Introduction
Cervical cancer is the fourth most common malignancy
in women worldwide. It was estimated that there were 604,000 new
diagnostic cases and 342,000 deaths in 2020. Approximately 90% of
new incidences and deaths worldwide in 2020 occurred in low- and
middle-income countries. In high-income countries, the mortality
rate is low because of the human papillomavirus (HPV) vaccine,
routine screening, and adequate treatment (1). However, the prognosis of patients
with advanced or recurrent cervical cancer remains
unacceptable.
The standard treatment for cervical cancer is
surgery or radiotherapy, and is selected according to the clinical
stage and treatment strategy. It is likely to differ between
Western and Asian countries. In Japan, 53.3, 24.3, 11.5, and 10.9%
of patients had stage I, II, III, and IV cervical cancer,
respectively. A total of 61.5% of patients received surgery alone
or surgery followed by concurrent chemoradiotherapy (CCRT)
(2). In Europe and the United
States, radiotherapy is a common treatment for patients with the
International Federation of Gynecology and Obstetrics (FIGO) stage
II cervical cancer, whereas in Japan, approximately half of these
patients undergo surgery or neoadjuvant chemotherapy followed by
surgery (3). Patients undergoing
surgery are required to receive adjuvant therapy based on recurrent
risk classification. Recurrent risk factors include pelvic lymph
node metastasis, parametrial invasion, stromal invasion,
lymph-vascular space invasion (LVSI), and tumor size. Recurrent
risk classification (high, intermediate, and low risk) is decided
based on these risk factors. The definition of intermediate risk is
based on the Sedlis criteria: 1) greater than one-third stromal
invasion, 2) capillary lymphatic space involvement, or 3) cervical
tumor diameters ≥4 cm (4). Other
studies have demonstrated the necessity of considering tumor
histology (5,6) and close or positive surgical margins
(7,8). Therefore, the definition of
intermediate risk has not been strictly described. Generally,
low-risk patients do not require adjuvant therapy. However,
high-risk patients are recommended postoperative treatment.
Furthermore, the most recent National Comprehensive Cancer Network
guidelines advocate adjuvant therapy for intermediate-risk patients
(9). However, the treatment for
intermediate-risk cases is not standardized and varies across
institutions. The question of whether all cases with intermediate
risk should receive adjuvant therapy is controversial and remains
an open question. Therefore, there is a need to explore markers for
adjuvant therapy in intermediate-risk groups, and this was the
focus of this study.
The prognosis for FIGO stage I-II cervical cancer is
relatively favorable; however, some patients experience early
relapse. Moreover, recurrent cases have limited treatment options
and are often considered to be incurable. Therefore, if future
recurrence in these stages can be predicted, options for
postoperative adjuvant therapy can be increased.
Recently, our group revealed that the protein,
Amphoterin-induced gene and open reading frame 2/adhesion molecule
with IgG domain 2 (AMIGO2) is a prognostic factor for colorectal
and gastric cancer in clinical samples (10,11).
However, the association between AMIGO2 levels and cervical cancer
remains unclear. In this study, using immunohistochemical analysis
of the cervical tumor samples and clinical evaluation of the
patients, we aimed to determine whether AMIGO2 can predict
recurrence and whether AMIGO2 is associated with prognostic factors
in cervical cancer. Currently, postoperative adjuvant treatment is
standard for the high-risk group, but postoperative treatment for
the intermediate-risk group varies from institution to institution,
and there is no appropriate marker for adjuvant treatment. The
results of this study clearly showed that AMIGO2 expression is a
marker for postoperative adjuvant therapy in the intermediate-risk
group. Therefore, we believe that our study would aid in
determining appropriate treatment strategies for intermediate-risk
group.
Materials and methods
Patient samples
The present study was approved by the institutional
review board of Tottori University Hospital (IRB number: 21A152).
Patients who underwent radical hysterectomy or radical
trachelectomy for preoperative diagnosis of early cervical cancer
(clinical T1N0M0 or T2N0M0) at Tottori University between 2005 and
2016 were included (12). The
clinical samples used in this study were not the patients who were
finally diagnosed with early-stage cervical cancer, but those who
underwent radical hysterectomy or radical trachelectomy for
preoperative early-stage cervical cancer. We chose this target
population because of the possibility of investigating the effect
of lymph node metastasis by AMIGO2 expression in the same T
classification. All patients provided opt-out consent in accordance
with institutional guidelines. Immunohistochemical analysis was
performed on 101 samples. Recurrent risk was classified as low,
intermediate, or high, based on the postoperative pathological
diagnosis. High risk is associated with positive pelvic lymph node
metastasis, and parametrial invasion. Intermediate risk is
determined by ‘greater than one-third stromal invasion,’ ‘capillary
lymphatic space involvement,’ or ‘cervical tumor diameters ≥4 cm,’
according to the Sedlis criteria (4). Low risk involves conditions that are
excluded from high and intermediate risk. All high-risk patients,
except one who refused treatment, received standard clinical
treatment (adjuvant CCRT; pelvic radiotherapy as a total of 45-50
Gy/5-6 weeks and chemotherapy with cisplatin, 40 mg/m2/week)
(9) Low- and intermediate-risk
patients (none of whom received adjuvant CCRT) were carefully
monitored. Clinical characteristics, recurrence, form of
recurrence, disease-free survival (DFS), and overall survival (OS)
were retrospectively investigated based on clinical records. Form
of recurrence was divided into distant metastasis and local
recurrence including vaginal vault or pelvic relapse.
Immunohistochemistry
The cervical cancer samples were fixed in formalin
and embedded in paraffin. Serial sections were cut at 4 µm,
deparaffinized in xylene for 15 min, and rehydrated through a
graded alcohol series for 15 min. The sections were autoclaved for
10 min in 10 mM citrate buffer (pH 6.0) in a microwave and were
incubated in 3% hydrogen peroxidase (Nichirei Biosciences Inc.,
426042, Tokyo, Japan) to block endogenous peroxidases for 20 min to
prevent non-specific antigen binding. The slides were subsequently
incubated with rat anti-AMIGO2 antibody (rTNK1Bo12a, 1:1,000
dilution) or mouse anti-Podoplanin antibody (D2-40, Nichirei
Biosciences Inc., 426042, Tokyo, Japan) overnight at 4˚C (13). The sections were then incubated
with goat polyclonal anti-rat IgG horseradish peroxidase-conjugated
antibody (Abcam, ab98425, Cambridge, United Kingdom, 1:300
dilution) or biotin-labeled rabbit polyclonal anti-mouse IgG
antibody, horseradish peroxidase-conjugated streptavidin (Nichirei
Biosciences Inc.) at 20˚C for 20 min, respectively. Secondary
staining was performed using a peroxidase substrate kit (Vector
Laboratories, SK-4105, Burlingame, CA, USA), and the sections were
counterstained with hematoxylin. A positive rate of >70 and ≤70%
was defined as high expression of AMIGO2 (AMIGO2-High group) and
low expression of AMIGO2 (AMIGO2-Low group), respectively, using a
microscope (Leica, DM500, Wetzlar, Germany).
Statistical analysis
Patient survival distribution was determined using
the Kaplan-Meier method and log-rank test. Categorical variables
were analyzed using Fisher's exact test. Univariate and
multivariate analyses were performed using the Cox proportional
hazard model. Statistical significance was set at P<0.05.
Statistical analyses were performed using EZR software version
1.54, 2020(14).
Results
Immunohistochemical detection of
AMIGO2 expression and clinicopathological factors in cervical
cancer
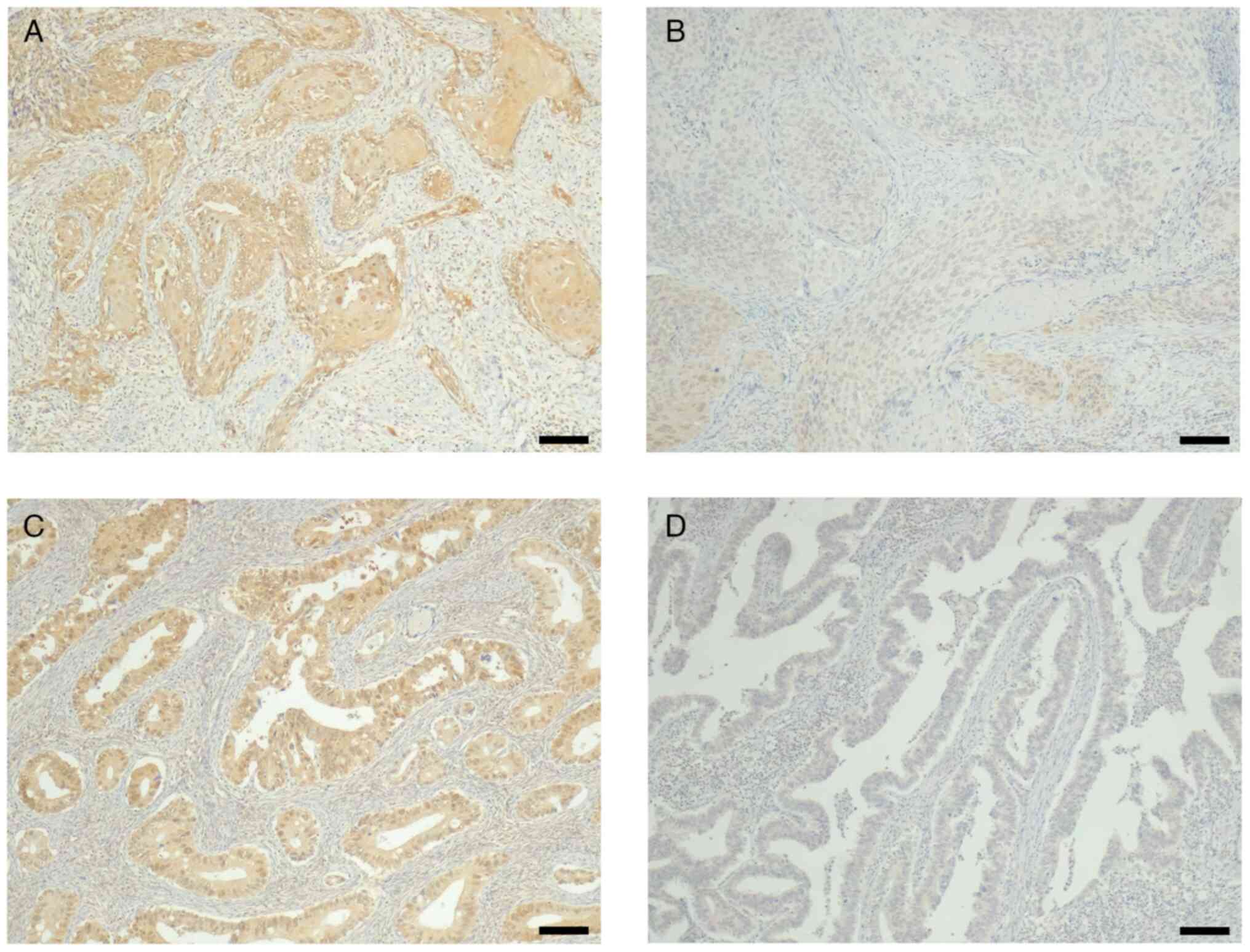
To confirm the expression of AMIGO2 in cervical
cancer, we performed immunohistochemical analysis using
AMIGO2-specific antibodies. Cervical carcinomas were histologically
classified into squamous cell carcinoma (SCC) and adenocarcinoma
including adenosquamous carcinoma (non-SCC), and analyzed for
AMIGO2 expression (Fig. 1);
however, no association was found between the histological type and
AMIGO2 expression (Table I). In
all histological types, AMIGO2 expression was higher in cancer
cells and lower in the surrounding stroma; AMIGO2 protein was
localized in both the nucleus and cytoplasm (Fig. 1A and C). Based on a cutoff of 70%
AMIGO2-positive cell fraction in cancer cells, cases were
classified as AMIGO2-High (Fig. 1A
and C) and AMIGO2-Low groups
(Fig. 1B and D), regardless of the histological
type.
 | Table IAMIGO2 expression and
clinicopathological factors in 101 cervical cancer patients. |
Table I
AMIGO2 expression and
clinicopathological factors in 101 cervical cancer patients.
| Parameter | AMIGO2-High
(n=40) | AMIGO2-Low
(n=61) | P-value |
|---|
| Age, years (range,
22-71 years) | | | 0.79 |
|
<60 | 32 | 51 | |
|
≥60 | 8 | 10 | |
| Histology | | | 0.2 |
|
SCC | 30 | 37 | |
|
Non-SCC | 10 | 24 | |
| Tumor size | | | 0.011 |
|
<4
cm | 32 | 59 | |
|
≥4 cm | 8 | 2 | |
| Lymph node
metastasis | | | <0.001 |
|
+ | 15 | 5 | |
|
- | 25 | 56 | |
| Parametrial
invasion | | | 0.0024 |
|
+ | 8 | 1 | |
|
- | 32 | 60 | |
| Stromal invasion | | | 0.023 |
|
+ | 22 | 19 | |
|
- | 18 | 42 | |
| LVSI | | | 0.0032 |
|
+ | 23 | 16 | |
|
- | 17 | 45 | |
Of the 101 cervical cancer samples evaluated, 39.6%
(40/101) were in the AMIGO2-High group and 60.4% (61/101) in the
AMIGO2-Low group. The correlation between clinicopathological
variables and AMIGO2 expression in tumor tissues is shown in
Table I. Approximately one-fifth
of patients (20/101; 19.8%) upstaged to FIGO stage IIIC1p because
of lymph node metastasis. The AMIGO2-High group had a higher
frequency of bulky tumors (≥4 cm, 8/40; 20.0%) than the AMIGO2-Low
group (2/61; 3.3%). Furthermore, lymph node metastases (15/40;
37.5% vs. 5/61; 8.2%), parametrial invasion (8/40; 20.0% vs. 1/61;
1.6%), stromal invasion (22/40; 55.0% vs. 19/61; 31.1%), and
LVSI-positive cases (23/40; 57.5% vs. 16/61; 26.2%) were all
significantly higher in the AMIGO2-High group (P<0.05). In
contrast, age and histological type did not differ between the two
groups.
To analyze for AMIGO2 expression in tumor cells
invading lymphatic vessels, immunohistochemistry was performed
using only two cases that were evaluable. Although the expression
intensity of AMIGO2 was different in the two cases, the expression
was confirmed in almost all invasive tumor cells (Fig. S1). Despite the high incidence, due
to the small number of cases available for analysis, it was not
possible to conclude whether invasive cancer cells have a
significantly higher incidence.
AMIGO2 expression as a predictor of
cervical cancer recurrence
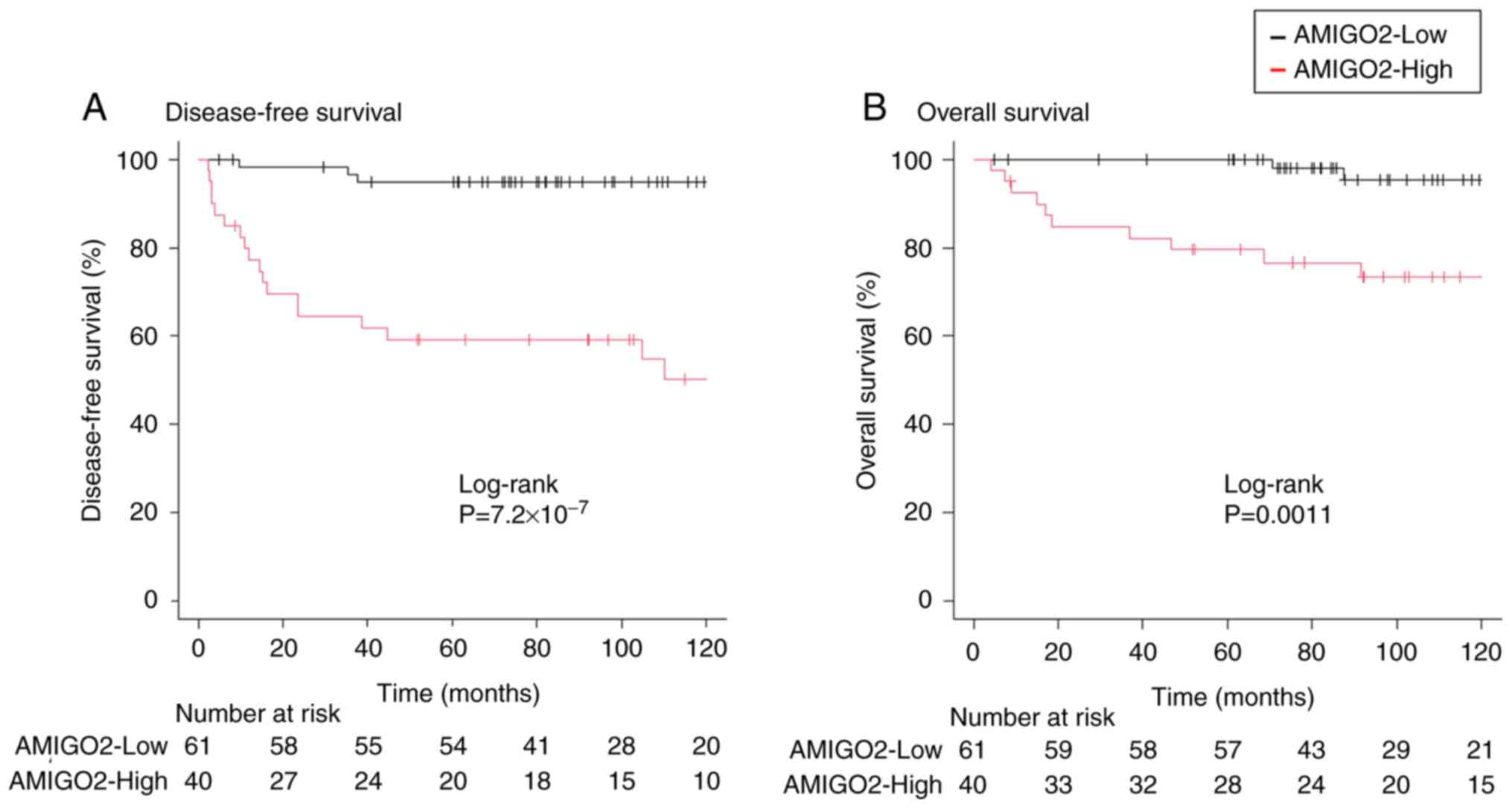
Kaplan-Meier survival analysis and log-rank tests
were performed to examine the relationship between AMIGO2
expression and prognosis in cervical cancer. Patients in the
AMIGO2-High group had shorter 5 year-DFS than those in the
AMIGO2-Low group [59% {95% confidence interval (CI) 42-73%} vs. 95%
(95% CI 85-98%) (P<0.001)] (Fig.
2A). Furthermore, at the 5-year OS, patients in the AMIGO2-High
group had clearly worse survival than those in the AMIGO2-Low group
[80% (95% CI 63-89%) vs. 100% {95% CI not available (NA)-NA}
(P=0.0011)] (Fig. 2B).
Next, we investigated (including AMIGO2 expression)
the independent risk factors for DFS and OS, respectively: in
univariate analysis of DFS, lymph node metastasis, tumor size,
parametrial invasion, stromal invasion, LVSI and AMIGO2 were
considered prognostic factors. Furthermore, in multivariate
analysis, AMIGO2 expression was the only independent prognostic
factor for DFS (Table II). When
the analysis was limited to the intermediate-risk group, AMIGO2
expression was also the only independent prognostic factor for DFS
(Table SI). In the univariate
analysis of OS, the same variable was an independent prognostic
factor for DFS. On the other hand, multivariate analysis revealed
no statistically independent prognostic factors for OS, including
AMIGO2 (Table III). It was
suggested that this is probably due in part to the small number of
cases. However, since the P value was 0.08, the lowest value
compared to the other factors, it was considered that there was a
trend, although not statistically significant.
 | Table IIMultivariate analysis for disease-free
survival. |
Table II
Multivariate analysis for disease-free
survival.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age | | | | | | |
|
≥60 years
vs. <60 years | 0.5 | 0.12-2.1 | 0.35 | | | |
| Histology | | | | | | |
|
Non-SCC vs.
SCC | 0.76 | 0.3-1.9 | 0.57 | | | |
| Tumor size | | | | | | |
|
≥4 cm vs.
<4 cm | 3.97 | 1.5-11 | 0.0074 | 1.7 | 0.58-5.1 | 0.33 |
| Lymph node
metastasisa | | | | | | |
|
Positive vs.
negative | 3.4 | 1.4-8.1 | 0.0055 | 0.79 | 0.28-2.3 | 0.66 |
| Parametrial
invasion | | | | | | |
|
Positive vs.
negative | 4.4 | 1.6-12 | 0.004 | 1.56 | 0.54-4.5 | 0.41 |
| Stromal
invasion | | | | | | |
|
Positive vs.
negative | 3.1 | 1.2-7.6 | 0.02 | 0.98 | 0.31-3.2 | 0.97 |
| LVSI | | | | | | |
|
Positive vs.
negative | 4.83 | 1.9-13 | 0.001 | 3.2 | 0.85-12 | 0.085 |
| AMIGO2
expression | | | | | | |
|
High vs.
low | 11.5 | 3.4-39 | <0.001 | 8.3 | 2.3-30 | 0.0012 |
 | Table IIIMultivariate analysis for overall
survival. |
Table III
Multivariate analysis for overall
survival.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age | | | | | | |
|
≥60 years
vs. <60 years | 0.48 | 0.06-3.7 | 0.48 | | | |
| Histology | | | | | | |
|
Non-SCC vs.
SCC | 0.89 | 0.27-3.0 | 0.85 | | | |
| Tumor size | | | | | | |
|
≥4 cm vs.
<4 cm | 8.9 | 2.8-28 | <0.001 | 3.6 | 0.98-13 | 0.053 |
| Lymph node
metastasisa | | | | | | |
|
Positive vs.
negative | 6.2 | 1.9-20 | 0.0018 | 2.3 | 0.42-12 | 0.34 |
| Parametrial
invasion | | | | | | |
|
Positive vs.
negative | 4.4 | 1.2-16 | 0.03 | 1.5 | 0.39-6.1 | 0.54 |
| Stromal
invasion | | | | | | |
|
Positive vs.
negative | 4.7 | 1.3-17 | 0.02 | 2.8 | 0.44-18 | 0.27 |
| LVSI | | | | | | |
|
Positive vs.
negative | 3.6 | 1.1-12 | 0.04 | 0.5 | 0.06-4.1 | 0.52 |
| AMIGO2
expression | | | | | | |
|
High vs.
low | 8.3 | 1.8-38 | 0.006 | 4.3 | 0.84-22 | 0.08 |
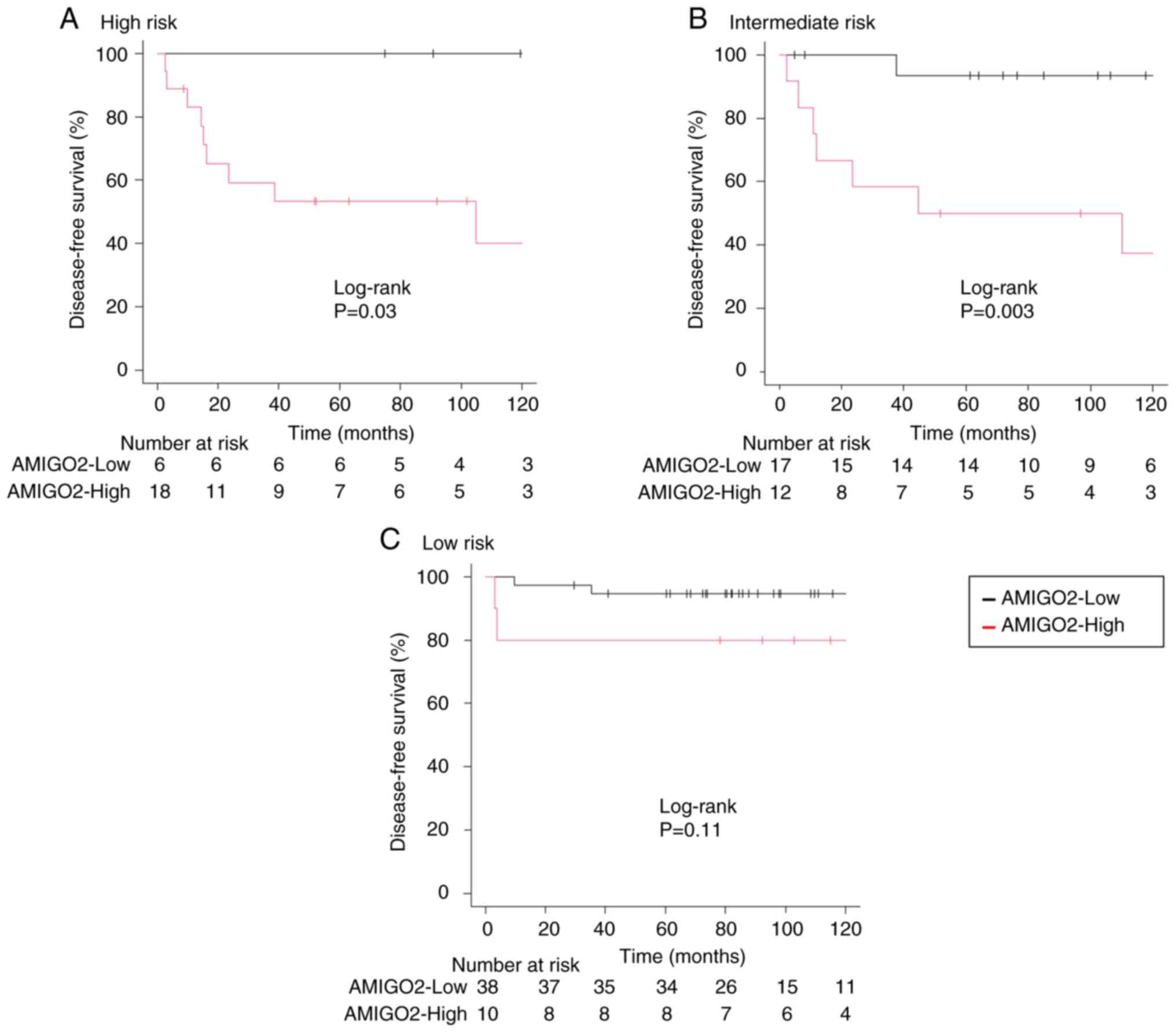
Patients with cervical cancer have been
postoperatively classified into three risk categories (high,
intermediate, and low risk) based on the risk factor assessment
(pelvic lymph node metastasis, parametric invasion, stromal
invasion, LVSI, and tumor size). Therefore, Kaplan-Meier curves for
5-year DFS were generated for each risk category. As shown in
Fig. 3, in the high- and
intermediate-risk groups, AMIGO2-High patients had a significantly
shorter 5-year DFS than AMIGO2-Low patients (Fig. 3A and B). In contrast, there was no association
between AMIGO2 expression and prognosis in the low-risk group
(Fig. 3C). In contrast, AMIGO2
expression did not affect OS according to risk classification (data
not shown). Finally, when we examined the correlation between
AMIGO2 expression and the site of recurrence by classifying distant
metastasis and local recurrence, we found no difference in the
recurrence patterns based on AMIGO2 expression (Table SII).
Discussion
The present study verified the relationship between
AMIGO2 expression and clinicopathological factors using clinical
specimens of cervical cancer in the present study. Our data clearly
demonstrated that high AMIGO2 expression is a prognostic factor for
cervical cancer. Notably, AMIGO2 expression can be used as an
indicator to predict the recurrence of intermediate-risk cervical
cancer, suggesting that AMIGO2 as a predictive marker could
contribute to the treatment strategy for the patient. To our
knowledge, this is the first report showing AMIGO2 expression as a
molecular marker that can predict recurrence risk in cervical
cancer.
Our previous studies i) identified AMIGO2 as a
driver gene for liver metastases using a mouse cell line (15), ii) extrapolated its function in
mouse cells to that in human cancer cell lines (16), and iii) indicated that high AMIGO2
expression acted as a driver for liver metastases in human gastric
and colorectal cancers and resulted in poor prognosis (10,11).
Additionally, Liu et al (17) reported that AMIGO2 is related to
peritoneal dissemination in an in vivo model using human
ovarian cancer cells. Thus, enhanced AMIGO2 expression may play a
crucial role in cancer prognosis by activating metastasis in
various cancers. The present study showed that higher expression of
AMIGO2 is associated with the recurrence of human cervical cancer,
suggesting that this molecule is involved in the progression of
cervical cancer as well as the above-mentioned cancer types.
In this study, high AMIGO2 expression in cervical
cancer was associated with poor prognosis in DFS and OS, with a
particularly strong association with DFS. A prognostic analysis of
early-stage cervical cancer cases similar to the present study
reported that 5-year OS and DFS were 83 and 74%, respectively
(18). Compared to these results,
the 5-year OS and DFS in this study were worse for AMIGO-High and
better for AMIGO-Low. Thus, the results of the present study
strongly suggest that AMIGO2 expression is a very useful prognostic
marker in human early-stage cervical cancer. The multivariate
analysis data strongly suggested that among all the factors, AMIGO2
expression was the only independent predictor of cervical cancer
prognosis, strongly suggesting its usefulness as a predictive
marker of recurrence. Interestingly, the present study indicated
that the AMIGO2-High group had a considerably shorter 5-year DFS
than the AMIGO2-Low intermediate-risk group. The criteria for
postoperative adjuvant therapy for these intermediate-risk patients
have not been defined yet. Moreover, the Japanese Society of
Gynecologic Oncology and the Korean Gynecologic Oncology Group
reported that 37.3 and 26% of intermediate-risk patients did not
receive adjuvant therapy, respectively (5,19).
Previously, our institution also had not administered adjuvant
therapy for intermediate-risk cases. This was because our previous
research demonstrated that deep stromal invasion can be excluded
from the list of criteria for adjuvant radiotherapy (20). However, the present study revealed
that the intermediate-risk group with high AMIGO2 expression
exhibits high metastasis (Fig. 3).
Thus, the intermediate-risk group with high expression of AMIGO2
should undergo adequate adjuvant therapy as well as the high-risk
group.
Lymph node involvement was newly incorporated into
staging and defined as stage IIIC in FIGO 2018. This is because
positive lymph node metastasis is strongly associated with poor
outcomes and low survival. Previous work from our lab on the
prognosis of patients with cervical cancer, also showed that those
with lymph node metastases had poor prognosis (21). In contrast, the present study
showed that lymph node metastasis was not an independent prognostic
factor. This was due to the small number of lymph node-positive
cases (n=20), which was considered a limitation of the study. In
this study, instead of comparing the presence or absence of lymph
node metastasis between the same stages, different stages were used
for comparison. The reason for this is due to the patient
background of the population diagnosed with early-stage cervical
cancer (clinical T1N0M0 or T2N0M0) at preoperative diagnosis. The
incidence of lymph node metastasis was higher in the AMIGO2-High
group than in the AMIGO2-Low group, and there was a clear
difference in the proportion of FIGO stage IIIC1 patients,
suggesting that AMIGO2 expression may affect lymph node metastasis
and may be associated with the prognosis of cervical cancer.
Furthermore, it would be possible to predict the prognosis by
examining AMIGO2 expression preoperatively.
In conclusion, this study revealed that AMIGO2
expression is an independent prognostic factor in cervical cancer
recurrence, suggesting that AMIGO2 expression is a marker for
cervical cancer recurrence. In patients who were classified as
intermediate-risk postoperatively, the high AMIGO2-expressing group
was shown to be at higher risk of recurrence, and it was
recommended that these patients be considered for postoperative
treatment as a high-risk group.
Supplementary Material
Immunohistochemical staining for
AMIGO2 expression in cervical cancer cells invading lymphatic
vessels. AMIGO2 expression in cancer cells in D2-40-positive
lymphatic vessels was analyzed using serial sections in two cases.
Scale bar, 100 μm. AMIGO2, amphoterin-induced gene and open
reading frame 2.
Multivariate analysis for disease-free
survival in intermediate-risk group.
No relationship was found between
AMIGO2 expression and recurrence sites.
Acknowledgements
The authors would like to thank Dr Hiroyuki
Satofuka, Professor Yasuhiro Kazuki and Professor Hiroyuki Kugoh
(Chromosome Engineering Research Center, Tottori University) for
their technical support in producing the specific monoclonal
antibody ‘rTNK1Bo12a’ for human AMIGO2.
Funding
Funding: This work was supported in part by a Grant-in-Aid from
the Japanese Ministry of Education, Culture, Sports, Science and
Technology to Futoshi Okada (grant no. 20K07447).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YI, SS, MO and FO established the study design and
analytical concept. YI, MO and DO collected and analyzed clinical
data. YI, RI, HS and MO performed histological analysis. YI and MO
confirm the authenticity of all the raw data. YI, MO, SS, HK, FT
and FO interpreted the data. HK, SS, FO and FT acquired the
funding. YI and SS were major contributors in writing the
manuscript. RI, HS, MO and FO made critical revisions to the
manuscript. All authors have read and approved the manuscript.
Ethics approval and consent to
participate
The present study was approved by the institutional
review board of Tottori University Hospital (IRB no. 21A152). All
patients provided opt-out consent in accordance with institutional
guidelines.
Patient consent for publication
The requirement for patient consent for publication
was waived due to the retrospective nature of the study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Nagase S, Ohta T, Takahashi F, Yamagami W
and Yaegashi N: Board Members of the 2020 Committee on Gynecologic
Oncology of the Japan Society of Obstetrics and Gynecology. Annual
report of the Committee on Gynecologic Oncology, the Japan Society
of Obstetrics and Gynecology: Annual patient report for 2018 and
annual treatment report for 2013. J Obstet Gynaecol Res.
48:541–552. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shigeta S, Shida M, Nagase S, Ikeda M,
Takahashi F, Shibata T, Yamagami W, Katabuchi H, Yaegashi N, Aoki D
and Mikami M: Epidemiological guideline influence on the
therapeutic trend and patient outcome of uterine cervical cancer in
Japan: Japan society of gynecologic oncology guideline evaluation
committee project. Gynecol Oncol. 159:248–255. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sedlis A, Bundy BN, Rotman MZ, Lentz SS,
Muderspach LI and Zaino RJ: A randomized trial of pelvic radiation
therapy versus no further therapy in selected patients with stage
IB carcinoma of the cervix after radical hysterectomy and pelvic
lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol.
73:177–183. 1999.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ryu SY, Kim MH, Nam BH, Lee TS, Song ES,
Park CY, Kim JW, Kim YB, Ryu HS, Park SY, et al: Intermediate-risk
grouping of cervical cancer patients treated with radical
hysterectomy: A Korean Gynecologic Oncology Group study. Br J
Cancer. 110:278–285. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Noh JM, Park W, Kim YS, Kim JY, Kim HJ,
Kim J, Kim JH, Yoon MS, Choi JH, Yoon WS, et al: Comparison of
clinical outcomes of adenocarcinoma and adenosquamous carcinoma in
uterine cervical cancer patients receiving surgical resection
followed by radiotherapy: A multicenter retrospective study (KROG
13-10). Gynecol Oncol. 132:618–623. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Diaz ES, Aoyama C, Baquing MA, Beavis A,
Silva E, Holschneider C and Cass I: Predictors of residual
carcinoma or carcinoma-in-situ at hysterectomy following cervical
conization with positive margins. Gynecol Oncol. 132:76–80.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Estape RE, Angioli R, Madrigal M, Janicek
M, Gomez C, Penalver M and Averette H: Close vaginal margins as a
prognostic factor after radical hysterectomy. Gynecol Oncol.
68:229–232. 1998.PubMed/NCBI View Article : Google Scholar
|
|
9
|
NCCN Clinical Practice Guidelines in
Oncology (NCCN Guidelines): Cervical Cancer. Version 1. National
Comprehensive Cancer Network, 2023.
|
|
10
|
Tanio A, Saito H, Amisaki M, Hara K,
Sugezawa K, Uejima C, Tada Y, Kihara K, Yamamoto M, Nosaka K, et
al: AMIGO2 as a novel indicator of liver metastasis in patients
with colorectal cancer. Oncol Lett. 21(278)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Goto K, Morimoto M, Osaki M, Tanio A,
Izutsu R, Fujiwara Y and Okada F: The impact of AMIGO2 on prognosis
and hepatic metastasis in gastric cancer patients. BMC Cancer.
22(280)2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Olawaiye AB, Baker TP, Washington MK and
Mutch DG: The new (Version 9) American Joint Committee on Cancer
tumor, node, metastasis staging for cervical cancer. CA Cancer J
Clin. 71:287–298. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Goto K, Osaki M, Izutsu R, Tanaka H,
Sasaki R, Tanio A, Satofuka H, Kazuki Y, Yamamoto M, Kugoh H, et
al: Establishment of an antibody specific for AMIGO2 improves
immunohistochemical evaluation of liver metastases and clinical
outcomes in patients with colorectal cancer. Diagn Pathol.
17(16)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kanda Y, Osaki M, Onuma K, Sonoda A,
Kobayashi M, Hamada J, Nicolson GL, Ochiya T and Okada F:
Amigo2-upregulation in tumour cells facilitates their attachment to
liver endothelial cells resulting in liver metastases. Sci Rep.
7(43567)2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Izutsu R, Osaki M, Jehung JP, Seong HK and
Okada F: Liver Metastasis formation is defined by AMIGO2 expression
via adhesion to hepatic endothelial cells in human gastric and
colorectal cancer cells. Pathol Res Pract.
237(154015)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Liu Y, Yang J, Shi Z, Tan X, Jin N,
O'Brien C, Ott C, Grisoli A, Lee E, Volk K, et al: In vivo
selection of highly metastatic human ovarian cancer sublines
reveals role for AMIGO2 in intra-peritoneal metastatic regulation.
Cancer Lett. 503:163–173. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Landoni F, Maneo A, Colombo A, Placa F,
Milani R, Perego P, Favini G, Ferri L and Mangioni C: Randamised
study of radical surgery versus radiotherapy for stage Ib-IIa
cervical cancer. Lancet. 350:535–540. 1997.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Shigeta S, Shimada M, Tsuji K, Nagai T,
Tanase Y, Matsuo K, Kamiura S, Iwata T, Yokota H and Mikami M: Risk
assessment in the patients with uterine cervical cancer harboring
intermediate risk factors after radical hysterectomy: A
multicenter, retrospective analysis by the Japanese Gynecologic
Oncology Group. Int J Clin Oncol. 27:1507–1515. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Shimada M, Kigawa J, Takahashi M, Minagawa
Y, Okada M, Kanamori Y, Itamochi H, Oishi T, Iba T and Terakawa N:
Stromal invasion of the cervix can be excluded from the criteria
for using adjuvant radiotherapy following radical surgery for
patients with cervical cancer. Gynecol Oncol. 93:628–631.
2004.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Osaku D, Komatsu H, Okawa M, Iida Y, Sato
S, Oishi T and Harada T: Re-classification of uterine cervical
cancer cases treated with radical hysterectomy based on the 2018
FIGO staging system. Taiwan J Obstet Gynecol. 60:1054–1058.
2021.PubMed/NCBI View Article : Google Scholar
|