashuryk O and Menkiszak J: Conservative treatment of a young
patient with thyroid carcinoma in adult ovarian teratoma-case
report. Gynecol Endocrinol. 30:187–191. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chadha S and Schaberg A: Malignant
transformation in benign cystic teratomas: Dermoids of the ovary.
Eur J Obstet Gynecol Reprod Biol. 29:329–338. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Doldi N, Taccagni GL, Bassan M, Frigerio
L, Mangili G, Jansen AM and Ferrari A: Hashimoto's disease in a
papillary carcinoma of the thyroid originating in a teratoma of the
ovary (malignant struma ovarii). Gynecol Endocrinol. 12:41–42.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bal A, Mohan H, Singh SB and Sehgal A:
Malignant transformation in mature cystic teratoma of the ovary:
Report of five cases and review of the literature. Arch Gynecol
Obstet. 275:179–182. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ryder M, Nikiforov YE and Fagin JA:
Follicular variant papillary thyroid carcinoma arising within an
ovarian teratoma. Thyroid. 17:179–180. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Quadri AM, Ganesan R, Hock YL, Karim SN
and Hirschowitz L: Malignant transformation in mature cystic
teratoma of the ovary: Three cases mimicking primary ovarian
epithelial tumors. Int J Surg Pathol. 19:718–723. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tanaka H, Sakakura Y, Kobayashi T, Yoshida
K, Asakura T and Taniguchi H: A case of thyroid-type papillary
carcinoma derived from ovarian mature cystic teratoma, resected by
laparoscopic surgery. Asian J Endosc Surg. 4:86–89. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lipson SA and Hricak H: MR imaging of the
female pelvis. Radiol Clin North Am. 34:1157–1182. 1996.PubMed/NCBI
|
|
18
|
Rim SY, Kim SM and Choi HS: Malignant
transformation of ovarian mature cystic teratoma. Int J Gynecol
Cancer. 16:140–144. 2006. View Article : Google Scholar : PubMed/NCBI
|