Introduction
Millimeter-wavelength electromagnetic waves (MWs)
possess wavelengths of 1-10 mm. A healthy living cell is
characterized by a spectrum of acoustoelectric oscillations (normal
oscillations) in the plasma membrane that belong to the MW range,
with the amplitude lowering and fading away when a cell is impaired
resulting in loss of viability and death (1,2). The
biological effects of electromagnetic irradiation depend on
characteristics such as induction, frequency and duration of
exposure. The short-wave range (30-300 GHz), corresponding to the
cell's natural oscillations, is the most attractive range for
investigations (3-5).
It is considered that the MW action on the cells leads to the
correction or restoration of their natural oscillations, which
results in increased membrane stability and the maintenance or
extension of the cell viability. Millimeter-wave irradiation is
applied for complex therapy (Millimeter Wave Therapy; MW therapy)
of various diseases, such as diabetes, cardiovascular and skin
diseases, rheumatoid arthritis and disorders of the male
reproductive system (6,7). For example, the complex treatment of
chronic prostatitis includes MW therapy with wavelengths of 7.1 or
5.6 mm, and an exposure duration of 20 mins (5).
Despite the increased interest in bioelecromagnetic
studies in the recent years, the mechanism of MW action remains
incompletely understood. A possible explanation of its therapeutic
effects includes its direct and indirect interaction with the skin
structural components and further neurogenic activation of
endogenous opioid systems, and is further discussed in a more
specific review (2). However, there
is very little information on the influence of MW on seminal
liquid, male gametes, and their apoptosis in particular.
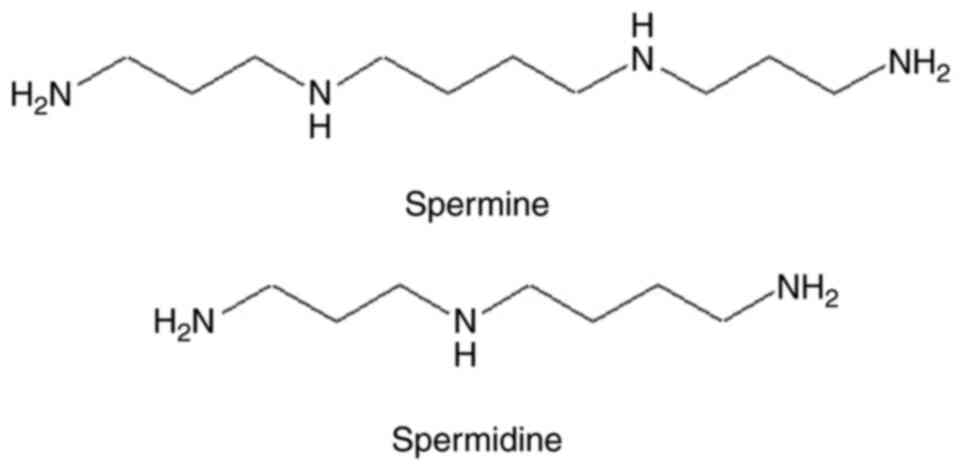
One of the most abundant components of the seminal
plasma is polyamines (PAs), which are widely present in all tissues
and biological fluids of the body (Fig.
1). They are essential for cell growth, cell proliferation and
differentiation (8,9), and have the ability to coordinate the
process of cell apoptosis (9-13).
The contents of the PAs spermine (Spm) and spermidine (Spd) in the
seminal plasma are significantly higher than in any other
biological fluid, which highlights the importance of these low
molecular weight organic polycations for human reproductive
function, especially in men (10,14).
However, there is a lack of studies aiming to understand the roles
of the human seminal plasma PA. It has been established that higher
PAs levels, such as that of Spd and Spm, are produced by the
prostate gland from putrescin and decarboxylated SAM, participate
in the regulation of the pH of seminal plasma, stabilize the
structure of sperm DNA, activate the motility of gametes, and are
considered to be a de-capacitating factor that participates in the
regulation of the sperm membrane integrity during fertilization
(8,14-16).
The cell membranes are considered the main targets for MW at the
molecular level (2,17). In this regard, the influence of
short-term low-intensity MW exposure on the sperm cell membranes
and the role of the seminal plasma components are of interest. It
was hypothesized that if any biological effects of the MW
irradiation on the sperm cells can be detected then the PA may be
involved in the development of these effects. The current study
aimed to reveal the biological effects of microwaves on male
gametes and the role of PA in the realization of these effects.
Materials and methods
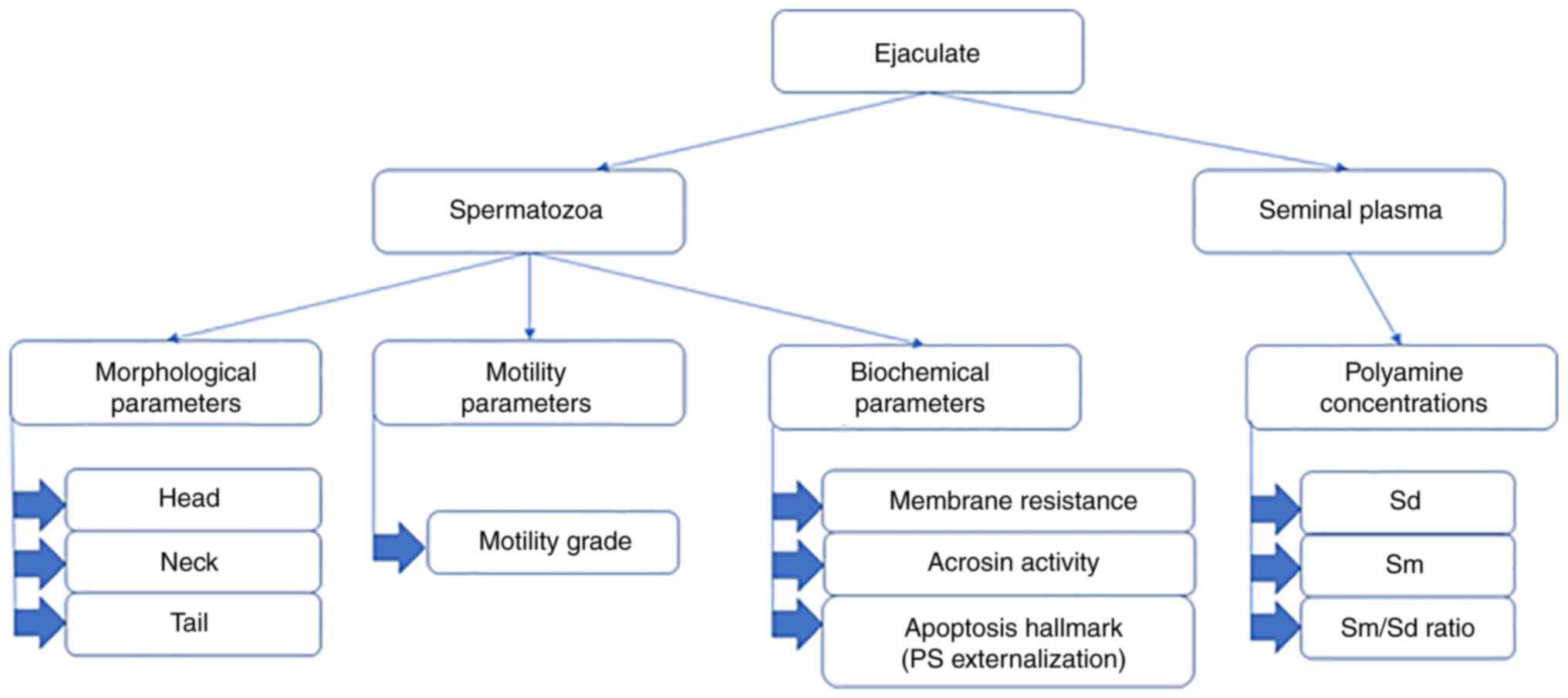
Study design
The ejaculates of healthy fertile men (n=25) aged
from 22-38 years old (y.o.) [(30.6±1.1 y.o. (mean ± SEM)], and of
subfertile men (n=78) aged 25-48 y.o. (34.1±0.8 y.o.) were studied.
The identification of normal and subfertile samples was based on
the spermogram parameters described below. As the investigation was
performed with participation of the Reproduction Center, the
preliminary basis for the identification of samples as subfertile
was also the inability for the donors to have children. The
durations of ‘barren marriages’ ranged from 6 months to 15 years.
No reproductive organ diseases were diagnosed in donors with
abnormal spermograms, the donors did not abuse alcohol and were not
smokers. The fertile samples were taken from the donors who had
children in the previous 3 years.
First, we studied the influence of MW irradiation on
spermatozoa from healthy donors. The whole ejaculate after complete
liquefaction were examined for the standard spermogram parameters.
Each sample was divided into three parts: Control F,
Exp1 F and Exp2 F. The Control F
was not exposed to the MW irradiation, Exp1 F was
exposed to the MW irradiation as a whole ejaculate, and Exp2
F was centrifugated at 12,580 rcf for 15 min at room
temperature, and divided into seminal plasma and sperm cells, after
which the seminal plasma and spermatozoa were exposed to MW
irradiation separately from each other. The Control F
and Exp1 F group, after MW exposure, were then also
centrifuged as above, and divided into seminal plasma and
spermatozoa. The seminal plasma and spermatozoa from all three
experiments were used for the specific assays. The spermogram
parameters were also evaluated in the Exp1 F and Exp2
F groups after MW exposure. Next, the effect of MW
treatment on spermatozoa with regard to metabolic processes was
assessed. The ejaculates from donors with pathospermia (Control
S, Exp1 S) were exposed to the MW treatment
and processed similarly to those of healthy donors. Figs. 2 and S1 outlines the study design briefly.
Ethical approval
The present study was performed in accordance with
The Code of Ethics of the World Medical Association (Declaration of
Helsinki) (18) and was approved by
the Local Ethics Committee of the Astrakhan State Medical
University of the Health Ministry of the Russian Federation
(protocol no. 2; 21st May 2021). Informed consent for participation
in the study and use of their samples was obtained from all
participants.
MW field generation
The electromagnetic field was produced by a
generator of monochromatic electromagnetic waves ‘Yav-1-7.1’
(Scientific Production Association, Istok). The MW parameters
(λ=7.1 mm, υ=42.194 GHz) as well as the duration of the experiment
have previously been determined to induce the intended bioeffects
without a heating effect, and are recommended for clinical and
experimental use (4,5,19). The
absence of a thermal effect ensured the specificity of biological
action (5,19,20).
Spermatozoa investigation
The assessment of the primary standard spermogram
parameters was performed according to the generally accepted
methods recommended by WHO and leading experts (21,22).
Microscopic studies of sperm were performed on a transmission
electron microscope; morphology and motility characteristics were
explored (21,22). The motile sperm cells were counted
using a Goryaev chamber. All these parameters were determinants for
the verifying the samples as normal or subfertile ones at the zero
point of the study. The biochemical investigations included
membrane resistance tests, acrosin activity assay and apoptosis
investigation by evaluation of PS externalization by
AnnexinV-propidium iodide (PI) staining.
Membrane resistance assessment
The sperm membrane resistance to the 1% sodium
chloride solution (Milovanov test) was explored (23). Briefly, the ejaculate was diluted
gradually with 1% sodium chloride solution and incubated for 3 min
at 37˚C with counting of motile sperm cells. The first dilution
(1:500) was performed by adding 10 ml 1% sodium chloride solution
to 0.02 ml ejaculate, next dilutions (1:1,000, 1:2,000, 1:4,000,
1:6,000, etc.) were obtained by adding 0.5 ml volumes of 1% NaCl
solution to the corresponding volumes of the first diluted (1:500)
solution. The number of motile sperms were counted in ejaculate
samples before and 3 min after each dilution under a light
microscope (magnification, x100), using a Goryaev chamber, and
accordance with methods recommended by WHO and leading experts
(21,22). The diluting was performed gradually
starting from 1:500 up to the complete cessation of spermatozoa
motility (23). The higher the
dilution at which the motility remained, the greater the membrane
resistance was considered to be. The membrane resistance was
evaluated in equivalent units (EU) corresponding to the degree of
dilution; for example, if the highest dilution maintaining sperm
motility was 1:4,000, then the resistance was considered 4,000 EU.
The mean ± SEM were then calculated.
The membrane resistance to acetic acid was evaluated
in the Joel test (23). The
ejaculate was diluted with 0.5% acetic acid solution (1:1) and
incubated at 37˚C. At 0 h (before the dilution) and every 10 min
after dilution, the number of motile spermatozoa was counted in the
ejaculate samples, up to the complete cessation of motility. The
duration of motility in these conditions was a marker of membrane
resistance.
Acrosine activity assay
The spermatozoa were washed using PBS (pH 6.5) to
remove the seminal plasma and extracted with 0.2 M acetate buffer
(pH 2.4). The activity of free acrosine (EC 3.4.21.10) was
determined spectrophotometrically as described by Schill (24). Briefly, benzoylarginine ethyl ester
was hydrolyzed by acrosine producing ethanol, the latter was then
assayed in an alcohol dehydrogenase reaction with formation of
NADH(H+) detected at 366 nm (24) on the Novaspec III spectrophotometer
(Amersham Biosciences). The total activity of acrosin was
determined following rapid thawing (at 23˚C for 30 min) of the
pre-frozen (at -196˚C liquid nitrogen) ejaculate. The pro-enzyme
activity was calculated by subtracting the activity of free
acrosine from the total acrosine activity. Acrosin activity was
expressed in international units per 1 million spermatozoa
(µU/106 cells) (24,25).
Apoptosis investigation
Sperm cells were washed to remove the seminal plasma
and incubated in Menezo B-2 medium (BioMerieux) in a humidified
incubator with 5% CO2 at 37˚C. The apoptotic process of
gametes was assessed using fluorescein-labeled Annexin V (AnV),
which binds to PS residues on the membrane surface of apoptotic
cells, and PI, a fluorescent DNA dye that allows differentiation of
cells with damaged membranes from those with intact membranes. The
FITC Annexin V Apoptosis Detection Kit was purchased from BD
Biosciences, Inc, and used according to the manufacturer's
protocol. During the early stage of apoptosis, cells bind AnV, but
like living cells, are impermeable to PI, therefore, they are
AnV+/PI-. The percentage of such cells among the total number of
cells was calculated (10,11). The microscopic studies were
performed on a fluorescent microscope at a magnification of x100.
The AnV+/PI-(green fluorescence without red fluorescence) cells
were counted using a Goryaev chamber.
Assay of PA levels
PA was extracted from seminal plasma using n-butanol
(1:1; pH=10) for 1 h at room temperature, and after evaporation of
the butanol phase, the remaining solution was electrophoretically
separated in 1.5% agar gel with 0.1 M citric acid buffer
(pH=3.4-3.6) for 1 h at room temperature, with a voltage of 200 V
and an amperage of 40 mA (Patent for invention RUS no. 2225981
dated 28.02.2002). Spm and Spd were visualized as pinkish-violet
spots after staining with ninhydrin and identified using standard
solutions (Fluka). The amount of PA in the sperm plasma of each man
was determined using scanning electrophoregrams, transferring the
image into a digital format on a PC using a specific computer
program ‘PN 5108’ (certificate of registration of a computer
program: RUS 2003612170 dated 21.07.2003). The concentrations of
Spm and Spd were calculated using a classical calibration curve
(plots reflecting the concentration-dependent peak areas for the
standard PA solutions). The method was tested with natural semen
samples (n=10) and showed the linearity within the working range of
0.05-40 µmol/ml, the detection limit for seminal plasma PA was
0.064 µmol/ml, variability interval 0.4 µmol/ml, maximum relative
error ≤15%.
Statistical analysis
Statistical evaluation was performed after checking
the distribution for normality (Shapiro-Wilk test) in Statistica
version 7.0 (StatSoft Inc.). Comparisons between the studied values
were assessed using an unpaired Student's t-test (P<0.05) or a
one-way ANOVA followed by a post-hoc Tukey's test for multiple
comparisons in Microsoft Excel 2016 (Microsoft Corporation) or SPSS
version 24 (IBM Corp.), respectively. Data are presented as the
mean ± SEM. Assessment of the correlation between parameters was
performed using a Pearson correlation coefficient analysis (r).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Characteristics of the spermatozoa of
the fertile donors
The standard spermogram characteristics were
obtained for the sperm cells from Exp1-2 F and Control
F samples (Fig. S2A).
An extended cytological study of the spermatozoa of fertile men did
not reveal significant changes in the number of the head
(amorphous, small, tapered, round, double-headed forms, etc.), neck
(‘bent’ neck, thin midpiece, etc.) or tail defects (two-tailed
forms, a short tail, etc.) in the experimental samples after
exposure to low-intensity MW irradiation compared to the Control
Samples (P>0.05, Table SI).
Also, no alterations in the motility of the spermatozoa were
observed after MW treatment of fertile men spermatozoa both in Exp1
F and Exp2 F (P>0.05, Table SII).
The evaluation of the functional state of sperm
membranes by their resistance to 1% sodium chloride solution
revealed that a short-term exposure to MW radiation resulted in a
26% increase in membrane resistance when applied to the whole
ejaculate (Exp1 F), and in a 17% increase when the cells
were separated from the plasma (Exp2 F). These findings
are summarized in Table I.
 | Table IChanges in the resistance of sperm
membranes and in apoptosis of fertile men after low-intensity
millimeter-wavelength electromagnetic wave exposure. |
Table I
Changes in the resistance of sperm
membranes and in apoptosis of fertile men after low-intensity
millimeter-wavelength electromagnetic wave exposure.
| Parameter | Control
F | Exp1
F | Exp2
F | p0-1 | p0-2 | p1-2 |
|---|
| Membrane resistance
to sodium chloride, EUc |
4,250.32±320.63 |
5,325.41±291.80 |
4,963.01±278.91 | 0.033a | 0.214 | 0.666 |
| Percentage of
AnV+/PI-spermatozoa,%c | 10.47±0.50 | 8.50±0.39 | 10.39±0.67 | 0.028a | 0.993 | 0.037a |
| Apoptotic
indexc,d | NA | 0.81±0.02 | 0.99±0.01 | NA | NA |
<0.01b |
The Joel test showed a significant increase in
spermatozoa resistance to acetic acid after the MW treatment. The
differences in both the Control F and the Exp
F were insignificant when incubated for <10 min, but
after 20-30 min of incubation, the differences became statistically
significant (P<0.05). Generally, the motility of sperm in
samples after MW exposure was maintained for ~10 min longer than in
Control F samples (Table
SIII).
PS externalization in the spermatozoa
of fertile donors
The next step of the present study was the
determination of apoptotic markers in spermatozoa. The results are
presented in Table I; Fig. S3A and B, E and
F. The content of АnV+/PI-sperms
in the Control F group was 10.47±0.50%. The percentage
of these early apoptotic gametes was reliably reduced by almost 20%
(P<0.01) in Exp1 F after MW exposure. The changes in
the content of АnV+/PI-spermatozoa in the Exp2 F did not
significantly differ rom the Control F (P>0.05). To
make the results of the short-term MW impact assessment more
demonstrative, the apoptosis index (AI) was calculated as follows:
AI=Apoptotic percentage the in experimental group/apoptotic
percentage in the Control F group.
This index shows the ratio of the AnV+/PI- gametes
after exposure to the MW radiation (Exp1 F) to the
number of such cells in the Control F group. AI values
<1 (as in the Exp1 F group) were indicative of
inhibition of apoptosis in gametes. The sodium chloride resistance
of sperm membranes after MW exposure (Exp1 F) correlated
inversely with the content of AnV+/PI- spermatozoa in ejaculates
(r=-0.5; P<0.01) and with AI (r=-0.4; P<0.05).
Enzymatic activity of acrosine in
spermatozoa of fertile donors
The determination of the enzymatic activity of
acrosine is used as a diagnostic test for evaluating spermatozoa
fertilization in vitro (24,25).
Serine proteinase EC 3.4.21.10 acrosine is one of the key acrosomal
enzymes and plays an important role in the process of oocyte
fertilization (25). However, there
is no data on the functioning of the acrosine system under the
influence of MW-irradiation in the available literature. The
activity of free acrosine was significantly lower in the
experimental samples, particularly in Exp1 F, and was
87% of that observed in the Control F group (Table II). The total activity of acrosin
did not change compared with the Control F group. The
pro-enzyme activity of acrosin in ejaculate samples after
MW-exposure compared to the control did not increase significantly,
increasing by ~4% (Table II). The
ratio of pro-acrosin/free acrosin was calculated, and its value
increased on average by almost 20% in Exp1 F compared
with the Control F (Table
II).
 | Table IIAcrosin activity in the spermatozoa
of fertile donors before and after the low-intensity
millimeter-wavelength electromagnetic wave exposure. |
Table II
Acrosin activity in the spermatozoa
of fertile donors before and after the low-intensity
millimeter-wavelength electromagnetic wave exposure.
| Enzyme
activity | Control
F | Exp1
F |
|---|
| Free acrosin
activity, µU/106 cellsb | 1.34±0.07 |
1.17±0.05a |
| Total acrosin
activity, µU/106 cellsb | 5.16±0.15 | 5.15±0.13 |
| Pro-acrosin
activity, µU/106 cellsb | 3.82±0.12 |
3.98±0.12a |
| Pro-acrosin/free
acrosin ratiob | 2.85±0.11 |
3.40±0.12a |
PA concentrations in seminal plasma of
fertile donors
The next step of the study was to reveal the role of
the seminal plasma PA on the effect of MW on spermatozoa. The
assessment of the PA content was performed on Control F,
Exp1 F and Exp2 F groups. The Control Samples
showed that the concentration of Spm was 1.197±0.111 µmol/ml, and
Spd was 1.265±0.150 µg/ml (Table
III, Fig. 3). The MW treatment
caused a significant decrease in the concentrations of both PAs in
the Exp1 F group (P<0.05). The Spd concentration
changed to a greater degree, so these alterations were not just
quantitative, but also involved the profile of PA content. The
change in the spectrum of PA levels in the seminal plasma after MW
exposure is illustrated by the shift in the Spm/Spd ratio
(0.95→1.22). The PA concentrations after MW treatment were not
altered in the absence of spermatozoa (Exp2 F,
P>0.05, Table III). However
strong correlations (r=0.9, P<0.05) between the number of
apoptotic cells and PA levels were observed for the Control
F and Exp1 F samples.
 | Table IIIThe concentration of polyamines in
the seminal plasma of fertile donors after low-intensity
millimeter-wavelength electromagnetic wave exposure in the presence
(Exp1 F) and absence (Exp2 F) of the sperm
cells. |
Table III
The concentration of polyamines in
the seminal plasma of fertile donors after low-intensity
millimeter-wavelength electromagnetic wave exposure in the presence
(Exp1 F) and absence (Exp2 F) of the sperm
cells.
| Parameter | Control
F | Exp1
F | Exp2
F | p0-1 | p0-2 | p1-2 |
|---|
| Spm,
µmol/mlc | 1.197±0.111 | 0.803±0.092 | 1.178±0.126 | 0.036a | 0.992 | 0.049a |
| Spd,
µmol/mlc | 1.265±0.152 | 0.804±0.055 | 1.281±0.145 | 0.030a | 0.996 | 0.024a |
|
Spm/Spdc | 0.95±0.03 | 1.22±0.03 | 0.93±0.05 |
<0.001b | 0.944 |
<0.001b |
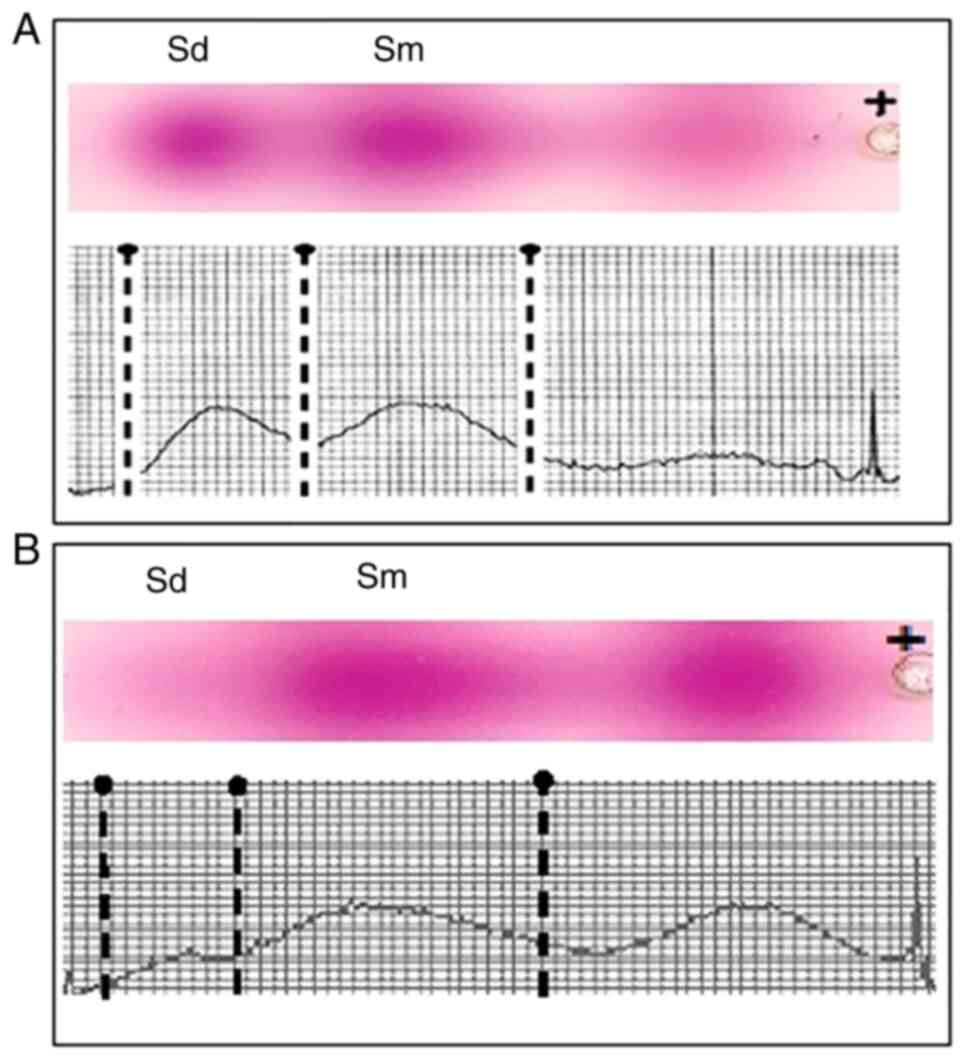
The PA electrophoregram and densitogram of seminal
plasma of a fertile man before and after the exposure of the
ejaculate to low-intensity MW are shown in Fig. 3. Two separate spots can be seen on
the platelets corresponding to Spd and Spm visualized in the
ninhydrin reaction. An additional spot of unknown substance appears
in the electrophoregram after MW exposure. This substance is
present not far from the PA, therefore it may be considered as a
substance similar to PAs. At the same time its velocity of
migration is lower than that of PA, suggesting it has a different
molecular weight/charge ratio. Presumably this spot might belong to
an acetylated Spd or Spm. Unfortunately, it was not possible to
determine the identity of the molecule accounting for this spot due
to a lack of standard components, and will thus form the focus of
future investigations.
The results gained for the fertile samples provide
evidence of the positive action of MW treatment, such as the
increase in membrane stability and improved functionality of
spermatozoa (lowered acrosin activity, inhibition of apoptosis).
This effect was observed mainly for the complete ejaculates against
the background of seminal plasma PA levels lowering, and was absent
or less pronounced in the sperm cells exposed to MW in the absence
of seminal plasma. The PAs did not ‘disappear’ from the
spermatozoa-free plasma (Exp2 F) after MW treatment.
Taken together these results reveal the involvement of the PA
system on the effect of MW upon sperm cells.
Characteristics of the spermatozoa
from the subfertile samples
The investigation of the influence of MW irradiation
on spermatozoa of subfertile samples was performed in order to
reveal any potential therapeutic effects (Fig. S2B; Fig. S3C and D). The complete ejaculates were tested
only (Control S and Exp1 S).
Due to the large variability in the parameters of
spermograms of the patients in the group of pathospermia, the
changes in the morphology of the gametes, in the functional state
of their membranes and in PS externalization as a marker of sperm
apoptosis, were not statistically significant (all P>0.05). The
reaction of subfertile spermatozoa to MW differed from that of the
normozoospermia samples. In particular, the number of progressively
motile gametes increased to 24% (Exp1 S) from 16%
(Control S), while the number of non-progressively
motile spermatozoa decreased from 20% in Control S to
12% in Exp1 S (P<0.05, Table IV). The quantity of immotile
spermatozoa did not change significantly (P>0.05, Table IV).
 | Table IVMotility of spermatozoa from
subfertile men before and after exposure to the
millimeter-wavelength electromagnetic wave irradiation. |
Table IV
Motility of spermatozoa from
subfertile men before and after exposure to the
millimeter-wavelength electromagnetic wave irradiation.
| | Spermatozoa
percentage, % | |
|---|
| Spermatozoa
motility characteristics | Control
S | Exp1
S | P-value |
| Progressively
motile, % | 16.9±2.3 |
24.0±1.3a | P<0.05 |
| Non-progressively
motile, % | 20.3±2.4 |
12.1±1.7a | P<0.05 |
| Immotile, % | 62.8±1.3 | 63.9±1.5 | P<0.05 |
PA concentrations in the seminal
plasma of subfertile samples
First the levels of PA in the spermoplasm of
subfertile men revealed that their levels drastically differed from
those of fertile men, in particular the residual concentration of
Spm and Spd was 58 and 15% from that of healthy donors,
respectively. The study of the dynamics of the PA in the subfertile
spermoplasm after MW treatment revealed two types of responses. In
the first type, there was no significant change in the levels of
PA, there was only a slight tendency to an increase in the levels
of Spd, although this increase was not significant. In the second
type of response, both Spm and Spd levels were significantly
decreased, which resembled the response in normozoospermia and led
to an increase in the Spm/Spd ratio.
Discussion
The parameters applied in the MW-electromagnetic
field are in accordance with those that are already
well-characterized and are known to induce a positive biological
effect without heating. These frequencies and regimens are applied
in therapeutic purposes, namely for the treatment of chronical
prostatitis (3,5). The duration of treatment in the
present study was within the therapeutically applied parameters. An
alternative to the constant EM field is a pulsed-radiation that is
used in telecommunication systems. The lack of the specific
equipment has limited our investigation to the constant field only.
Our preliminary experiments included the 20 and 40 min MW
exposures, but the results within this range of time exposures did
not differ (data not shown), therefore the experiments in the
present study were limited to 20 min of exposure only.
There have been several theories suggested that may
explain the effect of MW on cells. For example, changes in cell
membranes, water molecule rotation induced by MW, and direct and
indirect stimulation of nerve pathways are among possible mediators
of the actions of MW (1,2,6). The
aim of the present study was to determine any effect of MW on the
complete ejaculate and the role of the seminal plasma PA on the
effects of MW. The investigation of low-intensity MW radiation
impact on sperm cells in their native seminal plasma environment
and on isolated sperm cells (in cultural liquid) showed this
treatment increased sperm membrane stability and lowered apoptosis
of the sperm cells. The effect did not appear at the level of
morphology or motility of the cells, which is an expected result,
since it is unlikely that a short-term exposure can cause visible
morphological changes in spermatozoa (2,6).
A documented positive effect of MW irradiation
identified in the present study is the increased sperm membrane
stability, and this is consistent with the previous literature
reports (2-4).
To assess the functional state of sperm membranes, two methods were
used: i) A method using an external factor with increasing strength
(sodium chloride solution, Milovanov test) and ii) a method using a
constant external factor acting over an elongated time period
(acetic acid, Joel test). Both methods showed an increase in the
resistance of the membranes of sperm cells of fertile men after
exposure to MW. A more pronounced stabilizing effect was observed
for the cells in the presence of seminal plasma PA than in the
cultural liquid. The inhibition of cell apoptosis was correlated
with the degree of membrane stabilization and with the PA
concentrations.
The function of the acrosomal enzyme acrosin is
fundamental for ensuring the realization of the procreative
function of spermatozoa, and is closely related with the state of
the spermatozoa membranes (25).
The results of the present study indicated that in normozoospermia,
the MW treatment resulted in an increase in the pro-acrosin/free
acrosin ratio; thus, the premature activation of acrosin was
prevented, which is a favorable factor contributing to the
effective realization of the fertilizing activity of spermatozoa.
The increase in the pro-enzyme activity of acrosin may have been
due to a decrease in the activity of free acrosin as a result of
stabilization of the acrosomal membrane of the spermatozoa under
the influence of MW. However, the direct influence of the MW field
on the activity of acrosine by altering its conformation through
modification of its solvate shell cannot be excluded, and it is
likely the case that both mechanisms take place, and the extent of
the effects of each mechanism should be determined.
Spm and Spd (Fig. 1)
belong to the PA group, along with putrescine and cadaverine, which
are often termed diamines (8).
According to our previous results the content of Spm in human semen
ranges from 138.4-21,749.9 µmol/l and Spd from 17.9-1,170.8 µmol/l
(14), while the levels of PA in
the blood serum (and blood plasma) do not exceed 1 µmol/l (26). Thus, the seminal plasma PA
concentration greatly exceeds that of the other tissues, indicating
the importance of PA for normal sperm function (27-29).
The study design included the investigation of PA levels in
separated sperm plasma and in the complete ejaculate. The separated
sperm plasma (Exp2 F) did not show any changes in PA
levels after MW exposure, indicating that the lowering of PA levels
occurred in the presence of the sperm cells only (Exp1
F) and therefore may be attributed to the interaction of
PAs with these cells. Moreover, the lack of direct change in PA
concentration in Exp2 F showed the absence of an effect
on PA from MW irradiation. The mechanism by which PA concentration
was lowered in the Exp1 F group requires further study,
but it is hypothesized that PAs may be taken up by the cells or
absorbed by their membranes. Additional experiments are required to
clarify the fate of the PAs within the sperm cells. The
simultaneous effect of increased sperm membrane stability and
lowered expression of apoptotic markers together with the lowered
PA concentration in the environment (seminal plasma) may indicate
interaction of PA with the membrane and its stabilization through
this interaction. A previous study has reported on the ability of
PA to behave as a membrane-bound component of sperm cells (30). Thus, the uptake of PA by the sperm
cells or PA absorption into the membranes seems like a plausible
possibility. The decrease in concentrations observed for Spd and
Spm were comparable (64 and 67% vs. the Control F,
respectively). The membrane stabilizing effect of the PAs may also
result from the modulation of membrane fluidity under the action of
PA (31), which prevents changes in
the dynamics of the lipids of the cell membrane. Unfortunately, it
was not possible to measure the PA levels inside the sperm cells,
and further studies are required to clarify a possible mechanism by
which PA is taken up by the cells.
Infertility is known to be associated with a change
in PA concentrations in the ejaculate, which seems to influence
gamete viability (14,32,33).
Excessive production of PA results in a decreased number of mature
spermatozoa (34), whereas lowered
PA concentrations in the seminal liquid is correlated with
increased sperm apoptosis (35).
Our results correspond with previous studies, which reported a
decrease in PA levels in subfertile men (27-29).
This decrease may be due to their lowered synthesis or enhanced
degradation of PAs, and should form the focus of future studies. A
possible role in the regulation of sperm apoptosis may be
attributed to these polycationic molecules (35,36).
The antiapoptotic and cytoprotective effect of PA upon cells has
been well documented (8,37-41).
The MW irradiation of specific frequencies may induce apoptosis,
and this effect is studied as a possible therapeutic tool for the
management of cancer (42). The
electromagnetic frequency used in the present study did not result
in an upregulation of apoptotic cell markers compared with the
intact Control F as shown in Table III. One of the methods of
detecting apoptosis is the study of membrane phospholipid
distribution based on Annexin V-PI staining. The predominant
localization of exact classes of phospholipids within the inner or
outer leaflets of the cytoplasm membrane is one of the
prerequisites for maintaining cell viability. Phospholipid
asymmetry in the membrane is disturbed and PS moves to the outer
leaflet; when apoptosis is initiated and the cell loses its
viability (10,12). The results of the present study
demonstrated that PS translocation to the outer leaflet was reduced
after MW treatment when compared with the Control F. The
correlation between the decrease in PA concentration in the seminal
plasma and the decrease in the number of apoptotic gametes in Exp1
F serves as an indirect proof that PA may serve as an
inhibitory factor for apoptosis after MW treatment. Our previous
in vitro studies on human peripheral blood lymphocytes
showed the ability of PA to prevent apoptosis at physiological
concentrations (11). Taken
together, these results suggest that the mechanism of membrane
stabilization and prevention of PS migration to the outer membrane
leaflet under the action of MW radiation involves the seminal
plasma PA system.
Seminal plasma is the natural environment and can be
considered the primary source of PAs for the sperm cells, as the PA
contents (32) and the activity of
PA synthesizing enzymes is considerably higher in seminal plasma
than inside the gametes (43).
Thus, it is possible to conclude that the effects of MW on the fate
of ejaculate seem to be mediated and potentiated by the PA
system.
The comparison of results gained for normospermia
and pathospermia samples reveals some interesting differences. In
fertile samples, exposure to the MW field does not lead to a
significant change in sperm motility, likely due to the motor
potential of a normal spermatozoid being at its maximum under
physiological conditions. However, in pathospermia samples, where
the motility of spermatozoa is impaired and far from optimal, the
effect of MW appears to slightly, but significantly improve
motility, namely through an increase in the number of progressively
motile spermatozoa.
However, the response of the PA system to MW
exposure in pathospermia differed from that in normospermia and
demonstrated two types. In the first type of response, there was no
significant change in the levels of PA. In the second type of
response, the levels of both Spm and Spd significantly decreased,
but the Spm/Spd ratio increased, which resembled the response in
normozoospermia. It is interesting to note that according to the
medical history sheets data, the effectiveness of medical therapy
in pathospermia patients with the second type of response was
30-40% higher than in patients with the first type of response
(data not shown). Likely, the pathological changes in the membranes
are more entrenched with regard to the actual cell pathophysiology
in the patients who exhibit the first type of response than in the
patients who exhibit the second type of response, thus, their cells
do not respond as a physiological cell would be expected to, and
this may explain the poorer curability of such patients.
In conclusion, the biological effects of microwaves
on male gametes were shown. The protective and membrane-stabilizing
effects of MW are described, and the role of PA in the biological
effects of microwaves was determined. Differences in biological
reactions to MW irradiation in normospermia (healthy) and
pathospermia (men with impaired fertility) donors were also
revealed. Electromagnetic irradiation at a frequency of 42.194 GHz
and a wavelength of 7.1 nm, when used to treat human sperm for 20
min, resulted in certain specific biological effects without
thermal side-effects: i) No changes in morphology and practically
no effects on motility of spermatozoa were observed in healthy
samples; ii) it prevented the premature activation of acrosin in
samples from healthy donors, increasing the proacrosin/free acrosin
ratio by ~20%; iii) it increased the stability of the membranes of
sperm in the fertile samples, which was confirmed by the Milovanov
and Joel tests; iv) it caused a decrease in the levels of the
seminal plasma PA, and the decrease in the levels of Spd were more
pronounced; v) it reduced the number of apoptotic (AnV+/PI-)
gametes in the complete ejaculate from fertile men; vi) a decrease
in the number of apoptotic (AnV+/PI-) gametes was correlated with a
decrease in the levels of spermoplasm PA, which may indicate the
participation of seminal plasma PA in the biological effects of
microwaves; vii) it caused an increase in the motility of gametes
in pathospermia samples from the men with impaired fertility; viii)
in pathospermia, two types of reactions to the effects of MW
exposure were noted: in the first type of reaction, there were no
dynamics in the levels of spermoplasm PA; in the second type, the
trend in PA changes were similar to the reaction of normospermia
samples.
Supplementary Material
Detailed design of the study of
samples from fertile donors. The complete ejaculate was divided
into a Control F, Exp1 F and Exp2
F groups. The Control F group was processed
without MW treatment, whereas the Exp1 F and Exp2
F groups were treated with MW irradiation, but Exp2
F was preliminarily centrifugated to separate the
seminal plasma from spermatozoa, so that plasma and cells did not
interact during the MW exposure. In the final step, all the samples
were divided into seminal plasma and spermatozoa to explore the
corresponding parameters in both fractions.
Evaluation of sperm cell motility and
viability. The staining of sperm cells in (A) fertile and (B)
subfertile samples with eosin is shown. The arrow indicates a live
sperm, dead sperm colored with the eosin dye are depicted in a
red-orange color. The number of dead cells in (B) subfertile
samples is greater than that in (A) fertile samples. Magnification,
x100.
AnV+/PI-spermatozoa. The staining of
gametes with Annexin V-FITC for the determination of apoptosis in
(A and B) fertile and (C and D) subfertile samples is shown.
Spermatozoa are visible in the luminescence light (A nd C, dark
area) and in the transmitted light (B and D, light area). Green
fluorescence indicates (AnV+/PI-)-gametes. (E and F) Sections
demonstrate fertile samples before (control) and after (Exp1) the
MW exposure, only round heads of atypical gametes are colored (F).
Magnification, x100. AnV, Annexin V-FITC; PI, propidium
iodide.
Morphological characteristics of
spermatozoa from fertile men before and after low-intensity
millimeter-wavelength electromagnetic wave-exposure.b
Motility of spermatozoa from fertile
men before and after low-intensity millimeter-wavelength
electromagnetic wave exposure.b
Resistance of spermatozoa from fertile
men to acetic acid after exposure to low-intensity
millimeter-wavelength electromagnetic wave exposure.c
Acknowledgements
Not applicable.
Funding
Funding: This study has been supported by the RUDN University
Strategic Academic Leadership Program.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MVP conceived and designed the study, performed the
experiments and wrote the manuscript. DFZ, NRK and SVR recruited
the patients and controls, and collected the samples. EVN analyzed
the data, wrote and edited the manuscript and contributed to
conceptualization of the study. MLB, SPS, KS and AH analyzed the
data and edited the manuscript. MVP, DFZ, NRK and SVR confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The study has been carried out in accordance with
The Code of Ethics of the World Medical Association (Declaration of
Helsinki) and was approved by the Local Ethics Committee of the
Astrakhan State Medical University of the Health Ministry of the
Russian Federation (protocol no. 2; 21st May 2021). Informed
consent for participation in the study and use of their samples was
obtained from all participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Thackston KA, Deheyn DD and Sievenpiper
DF: Limitations on electromagnetic communication by vibrational
resonances in biological systems. Phys Rev E.
101(062401)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ziskin MC: Millimeter waves: acoustic and
electromagnetic. Bioelectromagnetics. 34:3–14. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Subbotina TI, Tereshkina OV, Khadartsev AA
and Yashin AA: Effect of low-intensity extremely high frequency
radiation on reproductive function in wistar rats. Bull Exp Biol
Med. 142:189–190. 2006.PubMed/NCBI View Article : Google Scholar : (In English,
Russian).
|
|
4
|
Nikoghosyan А, Heqimyan А and Ayrapetyan
S: Non-thermal microwave radiation-induced brain tissue dehydration
as a potential factor for brain functional impairment. Int J Basic
Appl Sci. 5:188–195. 2016.
|
|
5
|
Betskii OV, Devyatkov ND and Kislov VV:
Low intensity millimeter waves in medicine and biology. Crit Rev
Biomed Eng. 28:247–268. 2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tambiev AK and Kirikova NN: Novel concepts
of the causes of EHF-radiation-induced stimulating effects. Crit
Rev Biomed Eng. 28:60–76. 2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Iryanov YM and Kiryanov NA: Reparative
osteogenesis and angiogenesis in low intensity electromagnetic
radiation of ultra-high frequency. Vestn Ross Akad Med Nauk.
70:334–340. 2015.PubMed/NCBI View Article : Google Scholar : (In Russian).
|
|
8
|
Bae DH, Lane DJR, Jansson PJ and
Richardson DR: The old and new biochemistry of polyamines. Biochim
Biophys Acta Gen Subj. 1862:2053–2068. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Igarashi K and Kashiwagi K: The functional
role of polyamines in eukaryotic cells. Int J Biochem Cell Biol.
107:104–115. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ploskonos MV, Zulbalaeva DF, Kurbangalieva
NR and Ripp SV: Laboratory assessment of sperm apoptosis ability in
men with different fertility. The problems of reproduction.
26:77–84. 2020.
|
|
11
|
Hilal A, Ploskonos MV, Terentyev AA,
Syatkin SP, Neborak EV, Blagonravov ML, Protasov A, Kaitova Z and
Chibisov SM: Regulation of apoptosis of human immunocompetent cells
under the effect of polyamines. FEBS Open Bio. 8: (Suppl
1)(234)2018.
|
|
12
|
Fratini E, Cervelli M, Mariottini P,
Kanamori Y, Amendola R and Agostinelli E: Link between spermine
oxidase and apoptosis antagonizing transcription factor: A new
pathway in neuroblastoma. Int J Oncol. 55:1149–1156.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ploskonos MV, Syatkin SP, Neborak EV,
Hilal A, Sungrapova KY, Sokuyev RI, Blagonravov ML, Korshunova AY
and Terentyev AA: Polyamine analogues of propanediamine series
inhibit prostate tumor cell growth and activate the polyamine
catabolic pathway. Anticancer Research. 40:1437–1441.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ploskonos MV and Evdokimov VV: Polyamines
of urogenital tract men as factors of apoptosis regulation
spermatozoids. Urologiia. 4:74–79. 2019.PubMed/NCBI(In Russian).
|
|
15
|
Madeo F, Eisenberg T, Pietrocola F and
Kroemer G: Spermidine in health and disease. Science.
359(eaan2788)2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ozer Kaya S, Gur S, Erisir M, Kandemir FM,
Benzer F, Kaya E, Turk G and Sonmez M: Influence of vitamin E and
vitamin E-selenium combination on arginase activity, nitric oxide
level and some spermatological properties in ram semen. Reprod
Domest Anim. 55:162–169. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gapeev AB, Shved DM, Mikhaĭlik EN,
Korystov IuN, Levitman MKh, Shaposhnikova VV, Sadovnikov VB,
Alekhin AI, Goncharov NG and Chemeris NK: Antitumor effect of
low-intensity extremely high-frequency electromagnetic radiation on
a model of solid Ehrlich carcinoma. Biofizika. 54:1128–1136.
2009.PubMed/NCBI(In Russian).
|
|
18
|
World Medical Association. World Medical
Association Declaration of Helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194.
2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Korolev YN, Bobrovnitskii IP, Geniatulina
MS, Nikulina LA and Mikhailik LV: The ultrastructure of Sertoli
cells and spermatogonia in the rats exposed to radiation under
conditions of therapeutic and prophylactic application of
low-intensity electromagnetic emission. Vopr Kurortol Fizioter Lech
Fiz Kult. 95:35–40. 2018.PubMed/NCBI View Article : Google Scholar : (In Russian).
|
|
20
|
Korolev YN, Bragina EE, Nikulina LA and
Mikhailik LV: Action features of the of low-intensity
electromagnetic radiation at an early stage of the experimental
metabolic syndrome development induced by a diet high in
carbohydrates and fats. Vopr Kurortol Fizioter Lech Fiz Kult.
98:47–52. 2021.PubMed/NCBI View Article : Google Scholar : (In Russian).
|
|
21
|
Cooper TG, Noonan E, von Eckardstein S,
Auger J, Baker HW, Behre HM, Haugen TB, Kruger T, Wang C, Mbizvo MT
and Vogelsong KM: World Health Organization reference values for
human semen characteristics. Hum Reprod Update. 16:231–245.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
World Health Organization (WHO): WHO
laboratory manual for the examination and processing of human
semen. Vol 270. 5th edition. WHO, Geneva, 2010.
|
|
23
|
Dolgov VV, Lugovskaya SA and Fanchenko ND:
Laboratory diagnostics of male infertility: issued by the
Department of СLD, Moscow, p.145, 2006 (in Russian).
|
|
24
|
Schill WB: Acrosin activity in human
spermatozoa: Methodological investigations. Arch Dermatol Forsch.
248:257–273. 1973.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zahn A, Furlong LI, Biancotti JC,
Ghiringhelli PD, Marijn-Briggiler CI and Vazquez-Levin MH:
Evaluation of the proacrosin/acrosin system and its mechanism of
activation in human sperm extracts. J Reprod Immunol. 54:43–63.
2002.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Song J, Shan Z, Mao J and Teng W: Serum
polyamine metabolic profile in autoimmune thyroid disease patients.
Clin Endocrinology. 90:727–736. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Shohat B, Maayan R, Singer R, Sagiv M,
Kaufman H and Zukerman Z: Immunosuppressive activity and polyamine
levels of seminal plasma in azo-ospermic, oligospermic, and
normospermic men. Arch Androl. 24:41–50. 1990.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Fair WR, Clark RB and Wehner N: A
correlation of seminal polyamine levels and semen analysis in the
human. Fertil Steril. 23:38–42. 1972.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Shah GV, Sheth AR, Mugatwala PP and Rao
SS: Effect of spermine on adenyl cyclase activity of spermatozoa.
Experientia. 31:631–632. 1975.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Rubinstein S and Breitbart H: Cellular
localization of polyamines: Cytochemical and ultrastructural
methods providing new clues to polyamine function in ram
spermatozoa. Biol Cell. 81:177–183. 1994.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Benavides MP, Groppa MD, Recalde L and
Verstraeten SV: Effects of polyamines on cadmium- and
copper-mediated alterations in wheat (Triticum aestivum L) and
sunflower (Helianthus annuus L) seedling membrane fluidity. Arch
Biochem Biophys. 654:27–39. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Lefèvre PL, Palin MF and Murphy BD:
Polyamines on the reproductive landscape. Endocr Rev. 32:694–712.
2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Lundy SD, Sangwan N, Parekh NV, Selvam
MKP, Gupta S, McCaffrey P, Bessoff K, Vala A, Agarwal A, Sabanegh
ES, et al: Functional and taxonomic dysbiosis of the gut, urine,
and semen microbiomes in male infertility. Eur Urol. 79:826–836.
2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Ivanov IP, Rohrwasser A, Terreros DA,
Gesteland RF and Atkins JF: Discovery of a spermatogenesis
stage-specific ornithine decarboxylase antizyme: Antizyme 3. Proc
Natl Acad Sci USA. 97:4808–4813. 2000.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Korzun IA, Ploskonos MV, Syatkin SP,
Blagonravov ML, Gushchina YuSh, Eremina IZ, Kaitova ZS, Navid MN
and Aissa AA: Components of seminal plasma as factors regulating
apoptosis of male gametes. FEBS Open Bio. 9 (Suppl 1)(370)2019.
|
|
36
|
Hilal A, Ploskonos MV, Syatkin SP, Neborak
EV, Maksimova TV and Terentev AA: Apoptosis markers of
spermatozoids and polyamines of human spermoplasm. FEBS Open Bio. 9
(Suppl 1)(165)2019.PubMed/NCBI
|
|
37
|
Agostinelli E: Biochemical and
pathophysiological properties of polyamines. Amino Acids.
52:111–117. 2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Bekebrede AF, Keijer J, Gerrits WJJ and
Boer VCJ: The molecular and physiological effects of
protein-derived polyamines in the intestine. Nutrients.
12(197)2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Hussain T, Tan B, Ren W, Rahu N, Dad R,
Kalhoro DH and Yin Y: Polyamines: Therapeutic perspectives in
oxidative stress and inflammatory diseases. Amino Acids.
49:1457–1468. 2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Syatkin SP, Kirichuk AA, Soldatenkov AT,
Kutyakov SV, Neborak EV, Shevkun NA, Kuznetsova OM, Skorik AS and
Terent'ev AA: Screening of some dioxaboreninopyridine and aniline
derivatives for carcinogenic properties using a model cell-free
system of regenerating rat liver. Bull Exp Biol Med. 162:801–807.
2017.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Syatkin SP, Neborak EV, Khlebnikov AI,
Komarova MV, Shevkun NA, Kravtsov EG, Blagonravov ML and
Agostinelli E: The investigation of structure-activity relationship
of polyamine-targeted synthetic compounds from different chemical
groups. Amino Acids. 52:199–211. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Zhao R, Liu Y, Liu S, Luo T, Zhong GY, Liu
A, Zeng Q and Xin SX: Apoptosis-promoting effects on A375 human
melanoma cells induced by exposure to 35.2-GHz millimeter wave.
Technol Cancer Res Treat. 19(1533033820934131)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Jänne J, Hölttä E, Haaranen P and Elfving
K: Polyamines and polyamine-metabolizing enzyme activities in human
semen. Clin Chim Acta. 48:393–401. 1973.PubMed/NCBI View Article : Google Scholar
|