Introduction
Ovarian hyperstimulation syndrome (OHSS) is one of
the serious complications that occur in ovulation induction cycles
during infertility treatment or, occasionally, following
conception. OHSS is characterized by cystic ovarian swelling and
shifting of fluid from the circulation to the third space. Human
chorionic gonadotropin plays a central role in the onset of OHSS.
Human chorionic gonadotropin increases chemokine production in the
granulosa and theca cells surrounding the ovulating oocytes. These
chemokines bind to their specific receptors, expressed on local and
systemic endothelial cells, which, in turn, transactivate vascular
endothelial growth factor receptor-2 and its signaling pathway.
This signaling stimulates polymerization of cytoskeletal actin and
phosphorylation of adherens junction and tight junction molecules
in endothelial cells. These molecular events induce conformational
changes in the endothelial cells and vascular hyperpermeability. In
its severe form, OHSS potentially leads to life-threatening
conditions, such as massive ascites, pleural effusion, oliguria and
thrombosis/embolism following hemoconcentration (1).
Infertile women with polycystic ovarian syndrome
(PCOS) are at a high risk for developing OHSS in ovulation
induction protocols (2). PCOS is
also closely associated with obesity and insulin resistance. It was
recently demonstrated that weight loss following gastric bypass
surgery improved insulin resistance in obese patients with a
decrease in circulating branched-chain amino acid (BCAA) levels
(3). These findings suggest a
possible association between BCAA and OHSS. The aim of this study
was to investigate the follicular fluid BCAA level in infertile
women who developed OHSS during controlled ovarian stimulation in
an in vitro fertilization program.
Materials and methods
Subjects and methods
Between July, 2012 and September, 2012, follicular
fluid was retrieved from infertile patients at the time of oocyte
collection during in vitro fertilization/intracytoplasmic
sperm injection cycles (4). All the
patients had undergone controlled ovarian stimulation using
gonadotropin-releasing hormone agonist (short protocol) or
antagonist (flexible protocol) (5).
The follicular fluid samples were immediately frozen at −80°C until
measurement. Samples with macroscopic blood contamination were
excluded from the investigation. A total of 20 patients who
developed moderate-to-severe OHSS and 20 age- and body mass
index-matched normoresponders were enrolled in the study. The
follicular fluid concentration of BCAA (a total of leucine,
isoleucine and valine concentration) and tyrosine (standardization
control) were measured using an enzymatic assay (Diacolor-BTR kit;
Toyobo, Osaka, Japan).
This study was approved by our Institutional Review
Board (protocol no. 125081903) and all the subjects provided
informed consent.
Statistical analysis
The values were compared between the OHSS and the
normoresponder group using the two-tailed Student’s t-test,
non-parametric Mann-Whitney U test, or Pearson’s χ2
test.
Results
Demographics
There were no significant differences in
demographics between the patients and the normoresponders,
including infertility period, infertility category (85% primary
infertility rate in the OHSS and 80% primary infertility rate in
the normoresponder group) and the values of basal pituitary
hormones and estradiol (Table I).
However, the total human menopausal gonadotropin dose was
significantly lower in the OHSS compared to that in the
normoresponder group (P<0.0001). The number of the oocytes
retrieved and fertilized and the number of the embryos/blastocysts
frozen were significantly higher in the OHSS compared to that in
the normoresponder group (P<0.0001). Fresh embryo/blastocyst
transfer cycles were cancelled in all the patients with OHSS.
 | Table IDemographics and in vitro
fertilization outcome in patients who developed ovarian
hyperstimulation syndrome (OHSS) and in normoresponders. |
Table I
Demographics and in vitro
fertilization outcome in patients who developed ovarian
hyperstimulation syndrome (OHSS) and in normoresponders.
| Variables | OHSSa |
Normorespondersa | P-value |
|---|
| Age (years) | 34.0±3.3 | 33.4±3.9 | 0.60b |
| Body mass index
(kg/m2) | 20.7±2.1 | 20.1±1.8 | 0.64c |
| Infertility period
(months) | 31.0±26.3 | 24.9±11.7 | 0.26b |
| Basal luteinizing
hormone level (IU/l) | 4.9±2.5 | 4.4±3.0 | 0.58c |
| Basal follicle
stimulating hormone level (IU/l) | 5.2±1.5 | 5.4±2.1 | 0.75c |
| Basal estradiol level
(pg/ml) | 81.7±23.9 | 82.1±24.7 | 0.83c |
| Prolactin level
(ng/ml) | 14.1±5.7 | 16.5±9.7 | 0.33c |
| Total human
menopausal gonadotropin dose (IU) | 2,087.5±926.7 | 2,554.1±544.8 | <0.0001c |
| Number of oocytes
retrieved | 17.6±6.0 | 7.3±2.4 | <0.0001b |
| Number of oocytes
fertilized | 9.5±4.9 | 3.8±2.7 | <0.0001b |
| Number of fresh
embryos/blastocysts transferred | 0 | 0.8±0.7 | <0.0001b |
| Number of
embryos/blastocysts frozen | 6.1±4.2 | 1.9±2.4 | <0.0001b |
Association of PCOS and OHSS
The incidence of PCOS was significantly higher in
the OHSS (40%) compared to that in the normoresponder group (15%,
P=0.0001). The number of oocytes retrieved, fertilization,
blastocyst achievement and blastocyst freezing rates were also
significantly higher in the OHSS compared to those in the
normoresponder group (P<0.011), as were the cumulative clinical
pregnancy and ongoing pregnancy rates within three transfer cycles
(P<0.0004). There were no fatal complications in neither of the
two groups.
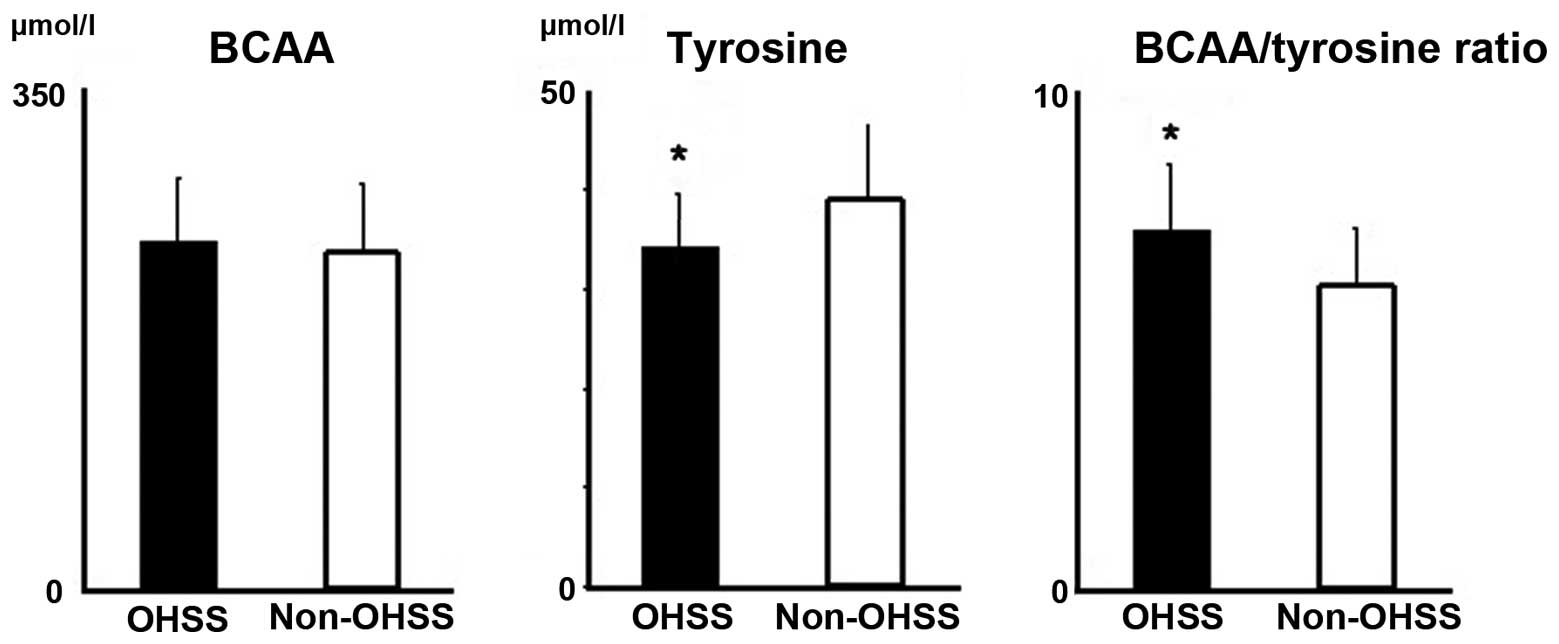
BCAA and tyrosine
The follicular fluid BCAA concentration was similar
between the two groups (P=0.55), whereas the tyrosine concentration
was significantly lower in the OHSS compared to that in the
normoresponder group (P=0.027, Fig.
1). Corresponding to these results, the BCAA/tyrosine ratio was
significantly higher in the OHSS compared to that in the
normoresponder group (P=0.034).
Discussion
In this study, the follicular fluid BCAA
concentration was found to be similar between infertile patients
with and those without OHSS. In the Japanese population, the
incidence of obesity in infertile women with PCOS is significantly
lower compared to that reported in Caucasian populations (5). The incidence of PCOS in our cohort was
significantly higher in the patients who developed
moderate-to-severe OHSS compared to that in non-OHSS patients,
whereas there were no obese women in the two groups. Thus, further
investigations are required to compare follicular fluid BCAA
concentration between obese and non-obese PCOS patients.
The follicular fluid tyrosine concentration, which
was measured as a standard control protein, was found to be
significantly lower in OHSS patients compared to that in
normoresponders. In the human body, tyrosine is an amino acid which
is synthesized from phenylalanine. The ovary is considered to be
one of the active sites of tyrosine synthesis (6). Tyrosine is converted to
L-3,4-dihydroxyphenylalanine by the action of hydroxylase and then
to dopamine by aromatic L-amino acid decarboxylase.
Dopamine receptor agonists, such as docarpamine and
cabergoline, are attracting increasing attention as promising
OHSS-preventive agents (7). The
binding of high-dose dopamine receptor agonists to dopamine
receptor-2 was shown to interfere with vascular endothelial growth
factor-mediated signaling by stimulating internalization of
vascular endothelial growth factor receptor-2, decreasing its
surface expression and rendering it unreachable to vascular
endothelial growth factor (7). A
decrease in the follicular fluid concentration of the dopamine
precursor tyrosine in OHSS patients supports the hypothesis that
tyrosine deficiency in growing follicles may lead to subsequent
dopamine deficiency and dopamine receptor-mediated signaling
attenuation, which may be involved in the etiology and pathogenesis
of OHSS. The potential limitation of this retrospective study is
the bias in participant selection. Although a larger sample size
would be required to address this issue, the marked difference in
this small cohort reflects the significance of the findings.
In conclusion, our results suggest an association
between low follicular fluid tyrosine level and the onset of OHSS.
As in the serum, tyrosine concentration in the follicular fluid is
easily measurable in the clinical practice and may be a potential
predictive marker of OHSS.
References
|
1
|
Kitaya K and Yamada H: Pathophysiological
roles of chemokines in human reproduction: an overview. Am J Reprod
Immunol. 65:449–459. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lainas GT, Kolibianakis EM, Sfontouris IA,
et al: Pregnancy and neonatal outcomes following luteal GnRH
antagonist administration in patients with severe early OHSS. Hum
Reprod. 28:1929–1942. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Laferrere B, Reilly D, Arias S, et al:
Differential metabolic impact of gastric bypass surgery versus
dietary intervention in obese diabetic subjects despite identical
weight loss. Sci Transl Med. 3:80re22011. View Article : Google Scholar
|
|
4
|
Hayashi T, Kitaya K, Tada Y, Taguchi S,
Funabiki M and Nakamura Y: Single curettage endometrial biopsy
injury in the proliferative phase improves reproductive outcome of
subsequent in vitro fertilization-embryo transfer cycle in
infertile patients with repeated embryo implantation failure. Clin
Exp Obstet Gynecol. 40:323–326. 2013.
|
|
5
|
Kitaya K, Tada Y, Taguchi S, Funabiki M,
Hayashi T and Nakamura Y: Local mononuclear cell infiltrates in
infertile patients with endometrial macropolyps versus micropolyps.
Hum Reprod. 27:3474–3480. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kurioka H, Takahashi K and Miyazaki K:
Glucose intolerance in Japanese patients with polycystic ovary
syndrome. Arch Gynecol Obstet. 275:169–173. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Soares SR: Etiology of OHSS and use of
dopamine agonists. Fertil Steril. 97:517–522. 2012. View Article : Google Scholar : PubMed/NCBI
|