|
1
|
Galanello R and Origa R: Beta-thalassemia.
Orphanet J Rare Dis. 5(11)2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
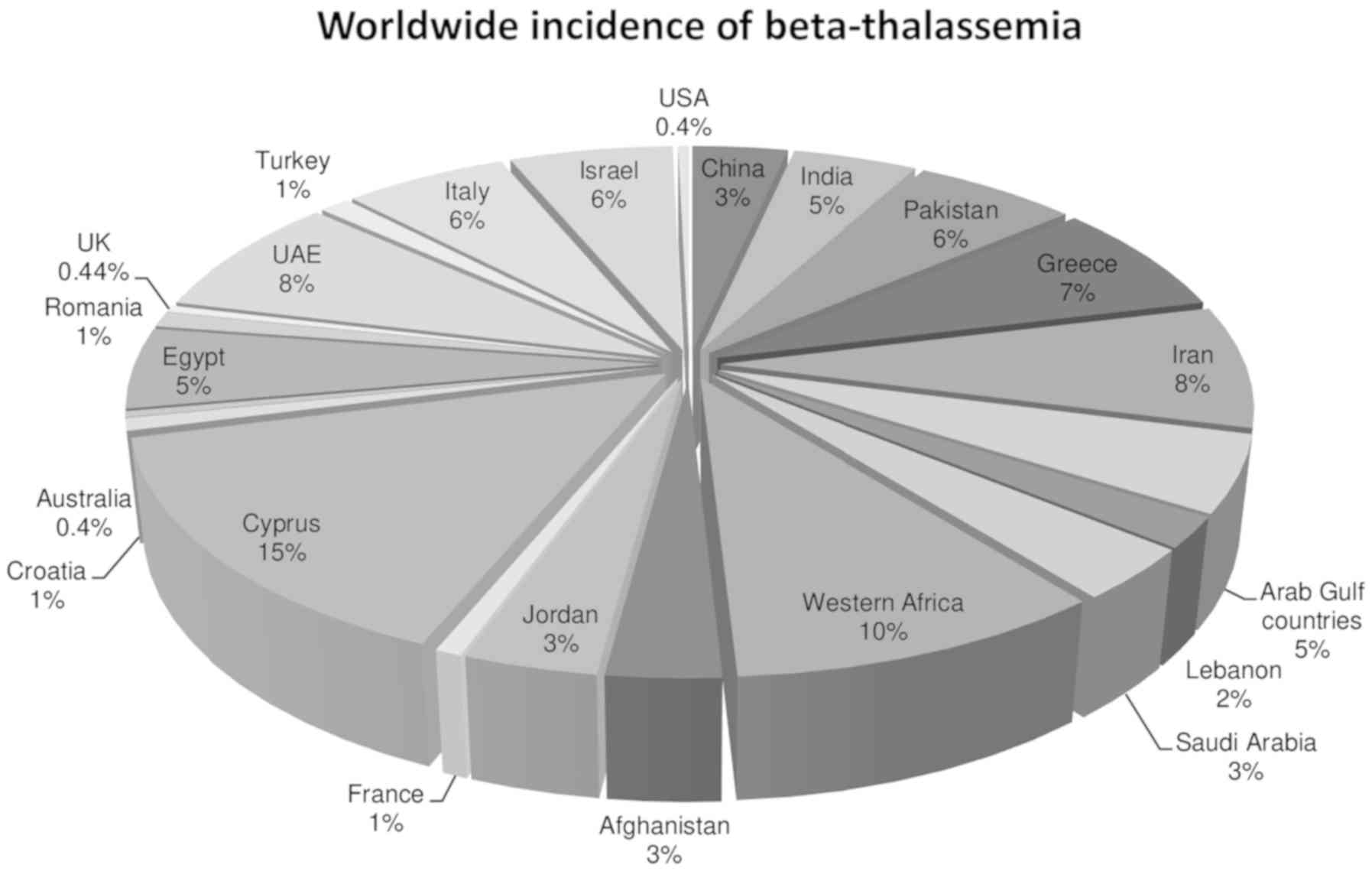
De Sanctis V, Kattamis C, Canatan D,
Soliman AT, Elsedfy H, Karimi M, Daar S, Wali Y, Yassin M, Soliman
N, et al: β-Thalassemia distribution in the old world: An ancient
disease seen from a historical standpoint. Mediterr J Hematol
Infect Dis. 9(e2017018)2017.PubMed/NCBI View Article : Google Scholar
|
|
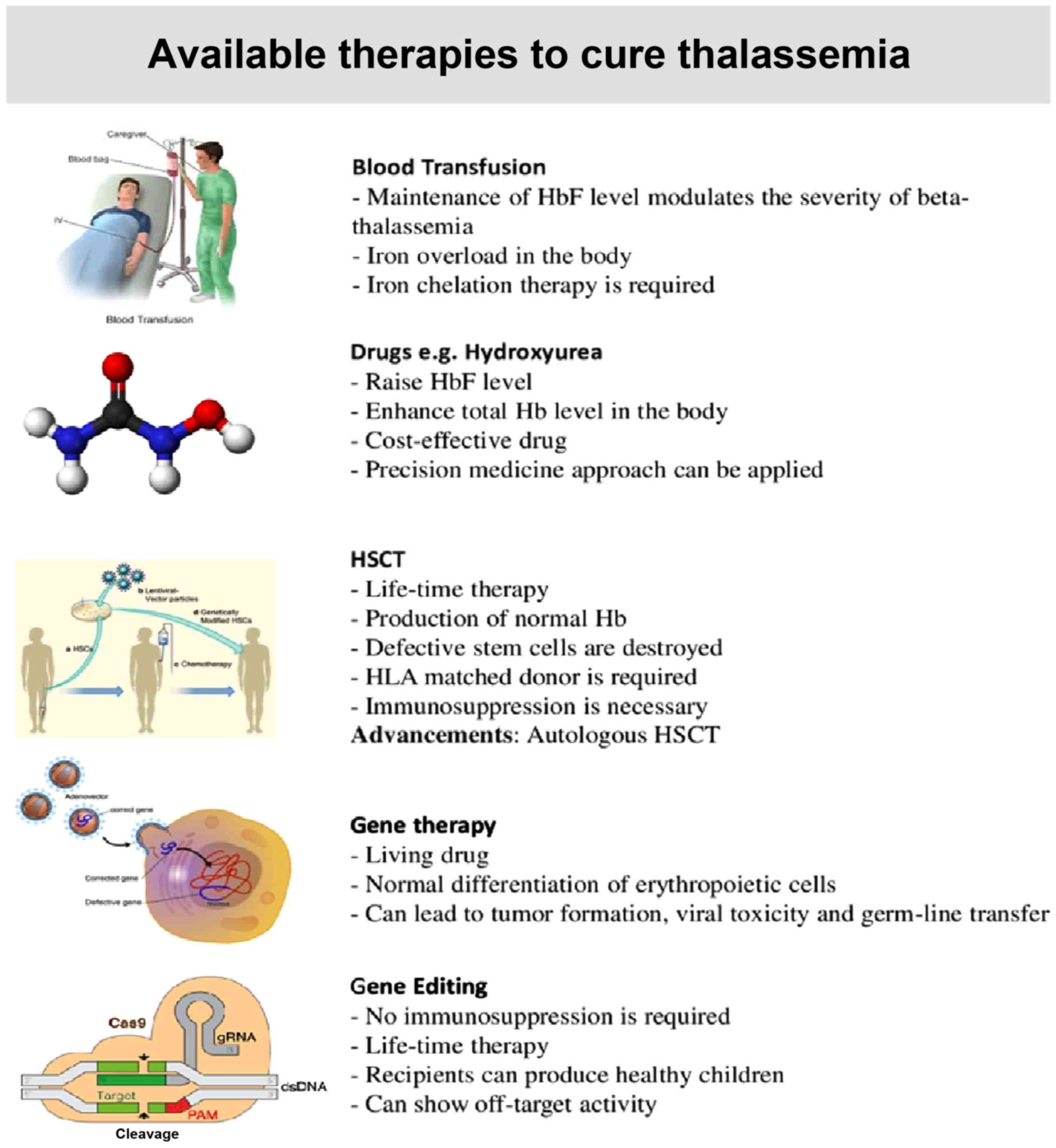
3
|
Haldane JBS: The rate of mutation of human
genes. Hereditas. 35:267–273. 1949.
|
|
4
|
Saeed U and Piracha ZZ: Thalassemia:
Impact of consanguineous marriages on most prevalent monogenic
disorders of humans. Asian Pacific J Tropical Dis. 6:837–840.
2016.
|
|
5
|
Hu L, Shang X, Yi S, Cai R, Li Z, Liu C,
Liang Y, Cai D, Zhang F and Xu X: Two novel copy number variations
involving the α-globin gene cluster on chromosome 16 cause
thalassemia in two Chinese families. Mol Genet Genomics.
291:1443–1450. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Muncie HL Jr and Campbell JS: Alpha and
beta thalassemia. Am Fam Physician. 80:339–344. 2009.PubMed/NCBI
|
|
7
|
Martin A and Thompson AA: Thalassemias.
Pediatr Clin North Am. 60:1383–1391. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Galanello R and Cao A: Alpha-thalassemia.
Genet Med. 13(83)2011.
|
|
9
|
Borgio JF, AbdulAzeez S, Al-Nafie AN,
Naserullah ZA, Al-Jarrash S, Al-Madan MS, Al-Muhanna F, Steinberg
MH and Al-Ali AK: A novel HBA2 gene conversion in cis or trans:
‘α12 allele’ in a Saudi population. Blood Cells Mol Dis.
53:199–203. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
AbdulAzeez S, Almandil NB, Naserullah ZA,
Al-Jarrash S, Al-Suliman AM, ElFakharay HI and Borgio JF:
Co-inheritance of alpha globin gene deletion lowering serum iron
level in female beta thalassemia patients. Mol Biol Rep.
47:603–606. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Haghpanah S, Vahdati S and Karimi M:
Comparison of quality of life in patients with β-Thalassemia
intermedia and β-thalassemia major in Southern Iran. Hemoglobin.
41:169–174. 2017.PubMed/NCBI View Article : Google Scholar
|
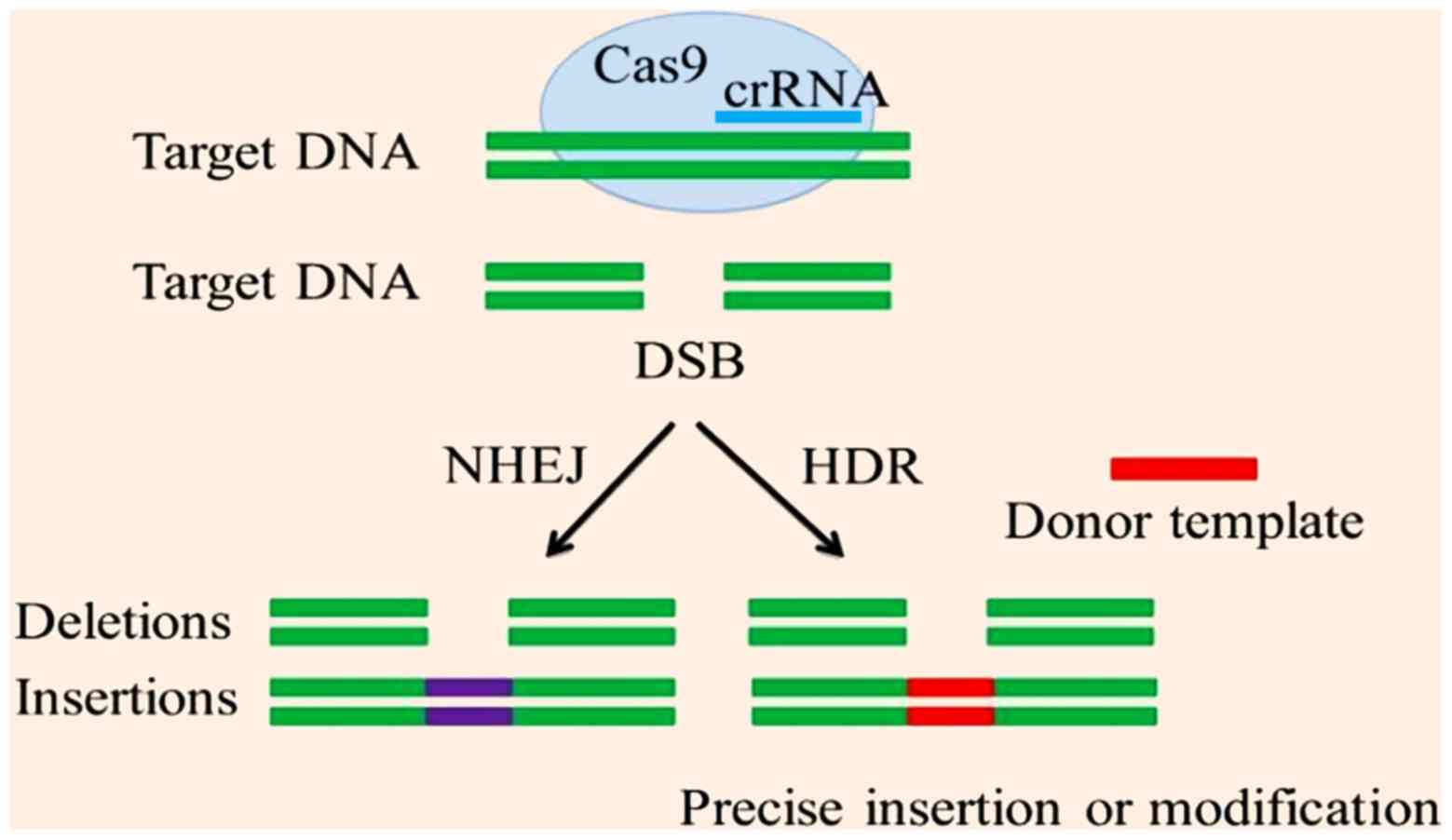
|
12
|
Choudhry VP: Thalassemia minor and major:
Current management. Indian J Pediatr. 84:607–611. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Thein SL: The molecular basis of
β-thalassemia. Cold Spring Harb Perspect Med.
3(a011700)2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Musallam K, Cappellini MD and Taher A:
Challenges associated with prolonged survival of patients with
thalassemia: Transitioning from childhood to adulthood. Pediatrics.
121:e1426–e1429. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ishfaq K, Naeem SB and Ali J:
Socio-economic factors of thalassemia major on Patients 'families:
A case study of the Children's hospital and the institute of child
health Multan, Pakistan. Int J Med Appl Health. 1:2013.
|
|
16
|
Goodnough LT, Brecher ME, Kanter MH and
AuBuchon JP: Transfusion medicine-blood transfusion. N Engl J Med.
340:438–447. 1999.
|
|
17
|
Brittenham GM: Iron-chelating therapy for
transfusional iron overload. N Engl J Med. 364:146–156.
2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Borgna-Pignatti C, Rugolotto S, De Stefano
P, Zhao H, Cappellini MD, Del Vecchio GC, Romeo MA, Forni GL,
Gamberini MR, Ghilardi R, et al: Survival and complications in
patients with thalassemia major treated with transfusion and
deferoxamine. Haematologica. 89:1187–1193. 2004.PubMed/NCBI
|
|
19
|
Low LC: Growth of children with
β-thalassemia major. Indian J Pediatr. 72:159–164. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wu K, Tsai F and Peng C: Growth hormone
(GH) deficiency in patients with β-thalassemia major and the
efficacy of recombinant GH treatment. Ann Hematol. 82:637–640.
2003.PubMed/NCBI View Article : Google Scholar
|
|
21
|
de Dreuzy E, Bhukhai K, Leboulch P and
Payen E: Current and future alternative therapies for
beta-thalassemia major. Biomed J. 39:24–38. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
de Montalembert M, Ribeil JA, Brousse V,
Guerci-Bresler A, Stamatoullas A, Vannier JP, Dumesnil C, Lahary A,
Touati M, Bouabdallah K, et al: Cardiac iron overload in
chronically transfused patients with thalassemia, sickle cell
anemia, or myelodysplastic syndrome. PLoS One.
12(e0172147)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wang M, Liu R, Liang Y, Yang G, Huang Y,
Yu C, Sun K, Lai Y and Xia Y: Iron overload correlates with serum
liver fibrotic markers and liver dysfunction: Potential new methods
to predict iron overload-related liver fibrosis in thalassemia
patients. United European Gastroenterol J. 5:94–103.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Iqbal A, Ansari SH, Parveen S, Khan IA,
Siddiqui AJ and Musharraf SG: Hydroxyurea treated β-thalassemia
children demonstrate a shift in metabolism towards healthy pattern.
Sci Rep. 8(15152)2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Pilo F and Angelucci E: Iron toxicity and
hemopoietic cell transplantation: Time to change the paradigm.
Mediterr J Hematol Infect Dis. 11(e2019030)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Anurathapan U, Locatelli F, Kwiatkowski
JL, Rasko JEJ, Schiller GJ, Porter J, Sauer MG, Thrasher AJ,
Chabannon C, Elliot H, et al: Lentiglobin gene therapy for
transfusion-dependent β-thalassemia: Outcomes from the phase 1/2
Northstar and phase 3 Northstar-2 studies. Biol Blood Marrow
Transplantation. 25 (Suppl):S66–S67. 2019.
|
|
27
|
Ribeil JA, Arlet JB, Dussiot M, Moura IC,
Courtois G and Hermine O: Ineffective erythropoiesis in
β-thalassemia. ScientificWorldJournal. 2013(394295)2013.
|
|
28
|
Al-Sharifi LM, Murtadha J, Shahad A,
Mohammed Y, Sura J, Waleed Z, Raheeq M, Sura A, Ehab H, Shahad M,
et al: Prevalence of hepatitis B and C in thalassemic patients and
its relation with type of thalassemia, frequency of blood
transfusion, and spleen status. Med J Babylon. 16:108–111.
2019.
|
|
29
|
Mettananda S, Pathiraja H, Peiris R,
Wickramarathne N, Bandara D, de Silva U, Mettananda C and
Premawardhena A: Blood transfusion therapy for β-thalassemia major
and hemoglobin E β-thalassemia: Adequacy, trends, and determinants
in Sri Lanka. Pediatr Blood Cancer. 66(e27643)2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sharma S, Sharma P and Tyler LN:
Transfusion of blood and blood products: Indications and
complications. Am Fam Physician. 83:719–724. 2011.PubMed/NCBI
|
|
31
|
Roberts DJ, Field S, Delaney M and Bates
I: Problems and approaches for blood transfusion in the developing
countries. Hematol Oncol Clin North Am. 30:477–495. 2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Mahmoud RA, El-Mazary AA and Khodeary A:
Seroprevalence of hepatitis C, hepatitis B, cytomegalovirus, and
human immunodeficiency viruses in multitransfused thalassemic
children in upper Egypt. Adv Hematol. 2016(9032627)2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Stainsby D: ABO incompatible
transfusions-experience from the UK Serious Hazards of Transfusion
(SHOT) scheme: Transfusions ABO incompatible. Transfus Clin Biol.
12:385–388. 2005.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Bird EM, Parameswaran U, William T, Khoo
TM, Grigg MJ, Aziz A, Marfurt J, Yeo TW, Auburn S, Anstey NM and
Barber BE: Transfusion-transmitted severe Plasmodium knowlesi
malaria in a splenectomized patient with beta-thalassaemia major in
Sabah, Malaysia: A case report. Malar J. 15(357)2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Stainsby D, Jones H, Asher D, Atterbury C,
Boncinelli A, Brant L, Chapman CE, Davison K, Gerrard R, Gray A, et
al: Serious hazards of transfusion: A decade of hemovigilance in
the UK. Transfus Med Rev. 20:273–282. 2006.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Papanikolaou G, Tzilianos M, Christakis
JI, Bogdanos D, Tsimirika K, MacFarlane J, Goldberg YP,
Sakellaropoulos N, Ganz T and Nemeth E: Hepcidin in iron overload
disorders. Blood. 105:4103–4105. 2005.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Origa R: β-thalassemia. Genet Med.
19(609)2017.
|
|
38
|
Williamson L, Lowe S, Love EM, Cohen H,
Soldan K, McClelland DB, Skacel P and Barbara JA: Serious hazards
of transfusion (SHOT) initiative: Analysis of the first two annual
reports. BMJ. 319:16–19. 1999.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ansari SH, Lassi ZS, Khowaja SM, Adil SO
and Shamsi TS: Hydroxyurea (hydroxycarbamide) for
transfusion-dependent β-thalassaemia. Cochrane Database Syst Rev.
3(CD012064)2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ansari SH, Lassi ZS, Ali SM, Adil SO and
Shamsi TS: Hydroxyurea for β-thalassaemia major. Cochrane Database
Syst Rev. 3(CD012064)2016.
|
|
41
|
Chandy M: Stem cell transplantation in
India. Bone Marrow Transplant. 42 (Suppl 1):S81–S84.
2008.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Jagannath VA, Fedorowicz Z, Al Hajeri A
and Sharma A: Hematopoietic stem cell transplantation for people
with β-thalassaemia major. Cochrane Database Syst Rev.
11(CD008708)2016.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Krishnamurti L, Bunn HF, Williams AM and
Tolar J: Hematopoietic cell transplantation for hemoglobinopathies.
Curr Probl Pediatr Adolesc Health Care. 38:6–18. 2008.PubMed/NCBI View Article : Google Scholar
|
|
44
|
El-Beshlawy A and El-Ghamrawy M: Recent
trends in treatment of thalassemia. Blood Cells Mol Dis. 76:53–58.
2019.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Anasetti C: Use of alternative donors for
allogeneic stem cell transplantation. Hematology Am Soc Hematol
Educ Program. 2015:220–224. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Angelucci E: Hematopoietic stem cell
transplantation in thalassemia. Hematology Am Soc Hematol Educ
Program. 2010:456–462. 2010.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Angelucci E: Hematopoietic stem cell
transplantation in thalassemia. Hematology. 2010:456–462.
2010.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Kyvernitakis A, Mahale P, Popat UR, Jiang
Y, Hosry J, Champlin RE and Torres HA: Hepatitis C virus infection
in patients undergoing hematopoietic cell transplantation in the
era of direct-acting antiviral agents. Biol Blood Marrow
Transplant. 22:717–722. 2016.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Hong KT, Kang HJ, Choi JY, Hong CR, Cheon
JE, Park JD, Park KD, Song SH, Yu KS, Jang IJ and Shin HY:
Favorable outcome of post-transplantation cyclophosphamide
haploidentical peripheral blood stem cell transplantation with
targeted Busulfan-based myeloablative conditioning using intensive
pharmacokinetic monitoring in pediatric patients. Biol Blood Marrow
Transplant. 24:2239–2244. 2018.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Gaziev D, Polchi P, Galimberti M,
Angelucci E, Giardini C, Baronciani D, Erer B and Lucarelli G:
Graft-versus-host disease after bone marrow transplantation for
thalassemia: An analysis of incidence and risk factors.
Transplantation. 63:854–860. 1997.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Mehta PA and Faulkner LB: Hematopoietic
cell transplantation for thalassemia: A global perspective BMT
tandem meeting 2013. Biol Blood Marrow Transplant. 19 (1
Suppl):S70–S73. 2013.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Taher AT, Weatherall DJ and Cappellini MD:
Thalassaemia. Lancet. 391:155–167. 2018.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Elborai Y, Uwumugambi A and Lehmann L:
Hematopoietic stem cell transplantation for thalassemia.
Immunotherapy. 4:947–956. 2012.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Bernaudin F, Pondarré C, Galambrun C and
Thuret I: Allogeneic/matched related transplantation for
β-thalassemia and sickle cell Anemia. Adv Exp Med Biol.
1013:89–122. 2017.
|
|
55
|
Pavone ME, Manuel S and Thompson A:
Fertility Preservation in a Female Adolescent with a
Hemoglobinopathy. In: Textbook of Oncofertility Research and
Practice. Woodruff T, Shah D and Vitek W (eds). Springer, Cham,
pp551-557, 2019.
|
|
56
|
Naldini L: Gene therapy returns to centre
stage. Nature. 526:351–360. 2015.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Kumar SR, Markusic DM, Biswas M, High KA
and Herzog RW: Clinical development of gene therapy: Results and
lessons from recent successes. Mol Ther Methods Clin Dev.
3(16034)2016.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Nienhuis AW: Development of gene therapy
for blood disorders: An update. Blood. 122:1556–1564.
2013.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Goswami R, Subramanian G, Silayeva L,
Newkirk I, Doctor D, Chawla K, Chattopadhyay S, Chandra D,
Chilukuri N and Betapudi V: Gene therapy leaves a vicious cycle.
Front Oncol. 9(297)2019.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Hacein-Bey-Abina S, Von Kalle C, Schmidt
M, McCormack MP, Wulffraat N, Leboulch P, Lim A, Osborne CS,
Pawliuk R, Morillon E, et al: LMO2-associated clonal T cell
proliferation in two patients after gene therapy for SCID-X1.
Science. 302:415–419. 2003.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Naldini L: Ex vivo gene transfer and
correction for cell-based therapies. Nat Rev Genet.
12(301)2011.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Cavazzana-Calvo M, Payen E, Negre O, Wang
G, Hehir K, Fusil F, Down J, Denaro M, Brady T, Westerman K, et al:
Transfusion independence and HMGA2 activation after gene therapy of
human β-thalassaemia. Nature. 467:318–322. 2010.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Srivastava A and Shaji RV: Cure for
thalassemia major-from allogeneic hematopoietic stem cell
transplantation to gene therapy. Haematologica. 102:214–223.
2017.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Montini E, Cesana D, Schmidt M, Sanvito F,
Bartholomae CC, Ranzani M, Benedicenti F, Sergi LS, Ambrosi A,
Ponzoni M, et al: The genotoxic potential of retroviral vectors is
strongly modulated by vector design and integration site selection
in a mouse model of HSC gene therapy. J Clin Invest. 119:964–975.
2009.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Miccio A, Cesari R, Lotti F, Rossi C,
Sanvito F, Ponzoni M, Routledge SJ, Chow CM, Antoniou MN and
Ferrari G: In vivo selection of genetically modified erythroblastic
progenitors leads to long-term correction of β-thalassemia. Proc
Natl Acad Sci USA. 105:10547–10552. 2008.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Roselli EA, Mezzadra R, Frittoli MC,
Maruggi G, Biral E, Mavilio F, Mastropietro F, Amato A, Tonon G,
Refaldi C, et al: Correction of beta-thalassemia major by gene
transfer in haematopoietic progenitors of pediatric patients. EMBO
Mol Med. 2:315–328. 2010.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Lidonnici MR, Paleari Y, Tiboni F,
Mandelli G, Rossi C, Vezzoli M, Aprile A, Lederer CW, Ambrosi A,
Chanut F, et al: Multiple integrated non-clinical studies predict
the safety of lentivirus-mediated gene therapy for β-thalassemia.
Mol Ther Methods Clin Dev. 11:9–28. 2018.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Rasko J, Walters M, Kwiatkowski J, Hongeng
S, Porter J, Sauer M, Thrasher A, Thuret I, Schiller G, Elliot H,
et al: Efficacy and safety of LentiGlobin gene therapy in patients
with transfusion-dependent β-thalassemia and
non-β0/β0 genotypes: Updated results from the
completed phase 1/2 Northstar and ongoing phase 3 Northstar-2
studies. Cytotherapy. 21(S14)2019.
|
|
69
|
Morgan RA, Gray D, Lomova A and Kohn DB:
Hematopoietic stem cell gene therapy: Progress and lessons learned.
Cell Stem Cell. 21:574–590. 2017.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Khosravi MA, Abbasalipour M, Concordet JP,
Berg JV, Zeinali S, Arashkia A, Azadmanesh K, Buch T and Karimipoor
M: Targeted deletion of BCL11A gene by CRISPR-Cas9 system for fetal
hemoglobin reactivation: A promising approach for gene therapy of
beta thalassemia disease. Eur J Pharmacol. 854:398–405.
2019.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Barzel A, Paulk NK, Shi Y, Huang Y, Chu K,
Zhang F, Valdmanis PN, Spector LP, Porteus MH, Gaensler KM, et al:
Promoterless gene targeting without nucleases ameliorates
haemophilia B in mice. Nature. 517:360–364. 2015.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Sadelain M, Rivière I, Wang X, Boulad F,
Prockop S, Giardina P, Maggio A, Galanello R, Locatelli F and
Yannaki E: Strategy for a multicenter phase I clinical trial to
evaluate globin gene transfer in beta-thalassemia. Ann N Y Acad
Sci. 1202:52–58. 2010.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Yannaki E and Stamatoyannopoulos G:
Hematopoietic stem cell mobilization strategies for gene therapy of
beta thalassemia and sickle cell disease. Ann N Y Acad Sci.
1202:59–63. 2010.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Mansilla-Soto J, Riviere I, Boulad F and
Sadelain M: Cell and gene therapy for the beta-thalassemias:
Advances and prospects. Hum Gene Ther. 27:295–304. 2016.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Wu C and Dunbar CE: Stem cell gene
therapy: The risks of insertional mutagenesis and approaches to
minimize genotoxicity. Front Med. 5:356–371. 2011.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Karponi G and Zogas N: Gene therapy for
beta-thalassemia: Updated perspectives. Appl Clin Genet.
12(167)2019.PubMed/NCBI View Article : Google Scholar
|
|
77
|
European Medicines Agency: Advanced
therapy medicinal products: Overview 2018. https://www.ema.europa.eu/en/human-regulatory/overview/advanced-therapy-medicinal-products-overview.
Accessed August 1, 2019.
|
|
78
|
Schuessler-Lenz M, Enzmann H and Vamvakas
S: Regulators' advice can make a difference: European medicines
agency approval of Zynteglo for beta thalassemia. Clin Pharmacol
Ther. 107(492)2020.PubMed/NCBI View Article : Google Scholar
|
|
79
|
European Medicines Agency: Zynteglo.
https://www.ema.europa.eu/en/medicines/human/EPAR/zynteglo#product-information-section.
Accessed June 3, 2019.
|
|
80
|
Hockemeyer D, Soldner F, Beard C, Gao Q,
Mitalipova M, DeKelver RC, Katibah GE, Amora R, Boydston EA,
Zeitler B, et al: Efficient targeting of expressed and silent genes
in human ESCs and iPSCs using zinc-finger nucleases. Nat
Biotechnol. 27:851–857. 2009.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Mushtaq M, Bhat JA, Mir ZA, Sakina A, Ali
S, Singh AK, Tyagi A, Salgotra RK, Dar AA and Bhat R: CRISPR/Cas
approach: A new way of looking at plant-abiotic interactions. J
Plant Physiol. 224:156–162. 2018.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Gupta RM and Musunuru K: Expanding the
genetic editing tool kit: ZFNs, TALENs, and CRISPR-Cas9. J Clin
Invest. 124:4154–4161. 2014.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Scott CT: The zinc finger nuclease
monopoly. Nat Biotechnol. 23:915–918. 2005.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Perez-Pinera P, Ousterout DG and Gersbach
CA: Advances in targeted genome editing. Curr Opin Chem Biol.
16:268–277. 2012.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Charpentier E and Doudna JA:
Biotechnology: Rewriting a genome. Nature. 495:50–51.
2013.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Christian M, Cermak T, Doyle EL, Schmidt
C, Zhang F, Hummel A, Bogdanove AJ and Voytas DF: Targeting DNA
double-strand breaks with TAL effector nucleases. Genetics.
186:757–761. 2010.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Gaj T, Gersbach CA and Barbas CF III: ZFN,
TALEN, and CRISPR/Cas-based methods for genome engineering. Trends
Biotechnol. 31:397–405. 2013.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Baliou S, Adamaki M, Kyriakopoulos AM,
Spandidos DA, Panayiotidis M, Christodoulou I and Zoumpourlis V:
CRISPR therapeutic tools for complex genetic disorders and cancer
(Review). Int J Oncol. 53:443–468. 2018.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Kim EJ, Kang KH and Ju JH: CRISPR-Cas9: A
promising tool for gene editing on induced pluripotent stem cells.
Korean J Intern Med. 32:42–61. 2017.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Stella S and Montoya G: The genome editing
revolution: A CRISPR-Cas TALE off-target story. Inside Cell.
1:7–16. 2016.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Murugan K, Babu K, Sundaresan R, Rajan R
and Sashital DG: The revolution continues: Newly discovered systems
expand the CRISPR-Cas toolkit. Mol Cell. 68:15–25. 2017.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Bhattacharyya S and Mukherjee A: CRISPR:
The revolutionary gene editing tool with Far-reaching applications.
In: Biotechnology Business-Concept to Delivery, Springer, pp47-56,
2020.
|
|
93
|
Ran FA, Hsu PD, Wright J, Agarwala V,
Scott DA and Zhang F: Genome engineering using the CRISPR-Cas9
system. Nat Protocols. 8(2281)2013.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Wang T, Wei JJ, Sabatini DM and Lander ES:
Genetic screens in human cells using the CRISPR-Cas9 system.
Science. 343:80–84. 2014.PubMed/NCBI View Article : Google Scholar
|
|
95
|
van Erp PB, Bloomer G, Wilkinson R and
Wiedenheft B: The history and market impact of CRISPR RNA-guided
nucleases. Curr Opin Virol. 12:85–90. 2015.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Sontheimer EJ and Barrangou R: The
bacterial origins of the CRISPR genome-editing revolution. Hum Gene
Ther. 26:413–424. 2015.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Hsu PD, Lander ES and Zhang F: Development
and applications of CRISPR-Cas9 for genome editing. Call.
157:1262–1278. 2014.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Makarova KS and Koonin EV: Annotation and
classification of CRISPR-Cas systems. In: CRISPR. Springer
Protocols, pp47-75, 2015.
|
|
99
|
Ishino Y, Krupovic M and Forterre P:
History of CRISPR-Cas from encounter with a mysterious repeated
sequence to genome editing technology. J Bacteriol. 200:e00580–17.
2018.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Koonin EV, Makarova KS and Zhang F:
Diversity, classification and evolution of CRISPR-Cas systems. Curr
Opin Microbiol. 37:67–78. 2017.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Shmakov S, Smargon A, Scott D, Cox D,
Pyzocha N, Yan W, Abudayyeh OO, Gootenberg JS, Makarova KS, Wolf
YI, et al: Diversity and evolution of class 2 CRISPR-Cas systems.
Nat Rev Microbiol. 15:169–182. 2017.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Makarova KS, Wolf YI, Alkhnbashi OS, Costa
F, Shah SA, Saunders SJ, Barrangou R, Brouns SJ, Charpentier E,
Haft DH, et al: An updated evolutionary classification of
CRISPR-Cas systems. Nat Rev Microbiol. 13:722–736. 2015.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Moon SB, Ko JH and Kim YS: Recent advances
in the CRISPR genome editing tool set. Exp Mol Med. 51:1–11.
2019.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Li Y and Peng N: Endogenous CRISPR-Cas
System-based genome editing and antimicrobials: Review and
prospects. Front Microbiol. 10(2471)2019.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Hidalgo-Cantabrana C and Barrangou R:
Characterization and applications of type I CRISPR-Cas systems.
Biochem Soc Trans. 28:15–23. 2020.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Zhang H and McCarty N: CRISPR-Cas9
technology and its application in haematological disorders. Br J
Haematol. 175:208–225. 2016.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Grevet JD, Lan X, Hamagami N, Edwards CR,
Sankaranarayanan L, Ji X, Bhardwaj SK, Face CJ, Posocco DF,
Abdulmalik O, et al: Domain-focused CRISPR screen identifies HRI as
a fetal hemoglobin regulator in human erythroid cells. Science.
361:285–290. 2018.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Dulmovits BM, Appiah-Kubi AO, Papoin J,
Hale J, He M, Al-Abed Y, Didier S, Gould M, Husain-Krautter S,
Singh SA, et al: Pomalidomide reverses γ-globin silencing through
the transcriptional reprogramming of adult hematopoietic
progenitors. Blood. 127:1481–1492. 2016.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Sankaran VG, Menne TF, Xu J, Akie TE,
Lettre G, Van Handel B, Mikkola HK, Hirschhorn JN, Cantor AB and
Orkin SH: Human fetal hemoglobin expression is regulated by the
developmental stage-specific repressor BCL11A. Science.
322:1839–1842. 2008.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Jensen TI, Axelgaard E and Bak RO:
Therapeutic gene editing in haematological disorders with
CRISPR/Cas9. Br J Haematol. 185:821–835. 2019.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Shariati L, Rohani F, Heidari Hafshejani
N, Kouhpayeh S, Boshtam M, Mirian M, Rahimmanesh I, Hejazi Z,
Modarres M, Pieper IL and Khanahmad H: Disruption of SOX6 gene
using CRISPR/Cas9 technology for gamma-globin reactivation: An
approach towards gene therapy of β-thalassemia. J Cell Biochem.
119:9357–9363. 2018.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Savić N and Schwank G: Advances in
therapeutic CRISPR/Cas9 genome editing. Transl Res. 168:15–21.
2016.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Porter J: Beyond transfusion therapy: New
therapies in thalassemia including drugs, alternate donor
transplant, and gene therapy. Hematology Am Soc Hematol Educ
Program. 2018:361–370. 2018.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Tang XD, Gao F, Liu MJ, Fan QL, Chen DK
and Ma WT: Methods for enhancing clustered regularly interspaced
short palindromic repeats/Cas9-mediated homology-directed repair
efficiency. Front Genet. 10(551)2019.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Dever DP, Bak RO, Reinisch A, Camarena J,
Washington G, Nicolas CE, Pavel-Dinu M, Saxena N, Wilkens AB,
Mantri S, et al: CRISPR/Cas9 β-globin gene targeting in human
haematopoietic stem cells. Nature. 539:384–389. 2016.
|
|
116
|
Chapman JR, Taylor MR and Boulton SJ:
Playing the end game: DNA double-strand break repair pathway
choice. Mol Cell. 47:497–510. 2012.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Rees HA and Liu DR: Base editing:
Precision chemistry on the genome and transcriptome of living
cells. Nat Rev Genet. 19:770–788. 2018.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Malzahn AL Lowder L and Yiping Qi: Plant
genome editing with TALEN and CRISPR. Cell Biosci.
7(21)2017.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Bortesi L and Fischer R: The CRISPR/Cas9
system for plant genome editing and beyond. Biotechnol Adv.
33:41–52. 2015.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Kim S, Kim D, Cho SW, Kim J and Kim JS:
Highly efficient RNA-guided genome editing in human cells via
delivery of purified Cas9 ribonucleoproteins. Genome Res.
24:1012–1019. 2014.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Enkler L, Richer D, Marchand AL, Ferrandon
D and Jossinet F: Genome engineering in the yeast pathogen Candida
glabrata using the CRISPR-Cas9 system. Sci Rep.
6(35766)2016.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Mou H, Kennedy Z, Anderson DG, Yin H and
Xue W: Precision cancer mouse models through genome editing with
CRISPR-Cas9. Genome Med. 7(53)2015.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Hendel A, Bak RO, Clark JT, Kennedy AB,
Ryan DE, Roy S, Steinfeld I, Lunstad BD, Kaiser RJ, Wilkens AB, et
al: Chemically modified guide RNAs enhance CRISPR-Cas genome
editing in human primary cells. Nat Biotechnol. 33:985–989.
2015.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Liang P, Ding C, Sun H, Xie X, Xu Y, Zhang
X, Sun Y, Xiong Y, Ma W, Liu Y, et al: Correction of β-thalassemia
mutant by base editor in human embryos. Protein Cell. 8:811–822.
2017.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Zhang XH, Tee LY, Wang XG, Huang QS and
Yang SH: Off-target effects in CRISPR/Cas9-mediated genome
engineering. Mol Ther Nucleic Acids. 4(e264)2015.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Lai K, Huang G, Su L and He Y: The
prevalence of thalassemia in mainland China: Evidence from
epidemiological surveys. Sci Rep. 7(920)2017.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Mondal SK and Mandal S: Prevalence of
thalassemia and hemoglobinopathy in eastern India: A 10-year
high-performance liquid chromatography study of 119,336 cases.
Asian J Transfus Sci. 10:105–110. 2016.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Ansari SH, Shamsi TS, Ashraf M, Bohray M,
Farzana T, Tahir Khan M, Perveen K, Erum S, Nadeem M, Ahmed M and
Raza F: Molecular epidemiology of β-thalassemia in Pakistan: Far
reaching implications. Int J Mol Epidemiol Genet. 2:403–408.
2011.PubMed/NCBI
|
|
129
|
Hammoud H, Ghanem H, Abdallah R, Semaan P,
Azzi J, Parra Prada E and Haidar Hassan K: Genetic mutations of
beta thalassemia in middle east countries *corresponding
aurthor. World J Pharm Pharmaceutical Sci. 9:134–150. 2020.
|
|
130
|
Şanlidağ B, Çağin B, Özenli Ö, Şahaloğlu
Ö, Dalkan C, Galip N, Babayiğit Hocaoğlu A and Bahçeciler N:
Prevalence of thalassemia trait & Iron deficiency anemia during
infancy in 2011-2013 in a thalassemia prevalent region: North
Cyprus. Iran J Public Health. 45:1038–1043. 2016.PubMed/NCBI
|
|
131
|
Kountouris P, Kousiappa I, Papasavva T,
Christopoulos G, Pavlou E, Petrou M, Feleki X, Karitzie E,
Phylactides M Fanis P, et al: The molecular spectrum and
distribution of haemoglobinopathies in Cyprus: A 20-year
retrospective study. Sci Re. 6(26371)2016.PubMed/NCBI View Article : Google Scholar
|
|
132
|
Angastiniotis M, Vives Corrons JL,
Soteriades ES and Eleftheriou A: The impact of migrations on the
health services for rare diseases in Europe: The example of
haemoglobin disorders. The Scientific World Journal.
2013(727905)2013.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Guler E, Caliskan U, Ucar Albayrak C and
Karacan M: Prevalence of beta-thalassemia and sickle cell anemia
trait in premarital screening in Konya urban area, Turkey. J
Pediatr Hematol. 29:783–785. 2007.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Mir SA, Alshehri BM, Alaidarous M, Banawas
SS, Dukhyil AAAB and Alturki MK: Prevalence of Hemoglobinopathies
(β-Thalassemia and Sickle Cell Trait) in the adult population of Al
Majma'ah, Saudi Arabia. Hemoglobin. 44:47–50. 2020.PubMed/NCBI View Article : Google Scholar
|
|
135
|
Fucharoen S and Weatherall DJ: Progress
toward the control and management of the thalassemias. Hematol
Oncol Clin North Am. 30:359–371. 2016.PubMed/NCBI View Article : Google Scholar
|
|
136
|
Persons DA: Gene therapy: Targeting
β-thalassaemia. Nature. 467:277–278. 2010.
|
|
137
|
Panigrahi I and Marwaha R: Mutational
spectrum of thalassemias in India. Indian J Hum Genet. 13:36–37.
2007.PubMed/NCBI View Article : Google Scholar
|
|
138
|
Ansari SH, Shamsi TS, Ashraf M, Farzana T,
Bohray M, Perveen K, Erum S, Ansari I, Ahmed MN, Ahmed M and Raza
F: Molecular epidemiology of β-thalassemia in Pakistan: Far
reaching implications. Indian J Hum Genet. 18:193–197.
2012.PubMed/NCBI View Article : Google Scholar
|
|
139
|
Al-Sultan A, Phanasgaonkar S, Suliman A,
Al-Baqushi M, Nasrullah Z and Al-Ali A: Spectrum of β-thalassemia
mutations in the eastern province of Saudi Arabia. Hemoglobin.
35:125–134. 2011.PubMed/NCBI View Article : Google Scholar
|
|
140
|
Hamamy HA and Al-Allawi NA:
Epidemiological profile of common haemoglobinopathies in Arab
countries. J Community Genet. 4:147–167. 2013.PubMed/NCBI View Article : Google Scholar
|
|
141
|
Amato A, Cappabianca MP, Colosimo A, Perri
M, Grisanti P, Zaghis I, Ponzini D and Lerone M: Current genetic
epidemiology of β-Thalassemias and structural hemoglobin variants
in the lazio region (Central Italy) following recent migration
movements. Adv Hematol. 2010(317542)2010.PubMed/NCBI View Article : Google Scholar
|
|
142
|
Boussiou M, Karababa P, Sinopoulou K,
Tsaftaridis P, Plata E and Loutradi-Anagnostou A: The molecular
heterogeneity of beta-thalassemia in Greece. Blood Cells Mol Dis.
40:317–319. 2008.PubMed/NCBI View Article : Google Scholar
|
|
143
|
Sultana G, Begum R, Akhter H, Shamim Z,
Rahim MA and Chubey G: The complete spectrum of beta (β)
thalassemia mutations in Bangladeshi population. Austin Biomark
Diagn. 3(1024)2016.
|
|
144
|
Kleinstiver BP, Pattanayak V, Prew MS,
Tsai SQ, Nguyen N, Zheng Z and Joung JK: High-fidelity CRISPR-Cas9
variants with undetectable genome-wide off-targets. Nature.
529:490–495. 2016.PubMed/NCBI View Article : Google Scholar
|
|
145
|
Acharya S, Mishra A, Paul D, Ansari AH,
Azhar M, Kumar M, Rauthan R, Sharma N, Aich M, Sinha D, et al:
Francisella novicida Cas9 interrogates genomic DNA with very
high specificity and can be used for mammalian genome editing. Proc
Natl Acad Sci USA. 116:20959–20968. 2019.PubMed/NCBI View Article : Google Scholar
|
|
146
|
Lee CM, Cradick TJ and Bao G: The
Neisseria meningitidis CRISPR-Cas9 system enables specific
genome editing in mammalian cells. Mol Ther. 24:645–654.
2016.PubMed/NCBI View Article : Google Scholar
|
|
147
|
Müller M, Lee CM, Gasiunas G, Davis TH,
Cradick TJ, Siksnys V, Bao G, Cathomen T and Mussolino C:
Streptococcus thermophilus CRISPR-Cas9 systems enable
specific editing of the human genome. Mol Ther. 24:636–644.
2016.PubMed/NCBI View Article : Google Scholar
|
|
148
|
Dugar G, Leenay RT, Eisenbart SK, Bischler
T, Aul BU, Beisel CL and Sharma CM: CRISPR RNA-dependent binding
and cleavage of endogenous RNAs by the Campylobacter jejuni
Cas9. Mol Cell. 69:893–905.e7. 2018.PubMed/NCBI View Article : Google Scholar
|
|
149
|
Moon SB, Lee JM, Kang JG, Lee NE, Ha DI,
Kim DY, Kim SH, Yoo K, Kim D, Ko JH, et al: Highly efficient genome
editing by CRISPR-Cpf1 using CRISPR RNA with a uridinylate-rich
3'-overhang. Nat Commun. 9(3651)2018.PubMed/NCBI View Article : Google Scholar
|
|
150
|
Yamano T, Zetsche B, Ishitani R, Zhang F,
Nishimasu H and Nureki O: Structural basis for the canonical and
non-canonical PAM recognition by CRISPR-Cpf1. Mol Cell.
67:633–645.e3. 2017.PubMed/NCBI View Article : Google Scholar
|