Introduction
Pericoronitis is the inflammation of soft tissues
around the crown of an erupting or partially erupted tooth
(1-3).
Based on the published guidelines for chronic pericoronitis
treatment and prevention of chronic or acute exacerbation (1,4),
surgery and the application of antimicrobial agents are recommended
as the most appropriate interventions. Furthermore, the health
status of the patient should be considered during the evaluation.
For example, removing an impacted third molar helps reduce pain and
other symptoms, and improves oral health and function for patients
(5,6). However, information remains limited
regarding considerations for the safe and effective implementation
of oral/dental surgical interventions in patients with chronic
medical comorbidities, such as schizophrenia and isovaleric
acidemia (IVA).
Schizophrenia, recently renamed integration
dysregulation syndrome in Japan (togo-shitcho-sho) (7), is a severe mental disorder resulting
from an interplay of multiple factors, including genetic causes,
and several environmental and psychosocial factors. The disease is
a public health problem, which affects ~24 million people or 1 in
300 people (0.32%) worldwide and is associated with significant
morbidity and premature mortality in individuals between the ages
of 10 and 20 years old (8,9). It has been reported that patients with
schizophrenia present profound alterations in thought, language,
perception and sense of self, with impaired social and occupational
functioning (9). The manifestation
and progression of symptoms also vary between individuals (10). Additionally, it has several
subtypes, including paranoid, catatonic, disorganized and
undifferentiated (9), diagnosed
through the primary presenting symptoms. These symptoms are
classified into three main categories: i) Positive symptoms,
including delusions, hallucinations, disordered thoughts and
behavior; ii) negative symptoms, such as apathy, social withdrawal
and blunted effects; and iii) cognitive symptoms, such as
impairment of attention, information processing and memory
(1,11). Furthermore, schizophrenia can result
in severe dental and periodontal diseases, including chronic
pericoronitis requiring surgery. In addition, the management of
comorbid dental diseases is associated with several challenges,
especially anesthesia-related complications during surgery. Such
challenges include the coexistence of physical illnesses, dangerous
behaviors and serious side effects from drug interactions between
antipsychotic and anesthetic agents (12,13).
IVA (MIM #243500) is a rare autosomal recessive
congenital metabolic disorder categorized as organic acidemia
(14). Homozygous mutations cause
IVA in the isovaleryl-CoA dehydrogenase gene (IVD; MIM #607036) on
chromosome 15q14-15(14).
Furthermore, IVA is relatively uncommon, with a frequency of
1:250,000, 1:365,000 and 1:62,500 births in the United States,
Taiwan and Germany, respectively (15,16).
IVA disorder results from an accumulation of isovaleric acid in the
body, which is toxic to the central nervous system (17). During IVA crises, detoxification is
achieved through alternative pathways that produce isovaleric
glycine, 3-hydroxyisovaleric acid and other metabolites excreted
via the urinary system. Gas chromatography/mass spectrometry
(GC/MS) is the ideal means of identifying the organic acidemia
metabolites (18,19). IVA exists in two forms: The acute
neonatal form, which leads to substantial metabolic acidosis from
the first days of life, and results in an individual succumbing to
the disease fairly rapidly (20),
and a chronic state in which severe ketoacidosis occurs
intermittently in older age groups (14). In both IVA forms, acute episodes of
metabolic decompensation can appear during catabolic states due to
impaired protein and fatty acid metabolism, infection, fasting and
other physiological stresses (21,22).
Patients with IVA requiring surgery also present various challenges
to the choice of anesthesia, as certain anesthetics can trigger
metabolic crises, including poor nutrition, electrolyte imbalance,
prolonged periods of fasting and other forms of stress (23). Despite various studies on IVA, there
are few reports on its perioperative management. Moreover, there
are no reports on adult surgery in patients with IVA, to the best
of our knowledge.
Through careful perioperative evaluation and
management strategies, significant challenges to dental surgery in
patients with coexisting comorbidities, such as schizophrenia and
IVA, can be minimized (1). The
present case report describes the unusual encounter and management
of a 20-year-old man suffering from bilaterally and partially
erupted third molar associated with chronic pericoronitis and
dental caries of the maxilla wisdom teeth with coexisting
schizophrenia and IVA. The pericoronitis was treated through
surgical removal of the third molar and the antagonistic maxilla
wisdom teeth under regional anesthesia. The patient recovered well
without any reported complications after 1 year of follow-up.
Case report
Patient information
A 20-year-old Japanese male patient was referred to
the Oral and Maxillofacial Department at Ryukyu University Hospital
in December 2020, with a history of bilateral chronic
pericoronitis. The patient was previously diagnosed with IVA at the
age of 5 years and 6 months old, as reported by his accompanying
mother - the next of kin. He had repeated fever, anemia, vomiting
and thrombocytopenia since the neonatal stage. GC/MS was performed
since the symptoms persisted, including vomiting, the distinct odor
of sweaty feet and general malaise, which were indicated by
isovaleryl glycine (114.7 ratio/mg; creatinine > undetected),
3-hydroxy-isovaleric acid (20.7 ratio/mg; creatinine >0.72),
4-hydroxy-isovaleric acid, 2-methyl succinic acid and 2-methyl
fumaric acid levels in the patient's urine specimen. Furthermore,
the patient was under treatment for undifferentiated schizophrenia
disorder, diagnosed in May 2020 at the Psychiatry Department of
Ryukyu University Hospital. The treatment for IVA included
L-aspartate Ca (one tablet, every 8 h daily), levocarnitine 250 mg
(twice daily with meals) and glycine 6.5 g daily. Additionally, the
treatment for schizophrenia was a second-generation antipsychotic
drug, Zyprexa (olanzapine) 10 mg, one tablet a day. He had neither
history of smoking nor drug addiction, no family history of
congenital anomalies and denied having any allergies. On
examination, although slightly nervous and anxious, he was not
agitated, uncooperative, or violent when approached by the
healthcare providers. Moreover, he was in good general condition,
with no pallor, oedema, jaundice, cervical or generalized
lymphadenopathy. His systemic examinations were also within normal
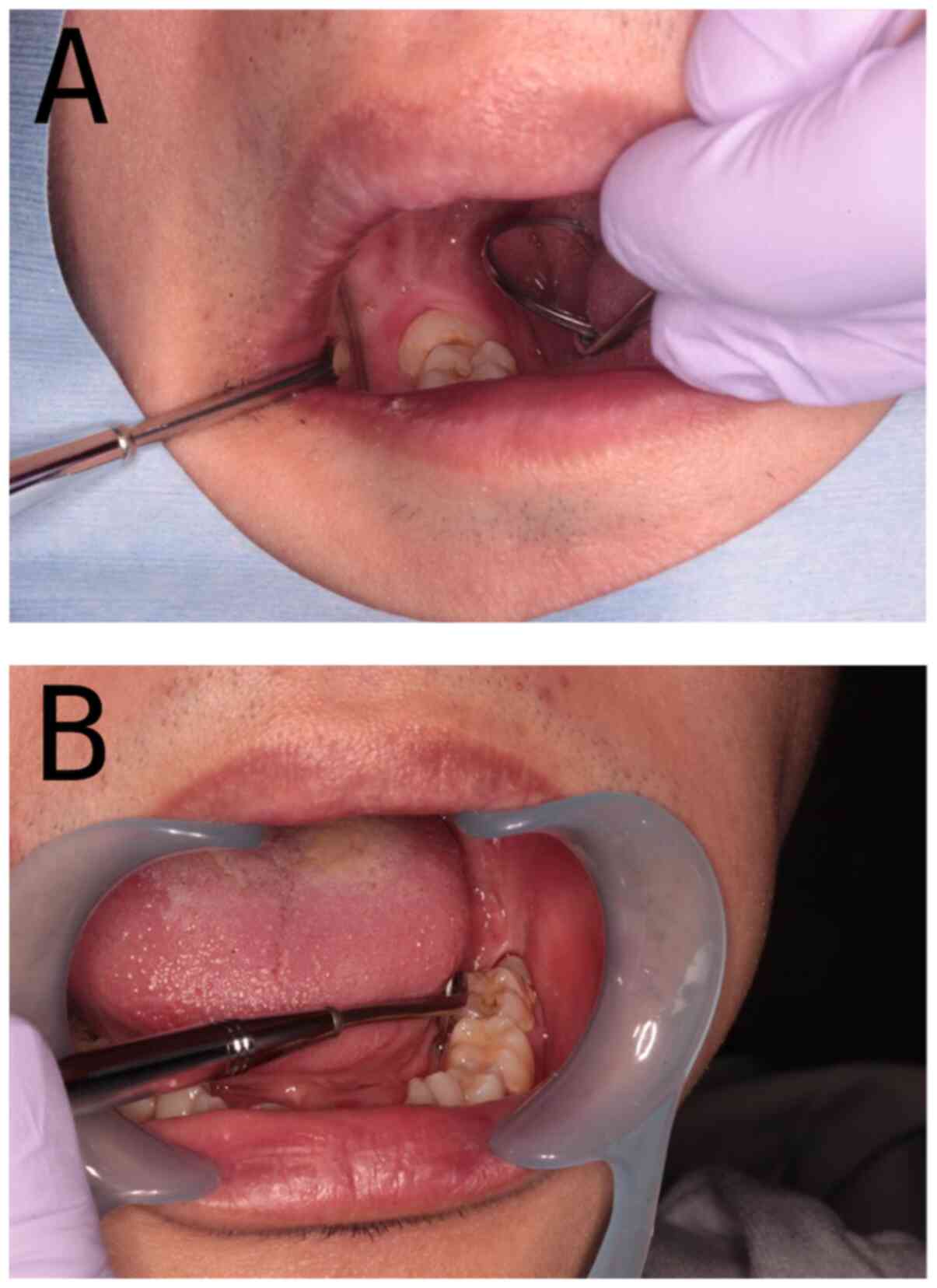
limits. Nevertheless, intraoral investigations revealed incomplete
eruption of the mandible wisdom teeth (also referred to as
mandibular or lower third molars) bilaterally with only a part of
the tooth's crown exposed in the oral cavity (Fig. 1). The operculum, the soft tissue
covering the partially visible crowns, also appeared slightly
inflamed. Additionally, we observed dental caries affecting the
fully erupted maxilla wisdom teeth bilaterally.
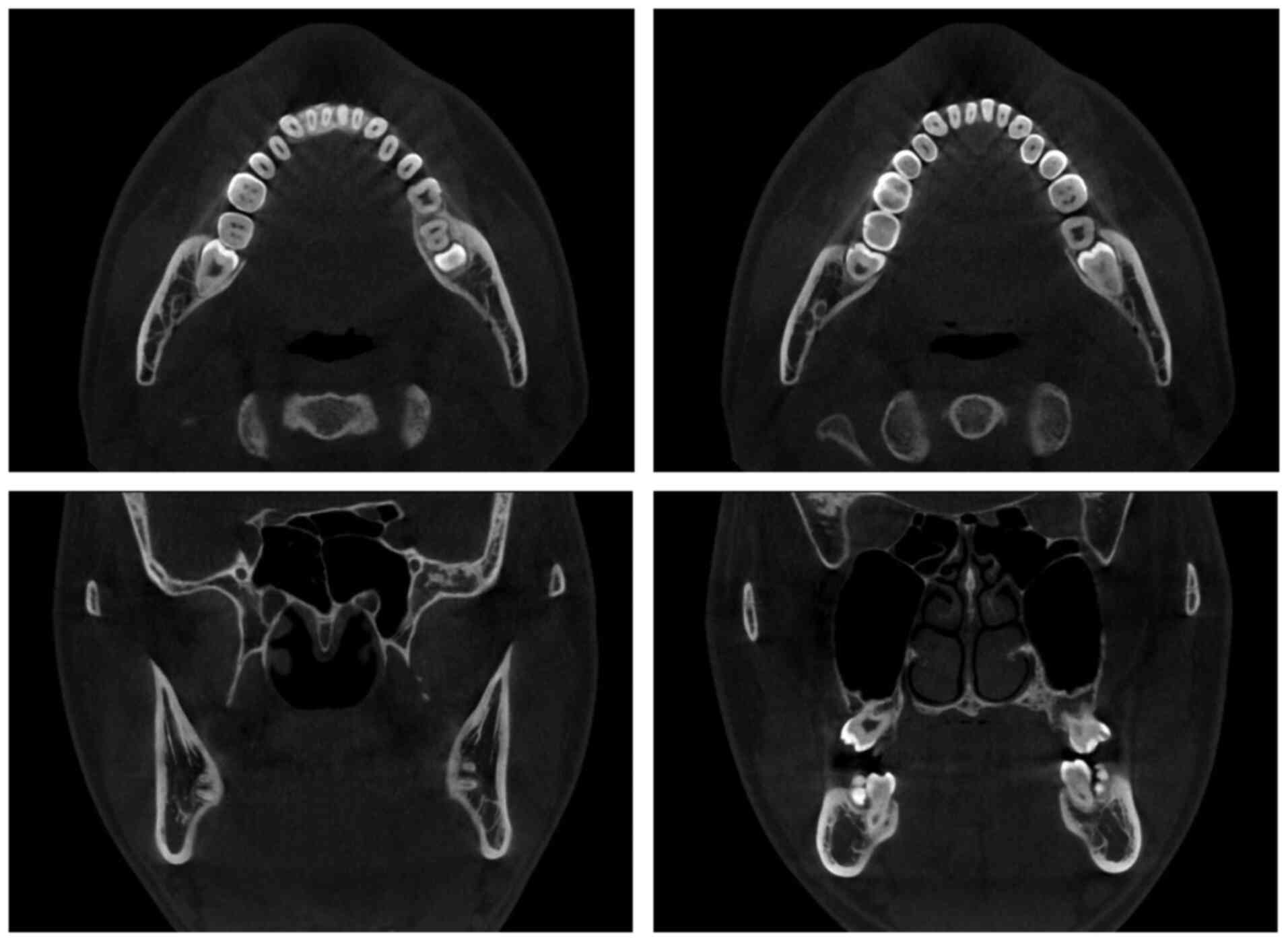
Investigations
Panoramic radiographic examination and cone-beam
computed tomography revealed that both lower third molars had
incomplete root development and were close to the mandibular canal
without bone involvement (Figs. 2
and 3). Alternatively,
electrocardiography (ECG) and echocardiogram did not indicate any
abnormalities. The blood biochemistry hematology results are shown
in Table I. As shown, no
abnormalities were observed in blood cells, renal function, and
liver function. Although some amino acid values were slightly
outside of reference values, a correction was not necessary.
 | Table IPreoperative hematology and
biochemistry laboratory test results. |
Table I
Preoperative hematology and
biochemistry laboratory test results.
| Analyte | Patient results | Reference
intervals | Units | Notes |
|---|
| White blood cell
count | 6.7 | 3.3-8.6 |
x103/µl | - |
| Neutrophils | 44.1 | 40.0-71.0 | % | - |
| Lymphocytes | 41.2 | 26.0-46.0 | % | - |
| Monocytes | 9.4 | 2.0-7.0 | % | High |
| Eosinophils | 4.6 | 0.0-6.0 | % | - |
| Basophils | 0.7 | 0.0-1.0 | % | - |
| Red blood cell
count | 5.03 | 4.35-5.55 |
x106/µl | - |
| Hemoglobin | 15.5 | 13.7-16.8 | g/dl | - |
| Biochemistry | | | | - |
| Blood urea
nitrogen | 10 | 8.0-20.0 | mg/dl | - |
| Serum
creatinine | 0.72 | 0.65-1.07 | mg/dl | - |
| Estimated
glomerular filtration rate | 117.6 | | | - |
| Total
bilirubin | 0.7 | 0.4-1.5 | mg/dl | - |
| Aspartate
aminotransferase | 25 | 13-30 | U/l | - |
| Alanine
aminotransferase | 41 | 10-42 | U/l | - |
| γ-glutamyl
transferase | 13 | 13-64 | U/l | - |
| Taurine | 37.9 | 39.5-93.2 | nmol/ml | Low |
| Aspartic acid | 2.7 | <2.4 | nmol/ml | High |
| Hydroxyproline | 15.3 | <21.6 | nmol/ml | - |
| Threonine | 108.5 | 66.5-188.9 | nmol/ml | - |
| Serine | 108.2 | 72.4-164.5 | nmol/ml | - |
| Asparagine | 37.0 | 44.7-96.8 | nmol/ml | Low |
| Glutamic acid | 31.0 | 12.6-62.5 | nmol/ml | - |
| Glutamine | 477.9 | 422.1-703.8 | nmol/ml | - |
| Sarcosine | TR | TR | nmol/ml | - |
| α-Aminoadipic
acid | ND | ND | nmol/ml | - |
| Proline | 225.9 | 78.8-272.7 | nmol/ml | - |
| Glycine | 324.0 | 151.0-351.0 | nmol/ml | - |
| Alanine | 348.7 | 208.7-522.7 | nmol/ml | - |
| Citrulline | 29.7 | 17.1-42.6 | nmol/ml | - |
| α-Aminobutyric
acid | 11.6 | 7.9-26.6 | nmol/ml | - |
| Valine | 259.4 | 147.8-307.0 | nmol/ml | - |
| Cystine | 10.6 | 13.7-28.3 | nmol/ml | Low |
| Cystathionine | ND | TR | nmol/ml | - |
| Methionine | 20.7 | 18.9-40.5 | nmol/ml | - |
| Isoleucine | 96.8 | 43.0-112.8 | nmol/ml | - |
| Leucine | 147.4 | 76.6-171.3 | nmol/ml | - |
| Tyrosine | 58.4 | 40.4-90.3 | nmol/ml | - |
| Phenylalanine | 58.1 | 42.6-75.7 | nmol/ml | - |
| γ-Amino
β-hydroxybutyric acid | ND | ND | nmol/ml | - |
| β-Alanine | 3.9 | TR | nmol/ml | - |
| β-Amino-iso-butyric
acid | ND | TR | nmol/ml | - |
| γ-Aminobutyric
acid | ND | ND | nmol/ml | - |
|
Monoethanolamine | 9.4 | <10.4 | nmol/ml | - |
| Homocysteine | ND | ND | nmol/ml | - |
| Histidine | 90.1 | 59.0-92.0 | nmol/ml | - |
|
3-Methylhistidine | 4.0 | <5.0 | nmol/ml | - |
|
1-Metnylhisticline | TR | <18.5 | nmol/ml | - |
| Carnosine | ND | ND | nmol/ml | - |
| Anserine | ND | ND | nmol/ml | - |
| Tryptophan | 54.8 | 37.0-74.9 | nmol/ml | - |
| Hydroxylysine | ND | ND | nmol/ml | - |
| Ornithine | 56.9 | 31.3-104.7 | nmol/ml | - |
| Lysine | 177.3 | 108.7-242.2 | nmol/ml | - |
| Arginine | 96.4 | 53.6-133.6 | nmol/ml | - |
Treatment and follow-up
Considering published reports (1,4), the
appropriate treatment/prevention strategy for comorbid dental
diseases in IVA and schizophrenia diagnosis was surgery and
antibiotic administration. Notably, the patient and his next of kin
also preferred surgery under general anesthesia (GA). However,
considering his medical history, the following perioperative
management strategies were implemented to minimize the risk factors
of complications: i) The surgical team chose regional anesthesia
(RA) to avoid IVA crises of disordered metabolism, including
glucose disturbances, hyperammonemia, hypocalcemia and non-anion
gap metabolic acidosis due to GA-associated prolonged fasting, poor
nutrition, electrolyte imbalance and other physiological stresses;
ii) 3% mepivacaine, and not bupivacaine or lidocaine, was selected
as the preferred drug for RA to reduce the risk of developing local
anesthetic systemic toxicity (LAST) based on the report of a
patient having a reduced threshold for developing malignant
dysrhythmias due to IVA-associated carnitine deficiency (24,25);
iii) since IVA can cause bone marrow suppression during crises,
postoperative infection was considered a risk factor for IVA
crises. Therefore, although bone marrow suppression was not
observed in blood biochemistry hematology results, we planned to
adequately prevent infection with antibacterial agents before and
after surgery (21,22); iv) antibiotics other than
pivalate-containing medications were used as IVA raises
acylcarnitine levels, and antibiotics containing pivalate already
have the possibility of increasing acylcarnitine levels (26); v) tooth extraction was conducted in
stages to avoid trismus related to removing all four teeth
immediately and seizures of IVA crisis due to poor eating; vi) the
patient was managed as an outpatient to reduce psychological stress
related to the coexisting pandemic restrictions for preventing
coronavirus disease-2019 caused by severe acute respiratory
syndrome coronavirus 2; and vii) although investigations revealed
normal ECG and echocardiogram findings, the continuation of
antipsychotic therapy, olanzapine, was evaluated in consultation
with the attending psychiatrist to avoid side effects of drug
interactions. The first stage involved removing the right
mandibular wisdom tooth, the second stage involved removing the
left mandibular wisdom tooth and the third stage involved removing
the bilateral maxilla wisdom teeth. During and shortly after
surgery, all the patient's vitals, including his level of
consciousness, pulse rate, percutaneous oxygen saturation and blood
pressure, were regularly monitored. To further reduce psychological
stress, the patient's favorite music was played. Infection
prevention involved 1,000 mg cefazolin sodium, administered
intravenously 30 min before the operation and oral amoxicillin (250
mg) every 8 h for 3 days after the operation.
Tooth extraction was performed as previously
described (27). A minimum of two
ampoules of 3% mepivacaine was used for each extraction stage.
Then, the gingiva was incised with a scalpel to show the alveolar
bone clearly. Next, we split a portion of the mandibular bone
around the exposed crown to extract the tooth by dividing the crown
and root. The incised soft tissue part was subsequently closed with
a suture. Finally, the maxilla wisdom teeth were extracted with an
elevator. Skilled oral surgeons performed the surgery to shorten
the operation time. Therefore, we completed all three different
stages of the operation within 30 min. Hemostasis was also
confirmed 30 min after surgery. Upon completing each surgical
procedure, the patient was instructed to avoid strenuous exercise,
drinking alcohol and long baths for a week. Pain medication, which
included 60 mg of loxoprofen sodium hydrate every 8 h for 7 days,
was also prescribed. However, no specific dietary restrictions were
applied.
Follow-up of the patient was done a day after
surgery and 7 days later. We physically examined the patient during
the scheduled 7th-day visit and removed the sutures simultaneously.
The patient recovered well after surgery without prolonged pain,
infection or loss of neurological function (Fig. 4) and he remained symptom-free after
1 year of follow-up.
Discussion
The past several decades have shown growing interest
in managing oral/dental diseases in patients with comorbid mental
and/or somatic disorders (28-30).
However, the practice of safe and effective oral/dental medicine in
patients with chronic and rare medical comorbidities remains
challenging. This case report describes a patient who suffered
chronic pericoronitis associated with bilateral lower third molar
impaction and dental caries in the antagonistic maxilla wisdom
teeth amid a coexistence of two medical conditions: Schizophrenia
and a rare congenital error of metabolism, IVA. These comorbid
dental diseases, coupled with two chronic and life-threatening
medical conditions, one of which is rare, is an unusual encounter
in dental surgery that is seldomly published. Nevertheless, the
case considers careful perioperative management strategies despite
the limited number of published guidelines or information on the
subject.
Schizophrenia is a complex, multifactorial disorder
with varying clinical presentations and progression of symptoms in
different individuals (10).
Therefore, the disease has several subtypes, including the
undifferentiated subtype diagnosed in this patient. However, the
patient appeared stabilized with prescribed antipsychotic agents,
given the relative calmness and cooperation exhibited in each of
the three stages of the surgical intervention. Second-generation
antipsychotic agents for management of schizophrenia, such as
olanzapine, can affect several receptor sites, including histamine,
serotonin, acetylcholine, α-adrenergic and dopaminergic receptors.
They also cause blurred vision, constipation, dry mouth, urinary
retention, sedation, hypotension and extrapyramidal movements.
Furthermore, the preoperative use of antipsychotics makes
schizophrenic patients more susceptible to the hypotensive action
of GA (13). However, discontinuing
antipsychotics can increase psychotic symptoms, such as
hallucinations and agitation. Therefore, patients with chronic
schizophrenia should continue their antipsychotics pre-operatively,
as abrupt withdrawal may cause psychotic symptom recurrence
(31). Here, although the choice of
RA was the most appropriate approach for the surgical removal of
the impacted third molars and the antagonist maxilla wisdom teeth
in this case, regular consultations with the attending psychiatrist
revealed that the patient was on glycine treatment; whose
short-lasting impact on serotonin levels can reduce the side
effects of the second-generation antipsychotic drugs. Therefore,
there was no need to discontinue antipsychotics in the
perioperative period.
Additionally, the patient had a congenital error of
metabolism, an organic acidemia of the IVA type. Patients with IVA
can successfully be treated with GA using agents like sevoflurane,
nitrous oxide, thiopental, fentanyl, desflurane, nitrous oxide and
vecuronium (23). However, reported
incidences of development of ventricular tachycardia shortly after
bupivacaine and epinephrine injection (25), and cardiac arrest following the use
of lidocaine as an RA agent have also been reported (24). Similarly, a report of a patient
having a reduced threshold for developing malignant dysrhythmias
due to IVA-associated carnitine deficiency has been described
(25). Moreover, patients with IVA
are at risk of acute acidosis and metabolic decompensation, largely
due to intercurrent illnesses or other physiological stresses,
including fasting (21,22). Furthermore, IVA is a disease that
raises acylcarnitine levels (32).
Therefore, avoiding antibiotics containing pivalate, which can
increase acylcarnitine levels is recommended (26). It has also been reported that
pancytopenia, isolated neutropenia and thrombocytopenia can occur
due to bone marrow suppression (33).
For the above reasons, it is paramount that patients
with IVA are subjected to a detailed management action plan that
can effectively reduce the risks of complications of surgery. Here
the patient requested surgery to be performed under GA. However,
prolonged fasting before GA poses a high risk of acute acidosis and
life-threatening metabolic decompensation. Hence, surgery was
performed under RA instead. Furthermore, the extraction of multiple
highly invasive wisdom teeth at once would have resulted in
deficient nutrient intake due to trismus and bleeding. Therefore,
surgery was divided into three stages to avoid stress and dietary
problems. When selecting local anesthetics, bupivacaine and
lidocaine were not considered to prevent the risk of the
development of LAST, which can trigger an IVA crisis (34). Moreover, the use of olanzapine for
schizophrenia also contraindicated adrenaline-containing lidocaine
as an RA agent (35). Hence, 3%
mepivacaine was chosen as a local anesthetic instead due to its
superior anesthetic effect and limited probability of severe side
effects. Similarly, although bone marrow suppression was not
observed in blood sampling, adequate plans were made to prevent
infection using broad-spectrum antibacterial agents. Furthermore,
while avoiding pivalate-containing options, antibiotics comprised
of intravenous cefazolin sodium (1,000 mg) 30 min before the
operation and oral amoxicillin were administered 3 days after the
procedure. Finally, efforts were made to minimize psychological and
other stresses due to surgery. First, the surgery was performed
while playing the patient's favorite music and taking breaks from
time to time. Secondly, all operations were performed by
experienced dentists familiar with oral surgery to shorten the
operational time, and finally the operating procedure was divided
into three stages.
Here, the unusual case of successful oral surgical
treatment in a patient with two coexisting chronic medical
conditions is described. The surgical management of comorbid dental
diseases in mental and metabolic disorders is associated with an
increased risk of postoperative complications. However, safe and
effective treatment is achievable with careful perioperative
considerations, as highlighted above.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed for the case
report are available from the corresponding author on reasonable
request.
Authors' contributions
SM and EHN contributed to the drafting of the
manuscript. SM, EHN, YC, TG and KN performed the literature search.
SM, EHN, TG, JS, SG, TK and HN collected the data and assisted in
drafting the case report section. SM was the primary surgeon. SM,
EHN, YS, KN and HN critically revised the manuscript. All authors
have read and approved the final manuscript. All authors confirm
the authenticity of all raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for both the surgical treatment and publication of any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Schmidt J, Kunderova M, Pilbauerova N and
Kapitan M: A review of evidence-based recommendations for
pericoronitis management and a systematic review of antibiotic
prescribing for pericoronitis among dentists: Inappropriate
pericoronitis treatment is a critical factor of antibiotic overuse
in dentistry. Int J Environ Res Public Health.
18(6796)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Singh P, Nath P, Bindra S, Rao SS and
Reddy KR: The predictivity of mandibular third molar position as a
risk indicator for pericoronitis: A prospective study. Natl J
Maxillofac Surg. 9:215–221. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nitzan DW, Tal O, Sela MN and Shteyer A:
Pericoronitis: A reappraisal of its clinical and microbiologic
aspects. J Oral Maxillofac Surg. 43:510–516. 1985.PubMed/NCBI View Article : Google Scholar
|
|
4
|
McArdle LW and Renton T: The effects of
NICE guidelines on the management of third molar teeth. Br Dent J.
213(E8)2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
World Health Organization (WHO):
International Statistical Classification of Diseases and Related
Health Problems. 10th revision. WHO, Geneva, pICD-10, 2010.
|
|
6
|
Phillips C, Norman J, Jaskolka M, Blakey
GH, Haug RH, Offenbacher S and White RP Jr: Changes over time in
position and periodontal probing status of retained third molars. J
Oral Maxillofac Surg. 65:2011–2017. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Maruta T and Matsumoto C: Renaming
schizophrenia. Epidemiol Psychiatr Sci. 28:262–264. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tiihonen J, Lönnqvist J, Wahlbeck K,
Klaukka T, Niskanen L, Tanskanen A and Haukka J: 11-year follow-up
of mortality in patients with schizophrenia: A population-based
cohort study (FIN11 study). Lancet. 374:620–627. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
World Health Organization (WHO): Chapter
5: Mental and behavioral disorders-Schizophrenia, schizotypal and
delusional disorders. In: International Statistical Classification
of Diseases and Related Health Problems. 10th Revision. WHO,
Geneva, ppF20-F29, 2019. https://icd.who.int/browse10/2019/en.
|
|
10
|
Galletly C, Castle D, Dark F, Humberstone
V, Jablensky A, Killackey E, Kulkarni J, McGorry P, Nielssen O and
Tran N: Royal Australian and New Zealand College of Psychiatrists
clinical practice guidelines for the management of schizophrenia
and related disorders. Aust NZJ Psychiatry. 50:410–472.
2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kay SR, Fiszbein A and Opler LA: The
positive and negative syndrome scale (PANSS) for Schizophrenia.
Schizophr Bull. 13:261–276. 1987.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chua-Tuan JL: Surgical adverse outcomes in
patients with Schizophrenia: A population-based study. J Emerg Med.
5:1061–1062. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kudoh A: Perioperative management for
chronic schizophrenic patients. Anaesth Analg. 101:1867–1872.
2005.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tanaka K, Budd MA, Efron ML and
Isselbacher KJ: Isovaleric acidemia: A new genetic defect of
leucine metabolism. Proc Natl Acad Sci USA. 56:236–242.
1966.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lin WD, Wang CH, Lee CC, Lai CC, Tsai Y
and Tsai FJ: Genetic mutation profile of isovaleric acidemia
patients in Taiwan. Mol Genet Metab. 90:134–139. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ensenauer R, Vockley J, Willard JM, Huey
JC, Sass JO, Edland SD, Burton BK, Berry SA, Santer R, Grünert S,
et al: A common mutation is associated with a mild, potentially
asymptomatic phenotype in patients with isovaleric acidemia
diagnosed by newborn screening. Am J Hum Genet. 75:1136–1142.
2004.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Grünert SC, Wendel U, Lindner M,
Leichsenring M, Schwab KO, Vockley J, Lehnert W and Ensenauer R:
Clinical and neurocognitive outcome in symptomatic isovaleric
acidemia. Orphanet J Rare Dis. 7(9)2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tanaka K and Isselbacher KJ: The isolation
and identification of N-isovalerylglycine from urine of patients
with isovaleric acidemia. J Biol Chem. 242:2966–2972.
1967.PubMed/NCBI
|
|
19
|
Vockley J and Ensenauer R: Isovaleric
acidemia: New aspects of genetic and phenotypic heterogeneity. Am J
Med Genet C Semin Med Genet. 142:95–103. 2006.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Newman CG, Wilson BD, Callaghan P and
Young L: Neonatal death associated with isovalericacidaemia.
Lancet. 2:439–442. 1967.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Berry GT, Yudkoff M and Segai S:
Isovaleric acidemia: Medical and neurodevelopmental effects of
long-term therapy. J Pediatr. 113 (1 Pt 1):58–64. 1998.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tanaka K: Isovaleric acidemia: Personal
history, clinical survey and study of the molecular basis. Prog
Clin Biol Res. 321:273–290. 1990.PubMed/NCBI
|
|
23
|
Yeoh C, Teng H, Jackson J, Hingula L, Irie
T, Legler A, Levine C, Chu I, Chai C and Tollinche L: Metabolic
disorders and anaesthesia. Curr Anesthesiol Rep. 9:340–359.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mrad S, El Tawil C, Sukaiti WA, Bou Chebl
R, Abou Dagher G and Kazzi Z: Cardiac arrest following liposuction:
A case report of lidocaine toxicity. Oman Med J. 34:341–344.
2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Weinberg GL, Laurito CE, Geldner P, Pygon
BH and Burton BK: Malignant ventricular dysrhythmias in a patient
with isovaleric acidemia receiving general and local anaesthesia
for suction lipectomy. J Clin Anaesth. 9:668–670. 1997.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Holme E, Greter J, Jacobson CE, Lindstedt
S, Nordin I, Kristiansson B and Jodal U: Carnitine deficiency
induced by pivampicillin and pivmecillinam therapy. Lancet.
2:469–473. 1989.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Porto GG, Vasconcelos BC, Gomes AC and
Albert D: Evaluation of lidocaine and mepivacaine for inferior
third molar surgery. Med Oral Patol Oral Cir Bucal. 12:E60–E64.
2007.PubMed/NCBI
|
|
28
|
Šarac Z, Zovko R, Ćurlin M and Filaković
P: Dental medicine and psychiatry: The need for collaboration and
bridging the professional gap. Psychiatr Danub. 32:151–158.
2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Šimunović Filipčić I and Filipčić I:
Schizophrenia and physical comorbidity. Psychiatr Danub. 30 (Suppl
4):S152–S157. 2018.PubMed/NCBI
|
|
30
|
Jakovljevic M and Borovecki F:
Epigenetics, resilience, comorbidity and treatment outcome.
Psychiatr Danub. 30:242–253. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kudoh A, Katagai H, Takase H and Takazawa
T: Effect of preoperative discontinuation of antipsychotics in
schizophrenic patients on outcome during and after anaesthesia. Eur
J Anaesthesiol. 21:414–416. 2004.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Vreken P, Van Lint AE, Bootsma AH,
Overmars H, Wanders RJ and Van Gennip AH: Quantitative plasma
acylcarnitine analysis using electrospray tandem mass spectrometry
for the diagnosis of organic acidaemias and fatty acid oxidation
defects. J Inherit Metab Dis. 22:302–306. 1999.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kelleher JF Jr, Yudkoff M, Hutchinson R,
August CS and Cohn RM: The pancytopenia of isovaleric acidemia.
Pediatrics. 65:1023–1027. 1980.PubMed/NCBI
|
|
34
|
Macfarlane AJR, Gitman M, Bornstein KJ,
El-Boghdadly K and Weinberg G: Updates in our understanding of
local anaesthetic systemic toxicity: A narrative review.
Anaesthesia. 76 (Suppl 1):S27–S39. 2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Elvir-Lazo OL, White PF, Cruz Eng H, Yumul
F, Chua R and Yumul R: Impact of chronic medications in the
perioperative period-anesthetic implications (Part II). Postgrad
Med. 133:920–938. 2021.PubMed/NCBI View Article : Google Scholar
|