Introduction
Kawasaki disease (KD) is one of the most common
vasculitides of childhood (1). The
cause of KD remains unknown; however, it is hypothesized that the
immune system is activated by infectious or environmental triggers
in genetically susceptible hosts (1).
Previous investigations into vasculitis and KD have reported them
as side effects of various vaccinations (2–4). Bonetto
et al (5) reviewed the
literature from January 1994 to June 2014. Although the majority of
the larger, higher quality studies identified no causal association
between vaccination and subsequent development of vasculitis,
including various studies on KD and Henoch-Schönlein purpura (HSP),
the influenza vaccination was ranked first in terms of the number
of published articles regarding vasculitis vaccine association
(according to vaccine type) and KD was third in terms of the number
of published articles regarding vasculitis vaccine association
(according to vasculitis type) (5).
Cases were reported in which children had received vaccinations,
such as those for yellow fever and hepatitis B, and developed KD
(2,3).
However, a report in 2015 on KD that occurred following influenza
vaccination was the only case reported in Japan (4). The present study describes the first
case of KD following immunization for influenza in South Korea and
reviews various studies regarding vasculitis following vaccination
and the causal association between them.
Case report
A male infant, aged 18 months, was admitted to Kyung
Hee University Hospital at Gangdong (Seoul, South Korea; 12 October
2015) for evaluation due to a high-grade fever that had started 5
days prior to the visit. The infant had been immunized for
influenza 24 h before the onset of fever. He was admitted as he had
experienced 6 days of high fever up to 40.0°C, a body rash that had
persisted for 2 days and nonsuppurative bilateral conjunctivitis.
Informed consent for the publication of this case report was waived
as the infant's next of kin could not be contacted despite numerous
attempts to do so.
The body temperature of the infant at the time of
admittance was 39.6°C. The physical examination demonstrated
bilateral conjunctival injection, cracked red lips, strawberry
tongue, erythema of the trunk and the Bacille Calmette-Guérin
inoculation site, and erythema and bilateral edema of the hands.
However, the cervical lymph nodes appeared normal. The peripheral
blood test exhibited leukocytosis (white blood cell count, 12,110
cells/µl), an elevated level of C-reactive protein (15.1 mg/dl) and
an elevated quantity of brain natriuretic peptide (403 pg/ml;
Table I). Echocardiography
demonstrated that the size of the coronary artery was within the
normal range, although the left ventricular ejection fraction was
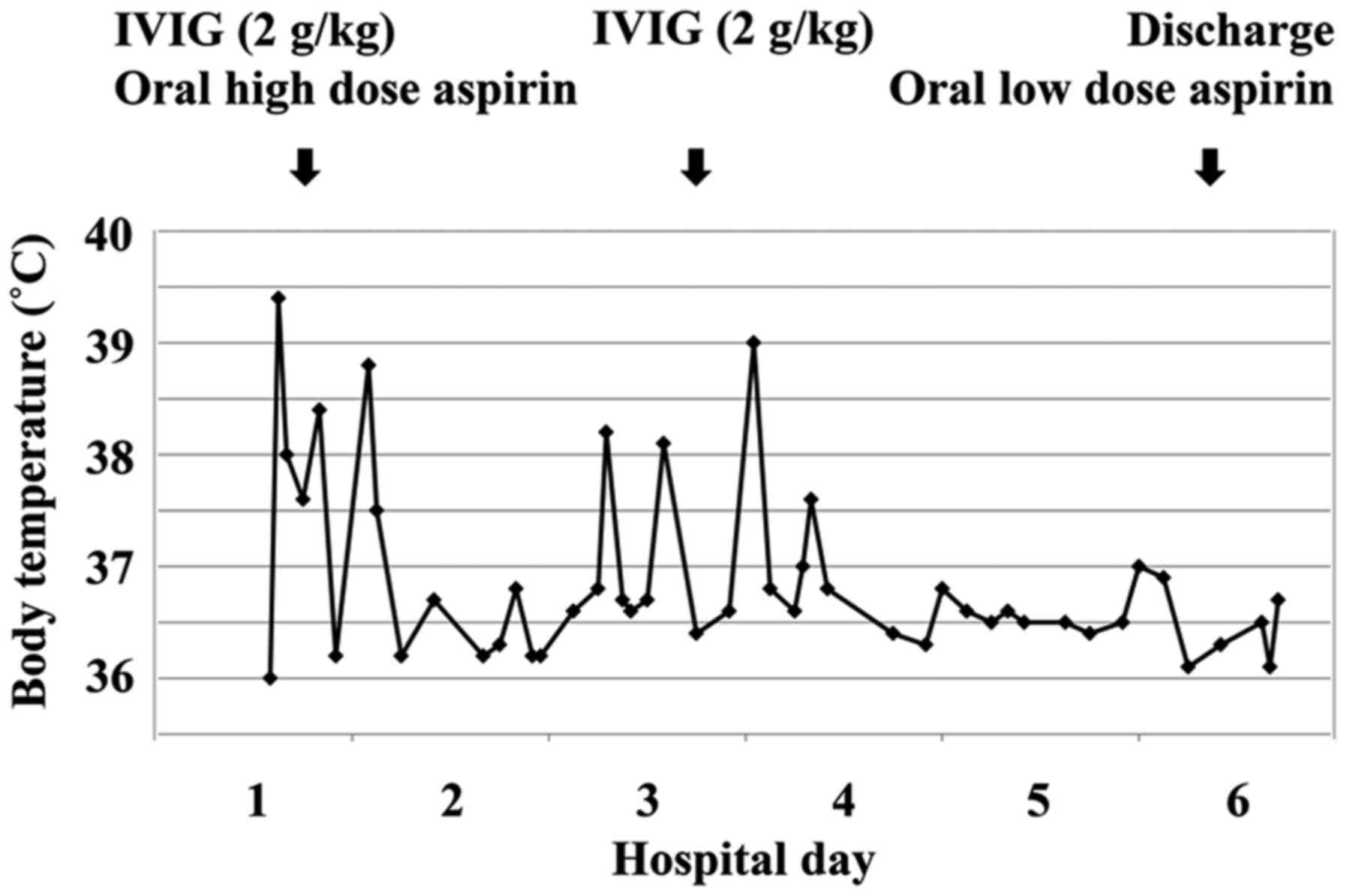
somewhat reduced to 50–55%. Based on these findings, KD treatment
was initiated with intravenous immunoglobulin (IVIG; 2 g/kg/dose)
for 1 day and oral administration of aspirin (50 mg/kg/day). After
the end of the IVIG treatment, the fever temporarily improved.
However, the infant was injected with additional IVIG as a result
of a relapse of fever. The second IVIG treatment resulted in the
rapid improvement of the KD symptoms, decreased white blood cell
count (8,330 cells/µl), level of C-reactive protein (8.6 mg/dl),
quantity of brain natriuretic peptide (172 pg/ml) and recovered
left ventricular ejection fraction (60%). Therefore, the dose of
oral aspirin was reduced to 5 mg/kg/day (Fig. 1). The elevated blood platelet count
(625,000 platelets/µl) was then confirmed 7 days after the onset of
the disease (Table I).
 | Table I.Laboratory data during the
illness. |
Table I.
Laboratory data during the
illness.
|
| Days after fever
onset |
|---|
|
|
|
|---|
| Parameter | 6 | 9 | 13 |
|---|
| White blood cells
(cells/µl) |
12.11×103 |
8.33×103 |
8.62×103 |
| Neutrophils (%) | 65 | 40 | 26 |
| Hemoglobin
(g/dl) | 10.4 | 10.9 | 10.6 |
| Hematocrit (%) | 31.4 | 34 | 33.4 |
| Blood platelets
(platelets/µl) |
344×103 |
377×103 |
625×103 |
| Erythrocyte
sedimentation rate (mm/h) | 70 | >120 | 110 |
| C-reactive protein
(mg/dl) | 15.1 | 8.6 | 1.2 |
| Aspartate
aminotransferase (IU/l) | 49 | 36 | 35 |
| Alanine
aminotransferase (IU/l) | 39 | 21 | 12 |
| Brain natriuretic
peptide (pg/ml) | 403 | 172 | 23 |
Discussion
Concerns have been raised regarding vaccinations
being a potential risk factor leading to KD (6). Various types of vasculitis have been
observed and reported in temporal association with the
administration of certain vaccines (5).
Abrams et al (6) collected and analyzed data of children
surveyed from 1996 to 2006 from the Vaccine Safety Datalink
(https://www.cdc.gov/vaccinesafety/ensuringsafety/monitoring/vsd/publications.html),
and investigated the relevance of childhood vaccines and KD.
However, the authors found no evidence that any of the vaccinations
increased the risk of KD (6).
Conversely, Zafrir et al (7) demonstrated a possible link between the
influenza vaccination and autoimmunity, though the mechanism
underlying the development of influenza vaccine-induced
vasculitides remains unknown. As an activated immune system
following infectious or environmental stimulation contributes to
the development of KD, the influenza vaccination may serve as a
trigger for the development of KD (4).
Bonetto et al (5) reviewed the literature from 1994 to 2014
and reported that influenza vaccination was ranked first in the
number of published articles on vasculitis vaccine association
(according to vaccine type) and KD was placed third in the number
of published articles on vasculitis vaccine association (according
to vasculitis type) (5). Despite the
large number of reports, as well as published case reports and case
series, suggesting an association between vaccination and
vasculitis, the few observational and clinical trials investigating
associations between various vaccines and vasculitis subtypes have
failed to confirm such an association (5). However, there is increasing evidence
establishing various types of infections as potential triggers or
causes of different types of vasculitis (5). Hoffman et al (8) reported a potential association between
the hepatitis B (HBV) and hepatitis C (HCV) infections and
polyarteritis nodosa (PAN) and cryoglobulinemic vasculitis. In
France, a successful campaign for vaccination against HBV was
followed by a decrease in the incidence of PAN (9). Furthermore, emerging evidence has led to
the hypothesis that there is a potential role of infection in KD as
well (10). Therefore, the potential
of vaccination-induced vasculitis requires consideration in the
context of the decreased risk of infection-induced vasculitis
(5).
Post-HBV, post-yellow fever and post-influenza
vaccination KD have previously been reported (2–4). However,
a 2015 report on KD that was performed following vaccination for
influenza was, to the best of our knowledge, the only case reported
in Japan (4). The present study
describes the first case of KD following immunization for influenza
in South Korea and reviews previous studies on vasculitis following
vaccination and the causal association between them.
In conclusion, it may be hypothesized that influenza
vaccination is a trigger of KD when considering the timing of
vaccination and onset of KD, although the present study was unable
to demonstrate a direct relevance of the influenza vaccine to the
onset of KD.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
JSW analyzed and interpreted the patient data
including the laboratory finding and the pattern of fever. KDH made
tables and graph including patient's information. HMY searched and
analyzed references. CSH reviewed and revised about the manuscript.
YKL performed an echocardiogram and was a major contributor in
writing the manuscript. The final version of the manuscript has
been read and approved by all authors.
Ethics approval and consent to
participate
Informed consent for the publication of this case
report was waived as the infant's next of kin could not be
contacted despite numerous attempts to do so.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sundel RP and Petty RE: Kasawaki
diseaseTextbook of Pediatric Rheumatology. 6th. Classidy JT, Laxer
RM, Petty RE and Lindsley CB: Elsevier Saunders; Philadelphia: pp.
505–520. 2011, View Article : Google Scholar
|
|
2
|
Miron D, Fink D and Hashkes PJ: Kawasaki
disease in an infant following immunisation with hepatitis B
vaccine. Clin Rheumatol. 22:461–463. 2003. View Article : Google Scholar
|
|
3
|
Schmöeller D, Keiserman MW, Staub HL,
Velho FP and de Fátima Grohe M: Yellow fever vaccination and
Kawasaki disease. Pediatr Infect Dis J. 28:1037–1038. 2009.
View Article : Google Scholar
|
|
4
|
Shimada S, Watanabe T and Sato S: A
Patient with Kawasaki Disease Following Influenza Vaccinations.
Pediatr Infect Dis J. 34:9132015. View Article : Google Scholar
|
|
5
|
Bonetto C, Trotta F, Felicetti P, Alarcón
GS, Santuccio C, Bachtiar NS, Pernus YB, Chandler R, Girolomoni G,
Hadden RDM, et al: Vasculitis as an adverse event following
immunization-Systematic literature review. Vaccine. 2015.
|
|
6
|
Abrams JY, Weintraub ES, Baggs JM,
McCarthy NL, Schonberger LB, Lee GM, Klein NP, Belongia EA, Jackson
ML, Naleway AL, et al: Childhood vaccines and Kawasaki disease,
Vaccine Safety Datalink, 1996–2006. Vaccine. 33:382–387. 2015.
View Article : Google Scholar
|
|
7
|
Zafrir Y, Agmon-Levin N and Shoenfeld Y:
Post-influenza vaccination vasculitides: A possible new entity. J
Clin Rheumatol. 15:269–270. 2009. View Article : Google Scholar
|
|
8
|
Hoffman GS and Calabrese LH: Vasculitis:
Determinants of disease patterns. Nat Rev Rheumatol. 10:454–462.
2014. View Article : Google Scholar
|
|
9
|
Guillevin L: Infections in vasculitis.
Best Pract Res Clin Rheumatol. 27:19–31. 2013. View Article : Google Scholar
|
|
10
|
Principi N, Rigante D and Esposito S: The
role of infection in Kawasaki syndrome. J Infect. 67:1–10. 2013.
View Article : Google Scholar
|