Introduction
Coronavirus disease 2019 (COVID-19), which is caused
by the spread of severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) and mainly transmitted by droplets and aerosols, has
become a global health issue (1). As
a preventive measure, oral procedures are limited to emergency
treatment due to their propensity for aerosol transmission
(2). Fever, cough, shortness of
breath and a sore throat are the most common symptoms of COVID-19,
which are also similar to the predominant symptoms of oral,
pharyngeal and cervical infections, such as peritonsillar abscess
(PA), tonsillitis, acute epiglottitis and deep neck abscess
(1,3,4).
Laboratory findings in patients with these diseases have revealed a
high leukocyte count and C-reactive protein (CRP) level, which are
indicators of bacterial infection (5). By contrast, laboratory findings in
patients with COVID-19 have revealed low leukocyte, neutrophil and
thrombocyte counts (6,7).
The present study describes a conservatively managed
case of PA and COVID-19 co-infection which revealed unconventional
laboratory findings.
Case report
A 41-year-old female patient presented at Bellland
General Hospital with a 3-day history of high fever and a severe
sore throat, followed by dysgeusia and dysosmia. The patient had no
relevant medical history and was not on any medication. Although
the patient denied having a cough or dyspnoea, the symptoms were
indicative of COVID-19. The nasopharyngeal swab specimen was
positive for SARS-CoV-2 (cut off index, 35099.4), as determined
using a quantitative antigen test (chemiluminescent enzyme
immunoassay; HISCL™ SARS-CoV-2 Ag reagent, Sysmex
Corporation). Furthermore, the patient exhibited a slight
difficulty in opening her mouth and speaking. An oral examination
revealed left-side peritonsillar swelling and reddening without
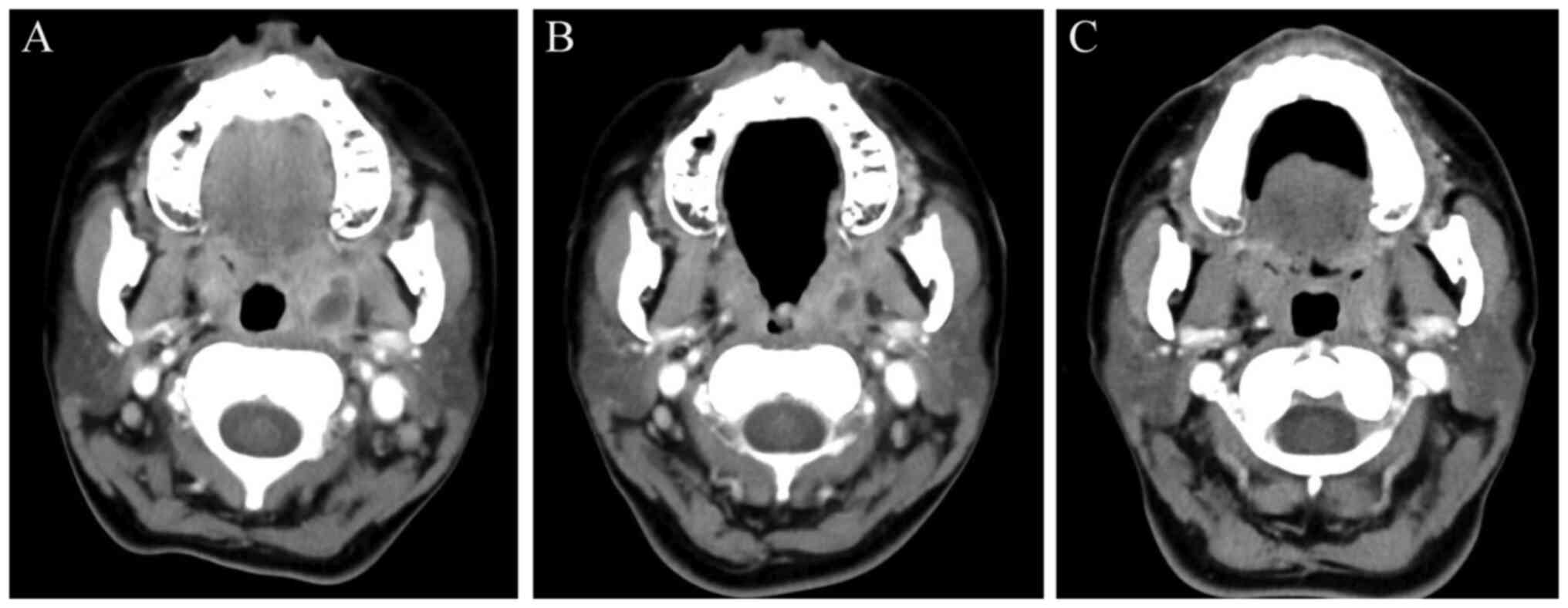
laryngeal oedema. A computed tomography (CT) scan revealed
left-sided PA (Fig. 1A).
Consequently, the patient was diagnosed with PA and concurrent
COVID-19, and was thus admitted to the isolation ward. The
laboratory findings of the patient revealed a normal leukocyte
count of 7,700/µl (reference range, 3,300-8.800/µl) and a normal
procalcitonin level of <0.02 (reference range, <0.02).
However, the CRP level was extraordinarily high at 9.42 (reference
range, <0.14). PA was treated with intravenous ceftriaxone
sodium hydrate (2 g/day) and clindamycin (600 mg/day) for 7 days.
The patient was also conservatively managed for COVID-19, as the
percutaneous oxygen saturation remained high without oxygen support
and the patient did not exhibit any signs of dyspnoea. Transoral
drainage by aspiration and incision was not performed due to the
risk of SARS-CoV-2 aerosolisation. At 2 days after hospitalisation,
the CRP level, leukocyte count and procalcitonin level of the
patient were 3.76, 5,100/µl and <0.02, respectively. The patient
began the oral intake of food and water following an improvement in
the severity of the sore throat. At 3 days after hospitalisation,
the CRP level was 2.17 and the leucocyte count was 4,700/µl. A CT
scan at this time point revealed a reduction in the left-side PA
cavity (Fig. 1B). At 7 days after
hospitalisation, the patient recovered and was discharged.
At the 1-week postoperative follow-up (14 days after
the initial visit to Bellland General Hospital), the patient's
condition was stable without fever or a sore throat. A CT scan at
this time point confirmed the absence of an abscess cavity
(Fig. 1C).
Discussion
COVID-19 is a highly infectious disease, and the
pandemic has changed the style of medical care and oral
examinations. The use of personal protective equipment, including
facial masks, shields, glasses, gloves, caps and gowns is essential
to reduce the risk of aerosol exposure to SARS-CoV-2 (1,2). The
diagnosis of COVID-19 has become increasingly rapid and simple due
to the widespread use of various SARS-CoV-2 tests (8). However, oral, pharyngeal and cervical
infections (e.g., PA, tonsillitis, acute epiglottitis, deep neck
abscess) may be overlooked if a thorough oral and
pharyngo-laryngeal evaluation is avoided due to the high
transmissibility of COVID-19. Akiyama et al (9) reported the necessity of careful
evaluation for life-threatening diseases in cases with fever during
the COVID-19 pandemic era.
PA is the most common deep infection of the head and
neck and is a life-threatening disease. PA is diagnosed by an oral
and pharyngeal examination, as well as through a CT scan and
endoscopic findings (4). Fever and a
sore throat are the predominant symptoms in patients with PA;
however, these symptoms have also been identified in patients with
COVID-19 (1,3). In the case described herein, COVID-19
was suspected due to the characteristic symptoms of the patient.
Moreover, the patient was tested for and diagnosed with COVID-19.
Furthermore, the slight difficulty exhibited by the patient in
opening her mouth and speaking was indicative of airway obstruction
caused by oral, pharyngeal and/or laryngeal oedema. Both the
oropharyngeal examination and CT scan revealed PA; the patient was
finally diagnosed with PA co-existing with COVID-19. Although
transoral drainage of abscesses is effective for patients with PA,
this procedure poses a high risk of COVID-19 transmission (4). The ENT UK guidelines recommend
restricting abscess drainage to severe cases with airway
compromise, sepsis, or those that do not improve with initial
medical therapy (2). The patient in
the present study was managed conservatively. Intravenous
antibiotics were administered without providing transoral drainage
or anti-COVID-19 medication, as dyspnoea and sepsis were not
observed and the COVID-19 symptoms of the patient were not severe.
The patient's condition improved, which was verified using a CT
scan.
Laboratory findings in the patient described herein
indicated that the CRP level was elevated, whereas the leukocyte
count had remained at normal levels since the initial examination.
The leucocyte count and CRP levels have been shown to be positively
associated in patients with PA (10). The unconventional laboratory findings
in the case in the present study may have been induced by the
simultaneous presence of PA and COVID-19, although there is no
clear evidence of an association between these diseases. Moreover,
the procalcitonin levels were normal during treatment.
Procalcitonin levels are elevated by bacterial infection and are a
reliable marker of sepsis, whereas a lack of an increase in
procalcitonin levels is observed in viral infections due to the
inhibition of tumour necrosis factor-α in the immune response
(11). Hu et al (12) reported that procalcitonin played the
role of an indicator, determining the disease severity of patients
infected with SARS-CoV-2. Considering these previous findings, the
level of procalcitonin in the case in the present study suggested
that the patient was moderately affected with PA and COVID-19. The
association between laboratory findings (e.g., leukocyte count, CRP
and procalcitonin levels) and bacterial co-infection in COVID-19
has not yet been established. To the best of our knowledge, this is
the first case report study featuring laboratory findings in a
patient with PA and COVID-19 co-infection. Further studies are thus
required in this area.
The importance of using personal protective
equipment and isolation to prevent exposure to aerosols containing
SARS-CoV-2, as well as the restriction of transoral procedures to
severe cases (e.g., airway obstruction) has been highlighted in the
COVID-19 pandemic era (2). Although
COVID-19 can be easily diagnosed with rapid tests, co-infection
with life-threatening oral, pharyngeal and laryngeal infections may
be underdiagnosed due to insufficient oral examination (9). These diseases should not be overlooked
due to the lack of appropriate evaluation.
In conclusion, the present study described a case of
a patient with PA and COVID-19 co-infection. The conservative
treatment of PA may be effective during the COVID-19 pandemic. A
careful examination is warranted in order to avoid the
underdiagnosis of life-threatening diseases co-existing with
COVID-19. While unconventional laboratory findings may indicate
bacterial co-infections with COVID-19, further studies are
warranted for confirmation.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AT made substantial contributions to the conception
of the study and the acquisition of data, and drafted the
manuscript. SM, NK, TN, TI and TK provided related scientific input
and collected the clinical data. SM, TI and TK critically revised
the manuscript. AT and TN confirm the authenticity of all the raw
data. All authors have accepted responsibility for the entire
content of this manuscript and have approved the submission. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report, including any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wiersinga WJ, Rhodes A, Cheng AC, Peacock
SJ and Prescott HC: Pathophysiology, transmission, diagnosis, and
treatment of coronavirus disease 2019 (COVID-19): A review. JAMA.
324:782–793. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Edwards MJ, James TW and Dalton CL: ENT UK
coronavirus disease 2019 adult tonsillitis and quinsy guidelines:
Translating guidance into practice. J Laryngol Otol. 135:579–583.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tsang HF, Chan LW, Cho WC, Yu AC, Yim AK,
Chan AK, Ng LP, Wong YK, Pei XM, Li MJ and Wong SC: An update on
COVID-19 pandemic: The epidemiology, pathogenesis, prevention and
treatment strategies. Expert Rev Anti Infect Ther. 19:877–888.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Galioto NJ: Peritonsillar abscess. Am Fam
Physician. 95:501–506. 2017.PubMed/NCBI
|
|
5
|
Hu L, Shi Q, Shi M, Liu R and Wang C:
Diagnostic value of PCT and CRP for detecting serious bacterial
infections in patients with fever of unknown origin: A systematic
review and meta-analysis. Appl Immunohistochem Mol Morphol.
25:e61–e69. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Usul E, Şan İ, Bekgöz B and Şahin A: Role
of hematological parameters in COVID-19 patients in the emergency
room. Biomark Med. 14:1207–1215. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei C, Hui DSC, et al: Clinical characteristics
of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hristov DR, Gomez-Marquez J, Wade D and
Hamad-Schifferli K: SARS-CoV-2 and approaches for a testing and
diagnostic strategy. J Mater Chem B. 9:8157–8173. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Akiyama Y, Morioka S, Wakimoto Y,
Kawashima A, Kanda K, Okuhama A, Suzuki T, Miyazato Y, Nomoto H,
Ide S, et al: Non-COVID-19 patients with life-threatening diseases
who visited a fever clinic: A single-center, observational study in
Tokyo, Japan. Intern Med. 59:3131–3133. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Seyhun N, Çalış ZA, Ekici M and Turgut S:
Epidemiology and clinical features of peritonsillar abscess: Is it
related to seasonal variations? Turk Arch Otorhinolaryngol.
56:221–225. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Müller B, Becker KL, Schächinger H,
Rickenbacher PR, Huber PR, Zimmerli W and Ritz R: Calcitonin
precursors are reliable markers of sepsis in a medical intensive
care unit. Crit Care Med. 28:977–983. 2000.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hu R, Han C, Pei S, Yin M and Chen X:
Procalcitonin levels in COVID-19 patients. Int J Antimicrob Agents.
56(106051)2020.PubMed/NCBI View Article : Google Scholar
|