Introduction
Spinal cord injury (SCI) can induce sudden memory
loss, as well as loss of motor function on the distal side
(1). Primary SCI reflects the
direct mechanical impact of trauma on the spine, while secondary
injury involves a complicated series of molecular processes,
including local edema, ionic homeostasis disruption, focal
bleeding, ischemia, inflammation and oxidative stress. Typically,
apoptosis leads to progressive degeneration in cases of SCI
(2,3). Decompression, medications and
prevention of secondary complications are important for post-SCI
functional recovery. Compounds aiding the recovery of neurological
function post-SCI have been used to protect surviving tissues
against degeneration; these substances promote axonal regeneration
and suppress inflammation and glial scarring (4–7).
Fibroblast growth factor 10 (FGF10), also known as
keratinocyte growth factor 2, is a basic protein consisting of
84–246 amino acids. It interacts mainly with embryonic epithelial
cells, stromal cells, fibroblasts and organs including the liver,
lung and intestine. FGF10 plays a role in the signaling of
epithelial mesenchymal cells during embryonic development, promotes
the formation and development of glands, and stimulates the
development of internal organs (8,9). A
neuroprotective effect of FGF10 has been demonstrated, and it can
inhibit inflammation via the PI3K/Akt pathway to protect against
acute brain injury (10). FGF10
promotes peripheral nerve regeneration by eliciting a PI3K/Akt
signaling-mediated antioxidant response (11). Furthermore, FGF10 activates the
FGFR2/PI3K/Akt signaling pathway and suppresses the activity of
microglia/macrophages associated with TLR4/NF-κB-dependent
neuroinflammation, thereby enhancing functional recovery after SCI
(12).
FGFs and their receptors have a wide range of
biological function via regulation of mitosis, survival, migration
and differentiation (13). There
are also evidences for the potential of FGF signaling on the
progression of tumor (14). For
most FGFs, malignant transformation is a potential risk (15). However, it has a wide range of
clinical applications as a drug and exhibits favorable safety
(16). There is little evidence
that FGF10 can promote the malignant transformation of neurological
tissue, and the spinal cord itself is not prone to canceration.
Therefore, it is still considered that FGF10 delivery has huge
potential when it was used in the hyperacute period in SCI.
However, FGF10 should not be administered
systemically. First, as a macromolecular protein, systemic FGF10
may induce enzyme degradation, and it struggles to penetrate the
blood-spinal cord barrier (BSCB). Second, FGF10 may induce mitosis,
which can cause cancers within normal tissues. To overcome these
drawbacks of protein-based medications, an in situ drug
delivery system can be used to deliver therapeutics to the injured
site. Due to its non-toxicity and biodegradability, gelatin is the
preferred protective agent for depot preparations. In a previous
study, locally implanted basic FGF (bFGF) and bone morphogenetic
protein (BMP) were slowly released from a gelatin sponge, thus
facilitating the regeneration of tracheal cartilage (17). Gelatin microspheres (GMSs) are
widely used to deliver various growth factors, including BMP2, bFGF
and vascular endothelial growth factor, as well as plasmids and
stem cells, thereby facilitating the remodeling and regeneration of
tissues (18–20). Compared with administration of free
bFGF, bFGF/GMSs group results in a less necrosis, less infiltration
of inflammatory cell, and a decreased the cavity ratio and less
apoptotic cells in injured spinal cord, and exerts improved effect
on motor function (20). The
administration of human recombinant osteopontin/GMSs at 1 h
post-ischemic brain reduced the mean infarct volume by 81.8%
compared with that of the untreated control group and extended the
therapeutic window at least to 12 h post-ischemic brain,
demonstrating a markedly enhanced therapeutic potency of GMSs for
the use of osteopontin in the post-ischemic brain (18). These studies suggested that
GMS-mediated drug delivery has huge potential in the hyperacute
period of neurological injury.
In the present study, porous GMSs were synthesized
using a simple FGF10-encapsulating procedure. More specifically,
GMSs loaded with FGF10 were administered to SCI rats; FGF10 was
then slowly released at the site of injury. Behavioral tests were
subsequently performed to assess the neuroprotective effects of
FGF10-loaded GMS, which were also assessed by histopathology and
apoptosis analyses.
Materials and methods
Reagents and antibodies
Every reagent utilized in the present study is
commercially available. FGF10 was provided by Grost Biotechnology.
Anti-caspase-3 (cat. no. 9661), anti-neurofilament (NF200, cat. no.
2836) and anti-β-actin primary antibodies (cat. no. 4967) and
donkey anti-rabbit polyclonal IgG-HRP secondary antibody (cat. no.
7074) were obtained from Cell Signaling Technology, Inc.
GMS fabrication
First, GMSs were synthesized via water-in-oil (w/o)
emulsion crosslinking, as previously described (17) with certain modifications. In brief,
the 15% gelatin solution (w/v) was first synthesized, followed by
dissolution of NaCl (0.2 g) in gelatin solution (4 ml; aqueous
phase). Then, the aqueous phase was introduced dropwise into
paraffin solution (40 ml) that contained 1.5% spann-80 and was
heated to 50°C. The mixture was subjected to a 30-min
emulsification at 137 × g under paddle stirring. After cooling in
an ice bath, the w/o emulsion was stirred for 30 min to
spontaneously gelate the gelatin aqueous phase. Thereafter, a
paraformaldehyde/isopropanol (40 ml, 5:35, v/v) solution was
introduced into the w/o emulsion, NaOH was added to adjust the
solution pH to 9.0, and the mixture was stirred for an additional 3
h for microsphere crosslinking. Subsequently, the samples were
centrifuged at 1,000 × g to collect microspheres at room
temperature. Residual oil was removed from the surface by washing
repeatedly with isopropanol, followed by overnight drying under
vacuum. Finally, NaCl (pore-forming agent) was removed by rinsing
the microspheres thrice with distilled water, followed by further
drying under vacuum. As a control, normal microspheres were
prepared by the same process, except that NaCl was not added.
FGF10-loaded GMS preparation
FGF10-loaded GMSs were fabricated as previously
described (20), with certain
modifications. In brief, 0.3 mg/ml FGF10 aqueous solution was added
to dry GMSs (100 mg) to encapsulate FGF10. The suspension was then
maintained for 4 h under ambient conditions. Distilled water (300
µl) was used to rinse the FGF10/GMS mixture twice for removal of
non-encapsulated FGF10. FGF10-loaded GMSs were then harvested for
lyophilization, followed by annealing via a 12-h incubation using
10% human serum albumin (MilliporeSigma) at 37°C. Immediately
before injection, FGF10-loaded GMSs were dried by adding sterile
phosphate-buffered saline (PBS; pH 7.4), and a 50-µl microsphere
suspension was prepared for each animal. Meanwhile, sterile PBS was
added to hydrate the unloaded dry microspheres used as a
control.
Encapsulation efficiency
An enzyme-linked immunosorbent assay (ELISA) kit
(cat. no. SEKH-0425; Beijing Solarbio Science & Technology Co.,
Ltd.) was used to determine the encapsulation efficiency. Briefly,
0.3 mg/ml FGF10 aqueous solution was introduced into the dry GMSs
at various ratios (50, 100, 200, 300, or 500 µg FGF10/100 mg dry
GMSs); the suspension was then maintained for 4 h under ambient
conditions. The FGF10/GMS mixture was rinsed twice with distilled
water (300 µl) to remove non-encapsulated FGF10. After rinsing, the
supernatant was harvested by centrifuging for 2 min at 800 × g at
room temperature. An ELISA kit was then utilized to quantify the
FGF10 level within the supernatant. The following formula was
applied to determine the loading efficiency for the FGF10-loaded
GMSs: Loading efficiency (%)=(FGF10 within supernatants)/total
FGF10×100. Each sample was tested in triplicate.
Microsphere characterization
Fluorescein isothiocyanate-labeled FGF10
(FITC-FGF10) was used to prepare FITC-FGF10-loaded GMSs for in
vitro release analysis, which was conducted using a previously
described method (21) with slight
modification. Specifically, FITC-FGF10-loaded GMSs (50 mg) were
dispersed in PBS (1.5 ml) and then placed in a thermostatic
oscillator. Microspheres were subjected to centrifugation for 5 min
at 1,000 × g at pre-set times. After collecting the supernatant
(150 µl), freshly prepared PBS was added to the system volume, such
that the volume remained the same. A microplate reader (Thermo
Fisher Scientific, Inc.) was used to quantify the fluorescence
intensity of the samples at 495 and 525 nm. The fluorescence
intensity of encapsulated FITC-FGF10 was considered analogous to
that of the FITC-FGF10 solution, which was obtained by dissolving
FITC-FGF10 in a volume identical to that of the release medium.
This formula was utilized to determine the cumulative release rate
of FITC-FGF10 from FITC-FGF10 microspheres in vitro.
Rat SCI model
Female Sprague-Dawley (SD) rats (n=48; age, 8–10
weeks) weighing 240–260 g were used in the experiments. The animals
were raised in the laboratory under standard conditions (20–24°C,
50–55% humidity, 12-h light/dark cycle) with free access to food
and water. Each rat was intraperitoneally injected with 50 mg/kg
pentobarbital sodium for anesthesia. Thereafter, laminectomy was
performed at the thoracic vertebra (T9-T10). After fully exposing
the spinal cord, 30 g vascular clips (Oscar, China) were used to
induce a moderate crushing injury for 1 min (22). The rats were randomized to the SCI
(n=36) and sham groups (n=12); for rats in the sham group, an
identical process was performed except that no crushing injury was
induced. Lesions were subsequently injected with 20 µl FGF10
solution (n=12)/FGF10-loaded microspheres (60 µg/rat, n=12) using a
16-G needle. An equivalent amount of saline was injected into rats
in the SCI (n=12) and sham groups. Postoperatively, all animals
were returned to their original environment, with manual bladder
expression performed twice per day until bladder function was
restored. All animals were aseptically collected after euthanasia
via CO2 inhalation (40% vol/min for 5 min), and relevant
spinal cords were removed for further experiments. The present
study was approved by the Animal Care and Use Committee of Hainan
Medical University (approval no. 2019–45; Haikou, China).
Recovery of locomotion
To assess recovery of locomotion post-SCI, the
Basso, Beattie and Bresnahan (BBB) locomotor rating scale was used,
together with a previously described incline plane test (23). Briefly, BBB scores reflect joint
movement and muscle strength, where a score of 0 indicates complete
paralysis and 21 normal locomotion. Two incline plane test
positions (left or right side up) were used; instances where rats
were able to maintain their position for 5 sec without falling were
recorded.
Hematoxylin-eosin (H&E) and Nissl
staining
To quantify necrotic tissue in the spinal cord
cavity area postoperatively, all animals were sacrificed on day 28
to collect spinal cord tissues, which were subjected to paraffin
embedding. Subsequently, 5-µm transverse slices were obtained and
stained with H&E for 5 min at room temperature. The transverse
sections were also treated with 1% cresyl violet acetate for 20 min
at room temperature for Nissl staining to measure surviving
neuronal cells.
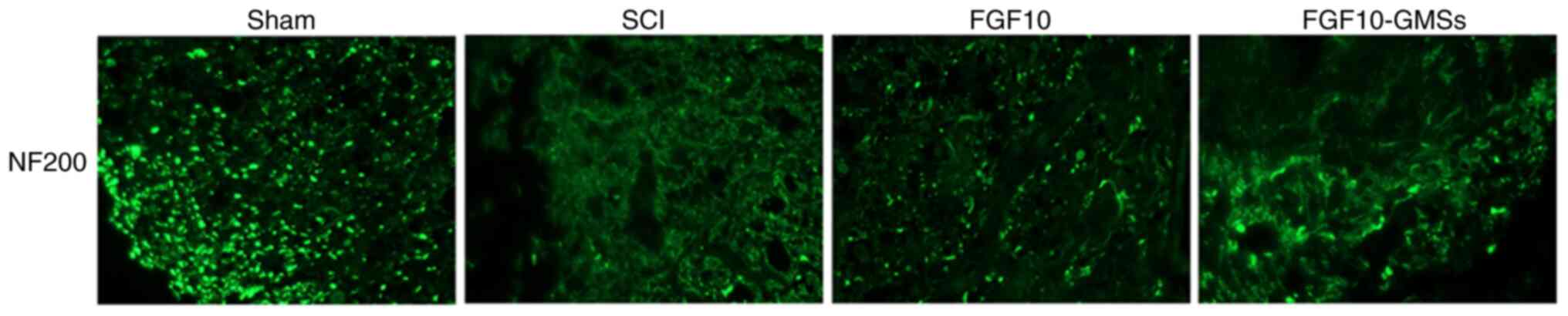
Immunohistochemical staining
The primary antibody against NF200 (1/500) was used
to incubate 5-µm transverse spinal cord sections overnight at 4°C,
followed by further incubation with the secondary antibody for 1 h
at 37°C. An optical microscope (ECLIPSE Ti-S; Nikon, Corporation)
was used for image acquisition. Thereafter, technicians blinded to
the treatments counted the positively stained cells in every
mesencephalic section in the striatum. Image-Pro Plus software
(version 7.0; Media Cybernetics, Inc.) was used to quantify cell
density.
TUNEL apoptosis assay
The one-step TUNEL Apoptosis Assay Kit (Roche
Diagnostics GmbH) was used to detect in vivo DNA
fragmentation. To test apoptotic DNA fragmentation, animals were
sacrificed and spinal cord tissues were collected, which were fixed
in 4% polyformaldehyde for 24 h at room temperature and then
subjected to paraffin embedding. Vertical slices (5 µm) were
deparaffinized via propyl glycol for 30 min in room temperature and
rehydrated via a gradient concentration of alcohol at room
temperature, and were then incubated with 0.1% Triton X-100 for 15
min on ice. Apoptotic cells in the tissue sections were stained
with TUNEL Apoptosis Assay Kit (Roche Diagnostics GmbH), according
to the manufacturer's instructions. A total of 50 µl terminal
deoxynucleotidyl transferase was mixed with 450 µl
fluorescein-labeled deoxyuridine triphosphate. The slides were
treated with the reaction mixture for 1 h at 37°C and with DAPI (5
µg/ml) for 8 min at room temperature. Images in five fields were
captured using the confocal ECLIPSE Ti-S microscope (Nikon
Corporation; magnification, ×40) to measure the apoptotic
level.
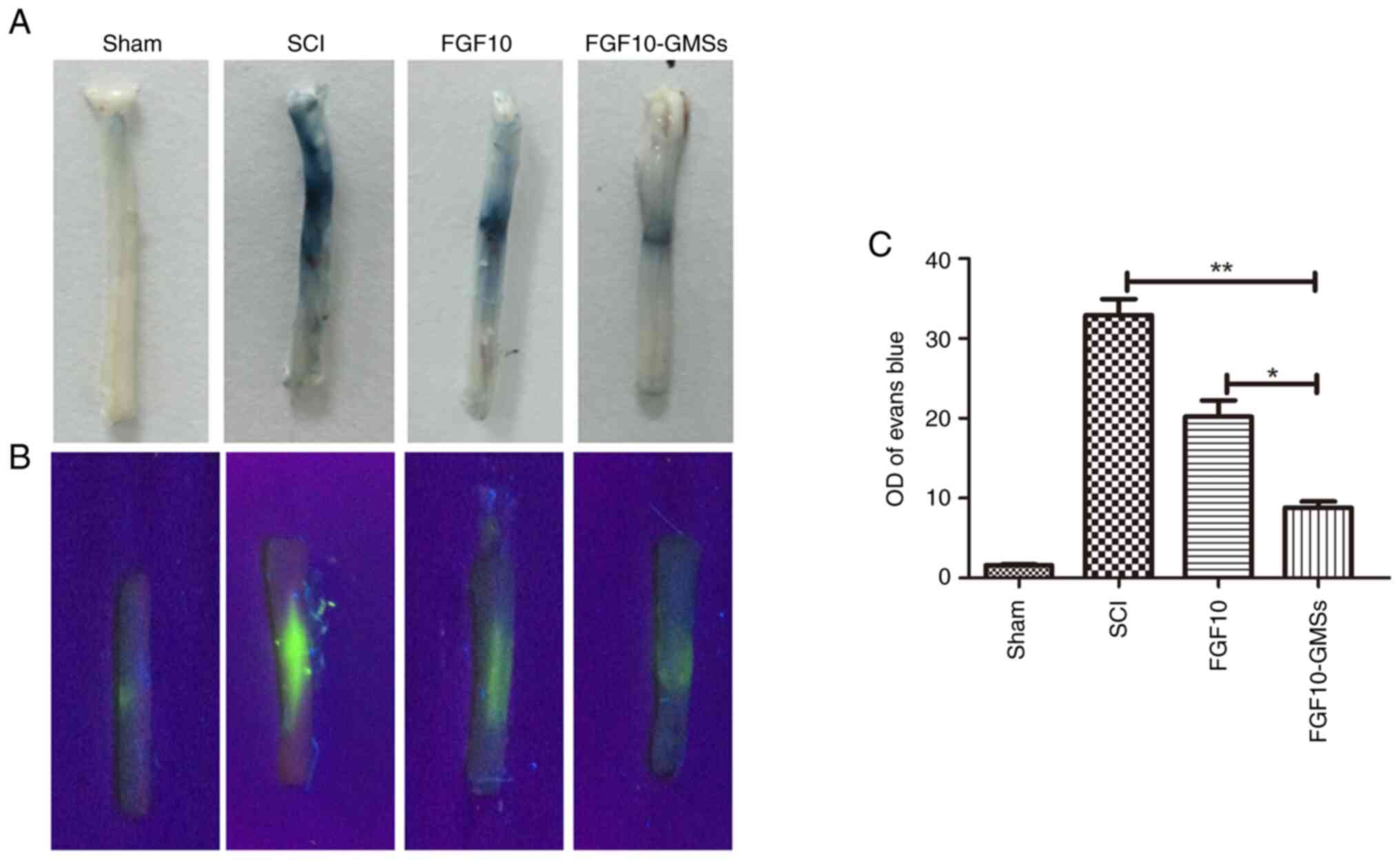
Measurement of BSCB disruption
Evans blue (EB) dye was used to analyze BSCB
disruption, as previously described by the authors (24). In brief, after SCI induction, each
rat was injected with 2% EB dye (4 ml/kg) on day 1 via the tail
vein. After 2 h, anesthesia was administered and sacrifice
performed, and 30-µm coronal spinal cord slices were prepared. A
confocal fluorescence microscope was used to observe EB
fluorescence intensity.
Western blot assay
Spinal cord tissue from T8 to T11 was obtained at 7
days after operation. Briefly, tissue was lysed using
radioimmunoprecipitation buffer (MilliporeSigma) containing
protease and phosphatase inhibitors (1 mM). Following the addition
of bicinchoninic acid reagent for determining protein
concentration, equal amounts of proteins (50 µg) were subjected to
10% gel separation, followed by transfer onto a polyvinylidene
difluoride membrane (Bio-Rad Laboratories Inc.). Thereafter, 5%
(w/v) milk (Bio-Rad Laboratories, Inc.) was utilized to block the
membrane for 90 min at room temperature, followed by incubation
with the primary antibody (anti-cleaved-caspase-3) at 4°C overnight
and incubation with the secondary antibody for 60 min at room
temperature. The ChemiDoc XRS+ imaging system (version
5.2; Bio-Rad Laboratories, Inc.) was used to visualize the
signal.
Statistical analysis
One-way ANOVA followed by Tukey's post hoc test was
utilized to compare more than two groups using GraphPad Prism 5.0
(Dotmatics). P<0.05 was considered to indicate a statistically
significant difference. Results are expressed as the mean ± SD.
Results
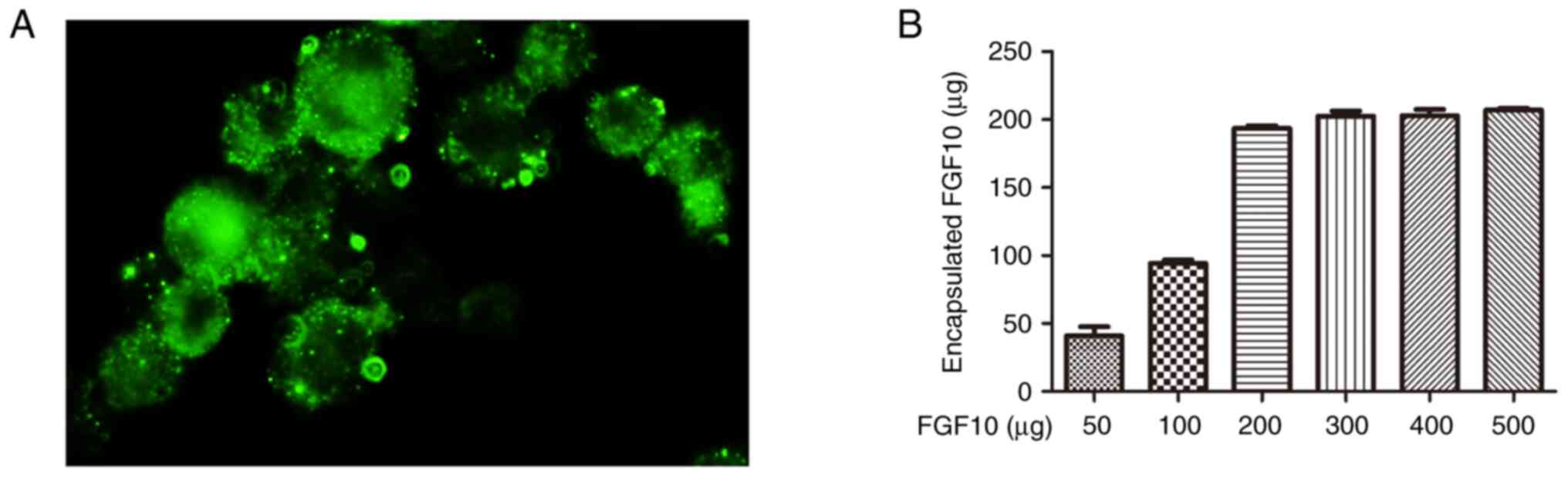
FGF10 encapsulation within porous
microspheres
To determine the maximum FGF10 load, FGF10 at
varying levels was mixed with freeze-dried microspheres (100 mg)
and incubated for 12 h. The actual FGF10 encapsulated level within
microspheres was then quantified (Fig.
1A) and increased according to the initial quantity used. When
the added FGF10 increased, the encapsulated FGF10 also increased
accordingly and after the addition of 200 µg FGF10, the
encapsulated FGF10 reached the maximum (200 µg/100 mg). To
investigate the distribution of encapsulated FGF10 within the
microspheres, FITC-FGF10 was encapsulated in porous GMSs by an
identical process. A uniform distribution of green fluorescence was
observed within bulk microspheres, reflecting high permeability of
the intact microspheres to FGF10 (Fig.
1B).
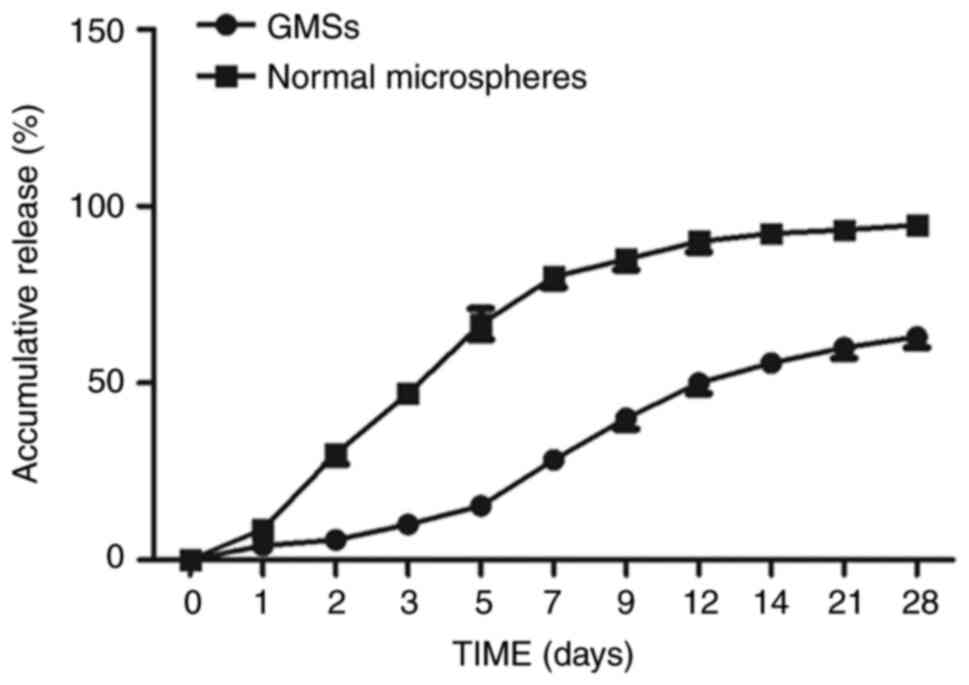
Sustained release of FGF10 from
FGF10-GMSs
To assess sustained release of FGF10 from GMSs, an
in vitro release assay was used. The cumulative release of
FGF10 from GMSs is demonstrated in Fig. 2. Normal GMSs rapidly released FGF10
in short bursts; ~30% of the encapsulated FGF10 was released within
the initial 48 h, with complete release being achieved within 2
weeks. By contrast, porous microspheres continuously and gradually
released FGF10 over 2 weeks, with no distinct burst release pattern
observed within the first 48 h. On day 28, the proportion of
encapsulated FGF10 released was only ~65%. The difference between
normal microsphere and porous GMSs may be attributed to the
distribution difference of FGF10 in the microsphere. Briefly, the
burst FGF10 release of microsphere was dependent on the FGF10
absorbed on the surface of microsphere. Compared with dense and of
little porosity surface of normal microsphere, the encapsulated
FGF10 in porous GMSs homogenously distributed inside the bulk
porous microspheres without a significant adsorption on their
surfaces, making the diffusion pathway along which FGF10 released
from microsphere longer.
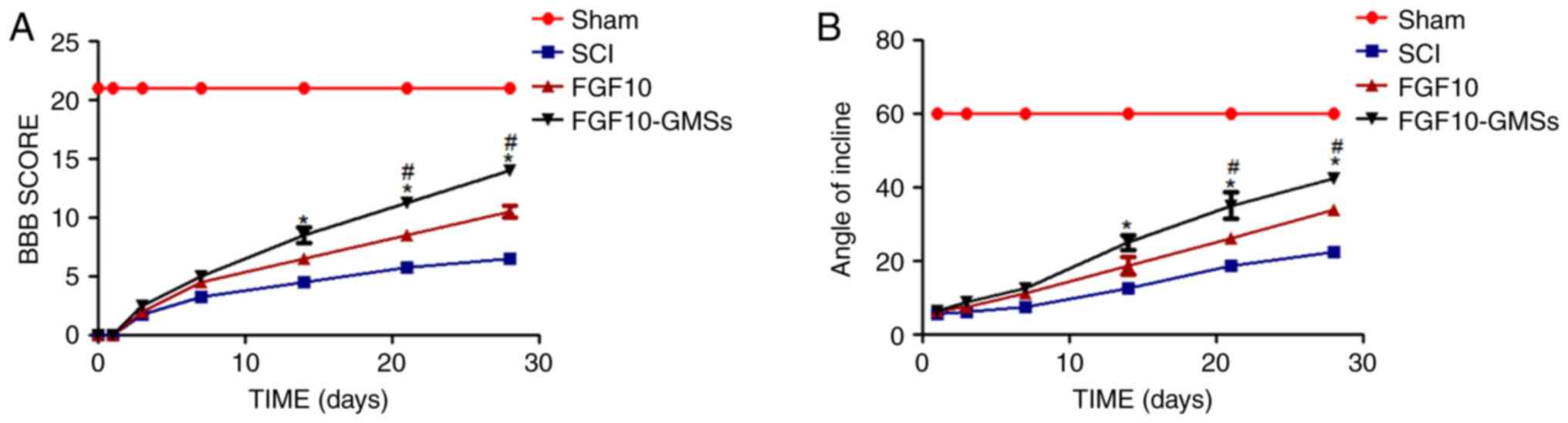
FGF10-GMSs promote locomotor recovery
after acute SCI in vivo
The BBB locomotor rating scale and incline plane
test scores were used to assess the therapeutic effect of
FGF10-GMSs. The sham group had normal BBB scores (21 points;
Fig. 3). At 1 and 3 days after
contusion, there was no significant difference in BBB scores among
the FGF10-GMS, FGF10 and SCI groups. Compared with the SCI group,
notable behavioral changes in the FGF10-GMS group were observed at
14 days (P<0.05). At 21 and 28 days, rats in the FGF10-GMS and
FGF10 group exhibited favorable motor function recovery (Fig. 3A), particularly those in the
FGF10-GMS group. The incline plane test results were consistent
with the BBB locomotor rating scale scores (Fig. 3B); GMSs enhanced the functional
improvement observed in SCI rats after FGF10 administration.
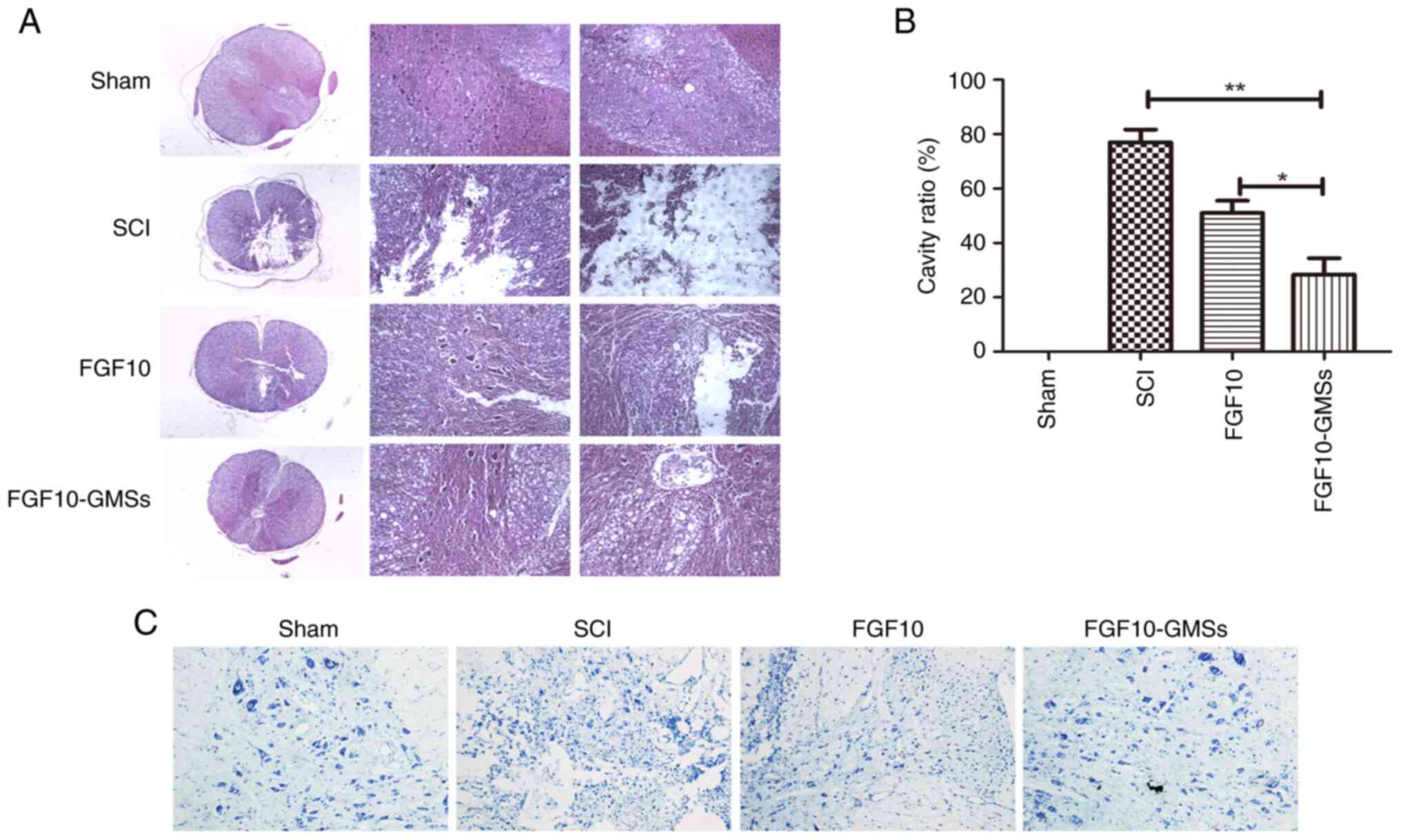
FGF10-GMSs improve histological injury
in SCI rats
According to the H&E and Nissl staining results,
destruction of central gray and peripheral white matter was most
pronounced in the SCI group and was accompanied by obvious motor
neuron loss in the anterior horn. Compared with the SCI and FGF10
groups, less necrosis, karyopyknosis and infiltrating
polymorphonuclear leukocytes were observed in the FGF10-GMS group,
along with a significantly smaller proportion of necrotic tissue in
the spinal cavity (Fig. 4).
FGF10-GMSs attenuate BSCB disruption
after SCI
The intensity of EB staining in spinal cord sections
was markedly weaker in the FGF10 group compared with the SCI group
as revealed in Fig. 5A, suggesting
that FGF10 enhanced the integrity of the BSCB after SCI. However,
the results indicated that the BSCB was best protected in the
FGF10-GMS group. To quantify the leakage of high molecular weight
molecules, FITC-dextran was injected into the tail vein. The
intensity of the FITC-dextran signal was significantly lower in the
FGF10 than SCI group (Fig. 5B and
C).
FGF10-GMSs promote regeneration of
injured neurons in SCI rats
NF proteins, including NF200, are markers of
neuronal repair (25).
Immunofluorescence staining was conducted to detect NF200 (Fig. 6). In the SCI group, NF200-positive
fibers showed obvious degradation, along with broken axons. While
the FGF10 group exhibited an increase in NF200 expression around
the lesion compared with the SCI group, this increase was even more
marked in the FGF10-GMS group.
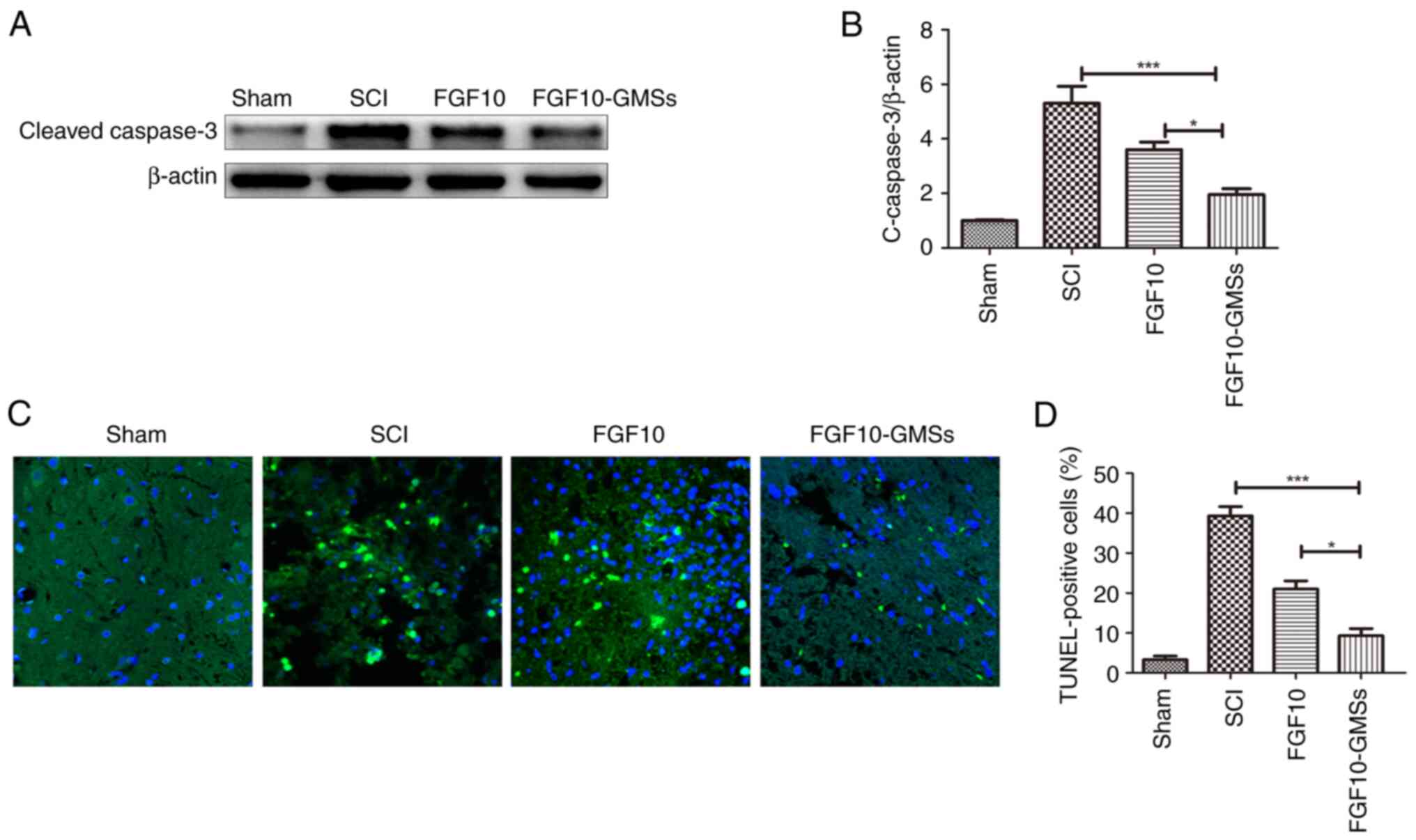
FGF10-GMSs inhibit apoptosis in SCI
rats
Caspase-3 initiates apoptosis signaling (26). The results of western blotting of
caspase-3 are presented in Fig. 7A and
B. Caspase-3 expression in the SCI group was obviously enhanced
28 days after injury compared with uninjured rats. Apoptosis was
suppressed to a greater extent in the FGF10-GMS group than in the
FGF10 and SCI groups. TUNEL assay was also conducted to detect
apoptosis and yielded similar results; the number of TUNEL-positive
cells 28 days after FGF10-GMS treatment was significantly decreased
compared with the FGF10 group (Fig.
7C).
Discussion
SCI may induce cystic cavity formation and neuronal
loss, thereby inhibiting axonal regeneration. Although great
progress has been made in the treatment of SCI, no optimal clinical
strategy has been established, and relatively few therapeutics have
been developed. Numerous factors limit the capacity for spontaneous
spinal cord regeneration, including insufficient growth-promoting
substances and the expression of growth inhibitors. FGF10 is highly
expressed within the nervous system and is released upon sublethal
cellular injury (10,12). However, FGF10 cannot be delivered
systemically; as a macromolecular protein, systemic delivery of
FGF10 may cause enzyme degradation, and it may also fail to cross
the BSCB. Similarly, growth factors are not utilized in the
clinical treatment of heart disease due to their low bioactivity
and short half-lives with direct in vivo injection (27). Furthermore, FGF10 may induce
mitosis, which can in turn result in cancer in normal tissues. To
resolve these issues, a controlled-release system is needed to
improve exogenous growth factor bioavailability.
Previously, implantable porous GMSs have been widely
investigated in the context of SCI regeneration due to their
tunable physical features and compatibility with molecular and
cellular treatments for wounds (20). Notably, implantable bFGF-GMSs
facilitate healing in SCI rats and accelerate neurological
functional recovery (20). Gelatin
hydrogel microspheres appear to be promising as a vehicle for
sustained growth factor release in clinical practice, to regenerate
injured brain tissues via their action on endogenous neural stem
cells (28). In fact, this
delivery system is already used extensively in animal models of
neurological injury. In the present study, porous GMSs were used
for sustained release of FGF10, which was locally implanted into
SCI rats to promote neurological functional recovery and neural
regeneration. The implantable porous GMSs were based on gelatin and
did not show toxicity. Gelatin is biodegradable and biocompatible
and thus suitable for implantation into the spinal cord (20). Instead of organic solvents, a w/o
emulsion containing materials for fabricating porous microspheres
was used. The encapsulated FGF10 easily penetrated the microsphere
surfaces of porous GMSs in aqueous solution.
In the rat SCI model of the present study, FGF10-GMS
treatment led to superior outcomes in terms of neuroprotection,
motor function and morphological recovery compared with FGF10
treatment. First, FGF10-GMS markedly increased BBB scores and
incline plane test performance compared with FGF10. On day 14 after
treatment, FGF10-GMS induced more rapid functional recovery in the
left hindlimb compared with FGF10 treatment. Second, H&E and
Nissl staining showed an obvious protective effect of FGF10-GMS, as
reflected by decreased levels of karyopyknosis, necrosis and
polymorphonuclear leukocyte infiltration relative to the FGF10 and
SCI groups. FGF10 release was significantly extended due to the
encapsulation with GMSs, which play an essential role in the
critical period for recovery processes, including controlling
inflammation and related tissue necrosis. A previous study has
revealed the neuroprotective effect of FGF10 on acute brain injury
via inhibit inflammation and tissue necrosis (10). Collectively, these data suggested
that GMS-loaded FGF10 delivery has huge potential when it was used
in the hyperacute period in SCI.
Apoptosis post-SCI modulates neuronal degeneration
(29,30). In the present study, FGF10-GMS
treatment suppressed apoptosis to a greater degree than did FGF10.
The expression of caspase-3, which is an important protein in
apoptotic pathways, was decreased following FGF10-GMS treatment,
suggesting that caspase-3 exerted anti-apoptotic effects; this was
supported by the TUNEL assay results. Immunohistochemical staining
of NF200 further verified the neuroprotective effects of FGF10 in
SCI rats. It has also been demonstrated that FGF10 enhanced the
functional recovery after SCI via inhibition of axonal injury and
the FGFR2/PI3K/Akt-dependent apoptosis (12), indicating that GMS-loaded FGF10
delivery has improved neuroprotective effects on axon protection
and anti-apoptosis in SCI.
BSCB integrity is important for maintaining spinal
cord function. In a previous study, BSCB disruption was detected at
1 h post-injury and persisted for 5 days. Typically, permeability
was greatest at 24 h post-injury (31). In the present study, FGF10 reduced
EB staining intensity on day 1, which was strongly associated with
BSCB penetrability; this effect was even greater in the FGF10-GMS
group. Thus, with targeted delivery, FGF10 can cross the BSCB and
accumulate at the lesion site more efficiently compared with other
administration routes. Furthermore, normal microspheres released
FGF10 in rapid bursts; 30% of the encapsulated FGF10 was released
within the first 48 h, and 100% was released over the following 2
weeks. By contrast, porous microspheres released FGF10 gradually
over 2 weeks, with no burst release pattern observed within the
first 48 h. GMS-loaded FGF10 delivery mode can ensure the
continuous release of FGF10, reduce the degradation of FGF10 in
tissues, and thus continue to play a protective role on injured
tissues.
In conclusion, FGF10 has been reported to have
anti-inflammatory, anti-apoptotic and axonal protection effects in
neurological injury. FGF10 was encapsulated into implantable porous
GMSs and released in a sustained manner in SCI rats. This delivery
exerted improved neuroprotective effects and created conditions
promoting axonal regeneration and functional restoration compared
with free FGF10. Therefore, GMS-loaded FGF10 delivery has huge
potential when being used in the hyperacute period in SCI.
Acknowledgements
Not applicable.
Funding
The present study was supported by Hainan Natural Science
Foundation Youth Fund Project (grant no. 820QN406).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YG, TH and YY designed the present study. YG, YY,
HQ, HZ and GW contributed to experiments and statistical analysis.
YY, HQ and HZ contributed to manuscript preparation and revision
for important intellectual content. YG and YY confirm the
authenticity of all the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Animal Care
and Use Committee of Hainan Medical University (2019-45, Haikou,
China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ren H, Han M, Zhou J, Zheng ZF, Lu P, Wang
JJ, Wang JQ, Mao QJ, Gao JQ and Ouyang HW: Repair of spinal cord
injury by inhibition of astrocyte growth and inflammatory factor
synthesis through local delivery of flavopiridol in PLGA
nanoparticles. Biomaterials. 35:6585–6594. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Anjum A, Yazid MD, Fauzi Daud M, Idris J,
Ng AMH, Selvi Naicker A, Ismail OHR, Athi Kumar RK and Lokanathan
Y: Spinal cord injury: Pathophysiology, multimolecular
interactions, and underlying recovery mechanisms. Int J Mol Sci.
21:75332020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang Y, Al Mamun A, Yuan Y, Lu Q, Xiong
J, Yang S, Wu C, Wu Y and Wang J: Acute spinal cord injury:
Pathophysiology and pharmacological intervention (Review). Mol Med
Rep. 23:4172021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kawabata S, Takano M, Numasawa-Kuroiwa Y,
Itakura G, Kobayashi Y, Nishiyama Y, Sugai K, Nishimura S, Iwai H,
Isoda M, et al: Grafted Human iPS cell-derived oligodendrocyte
precursor cells contribute to robust remyelination of demyelinated
axons after spinal cord injury. Stem Cell Reports. 6:1–8. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang HY, Wang ZG, Wu FZ, Kong XX, Yang J,
Lin BB, Zhu SP, Lin L, Gan CS, Fu XB, et al: Regulation of
autophagy and ubiquitinated protein accumulation by bFGF promotes
functional recovery and neural protection in a rat model of spinal
cord injury. Mol Neurobiol. 48:452–464. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Assinck P, Duncan GJ, Plemel JR, Lee MJ,
Stratton JA, Manesh SB, Liu J, Ramer LM, Kang SH, Bergles DE, et
al: Myelinogenic plasticity of oligodendrocyte precursor cells
following spinal cord contusion injury. J Neurosci. 37:8635–8654.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim M, Kim KH, Song SU, Yi TG, Yoon SH,
Park SR and Choi BH: Transplantation of human bone marrow-derived
clonal mesenchymal stem cells reduces fibrotic scar formation in a
rat spinal cord injury model. J Tissue Eng Regen Med.
12:e1034–e1045. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Itoh N and Ohta H: Fgf10: A
paracrine-signaling molecule in development, disease, and
regenerative medicine. Curr Mol Med. 14:504–509. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chao CM, Moiseenko A, Zimmer KP and
Bellusci S: Alveologenesis: Key cellular players and fibroblast
growth factor 10 signaling. Mol Cell Pediatr. 3:172016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li YH, Fu HL, Tian ML, Wang YQ, Chen W,
Cai LL, Zhou XH and Yuan HB: Neuron-derived FGF10 ameliorates
cerebral ischemia injury via inhibiting NF-κB-dependent
neuroinflammation and activating PI3K/Akt survival signaling
pathway in mice. Sci Rep. 6:198692016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dong L, Li R, Li D, Wang B, Lu Y, Li P, Yu
F, Jin Y, Ni X, Wu Y, et al: FGF10 enhances peripheral nerve
regeneration via the preactivation of the PI3K/Akt
signaling-mediated antioxidant response. Front Pharmacol.
10:12242019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen J, Wang Z, Zheng Z, Chen Y, Khor S,
Shi K, He Z, Wang Q, Zhao Y, Zhang H, et al: Neuron and
microglia/macrophage-derived FGF10 activate neuronal FGFR2/PI3K/Akt
signaling and inhibit microglia/macrophages TLR4/NF-κB-dependent
neuroinflammation to improve functional recovery after spinal cord
injury. Cell Death Dis. 8:e30902017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Farooq M, Khan AW, Kim MS and Choi S: The
role of fibroblast growth factor (FGF) signaling in tissue repair
and regeneration. Cells. 10:32422021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Turner N and Grose R: Fibroblast growth
factor signalling: From development to cancer. Nat Rev Cancer.
10:116–129. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen L, Zhang Y, Yin L, Cai B, Huang P, Li
X and Liang G: Fibroblast growth factor receptor fusions in cancer:
Opportunities and challenges. J Exp Clin Cancer Res. 40:3452021.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hui Q, Jin Z, Li X, Liu C and Wang X: FGF
family: From drug development to clinical application. Int J Mol
Sci. 19:18752018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chang SS, Yokomise H, Matsuura N, Gotoh M
and Tabata Y: Novel therapeutic approach for pulmonary emphysema
using gelatin microspheres releasing basic fibroblast growth factor
in a canine model. Surg Today. 44:1536–1541. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jin Y, Kim IY, Kim ID, Lee HK, Park JY,
Han PL, Kim KK, Choi H and Lee JK: Biodegradable gelatin
microspheres enhance the neuroprotective potency of osteopontin via
quick and sustained release in the post-ischemic brain. Acta
Biomater. 10:3126–3135. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kempen DH, Lu L, Heijink A, Hefferan TE,
Creemers LB, Maran A, Yaszemski MJ and Dhert WJ: Effect of local
sequential VEGF and BMP-2 delivery on ectopic and orthotopic bone
regeneration. Biomaterials. 30:2816–2825. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lan L, Tian FR, ZhuGe DL, ZhuGe QC, Shen
BX, Jin BH, Huang JP, Wu MZ, Fan LX, Zhao YZ and Xu HL: Implantable
porous gelatin microspheres sustained release of bFGF and improved
its neuroprotective effect on rats after spinal cord injury. PLoS
One. 12:e01738142017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Minardi S, Pandolfi L, Taraballi F, De
Rosa E, Yazdi IK, Liu X, Ferrari M and Tasciotti E: PLGA-Mesoporous
silicon microspheres for the in vivo controlled temporospatial
delivery of proteins. ACS Appl Mater Interfaces. 7:16364–16373.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang Q, He Y, Zhao Y, Xie H, Lin Q, He Z,
Wang X, Li J, Zhang H, Wang C, et al: A thermosensitive
heparin-poloxamer hydrogel bridges aFGF to treat spinal cord
injury. ACS Appl Mater Interfaces. 9:6725–6745. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Basso DM, Beattie MS and Bresnahan JC: A
sensitive and reliable locomotor rating scale for open field
testing in rats. J Neurotrauma. 12:1–21. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zheng B, Ye L, Zhou Y, Zhu S, Wang Q, Shi
H, Chen D, Wei X, Wang Z, Li X, et al: Epidermal growth factor
attenuates blood-spinal cord barrier disruption via PI3K/Akt/Rac1
pathway after acute spinal cord injury. J Cell Mol Med.
20:1062–1075. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu WG, Wang ZY and Huang ZS: Bone
marrow-derived mesenchymal stem cells expressing the bFGF transgene
promote axon regeneration and functional recovery after spinal cord
injury in rats. Neurol Res. 33:686–693. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xin DQ, Hu ZM, Huo HJ, Yang XJ, Han D,
Xing WH, Zhao Y and Qiu QH: Schisandrin B attenuates the
inflammatory response, oxidative stress and apoptosis induced by
traumatic spinal cord injury via inhibition of p53 signaling in
adult rats. Mol Med Rep. 16:533–538. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Beenken A and Mohammadi M: The FGF family:
Biology, pathophysiology and therapy. Nat Rev Drug Discov.
8:235–253. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Nakaguchi K, Jinnou H, Kaneko N, Sawada M,
Hikita T, Saitoh S, Tabata Y and Sawamoto K: Growth factors
released from gelatin hydrogel microspheres increase new neurons in
the adult mouse brain. Stem Cells Int. 2012:9151602012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rong Y, Liu W, Wang J, Fan J, Luo Y, Li L,
Kong F, Chen J, Tang P and Cai W: Neural stem cell-derived small
extracellular vesicles attenuate apoptosis and neuroinflammation
after traumatic spinal cord injury by activating autophagy. Cell
Death Dis. 10:3402019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jia G, Zhang Y, Li W and Dai H:
Neuroprotective role of icariin in experimental spinal cord injury
via its antioxidant, antineuroinflammatory and antiapoptotic
properties. Mol Med Rep. 20:3433–3439. 2019.PubMed/NCBI
|
|
31
|
Lee JY, Kim HS, Choi HY, Oh TH and Yune
TY: Fluoxetine inhibits matrix metalloprotease activation and
prevents disruption of blood-spinal cord barrier after spinal cord
injury. Brain. 135:2375–2389. 2012. View Article : Google Scholar : PubMed/NCBI
|