Introduction
Contrast-induced nephropathy (CIN) is a common
adverse event observed in the diagnosis and treatment of coronary
intervention (1). Renal function
appears to deteriorate rapidly after the injection of an iodine
contrast agent. CIN was first described in the 1950s in case
reports of fatal acute renal failure that had occurred following
intravenous pyelography in patients with renal disease arising from
multiple myeloma (2). In the
majority of cases, CIN is considered non-oliguric acute renal
failure, with patients exhibiting asymptomatic transient decline in
renal function. As a result, CIN may go undetected by clinicians
who do not assess renal function in the days following contrast
administration (3). The generally
accepted definition of CIN is a 25% relative increase, or a 0.5
mg/dl (44 mmol/l) absolute increase, in Scr levels within 48-72 h
of contrast exposure, in the absence of an alternative explanation
(4). The rise in Scr levels peaks
after 3-5 days, and returns to baseline levels within 10-14 days
(5). Risk factors associated with
CIN include chronic kidney disease, contrast type and dose,
diabetes mellitus, route of administration (intravenous vs.
intra-arterial), congestive heart failure, age and use of
nonsteroidal anti-inflammatory drugs (6). CIN prolongs hospitalization time and
cost, and also worsens clinical symptoms, increases the incidence
of adverse events, and carries with it a heavy economic burden for
the patients and society (7). CIN is
observed in 6-15.7% of patients who undergo coronary angiography in
the setting of acute coronary syndrome (ACS) and contemporary
management (8). At present, the
pathogenesis of CIN is not fully understood, and there is no clear
treatment. Therefore, early recognition of high-risk groups is
particularly crucial for active prevention and treatment of CIN.
Although several scoring systems used to predict the risk of CIN
based on risk factors have been developed, identification of novel
biomarkers may also assist in identifying at risk patients.
Fibrinogen (FIB) or antithrombin III (AT-III) alone possess
relatively little value for predicting the risk of CIN; however,
the combination of the two factors has not been previously
explored, to the best of our knowledge. Therefore, the current
prospective study investigated the value of FIB combined with
AT-III for predicting the risk of CIN after percutaneous coronary
intervention (PCI).
Patients and methods
Patient population
All patients undergoing PCI admitted to The
Affiliated Hospital of Xuzhou Medical University (Xuzhou, China)
between October 2018 and May 2019 were prospectively enrolled in
the present study. The exclusion criteria were: i) Administration
of radio-contrast agents 48 h prior to the procedure or 72 h
post-procedure; ii) lack of data on pre-procedural or
post-procedural Scr levels; iii) administration of nonsteroidal
nephrotoxic drugs 48 h before or 72 h post-PCI; iv) chronic kidney
disease; v) patients with a malignant tumor, autoimmune disease,
those who had undergone surgery recently, or patients with a
history of trauma within the preceding month; vi) patients with a
pulmonary thromboembolism, venous thromboembolism or a history of
peripheral vascular disease; and vii) patients with infectious or
inflammatory diseases. The contrast agent used was the low-osmotic
and nonionic contrast agent iohexol, which was administered by
injection (Yangtze River Pharmaceutical Group); the osmotic
concentration was ~800 mOsm/Kg.
The final study population consisted of 394 patients
(242 men and 152 women). The ages of the patients ranged from 29-95
years, with a median age of 66 years. In the CIN group, the age
ranged from 42-95 years, with a median age of 67 years, including
29 men and 19 women. In the non-CIN group, the age ranged from
29-85 years, with a median age of 66 years, and consisted of 213
men and 119 women. Patients were hydrated using normal saline at a
rate of 1 ml/kg/h at the start of the procedure or just before the
procedure, and was continued for 12 h after the procedure ended.
For emergency coronary interventional procedures, physiological
(0.9%) saline was administered intravenously at a rate of 1 ml/kg/h
for 12 h following contrast exposure. Coronary angiography and PCI
were performed by interventional cardiologists, according to the
standard clinical practice using the radial or femoral approach
(9). All patients were administered
aspirin (loading dose, 300 mg) and clopidogrel (loading dose, 300
mg) or ticagrelor (180 mg) upon presentation, and were subsequently
administered a daily dose of aspirin (100 mg/day) and clopidogrel
(75 mg/day) or ticagrelor (90 mg/day). The study protocol was
performed in accordance with the Declaration of Helsinki (10) and was approved by the Ethics
Committee of the Affiliated Hospital of Xuzhou Medical University.
All patients provided written informed consent.
Diagnosis of CIN
CIN was defined as a Scr level that was 25% higher
than before intravenous injection of contrast media, or an absolute
value of 44.2 µmol/l (0.5 mg/dl) within 48 to 72 h, with other
causes of renal damage excluded (11). According to the changes of Scr
levels, patients were divided into a CIN group and non-CIN
group.
Data collection
For all patients, the demographic characteristics,
medical history, and variables related to the procedure were
recorded. Routine laboratory data before and after the PCI
procedures included routine tests of blood, liver and kidney
function, as well as measurements of serum lipids, glucose, FIB and
AT-III levels, amongst others.
All Scr levels were measured in a biochemical
laboratory at the hospital using an Olympus AU2700 automatic
biochemical analyzer (Olympus Corporation).
FIB and AT-III were measured using a Sysmex CA-7000
automatic coagulation analyzer and the analyzers original matching
reagent (JEOL, Ltd.).
The estimated glomerular filtration rate was
calculated using a modification of diet in renal disease equation
for patients as follows: GFR (ml/min/1.73 m2)=186 x Scr
(mg/dl)-1.154 x age (years)-0.203 x (0.742 if
female) (12).
Statistical analysis
All statistical analyses were performed using SPSS
version 21.0 (IBM Corp.). For normally distributed data, continuous
variables are shown as the mean ± the standard deviation.
Otherwise, the median and interquartile range (25-75% values) are
displayed, and non-parametric tests were used for analysis.
Categorical variables are shown as the number and percentage (%),
and were compared using a χ2 test or Fisher's exact
test. Comparison of parametric values between two groups was
performed using an independent-samples Student's t-test.
Comparisons of nonparametric values between two groups were
compared using a Mann-Whitney U-test. Receiver operating
characteristic (ROC) curve analysis was used to determine the
optimal cut-off values of FIB and AT-III levels for detection of
CIN using MedCalc version 19.06.6 (MedCalc Software byba). Multiple
logistical regression analysis was used to identify independent
risk factors of CIN. P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline clinical characteristics and
laboratory findings of the patients
The recruited cohort consisted of 394 patients
receiving PCI with a mean age of 64.4±11.1 years, and 242 patients
(61.4%) were men. A total of 48 (12.2%) patients developed CIN. The
univariate analysis of the clinicopathological characteristics and
the baseline of the assessed parameters, including the conventional
risk factors for CIN between the patients with and without CIN are
shown in Table I. Distribution of
sexes, hypertension and smoking status did not differ significantly
between thew two groups. Additionally, there were no significant
differences observed between the CIN and the non-CIN groups
regarding the use of antihypertensive, antiplatelet or
anti-ischemic, lipid-lowering drugs, or oral antidiabetic drugs.
The average dose of contrast media in the CIN group was
significantly larger than the dose administered in the non-CIN
group (P=0.024).
 | Table IBaseline clinical characteristics of
the CIN and non-CIN groups. |
Table I
Baseline clinical characteristics of
the CIN and non-CIN groups.
| Variables | Non-CIN, n=346 | CIN, n=48 | P-value |
|---|
| Age, years | 64.17±10.95 | 66.44±11.72 | 0.182 |
| Sex, male, n (%) | 213 (61.6) | 29 (60.4) | 0.879 |
| Smoker, n (%) | 114 (32.9) | 20 (41.7) | 0.234 |
| hypertension, n
(%) | 199 (57.5) | 27 (56.3) | 0.868 |
| Diabetes, n (%) | 82 (23.7) | 12 (25.0) | 0.843 |
| Body mass index,
kg/m2 | 25.88±3.34 | 25.29±4.19 | 0.268 |
| Systolic blood
pressure, mmHg | 133.14±19.47 | 131.33±24.54 | 0.626 |
| Diastolic blood
pressure, mmHg | 78.55±11.70 | 79.42±14.86 | 0.700 |
| Contrast media,
ml | 112.67±43.09 | 127.50±37.27 | 0.024a |
| AMI, n (%) | 108 (31.2) | 23 (47.9) | 0.021a |
| Medication |
|
β-blocker, n
(%) | 288 (83.2) | 40 (83.3) | 0.987 |
|
ACEI/ARB, n
(%) | 193 (55.8) | 25 (52.1) | 0.629 |
|
CCB, n
(%) | 94 (27.2) | 13 (27.1) | 0.990 |
|
Diuretics, n
(%) | 118 (34.1) | 25 (52.1) | 0.015a |
|
Statin, n
(%) | 319 (92.2) | 46 (95.8) | 0.366 |
|
LMWH, n
(%) | 154 (44.5) | 32 (66.7) | 0.004b |
|
Nitrates, n
(%) | 221 (63.9) | 31 (64.6) | 0.923 |
Patients who developed CIN were likely to exhibit
higher levels of FIB (P=0.001) and lower AT-III activity
(P<0.001). Furthermore, these patients with CIN were likely to
exhibit lower albumin levels (P<0.001). Patients who experienced
a myocardial infarction were more likely to develop CIN (P=0.021).
In the CIN group, the diuretic (P=0.015) and low molecular weight
heparin usage (P=0.004) was significantly more common. The results
of laboratory analysis are presented in Table II.
 | Table IILaboratory results of the CIN and
non-CIN groups. |
Table II
Laboratory results of the CIN and
non-CIN groups.
| A,
Pre-operative |
|---|
| Variables | Non-CIN,
n=348a | CIN,
n=49a | P-value |
|---|
| Triglyceride,
mmol/l | 1.35
(1.01-1.91) | 1.26
(0.95-1.52) | 0.204 |
| Total cholesterol,
mmol/l | 4.43±1.18 | 4.28±1.07 | 0.44 |
| High-density
lipoprotein, mmol/l | 1.12
(0.95-1.32) | 1.13
(0.98-1.36) | 0.72 |
| Low-density
lipoprotein, mmol/l | 2.70±1.00 | 2.59±0.79 | 0.563 |
| Albumin, g/l | 42.79±4.47 | 39.33±3.93 |
<0.001b |
| Glucose,
mmol/l | 6.71±2.58 | 7.15±3.02 | 0.301 |
| Fibrinogen,
g/l | 2.90
(2.42-3.35) | 3.23
(2.80-3.80) | 0.001b |
| Antithrombin III,
% | 91.54±11.73 | 83.65±10.93 |
<0.001b |
| NLR | 2.99
(2.05-5.03) | 3.29
(2.41-5.85) | 0.305 |
| PLR | 139.00
(105.63-179.00) | 146.32
(112.31-191.67) | 0.163 |
| Serum creatinine,
µmol/l | 67.00
(57.00-78.25) | 67.00
(54.00-75.50) | 0.299 |
| Cystatin C,
mg/l | 0.78
(0.71-0.91) | 0.81
(0.71-0.88) | 0.985 |
| Uric acid,
µmol/l | 306.50
(248.00-365.00) | 296.50
(258.00-349.75) | 0.513 |
| eGFR, ml/min | 101.84±24.19 | 107.04±34.23 | 0.313 |
| B,
Post-operative |
| Serum creatinine,
µmol/l | 67.00
(57.00-78.00) | 87.00
(73.75-102.5) |
<0.001b |
| Cystatin C,
mg/l | 0.74
(0.67-0.86) | 0.84
(0.74-1.08) |
<0.001b |
| Uric acid,
µmol/l | 280.00
(222.75-353.25) | 332.00
(268.00-411.50) | 0.001 |
| eGFR, ml/min | 101.05±25.98 | 75.54±25.04 |
<0.001b |
Multiple logistical regression
analysis of risk factors for CIN
Multiple logistical regression analysis included the
following factors: Acute myocardial infarction, albumin, contrast
media volume, FIB, AT-III, and diuretic and low molecular weight
heparin usage. Multivariate analyses indicated that albumin [odds
ratio (OR), 0.893; 95% confidence intervals (CI), 0.815-0.978;
P=0.015), FIB (OR, 1.613; 95% CI, 1.127-2.306; P=0.009) and AT-III
(OR, 0.946; 95% CI, 0.916-0.977; P=0.001), were independent
predictors for CIN (Table
III).
 | Table IIIMultiple logistical regression
analysis of risk factors for CIN. |
Table III
Multiple logistical regression
analysis of risk factors for CIN.
| Variables | B | SE | Wald-value | P-value | Odds ratio | 95% confidence
intervals |
|---|
| Albumin | -0.114 | 0.047 | 5.958 | 0.015a | 0.893 | 0.815-0.978 |
| AT-III | -0.055 | 0.016 | 11.332 | 0.001b | 0.946 | 0.916-0.977 |
| FIB | 0.478 | 0.183 | 6.848 | 0.009b | 1.613 | 1.127-2.306 |
| Contrast media | 0.006 | 0.004 | 2.238 | 0.135 | 1.006 | 0.998-1.015 |
| AMI | 0.223 | 0.391 | 0.327 | 0.568 | 1.250 | 0.581-2.690 |
| Diuretic | -0.168 | 0.358 | 0.220 | 0.639 | 0.845 | 0.419-1.705 |
| LMWH | -0.553 | 0.379 | 2.134 | 0.144 | 0.575 | 0.274-1.208 |
Value of FIB and AT-III in predicting
CIN
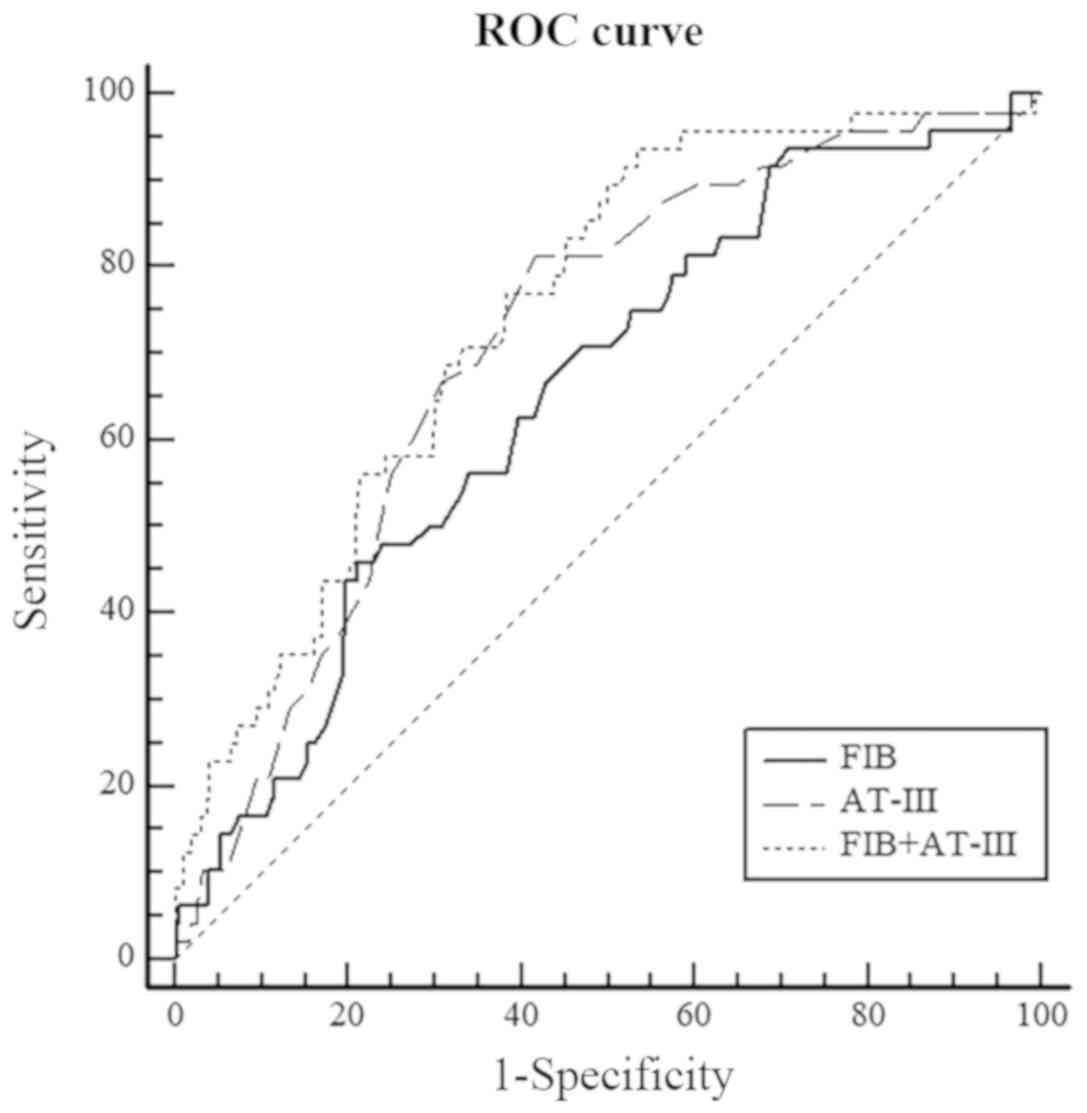
Regarding FIB, the area under the ROC curve (AUC)
for predicting CIN was 0.653. The optimal cut-off value was 3.48
g/l with a sensitivity of 45.8% and specificity of 79.7% (95% CI,
0.603-0.701; P=0.0002). For AT-III, the AUC was 0.711, and the
optimal cut-off value was 89.5% with a sensitivity of 81.3% and
specificity of 58.2% (95% CI, 0.659-0.758; P<0.001). FIB and
AT-III were incorporated into the CIN risk factor regression
analysis. The probability of the combination of FIB and AT-III
predicting the occurrence of CIN was: Logit (P)=2.059+0.600
FIB-0.066 AT-III. The optimal cut-off value for the combination was
calculated; when the predicted incidence of CIN was higher than
0.090424, patients were more likely to exhibit CIN following PCI.
When combining FIB and AT-III, the AUC was 0.747. The optimal
cut-off value was 0.090424, with a diagnostic sensitivity of 93.8%
and specificity of 46.6% (95% CI, 0.697-0.792; P<0.001). FIB
combined with AT-III exhibited improved predictive accuracy in of
CIN (FIB vs. AT-III, AUC=0.653 vs. 0.711, P=0.292; FIB vs. FIB +
AT-III, AUC=0.653 vs. 0.747, P=0.012; AT-III vs. FIB + AT-III,
AUC=0.711 vs. 0.747, P=0.138). The results of ROC analysis are
presented in Table IV and Fig. 1.
 | Table IVPredictive values of FIB and AT-III
for CIN based on the receiver operating characteristic curves. |
Table IV
Predictive values of FIB and AT-III
for CIN based on the receiver operating characteristic curves.
| Variables | AUC | P-value | 95% CI | Sensitivity
(%) | Specificity
(%) | Cut-off value |
|---|
| FIB | 0.653 | 0.0002a | 0.603-0.701 | 45.8 | 79.7 | 3.48 g/l |
| AT-III | 0.711 |
<0.0001a | 0.659-0.758 | 81.3 | 58.2 | 89.5% |
| FIB + AT-III | 0.747 |
<0.0001a | 0.697-0.792 | 93.8 | 46.6 | 0.090424 |
Discussion
The present study demonstrated that FIB, AT-III and
albumin were independent predictors of CIN in patients undergoing
PCI. Based on the results of the present study, the risk of CIN
increased as the level of FIB increased or the activity of AT-III
decreased. This study also suggested that the combination of FIB
and AT-III was a better predictor of CIN after PCI.
With the increasing number of interventional
procedures available, more patients will inevitably be assessed
using iodine contrast agents as interventional procedures require
its use, and these contrast reagents are associated with an
increased risk of acute kidney injury (13). CIN results in a rapid decline of
kidney function after administration of iodinated contrast material
(14). CIN is one of the most common
causes of hospitalization in patients with acquired kidney injury,
and is known to increase the rates of morbidity and mortality,
increase the costs of health care, as well as prolong the duration
of hospitalization (15). At
present, there are no specific treatment options for CIN (16). Therefore, early identification and
intervention of patients with a high risk of experiencing CIN
clinical events, is of great significance for improving patient
outcomes.
FIB is a serum glycoprotein synthesized by
hepatocytes. It is a major plasma coagulation factor and serves an
important role in the inflammatory process (17). Increased levels of FIB result in an
increase in blood viscosity, leading to shear stress damage in
endothelial cells (18). Studies
have shown that FIB in tissues is significantly elevated in acute
kidney injury caused by ischemia-reperfusion (19-21).
FIB causes severe renal dysfunction by increasing renal fibrosis
(22).
Numerous previous studies have shown that serum FIB
levels are associated with cardiovascular risk factors or
cardiovascular events (23-26).
Furthermore, FIB is associated with acute kidney injury (27), and studies have shown that FIB levels
in tissues are significantly elevated in ischemia-induced acute
renal injury caused by ischemia-reperfusion (22). FIB is an important regulator of
coagulation, inflammation, wound healing and angiogenesis, and
functions by interacting with blood cells, endothelial cells and
other types of cells (28).
Additionally, FIB is an acute-phase protein and a marker of
inflammation, as it is induced by cytokines, such as interleukin-6
(29,30); thus, its expression is increased
during inflammation. Inflammation is one of the primary mechanisms
involved in the pathogenesis of CIN (31). Neutrophil-to-lymphocyte ratio (NLR)
and platelet-to-lymphocyte ratio (PLR) are common inflammatory
markers. However, this difference was not significant. In addition,
the increased levels of FIB may have increased blood viscosity,
leading to insufficient perfusion of the kidney, and thus may
increase the risk of CIN.
AT-III is the most important type of antithrombin,
and its activity is often used as a laboratory indicator for
judging anticoagulant levels and detection of thrombotic diseases
(32). AT-III not only exhibited a
strong anticoagulant effect, but also a strong anti-inflammatory
effect. Thus AT-III levels may serve as a prognostic biomarker in
neonatal sepsis, where a marked decrease in the levels of AT-III
levels in septic neonates is observed (33). The decrease in the levels of AT-III
is predictive of a poor outcome in sepsis (34). Furthermore, several studies have
shown that AT-III exhibits a protective effect on contrast CIN
(35). Previously, a study showed
that patients with low levels of AT-III activity presented a high
risk of developing acute kidney injury after cardiac surgery.
Insufficiency of endogenous AT-III exacerbated the renal
ischemia/reperfusion injury in rats (36). However, administration of exogenous
AT-III may exhibit a protective effect against CIN through its
anti-inflammatory and antioxidant effects, as well as by improving
renal blood flow (35). The levels
of AT-III were associated with the severity of coronary artery
stenosis (37). Previous studies
suggested that in patients with coronary artery disease, AT-III
activity was closely associated with a hypercoagulable state or
thrombosis. Additionally, the decrease in AT-III activity may
indicate acute coronary events, and the extent of the decrease in
activity level was positively correlated with the degree of
coronary stenosis (25,38-40).
However, to the best of our knowledge, there are no
studies that have explored the value of combining FBI and AT-III to
predict CIN. In the present study, it was shown that the
combination of these two biomarkers exhibited improved predictive
value for CIN. Additionally, a higher level of FIB was positively
associated with the risk of CIN. In contrast to FIB, AT-III
activity was a protective factor against CIN.
The present study has several limitations. First,
the follow-up assessment of renal function was 1-3 days after PCI;
therefore, a later increase in Scr levels in certain patients who
did exhibit deteriorated renal function within 48 h of the
procedure may have been missed. This oversight may result in a
slight underestimation of CIN. Second, the number of enrolled
patients was relatively small, particularly regarding patients with
low AT-III activity levels, and all the patients recruited were
from a single health care institution, and thus, a selection bias
during enrollment was inevitable. In future studies, larger cohorts
from multiple centers should be used to confirm the validity of the
results presented.
In conclusion, the present study demonstrated that
3.48 g/l was the optimal cut-off value of preoperative FIB, and
89.5% was the optimal cut-off value of preoperative AT-III, which
were effective predictors of CIN following PCI. Furthermore, the
combination of FIB and AT-III was a better predictor of a high risk
of CIN compared with FIB alone. These results may provide a simple
and easy indicator for use in predicting the risk of CIN.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YS designed the study and drafted the manuscript. DZ
collected the data. QZ analyzed the data. WL designed the study,
analyzed data and edited the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was performed in accordance with
the Declaration of Helsinki and was approved by the Ethics
Committee of the Affiliated Hospital of Xuzhou Medical University
(Xuzhou, China). All patients provided written informed
consent.
Patient consent for publication
All patients signed informed consent approved by the
Institutional Review Board of the Affiliated Hospital of Xuzhou
Medical University.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mamoulakis C, Tsarouhas K, Fragkiadoulaki
I, Heretis I, Wilks MF, Spandidos DA, Tsitsimpikou C and Tsatsakis
A: Contrast-induced nephropathy: Basic concepts, pathophysiological
implications and prevention strategies. Pharmacol Ther. 180:99–112.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Katzberg RW and Haller C: Contrast-induced
nephrotoxicity: Clinical landscape. Kidney Int Suppl.
(S3-S7)2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Andreucci M, Faga T, Pisani A, Sabbatini
M, Russo D and Michael A: Prevention of contrast-induced
nephropathy through a knowledge of its pathogenesis and risk
factors. ScientificWorldJournal. 2014(823169)2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Morcos SK and Thomsen HS: European Society
of Urogenital Radiology: European society of urogenital radiology
guidelines on administering contrast media. Abdom Imaging.
28:187–190. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Andreucci M, Solomon R and Tasanarong A:
Side effects of radiographic contrast media: Pathogenesis, risk
factors, and prevention. Biomed Res Int.
2014(741018)2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Moos SI, van Vemde DN, Stoker J and Bipat
S: Contrast induced nephropathy in patients undergoing intravenous
(IV) contrast enhanced computed tomography (CECT) and the
relationship with risk factors: A meta-analysis. Eur J Radiol.
82(e387-e399)2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
McCullough PA, Adam A, Becker CR, Davidson
C, Lameire N, Stacul F and Tumlin J: CIN Consensus Working Panel.
Epidemiology and prognostic implications of contrast-induced
nephropathy. Am J Cardiol. 98(5K-13K)2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Guillon B, Ecarnot F, Marcucci C, Ducloux
D, Chatot M, Badoz M, Bonnet B, Chopard R, Frey P, Meneveau N and
Schiele F: Incidence, predictors, and impact on six-month mortality
of three different definitions of contrast-induced acute kidney
injury after coronary angiography. Am J Cardiol. 121:818–824. 2018.
View Article : Google Scholar
|
|
9
|
Gilchrist IC, Awuor SO, Davies RE and
Ukaigwe AC: Controversies in complex percutaneous coronary
intervention: Radial versus femoral. Expert Rev Cardiovasc Ther.
15:695–704. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
General Assembly of the World Medical
Association. World medical association declaration of Helsinki:
Ethical principles for medical research involving human subjects. J
Am Coll Dent. 81:14–18. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Rear R, Bell RM and Hausenloy DJ:
Contrast-induced nephropathy following angiography and cardiac
interventions. Heart. 102:638–648. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Levey AS, Bosch JP, Lewis JB, Greene T,
Rogers N and Roth D: A more accurate method to estimate glomerular
filtration rate from serum creatinine: A new prediction equation.
Modification of diet in renal disease study group. Ann Intern Med.
130:461–470. 1999.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Muñoz de Bustillo Llorente E and de Miguel
Balsa E: Radiological iodinated contrast-induced nephropathy. Rev
Clin Esp. 219:403–410. 2019.(In English, Spanish).
|
|
14
|
Azzalini L, Spagnoli V and Ly HQ:
Contrast-induced nephropathy: From pathophysiology to preventive
strategies. Can J Cardiol. 32:247–255. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gosling R and Iqbal J: Predicting contrast
induced nephropathy in patients undergoing percutaneous coronary
intervention. J Thorac Dis. 11:2672–2674. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fähling M, Seeliger E, Patzak A and
Persson PB: Understanding and preventing contrast-induced acute
kidney injury. Nat Rev Nephrol. 13:169–180. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Fibrinogen Studies C, Danesh J, Lewington
S, Thompson SG, Lowe GD, Collins R, Kostis JB, Wilson AC, Folsom
AR, Wu K, et al: Plasma fibrinogen level and the risk of major
cardiovascular diseases and nonvascular mortality: An individual
participant meta-analysis. JAMA. 294:1799–1809. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lowe GD, Fowkes FG, Dawes J, Donnan PT,
Lennie SE and Housley E: Blood viscosity, fibrinogen, and
activation of coagulation and leukocytes in peripheral arterial
disease and the normal population in the Edinburgh artery study.
Circulation. 87:1915–1920. 1993.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Druid H, Nilsson I, Rammer L and Skude G:
Effect of anticoagulation on renal function and protein excretion
in experimental acute ischemic renal failure. Ren Fail. 21:647–657.
1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sörensen-Zender I, Rong S, Susnik N, Lange
J, Gueler F, Degen JL, Melk A, Haller H and Schmitt R: Role of
fibrinogen in acute ischemic kidney injury. Am J Physiol Renal
Physiol. 305(F777-F785)2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Huang MJ, Wei RB, Su TY, Wang Y, Li QP,
Yang X, Lv XM and Chen XM: Impact of acute kidney injury on
coagulation in adult minimal change nephropathy. Medicine
(Baltimore). 95(e5366)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Krishnamoorthy A, Ajay AK, Hoffmann D, Kim
TM, Ramirez V, Campanholle G, Bobadilla NA, Waikar SS and Vaidya
VS: Fibrinogen β-derived Bβ(15-42) peptide protects against kidney
ischemia/reperfusion injury. Blood. 118:1934–1942. 2011.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mayosi BM, Keavney BD, Watkins HC, Vickers
MA and Green FR: Quantitative genetic study of plasma fibrinogen
level and the-455 G/A polymorphism of the beta-fibrinogen gene
using novel family-based association methods. Circulation.
102(104)2000.
|
|
24
|
Carty CL, Cushman M, Jones D, Lange LA,
Hindorff LA, Rice K, Jenny NS, Durda JP, Walston J, Carlson CS, et
al: Associations between common fibrinogen gene polymorphisms and
cardiovascular disease in older adults. The cardiovascular health
study. Thromb Haemost. 99:388–395. 2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Thompson SG, Fechtrup C, Squire E, Heyse
U, Breithardt G, van de Loo JC and Kienast J: Antithrombin III and
fibrinogen as predictors of cardiac events in patients with angina
pectoris. Arterioscl Throm Vas. 16:357–362. 1996.PubMed/NCBI View Article : Google Scholar
|
|
26
|
De Luca G, Verdoia M, Cassetti E, Schaffer
A, Cavallino C and Bolzani V: Novara Atherosclerosis Study Group
(NAS). High fibrinogen level is an independent predictor of
presence and extent of coronary artery disease among Italian
population. J Thromb Thrombolysis. 31:458–463. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Docherty NG and Godson C: Fibrinogen as a
damage-associated mitogenic signal for the renal fibroblast. Kidney
Int. 80:1014–1016. 2011.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Laurens N, Koolwijk P and De Maat MP:
Fibrin structure and wound healing. J Thromb Haemost. 4:932–939.
2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kerr R, Stirling D and Ludlam CA:
Interleukin 6 and haemostasis. Brit J Haematol. 115:3–12.
2001.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Szaba FM and Smiley ST: Roles for thrombin
and fibrin(ogen) in cytokine/chemokine production and macrophage
adhesion in vivo. Blood. 99:1053–1059. 2002.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hossain MA, Costanzo E, Cosentino J, Patel
C, Qaisar H, Singh V, Khan T, Cheng JS, Asif A and Vachharajani TJ:
Contrast-induced nephropathy: Pathophysiology, risk factors, and
prevention. Saudi J Kidney Dis Transpl. 29:1–9. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Meng R, Li ZY, Ji X, Ding Y, Meng S and
Wang X: Antithrombin III associated with fibrinogen predicts the
risk of cerebral ischemic stroke. Clin Neurol Neurosur.
113:380–386. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ersoy B, Nehir H, Altinoz S, Yilmaz O,
Dundar PE and Aydogan A: Prognostic value of initial antithrombin
levels in neonatal sepsis. Indian Pediatr. 44:581–584.
2007.PubMed/NCBI
|
|
34
|
Samra N, AlGhwass M, Elgawhary S, Hassan
M, Bekhit O, Mohamed W and Eid M: Serum level of antithrombin III
(ATIII) could serve as a prognostic biomarker in neonatal sepsis.
Fetal Pediatr Pathol. 38:290–298. 2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Lu Z, Cheng D, Yin J, Wu R, Zhang G, Zhao
Q, Wang N, Wang F and Liang M: Antithrombin III protects against
contrast-induced nephropathy. EBioMedicine. 17:101–107.
2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wang F, Zhang G, Lu Z, Geurts AM, Usa K,
Jacob HJ, Cowley AW, Wang N and Liang M: Antithrombin III/SerpinC1
insufficiency exacerbates renal ischemia/reperfusion injury. Kidney
Int. 88:796–803. 2015. View Article : Google Scholar
|
|
37
|
Lu J, Niu D, Zheng D, Zhang Q and Li W:
Predictive value of combining the level of lipoprotein-associated
phospholipase A2 and antithrombin III for acute coronary syndrome
risk. Biomed Rep. 9:517–522. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Lipets EN and Ataullakhanov FI: Global
assays of hemostasis in the diagnostics of hypercoagulation and
evaluation of thrombosis risk. Thromb J. 13(4)2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Brummel-Ziedins K, Undas A, Orfeo T,
Gissel M, Butenas S, Zmudka K and Mann KG: Thrombin generation in
acute coronary syndrome and stable coronary artery disease:
Dependence on plasma factor composition. J Thromb Haemost.
6:104–110. 2008.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hong X, Shan PR, Hu L, Huang ZQ, Wu GJ,
Xiao FY and Huang WJ: Relationship between antithrombin-III value
with acute coronary syndrome and preprocedural TIMI flow grade.
Zhonghua Yi Xue Za Zhi. 92:831–834. 2012.PubMed/NCBI(In Chinese).
|