Introduction
Cerebral palsy (CP) is a heterogeneous disorder and
there are several degrees of motor impairment and permanent
non-progressive neurologic deficits due to the injury of the
immature brain (1). CP is the most
prevalent cause of disabilities in children. The overall global
prevalence of CP is 2-3 per 1,000 live births (1). The motor disorders of CP include
disturbances of sensation, perception, cognition, communication and
behavior; and these symptoms are caused by epilepsy and secondary
musculoskeletal disorders (2). Aside
from the physical and mental disabilities, children with CP are
often malnourished due to disruption of the enteric neural pathways
resulting in problems swallowing, and as a result exhibit
gastroesophageal reflux and difficulty in breathing (3). Previous studies have reported the
negative effects of malnutrition on muscle strength, impairment of
motor function and weakness of the respiratory muscle (4), pre-dispositions to congestive heart
failure (5), impairments in wound
healing and immune function, and increased risk of postoperative
complications (6).
The classification of CP is based on the motor type
and distribution including ataxia, athetoid, diplegia, double
hemiplegia, hemiplegia and quadriplegia (3). The Gross Motor Function Classification
System (GMFCS) is used in clinical practice (3). Studies have shown that a persistent and
exacerbated inflammatory response in the central nervous system can
cause neuronal damage (7,8). To the best of our knowledge, there are
no studies aimed at identifying inflammatory biomarkers that can
indicate the severity of CP.
Peripheral blood tests are routinely used in
clinical practice. Several studies have reported that the
neutrophil-to-lymphocyte ratio (NLR) and lymphocyte-to-monocyte
ratio (LMR) may serve as biomarkers of an inflammatory response,
and may be used as prognostic factors to predict the outcome or the
severity of various malignancies (9), cardiovascular disease (10), systemic lupus erythematosus (11), hip fracture and polytrauma (12). Moreover, studies have demonstrated
that NLR is associated with nutritional status in geriatric and
cancer patients (13,14).
The healthcare costs for CP children with
co-morbidities are high. In Australia, the cost of taking care of a
single CP child is $43,431 per year (15). There are two primary means of
providing healthcare for children with CP: Home-based procedures
and rehabilitation center-based procedures. Home-based patients
exhibit improved social acceptance, functioning, participation and
physical health, emotional wellbeing and self-esteem, as well as
family health; in addition, these patients do not need to spend a
lot of time traveling to the doctor, and thus have lower
transportation costs (15). However,
the healthcare costs for these patients are higher compared to
children living in a rehabilitation center.
As CP children may live in different settings, the
aim of the present study was to investigate the physical growth,
nutritional status and inflammatory predictors between children
living at home and the rehabilitation center. It was hypothesized
that CP children living at home would exhibit improved physical
growth, nutritional status and lower inflammatory parameters when
compared with CP children living in a rehabilitation center. The
relationships between these parameters and the severity of the
motor impairment in CP children were also examined.
Materials and methods
Ethics
The study protocol used in the present study
conformed to the ethical standards outlined in the Declaration of
Helsinki and was approved by the Institutional Review Board on
Human Research of the Faculty of Medicine, Chulalongkorn
University. Informed consent was obtained from one of the parents
or the legal guardian of the children, as well as from the child
prior to his/her participation in the study.
Study participants
A total of 86 CP children were enrolled in a
cross-sectional analytical study that was performed between June
and December 2013. A total of 6 children were excluded as they had
a history of gastrostomy (n=2), osteotomy around the knee (n=2), or
were infections during the screening period (n=2). A total of 80
children with CP (45 males and 35 females) were eligible for
analysis. The mean age in this study population was 8.52±1.92
years. These children were recruited from either a home-living
setting (n=34) or a rehabilitation center (n=46). The home-living
participants were those who lived at home and visited the
rehabilitation center during office hours. Participants who lived
at the rehabilitation center for at least 9 months were enrolled
into the study.
Determination of clinical
parameters
For the anthropometric measurements in the present
study, the body weight was obtained and the height was calculated
using Stevenson's recommended formula (16). The height (cm) was measured while in
a sitting position from the knee to the floor. This measurement was
taken 3 times, and the mean height was used. The body mass index
(BMI) was calculated. To evaluate the nutritional status of the
children, the anthropometric indices, including weight-for-age,
height-for-age and weight-for-height, were used to calculate the z
score based on the World Health Organization reference population
median (17). Z-scores >2
standard deviations lower than the mean, for weight-for-age,
height-for-age and weight-for-height, were considered as
underweight, stunted and wasted, respectively.
The motor function for all CP children was evaluated
and assigned according to the Gross Motor Function Classification
System (GMFCS) level by certified physical therapists (18). The severity levels of motor
impairment were divided into two groups: Mild motor impairment
(GMFCS levels I-III) and severe motor impairment (GMFCS levels
IV-V).
Peripheral blood counts were obtained from all
participants as part of routine analysis. An automated hematology
analyzer (Advia 2120 Hematology system; Siemens Healthineers) was
utilized to obtain the complete blood count (CBC). Neutrophil and
lymphocyte counts were extracted from the differential blood
pictures. The NLR was calculated by dividing the absolute count of
neutrophils by the number of lymphocytes from the CBCs.
Additionally, the LMR was determined by dividing the absolute
number of lymphocytes to the number of the monocytes.
Statistical analysis
Statistical analysis was performed using SPSS
version 22.0 (IBM Corp.). Continuous data are presented as the mean
± standard error of the mean. Categorical data are summarized as
the frequency and percentages. Comparisons of the frequencies of
various demographic variables between the two groups were performed
using a χ2 test. The distributions of the continuous
data were examined using a Q-Q plot, Shapiro-Wilk's test and a
Kolmogorov-Smirnov test. To compare the means between the two
groups, an unpaired Student's t-test was used for variables that
were normally distributed. A Mann-Whitney U test was used for
variables that did not have a normal distribution. For comparisons
between >2 groups of variables, a Kruskal-Wallis one-way ANOVA
with a Dunn's post hoc test was used for all pairwise comparisons.
Pearson's and Spearman's correlation analysis were used to examine
the relationship between variables. P<0.05 was used to indicate
a statistically significant difference.
Results
The participants were divided into two groups, those
living at home and those living in the rehabilitation center. The
clinical characteristics of the participants are shown in Table I. There were no significant
differences in the clinical characteristics between the two groups
of children. Diplegic CP was the most common type of CP amongst
participants living at home and the rehabilitation center. The
severity of the motor impairment was categorized by GMFCS levels.
In both care settings, the children had mild and severe motor
impairments.
 | Table IClinical characteristics of CP
children living at home or the rehabilitation center. |
Table I
Clinical characteristics of CP
children living at home or the rehabilitation center.
| Characteristics | Living at home, n
(%) | Living at
rehabilitation centre, n (%) | P-value |
|---|
| Total | 34 | 46 | |
| Sex | | | |
|
Male | 18 (52.9) | 27 (58.7) | 0.18 |
|
Female | 16 (47.1) | 19 (41.3) | 0.612 |
| CP type | | | |
|
Ataxia | 1 (2.9) | 0 (0) | - |
|
Athetoid | 4 (11.8) | 4 (8.7) | 1 |
|
Diplegia | 19 (55.9) | 33 (71.7) | 0.052 |
|
Double
hemiplegia | 1 (2.9) | 1 (2.2) | 1 |
|
Hemiplegia | 1 (2.9) | 5 (10.9) | 0.102 |
|
Quadriplegia | 8 (23.5) | 3 (6.5) | 0.132 |
| GMFCS level | | | |
|
MMI | 16 (47.1) | 28 (60.9) | 0.07 |
|
Level
II | 3 (8.8) | 6(13) | 0.317 |
|
Level
III | 13 (38.2) | 22 (47.9) | 0.128 |
|
SMI | 18 (52.9) | 18 (39.1) | 1 |
|
Level
IV | 11 (32.4) | 15 (32.6) | 0.433 |
|
Level V | 7 (20.6) | 3 (6.5) | 0.206 |
| Malnutrition | | | |
|
Underweight | 12 (35.3) | 19 (41.3) | 0.209 |
|
Stunted | 17(50) | 25 (54.3) | 0.217 |
|
Wasted | 3 (8.8) | 8 (17.4) | 0.132 |
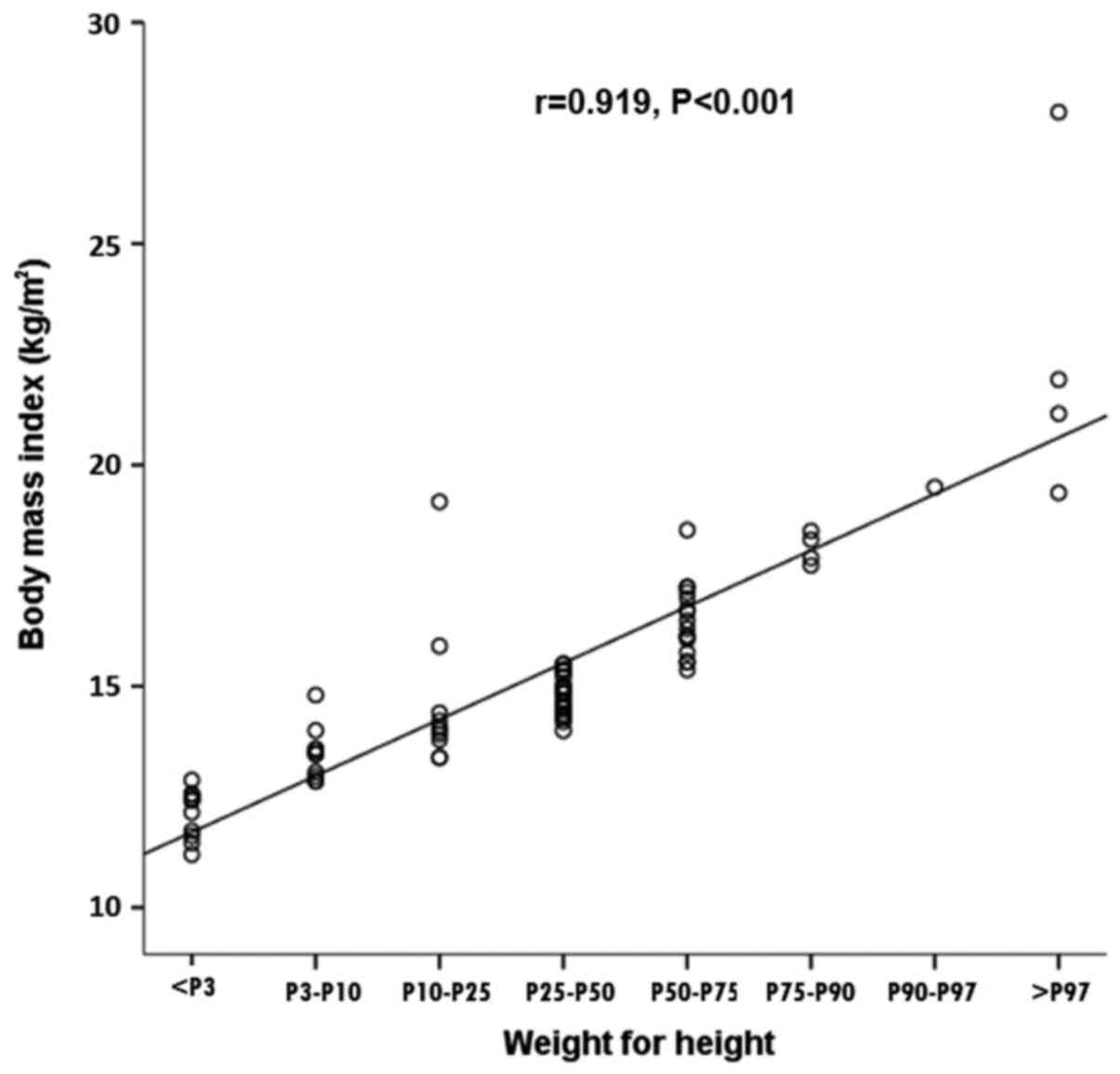
For anthropometric parameters, the height, weight
and BMI were not significantly different between the children
living at home and the rehabilitation center. However, the
percentage of underweight, stunted and wasted participants was
higher amongst children living at the rehabilitation center
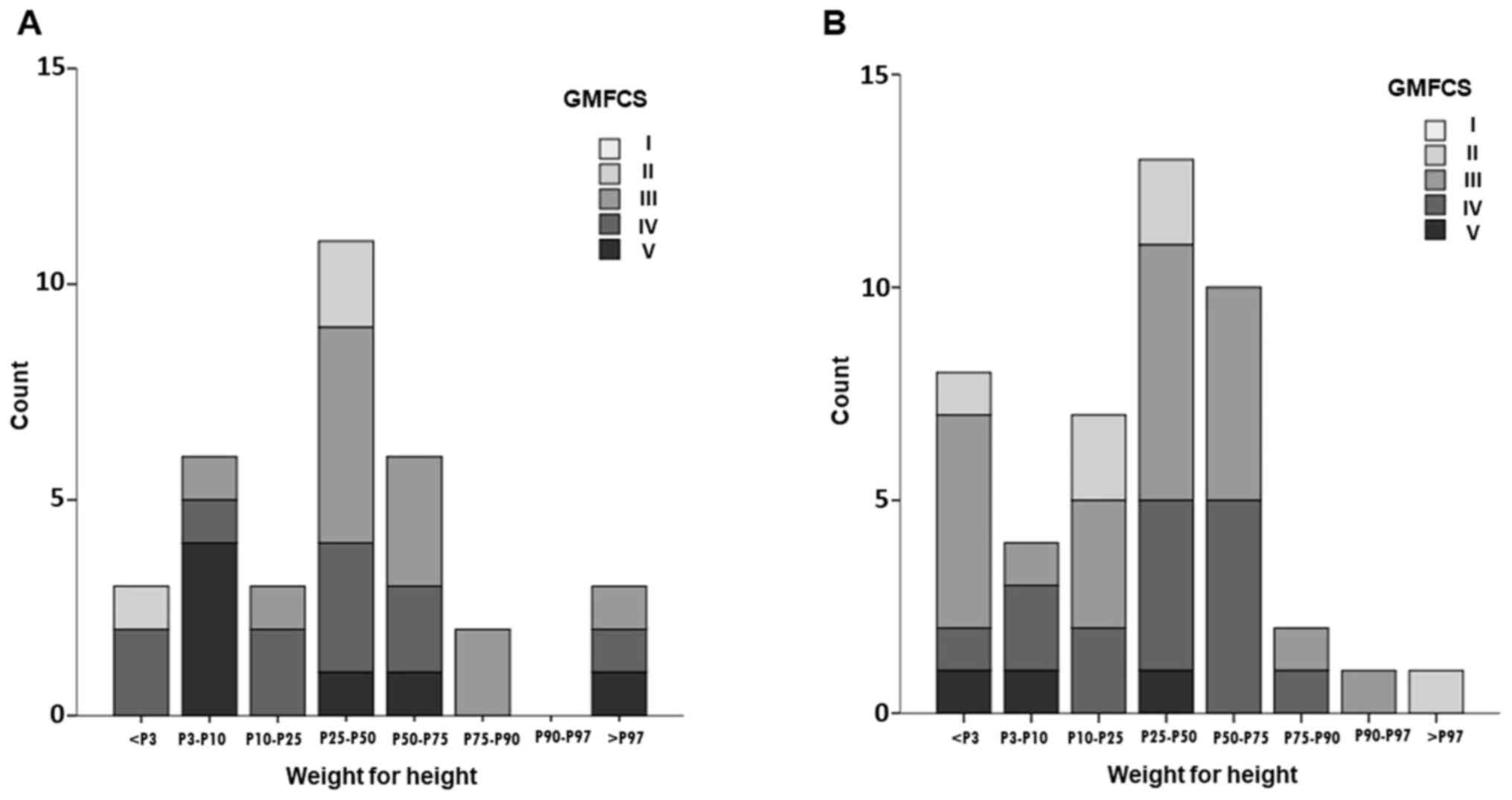
compared with those living at home (Table I). The weight-for-height percentiles
were strongly correlated with BMI in CP children (r=0.919,
P<0.001; Fig. 1). The
distribution of weight-for-height percentiles with stacking of each
GMFCS level demonstrated left shifting, particularly in children
living at the rehabilitation center (Fig. 2).
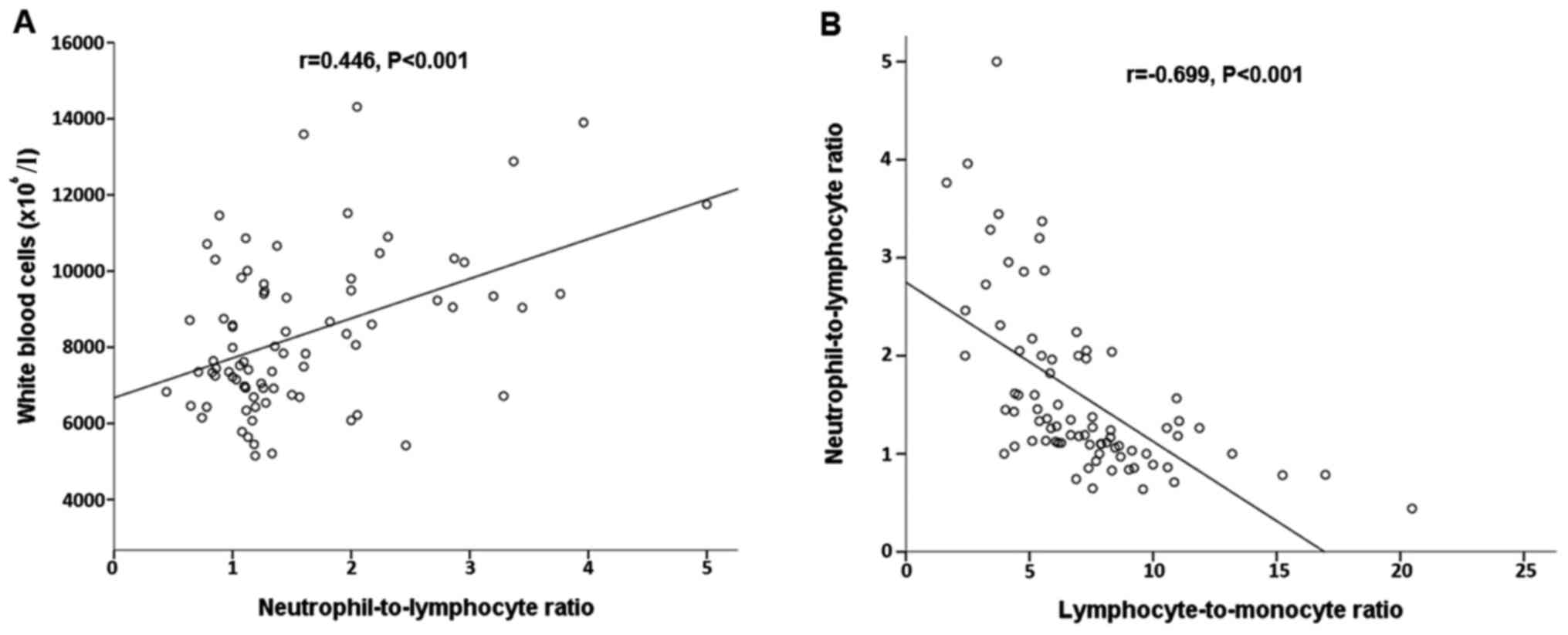
The CBC analysis showed that total white blood cell
counts, neutrophil counts and the NLR values were significantly
greater in the CP children at the rehabilitation center compared
with those living at home (P<0.05; Table II). There was a direct association
between the total white blood cell count and the NLR (r=0.446,
P<0.001). However, NLR was inversely correlated with LMR in CP
children, as illustrated in Fig. 3
(r=-0.699, P<0.001).
 | Table IIComparison of anthropometric and
biochemical parameters of study samples compared between children
with CP living at home or the rehabilitation center. |
Table II
Comparison of anthropometric and
biochemical parameters of study samples compared between children
with CP living at home or the rehabilitation center.
|
Characteristics | Living at home,
n=34 mean ± SEM | Living at
rehabilitation centre, n=46 mean ± SEM | P-value |
|---|
| Age, years | 8.41±0.4 | 8.52±0.28 | 0.819 |
| Height, cm | 115.21±2.73 | 114.52±1.79 | 0.828 |
| Weight, kg | 22.14±1.13 | 21.64±1.03 | 0.778 |
| BMI,
kg/m2 | 15.46±0.41 | 15.02±0.4 | 0.376 |
| Haemoglobin,
g/dl | 13.06±0.16 | 12.76±0.15 | 0.18 |
| Haematocrit, % | 38.77±0.46 | 38.25±0.39 | 0.386 |
| White blood cells,
x106/l |
7,785.59±339.46 |
8,728.04±297.02 | 0.022a |
| Neutrophils,
x106/l | 3,726.5±238.25 | 4,791.3±257.5 | 0.002b |
| Lymphocytes,
x106/l | 3,111.8±144.34 |
2,939.13±130.05 | 0.38 |
| Monocytes,
x106/l | 455.6±31.34 | 488.7±27.12 | 0.273 |
|
Neutrophil-to-lymphocyte ratio | 1.29±0.1 | 1.81±015 | 0.003b |
|
Lymphocyte-to-monocyte ratio | 7.82±0.62 | 6.66±0.41 | 0.106 |
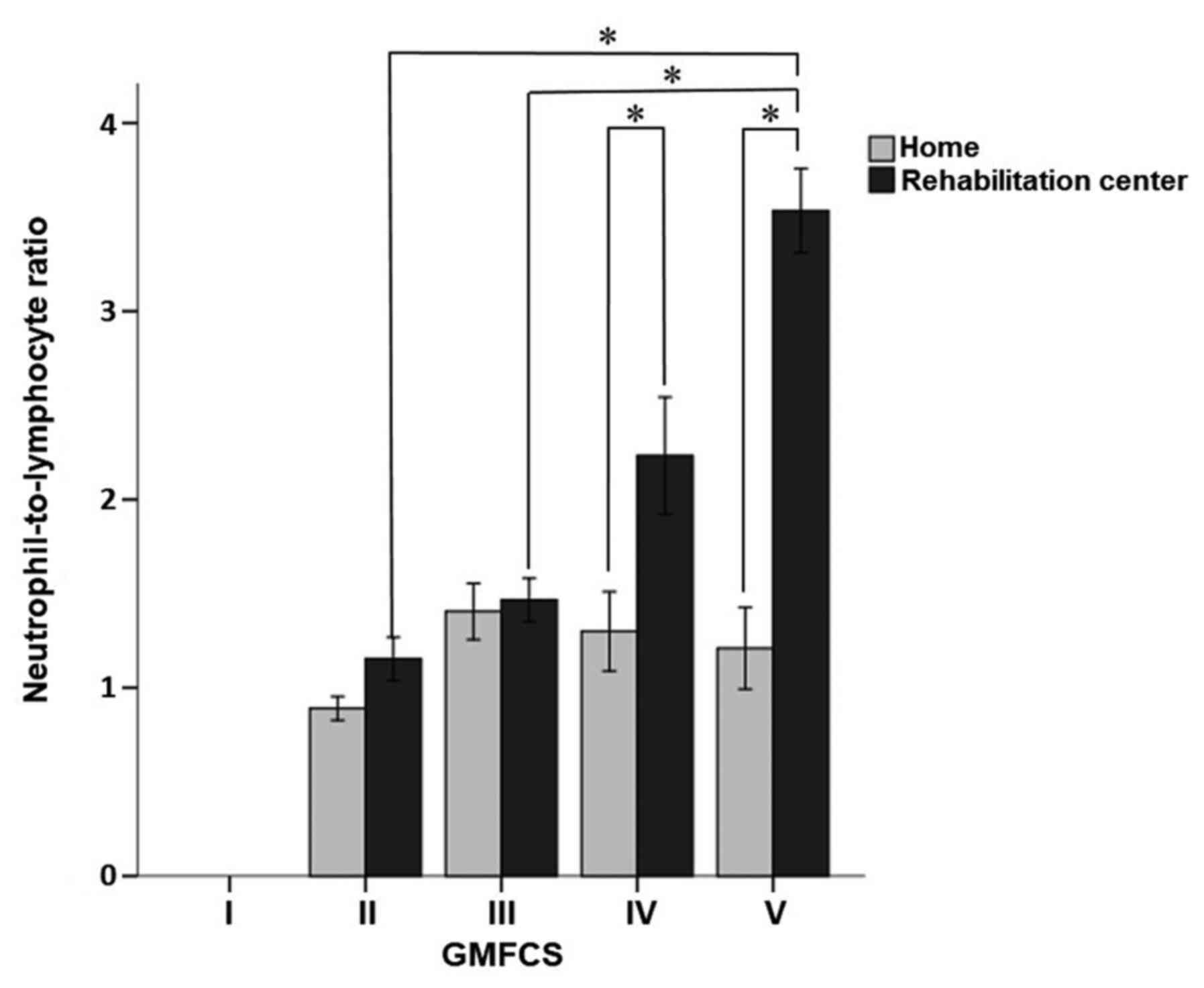
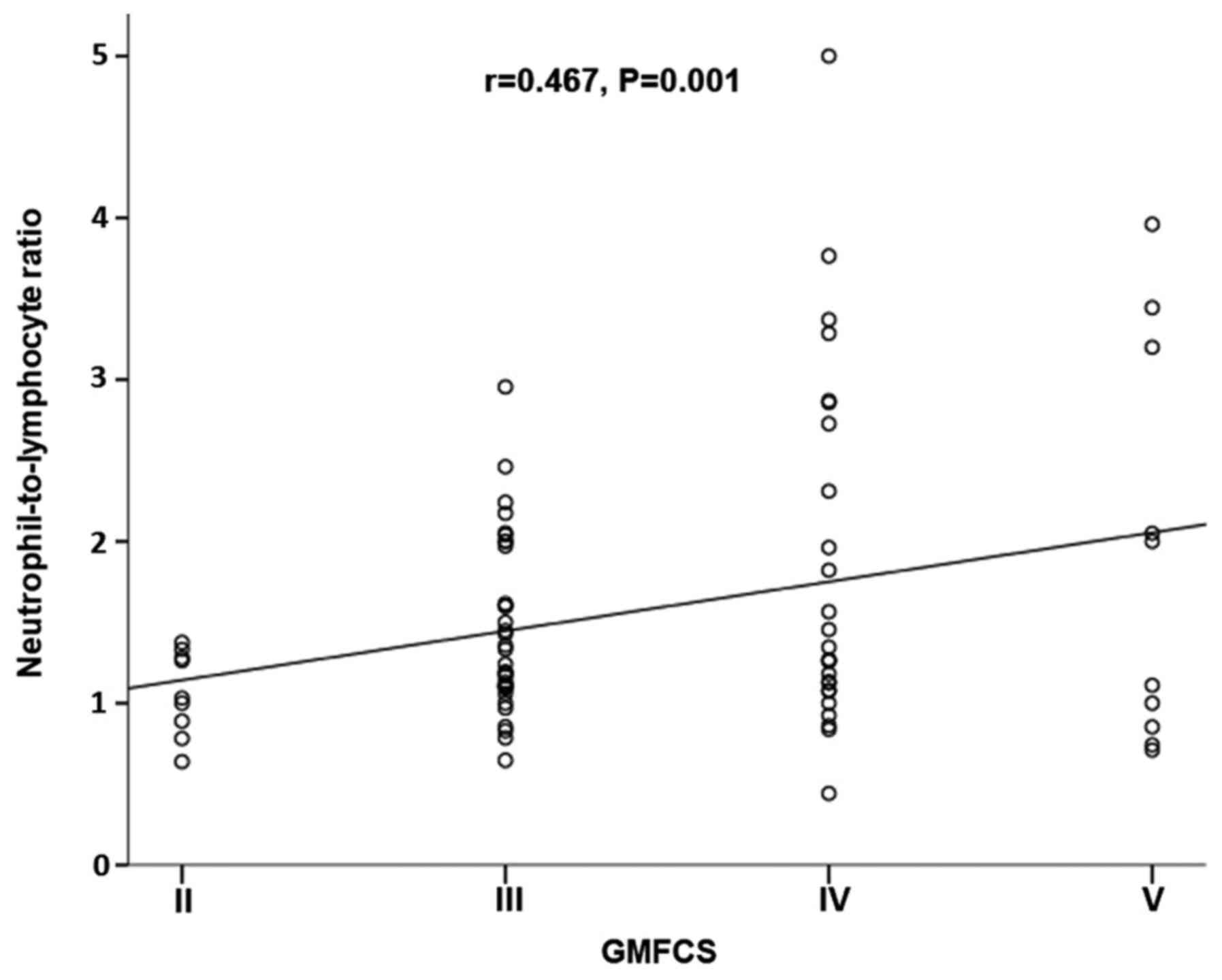
Overall, the NLR of the children in the
rehabilitation center was significantly higher than those living at
home (P=0.003; Table II).
Additionally, the NLR was significantly higher in children with
severe motor impairment (P=0.001; Table III; Fig.
4). In the rehabilitation center, the NLR values between mild
and severe motor impairments were statistically different (P=0.006)
and the proportion of children with GMFCS level V was greater than
those with levels II and III (P=0.021 and P=0.04, respectively;
Table III; Fig. 4). However, the NLR values were not
significantly different amongst children based on severity of motor
impairment. NLR was significantly positively correlated with GMFCS
level (r=0.467, P=0.001; Fig.
5).
 | Table IIIComparison of NLR and motor
impairment severity between children with CP living at home-living
and those living at a rehabilitation center. |
Table III
Comparison of NLR and motor
impairment severity between children with CP living at home-living
and those living at a rehabilitation center.
|
Characteristics | Living at home,
n=34 n (mean ± SEM) | Living at
rehabilitation centre, n=46 n (mean ± SEM) | P-value |
|---|
| MMI | | | |
|
GMFCS level
II | 3 (0.89±0.63) | 6 (1.15±0.11) | 0.121 |
|
GMFCS level
III | 13 (1.41±0.15) | 22 (1.47±0.11) | 0.759 |
|
Total | 16 (1.31±0.13) | 28 (1.4±0.1) | 0.38 |
| SMI | | | |
|
GMFCS level
IV | 11 (1.3±0.21) | 15 (2.23±0.31) | 0.014a |
|
GMFCS level
V | 7 (1.21±0.22) | 3 (3.53±0.22) | 0.017a |
|
Total | 18 (1.26±0.15) | 18 (2.45±0.29) | 0.001b |
| Overall | 34 (1.29±0.1) | 46 (1.81±0.15) | 0.003b |
| P (MMI/SMI) | 0.437 | 0.006b | |
| P (GMFCS) | 0.194 | 0.01b | |
Discussion
The aim of the present study was to evaluate the
physical growth, nutritional status, and the inflammatory
parameters of NLR and LMR between CP children living at home
compared with those living in a rehabilitation center. The results
showed that almost half of the children had one form of
malnutrition. The most common type of malnutrition was stunted
growth (50% of children at home and 54.3% of children at the
center), followed by being underweight (35.3% of children at home
and 41.3% of children at center) and wasted (8.8% of children at
home and 17.4% of children at center), in agreement with a previous
study (19).
Henderson et al (20) reported that residential care children
showed improved growth and nutrition scores, lower height Z scores,
similar weight and muscle mass, and greater subcutaneous fat Z
scores than children living at home. In contrast, the results of
the present study showed higher percentages of all forms of
malnutrition in CP children living at the rehabilitation center
compared with those living at home.
In routine medical practice, CBC and differentiation
analysis are commonly used (21,22). In
the present study, the severity of the motor impairments was
associated with higher NLR values, particularly in CP children
living at the rehabilitation center. NLR values were significantly
higher in CP children with severe motor impairment in the
rehabilitation center.
NLR is easy to calculate and can provide useful
information. Increases in NLR are indicative of systemic
inflammation and physiological stress responses, including an
increase in neutrophil counts, a decrease in lymphocyte counts, or
both (23). Recently, NLR has been
shown to be a good prognostic parameter for assessment of various
diseases and was correlated with the treatment or operational
outcomes of several clinical conditions, including gastric, liver
and colorectal cancer (24-26).
Additionally, NLR is positively correlated with several biomarkers
of cancer, such as carbohydrate antigen 19-9 and carcinoembryonic
antigen, and was associated with advanced stage malignancies
(27,28), and overall survival and mortality for
various diseases (29,30).
Persistent elevation in inflammation-related
proteins during the first two postnatal weeks is associated with
the diagnosis of CP, and this pattern of expression was also
observed in severely cognitively impaired children (31). CP is a neurodevelopmental disorder
and is attributed to injury in the developing brain. Various animal
models of CP have shown that the injury to the central nervous
system is due to hypoxia-ischemia and inflammation in the brain
(32). Furthermore, elevated
inflammatory response-associated proteins may reflect the ongoing
damage of the brain cells resulting in brain dysfunction (33).
Over half of neuroanatomical abnormalities in CP
patients are white matter injuries, cystic periventricular
leukomalacia and periventricular hemorrhagic infarction (34). The ELGAN cohort found that systemic
inflammation was associated with white matter abnormalities
(35). Inflammatory cytokines and
inflammation related proteins are present during the neonatal
period (36,37). Additionally, levels of IL-1β, IL-6,
TNF and CXCL8/IL-8 in children with CP are persistently elevated
(8). Unfortunately, the markers
mentioned above are rarely used in routine medical practices, and
only in research. Thus, our proposed low cost, accessible
inflammatory predictor, NLR, may be an improved prognostic
parameter for CP; however, additional studies are required to
confirm these results.
The present study has some limitations. First, this
was a cross-sectional study. Therefore it was not possible to
determine a cause-effect relationship. Second, a healthy control
group was not available for comparison. Third, the sample size was
too small, and thus made identification of significant differences
between groups difficult. Finally, it is possible that the
environment, family participation and emotional stress may be
different between the two groups, and this may affect the overall
quality of life of CP children.
In conclusion, a high NLR value was associated with
severe motor impairment in children with CP, particularly those
living in rehabilitation centers. These results suggest that NLR
may be used as a prognostic predictor of severe motor impairment.
However, further studies on the value and relevance of NLR are
required to ascertain whether it can be used to predict treatment
and/or surgical outcomes, as well as mortality and survival amongst
CP children.
Acknowledgements
The authors would also like to thank Ms. Pirapon
June Ohata, HIV-NAT, Thai Red Cross AIDS Research Center, Bangkok,
Thailand for reviewing and proof-reading the manuscript.
Funding
This study was financially supported by the
Osteoarthritis and Musculoskeleton Research Unit, the
Ratchadapiseksompotch Fund, Chulalongkorn University (grant no.
CU_GR_63_95_30_02) and the Prince Mahidol Award Youth Program,
Prince Mahidol Award Foundation.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
KR, CA, PO, SW, NL and SH conceived and designed the
experiments. KR, CA, PO, SW, NL and SH performed the experiments
and analyzed the data. CA, NL and SH provided the materials and
analytical tools. CA, PO, SW and NL recruited the participants,
obtained the written informed consents and collected the clinical
data. KR and SH wrote and revised the manuscript. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
The study protocol used in the present study
conformed to the ethical standards outlined in the Declaration of
Helsinki and was approved by the Institutional Review Board on
Human Research of the Faculty of Medicine, Chulalongkorn
University. Informed consent was obtained from one of the parents
or the legal guardian, as well as from the child prior to his/her
participation in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rattanatharn R and Siriphaosuwankul W:
Back and hip muscles with EMG biofeedback training in diplegic
cerebral palsy to improve balance and gait: A randomized control
trial. Chula Med J. 63:31–39. 2019.
|
|
2
|
Mahasup P and Kanchanomai S: Comparison of
lower extremity range of motion during walking between children
with cerebral palsy and normal children. Chula Med J. 63:171–177.
2019.
|
|
3
|
Gulati S and Sondhi V: Cerebral palsy: An
overview. Indian J Pediatr. 85:1006–1016. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kuperminc MN and Stevenson RD: Growth and
nutrition disorders in children with cerebral palsy. Dev Disabil
Res Rev. 14:137–146. 2008.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Viart P: Hemodynamic findings in servere
protein-calorie malnutrition. Am J Clin Nutr. 30:334–348.
1977.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cross MB, Yi PH, Thomas CF, Garcia J and
Della Valle CJ: Evaluation of malnutrition in orthopaedic surgery.
J Am Acad Orthop Surg. 22:193–199. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fleiss B and Gressens P: Tertiary
mechanisms of brain damage: A new hope for treatment of cerebral
palsy? Lancet Neurol. 11:556–566. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Magalhaes RC, Moreira JM, Lauar AO, da
Silva AAS, Teixeira AL and E Silva ACS: Inflammatory biomarkers in
children with cerebral palsy: A systematic review. Res Dev Disabil.
95(103508)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Templeton AJ, McNamara MG, Šeruga B,
Vera-Badillo FE, Aneja P, Ocaña A, Leibowitz-Amit R, Sonpavde G,
Knox JJ, Tran B, et al: Prognostic role of neutrophil-to-lymphocyte
ratio in solid tumors: A systematic review and Meta-analysis. J
Natl Cancer Inst. 106(dju124)2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Afari ME and Bhat T: Neutrophil to
lymphocyte ratio (NLR) and cardiovascular diseases: An update.
Expert Rev Cardiovasc Ther. 14:573–577. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wang L, Wang C, Jia X, Yang M and Yu J:
Relationship between Neutrophil-to-lymphocyte ratio and systemic
lupus erythematosus: A meta-analysis. Clinics (Sao Paulo).
75(e1450)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Alexandru L, Haragus H, Deleanu B, Timar
B, Poenaru DV and Vlad DC: Haematology panel biomarkers for
humeral, femoral, and tibial diaphyseal fractures. Int Orthop.
43:1567–1572. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kaya T, Açıkgöz SB, Yıldırım M, Nalbant A,
Altaş AE and Cinemre H: Association between
neutrophil-to-lymphocyte ratio and nutritional status in geriatric
patients. J Clin Lab Anal. 33(e22636)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sato Y, Gonda K, Harada M, Tanisaka Y,
Arai S, Mashimo Y, Iwano H, Sato H, Ryozawa S, Takahashi T, et al:
Increased Neutrophil-to-lymphocyte ratio is a novel marker for
nutrition, inflammation and chemotherapy outcome in patients with
locally advanced and metastatic esophageal squamous cell carcinoma.
Biomed Rep. 7:79–84. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sharif Azar E, Ravanbakhsh M, Torabipour
A, Amiri E and Haghighyzade MH: Home-based versus center-based care
in children with cerebral palsy: A cost-effectiveness analysis. J
Med Life. 8:245–251. 2015.PubMed/NCBI
|
|
16
|
Stevenson RD: Use of segmental measures to
estimate stature in children with cerebral palsy. Arch Pediatr
Adolesc Med. 149:658–662. 1995.PubMed/NCBI View Article : Google Scholar
|
|
17
|
de Onis M and Blössner M: The world health
organization global database on child growth and malnutrition:
Methodology and applications. Int J Epidemiol. 32:518–526.
2003.PubMed/NCBI View Article : Google Scholar
|
|
18
|
CanChild: Gross Motor Function
Classification System-Expanded and Revised (GMFCS-E&R).
CanChild, Hamilton, ON, 2019. urihttps://canchild.ca/en/resources/42-gross-motor-function-classification-system-expanded-revised-gmfcs-e-rsimplehttps://canchild.ca/en/resources/42-gross-motor-function-classification-system-expanded-revised-gmfcs-e-r.
Accessed September 30, 2020.
|
|
19
|
Khan S, Zaheer S and Safdar NF:
Determinants of stunting, underweight and wasting among children
<5 years of age: Evidence from 2012-2013 Pakistan demographic
and health survey. BMC Public Health. 19(358)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Henderson RC, Grossberg RI, Matuszewski J,
Menon N, Johnson J, Kecskemethy HH, Vogel L, Ravas R, Wyatt M,
Bachrach SJ and Stevenson RD: Growth and nutritional status in
residential center versus home-living children and adolescents with
quadriplegic cerebral palsy. J Pediatr. 151:161–166.
2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kurt-Mangold ME, Grieme CV, Krasowski MD
and Rosenthal NS: Clinical utility of ordered pathology blood smear
reviews-an overused resource? Clin Lab. 64:99–104. 2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Barnes PW, McFadden SL, Machin SJ and
Simson E: The international consensus group for hematology review:
Suggested criteria for action following automated CBC and WBC
differential analysis. Lab Hematol. 11:83–90. 2005.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zahorec R: Ratio of neutrophil to
lymphocyte Counts-rapid and simple parameter of systemic
inflammation and stress in critically ill. Bratisl Lek Listy.
102:5–14. 2001.PubMed/NCBI(In En, Slovak).
|
|
24
|
Li H, Zhao Y and Zheng F: Prognostic
significance of elevated preoperative neutrophil-to-lymphocyte
ratio for patients with colorectal cancer undergoing curative
surgery: A Meta-analysis. Medicine (Baltimore).
98(e14126)2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang Y, Peng C, Cheng Z, Wang X, Wu L, Li
J, Huang C, Guo Q and Cai H: The prognostic significance of
preoperative Neutrophil-lymphocyte ratio in patients with
hepatocellular carcinoma receiving hepatectomy: A systematic review
and meta-analysis. Int J Surg. 55:73–80. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Nakamura N, Kinami S, Tomita Y, Miyata T,
Fujita H, Takamura H, Ueda N and Kosaka T: The
neutrophil/lymphocyte ratio as a predictor of successful conversion
surgery for stage IV gastric cancer: A retrospective study. BMC
Cancer. 20(363)2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Tang H, Lu W, Li B, Li C, Xu Y and Dong J:
Prognostic significance of neutrophil-to-lymphocyte ratio in
biliary tract cancers: A systematic review and Meta-analysis.
Oncotarget. 8:36857–36868. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tang H, Li B, Zhang A, Lu W, Xiang C and
Dong J: Prognostic significance of Neutrophil-to-lymphocyte ratio
in colorectal liver metastasis: A systematic review and
Meta-analysis. PLoS One. 11(e0159447)2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kuang ZS, Yang YL, Wei W, Wang JL, Long
XY, Li KY, Li KY, Tong CY, Sun Z and Song ZJ: Clinical
characteristics and prognosis of community-acquired pneumonia in
autoimmune disease-induced immunocompromised host: A retrospective
observational study. World J Emerg Med. 11:145–151. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Krishnan A, Hsu J, Ha JS, Broderick SR,
Shah PD, Higgins RS, Merlo CA and Bush EL: Elevated neutrophil to
lymphocyte ratio is associated with poor long-term survival and
graft failure after lung transplantation. Am J Surg: Apr 18, 2020
(Epub ahead of print).
|
|
31
|
O'Shea TM, Allred EN, Kuban KC, Dammann O,
Paneth N, Fichorova R, Hirtz D and Leviton A: Extremely Low
Gestational Age Newborn (ELGAN) Study Investigators. Elevated
concentrations of Inflammation-related proteins in postnatal blood
predict severe developmental delay at 2 years of age in extremely
preterm infants. J Pediatr. 160:395–401.e4. 2012.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Cavarsan CF, Gorassini MA and Quinlan KA:
Animal models of developmental motor disorders: Parallels to human
motor dysfunction in cerebral palsy. J Neurophysiol. 122:1238–1253.
2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Malaeb S and Dammann OL: Fetal
inflammatory response and brain injury in the preterm newborn. J
Child Neurol. 24:1119–1126. 2009.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Novak I, Morgan C, Adde L, Blackman J,
Boyd RN, Brunstrom-Hernandez J, Cioni G, Damiano D, Darrah J,
Eliasson AC, et al: Early, accurate diagnosis and early
intervention in cerebral palsy: Advances in diagnosis and
treatment. JAMA Pediatr. 171:897–907. 2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Leviton A, Kuban K, O'Shea TM, Paneth N,
Fichorova R, Allred EN and Dammann O: The relationship between
early concentrations of 25 blood proteins and cerebral white matter
injury in preterm newborns: The ELGAN study. J Pediatr.
158:897–903.e1-e5. 2011.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kuban KC, O'Shea TM, Allred EN, Paneth N,
Hirtz D, Fichorova RN and Leviton A: ELGAN Study Investigators.
Systemic inflammation and cerebral palsy risk in extremely preterm
infants. J Child Neurology. 29:1692–1698. 2014.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Kadhim H, Tabarki B, Verellen G, De Prez
C, Rona AM and Sébire G: Inflammatory cytokines in the pathogenesis
of periventricular leukomalacia. Neurology. 56:1278–1284.
2001.PubMed/NCBI View Article : Google Scholar
|