Introduction
Slipped capital femoral epiphysis (SCFE) is a
relatively common adolescent hip disorder, accounting for ~10.8
cases per 100,000 patients (1).
This is explained by the fact that the physis is exhibits prominent
levels of lysis during growth. The risk of epiphyseal displacement
is also affected by normal proximal femoral development, physeal
orientation, acetabular morphology as well as the endocrinological
status of the adolescent (1,2).
During SCFE, a mechanical overload to the proximal femoral physis
occurs, which leads to an anterior translation and external
rotation of the metaphysic, respecting the upper femoral epiphysis
(3,4). Regarding SCFE symptomatology, limping
and pain in the affected groin, lateral or posterior hip, thigh or
ipsilateral knee are commonly observed. SCFE is also likely to
present as knee pain, which may account for the high rates of
misdiagnoses of this condition (5).
Several classification systems have been developed
for SCFE. According to the duration of the symptoms, SCFE can be
classified as acute, chronic or acute-on-chronic (6). Acute SCFE presents within 3 weeks of
the onset of symptoms, and accounts for 10-15% of all SCFE cases.
Moreover, acute SCFE is associated with a higher rate of avascular
necrosis and can occur after trauma or an identifiable inciting
injury (6). Chronic SCFE, accounts
for ~85% of cases, and implies at least 3 weeks of symptoms.
Patients with predisposing symptoms of pain and limping, who then
experience a new injury exhibit immediate worsening, the so-called
acute-on-chronic slip (7). Loder
et al (8) introduced the
concept of physeal stability, categorizing SCFE as either stable or
unstable based on the subject's ability to bear weight.
A patient with unstable SCFE experiences severe hip
pain that does not allow for a normal gait (8). The patient will often have a medical
history involving the hip, thigh and/or knee pain, and a previous
trauma (usually minor and does not justify the condition alone). An
affected patient tends to externally rotate the affected hip and
counteracts any passive movement of the hip when lying down. The
rate of osteonecrosis in unstable SCFE is increased to ~24%
(9). Additional grading is based on
the radiographic severity, which is described by epiphyseal
displacement as a fraction of the total physeal diameter (10). Using this grading, slips can be mild
(<33%), moderate (33-50%) or severe (>50%). One of the most
commonly used classifications is the slip angle of Southwick
(11), in which the difference in
the angle subtended by the proximal femoral physis and the
ipsilateral femoral shaft are compared between affected and
unaffected sides (12). SCFE
requires surgical management, except in rare instances, as
stabilization of the epiphysis and early fusion of the proximal
femoral physis prevents further displacement.
Regarding scoliosis, it is defined as a lateral
curvature of the spine >10˚ on a radiograph, which is typically
associated with spinal rotation. The three types of scoliosis are
congenital, idiopathic and neuromuscular. Idiopathic scoliosis
specifically is classified into infantile idiopathic scoliosis,
which is identified in patients <3 years old; juvenile
idiopathic scoliosis, which appears in children aged 3-10 years,
and adolescent scoliosis in patients >10 years (13). Dickson and Archer (14) proposed a two-group classification
system that included early onset (≤5 years old) and late onset (≥6
years old) scoliosis, since juvenile scoliosis is rare (15,16)
The prevalence of curves >30˚ is ~0.2%, and it is <0.1% for
curves ≥40˚ (17).
The main cause of Adolescent Idiopathic Scoliosis
has not been precisely identified, and it may be multifactorial.
Genetics are hypothesized to play a leading role in the occurrence
of scoliosis; however no mode of inheritance has been identified as
of yet, to the best of our knowledge. Skeletally immature patients
have a risk of curvature progression of ~20% for curvatures of 20˚,
a risk of 60% at 30˚ and 90% at 50˚ (15). More severe curves are often
associated with physical problems, such as increased back pain,
cardiorespiratory dysfunction proportional to the severity of the
curve, and an increased risk of pulmonary heart disease and death
with curves >100˚ (18).
Additionally, the psychological distress is also elevated with
greater curvatures.
The aim of this case report is to present a rare
case of acute-on-chronic SCFE in a patient undergoing surgical
fixation of idiopathic scoliosis.
Case report
A male patient aged 14 with a health record of
supraventricular tachycardia under medication for the past 2 years,
BMI=30 kg/m2 and chronic SCFE of the left hip, was
admitted to the Department of Spine Surgery and Scoliosis at KAT
General Hospital, for surgical fixation of idiopathic scoliosis of
the thoracic spine, with a Cobb angle of 45˚. Left hip SCFE was
irrelevant to the existing scoliosis and curvature, as there are no
case series available in the literature describing any relevance
between the scoliosis curvature and the hip SCFE, to the best of
our knowledge.
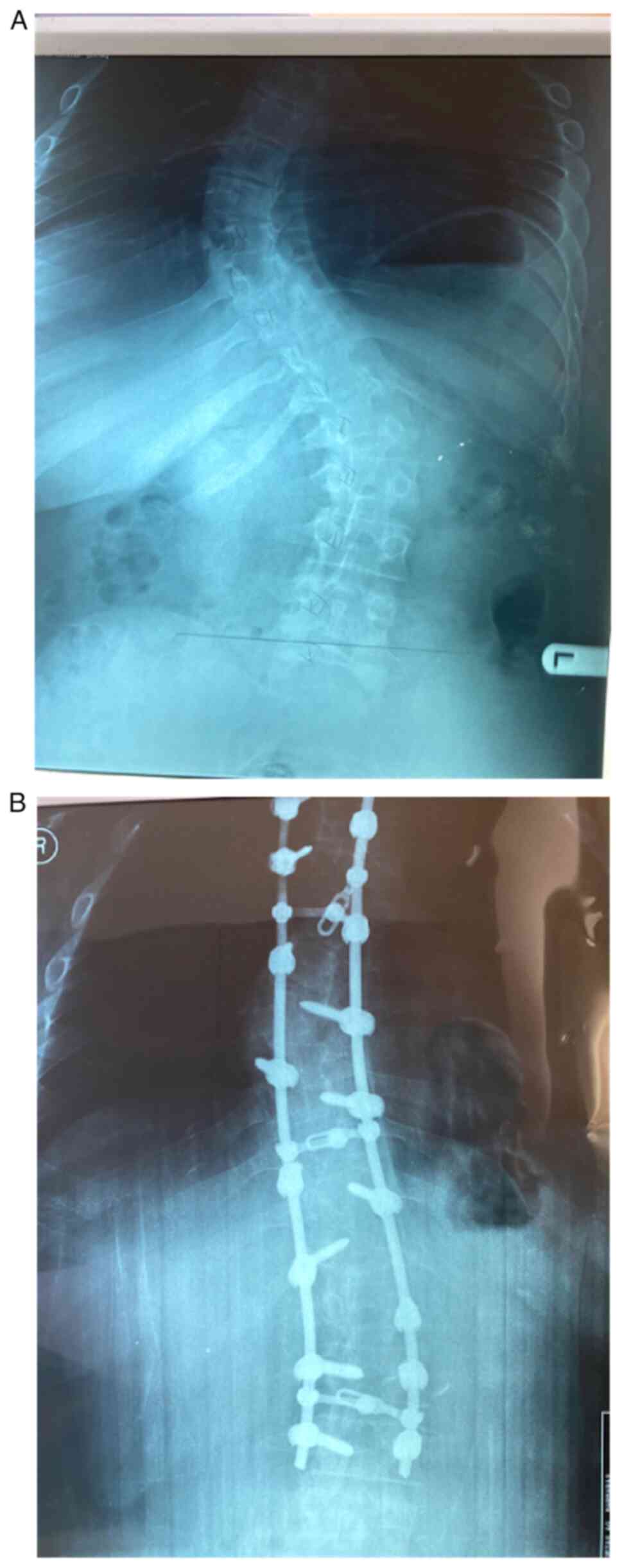
A posterior lumbar fusion with instrumentation from
T3 to L3 was performed under general anesthesia; however,
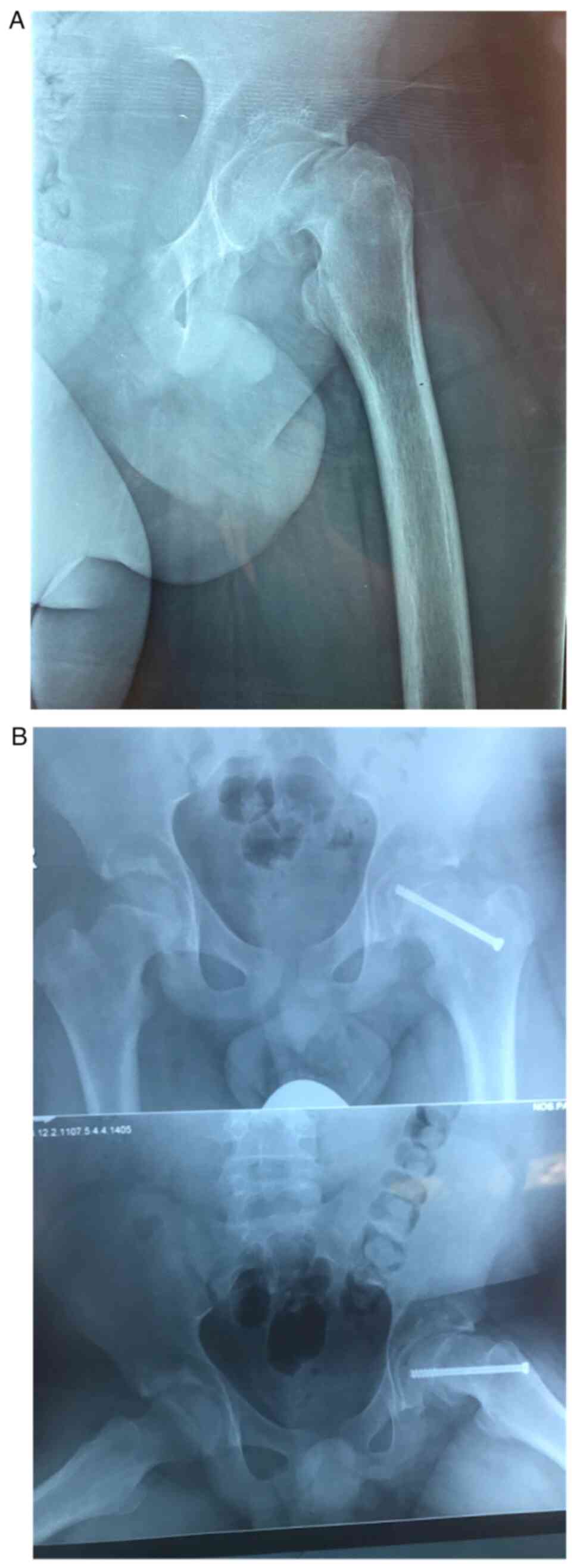
post-operatively the patient reported acute pain in the left hip
joint. Emergent postoperative imaging revealed an acute SCFE on the
grounds of the chronic SCFE on the left hip. However there were no
available pre-operative pelvic radiographs in the patient's history
regarding an existing SCFE of the left hip. The patient was
immediately referred to the Second Department of Orthopaedics at
the ‘Agia Sofia’ Children's Hospital of Athens to undergo surgical
intervention for the SCFE. The patient underwent percutaneous pin
fixation of the left hip with a single screw, and discharged
without any events. During a follow-up on 1 month after the
operation, the patient showed both clinical and radiological
recovery. On the last follow-up, 3 years after the operation, the
patient was satisfied with his recovery, with a VAS score of
98/100, and he reported a full return to his daily activities. The
patient provided informed consent for publication of this case
report (Figs. 1 and 2).
Discussion
Reviews of large national databases in the USA
report an SCFE incidence rate of 10,117 per 100,000, with a 1.4:2.0
female/male ratio (1). The average
age of diagnosis is 12 years, and the majority of patients who
present with SCFE who are outside the age range of 10-16 represent
atypical SCFE, possibly associated with endocrinological diagnoses
(2). Although a common presentation
of SCFE is that of an obese, hypogonadal male during an adolescent
growth spurt, most SCFEs occur in the absence of an endocrine
disorder (3). Conversely, the goal
of scoliosis management is to prevent further progression of the
curvature. Management decisions are made based on the curve
severity at presentation, pattern and location of curvature, and
growth potential of the patient (chronological age, menarche status
and Risser sign) (13). The
majority of adolescents will not require intervention and <10%
require active treatment (17).
Management options include observation and nonsurgical or surgical
treatment. The goals of surgical treatment are to prevent
progression, achieve maximal permanent correction of deformity,
improve appearance and keep short-term and long-term complications
to a minimum. Surgery is typically performed in patients with Cobb
angles >45˚; however, additional factors, including age, curve
progression and symptoms, such as pulmonary compromise, are
important factors to be considered (19,20).
The presence of an acute slipped femoral capital on
an existing chronic SCFE simultaneously with surgical fixation of
idiopathic scoliosis has not yet described in the existing
literature, to the best of our knowledge. Of particular interest in
this case is the cause of the acute slippage of the femoral capital
right post-operatively. The patients position during the surgical
instrumentation of the spine, which is a prone position under
general anesthesia in four post frame with both hips at 90˚
flexion, could be a reason that is likely to have led to this
event. Additionally, the metabolic status of the patient, which
included obesity, chronic asthma and cardiac tachyarrhythmias under
ablation and constant medication, may have also contributed to the
factors that led to a slipped femoral capital from the beginning.
Prevention of the progress of any existing SCFE in patients
undergoing spinal surgery is essential, including thorough
radiographic pre-operative control and analysis of their detailed
medical history.
In conclusion, the current case report, which is
extremely rare in the current literature, describes the
significance of pre-operative planning for each procedure in
pediatric orthopedic surgery, particularly in patients with a
medical history. The spinal surgeon should consider, in every acute
change, the clinical presentation of the patient, especially in the
hip after surgical interventions of the spine in pediatric
patients, as SCFE is quite common during early adolescence.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
EP, FK, IAT and PK collected the patients' medical
information and scientific data, analyzed them and wrote the
manuscript. IC and JA conceived the study, interpreted the data and
edited the manuscript.. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient consented for publication of their
data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Georgiadis A and Zaltz I: Slipped capital
femoral epiphysis: How to evaluate with a review and update of
treatment. Pediatr Clin North Am. 61:1119–1135. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Loder RT, Starnes T and Dikos G: Atypical
and typical (idiopathic) slipped capital femoral epiphysis.
Reconfirmation of the age-weight test and description of the height
and age-height tests. J Bone Joint Surg Am. 88:1574–1581.
2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mann DC, Weddington J and Richton S:
Hormonal studies in patients with slipped capital femoral epiphysis
without evidence of endocrinopathy. J Pediatr Orthop. 8:543–545.
1988.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kocher MS, Bishop JA, Weed B, Hresko MT,
Millis MB, Kim YJ and Kasser JR: Delay in diagnosis of slipped
capital femoral epiphysis. Pediatrics. 113:e322–e325.
2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kaplan SR and Klinghoffer L: Knee pain in
slipped femoral capital epiphysis causing a delay in diagnosis. Am
J Surg. 101:798–802. 1961.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Aronsson DD and Loder RT: Treatment of the
unstable (acute) slipped capital femoral epiphysis. Clin Orthop
Relat Res. 99–110. 1996.PubMed/NCBI
|
|
7
|
Aadalen RJ, Weiner DS, Hoyt W and Herndon
CH: Acute slipped capital femoral epiphysis. J Bone Joint Surg Am.
56:1473–1487. 1974.PubMed/NCBI
|
|
8
|
Loder RT, Richards BS, Shapiro PS, Reznick
LR and Aronson DD: Acute slipped capital femoral epiphysis: The
importance of physeal stability. J Bone Joint Surg Am.
75:1134–1140. 1993.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zaltz I, Baca G and Clohisy JC: Unstable
SCFE: Review of treatment modalities and prevalence of
osteonecrosis. Clin Orthop Relat Res. 471:2192–2198.
2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wilson PD, Jacobs B and Schecter L:
Slipped capital femoral epiphysis: An end-result study. J Bone
Joint Surg Am. 47:1128–1145. 1965.PubMed/NCBI
|
|
11
|
Southwick WO: Osteotomy through the lesser
trochanter for slipped capital femoral epiphysis. J Bone Joint Surg
Am. 49:807–835. 1967.PubMed/NCBI
|
|
12
|
Loder RT: Effect of femur position on the
angular measurement of slipped capital femoral epiphysis. J Pediatr
Orthop. 21:488–494. 2001.PubMed/NCBI
|
|
13
|
Burton MS: Diagnosis and treatment of
adolescent idiopathic scoliosis. Pediatr Ann. 42:e233–e237.
2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Dickson RA and Archer IA: Surgical
treatment of late-onset idiopathic thoracic scoliosis. The leeds
procedure. J Bone Joint Surg Br. 69:709–714. 1987.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bunnell WP: The natural history of
idiopathic scoliosis. Clin Orthop Relat Res. 20–25. 1988.PubMed/NCBI
|
|
16
|
Roach JW: Adolescent idiopathic scoliosis.
Orthop Clin North Am. 30:353–365, vii-viii. 1999.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Miller NH: Cause and natural history of
adolescent idiopathic scoliosis. Orthop Clin North Am. 30:343–352,
vii. 1999.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tambe AD, Panikkar SJ, Millner PA and
Tsirikos AI: Current concepts in the surgical management of
adolescent idiopathic scoliosis. Bone Joint J. 100-B:415–424.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kim HJ, Blanco JS and Wildmann RF: Update
on the management of idiopathic scoliosis. Curr Opin Pediatr.
21:55–64. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chowdhry M, Matsen Ko L, Franklin C and
Parvizi J: Reactive scoliosis: A challenging phenomenon in
adolescent patients with hip arthritis. Arthroplast Today.
3:160–163. 2017.PubMed/NCBI View Article : Google Scholar
|